Abstract
Introduction
The largest cohort of critically ill patients evaluating intragastric and small intestinal delivery of nutrients was recently reported. This systematic review included recent data to compare the effects of small bowel and intragastric delivery of enteral nutrients in adult critically ill patients.
Methods
This is a systematic review of all randomised controlled studies published between 1990 and March 2013 that reported the effects of the route of enteral feeding in the critically ill on clinically important outcomes.
Results
Data from 15 level-2 studies were included. Small bowel feeding was associated with a reduced risk of pneumonia (Relative Risk, RR, small intestinal vs. intragastric: 0.75 (95% confidence interval 0.60 to 0.93); P = 0.01; I2 = 11%). The point estimate was similar when only studies using microbiological data were included. Duration of ventilation (weighted mean difference: -0.36 days (-2.02 to 1.30); P = 0.65; I2 = 42%), length of ICU stay (WMD: 0.49 days, (-1.36 to 2.33); P = 0.60; I2 = 81%) and mortality (RR 1.01 (0.83 to 1.24); P = 0.92; I2 = 0%) were unaffected by the route of feeding. While data were limited, and there was substantial statistical heterogeneity, there was significantly improved nutrient intake via the small intestinal route (% goal rate received: 11% (5 to 16%); P = 0.0004; I2 = 88%).
Conclusions
Use of small intestinal feeding may improve nutritional intake and reduce the incidence of ICU-acquired pneumonia. In unselected critically ill patients other clinically important outcomes were unaffected by the site of the feeding tube.
Similar content being viewed by others
Introduction
In the critically ill, nutritional therapy is a component of standard care. Delivery into the gastrointestinal tract is the preferred route of nutrient administration, via a tube into either the stomach or small intestine [1]. However, whether these feeding tubes should be preferentially placed into the stomach or small intestine remains contentious. Several clinical practice guidelines have recommended that enteral nutrition should be commenced using an intragastric tube [1, 2], whereas other guidelines advise that when small bowel feeding is feasible that this route is preferable [3].
The advantages of commencing with intragastric feeding include that naso- or oro-gastric tubes are relatively easy to insert, so that once a decision is made to feed, delivery of nutrient can promptly commence. However, disadvantages of the intragastric approach include delayed gastric emptying, which occurs frequently in the critically ill [4, 5], and predisposes to inadequate nutrient administration. Indeed, observational studies, in which most patients receive intragastric feeding, have shown that the proportion of calories and protein delivered to critically ill patients are about 50 to 70% of targeted calorie and protein loads [6–8].
Small intestinal feeding tubes are more difficult to insert, often requiring specific expertise and equipment. Their potential advantages include bypassing the stomach, which should theoretically 'guarantee' delivery of nutrients, as the major gastrointestinal motility disorders in the critically ill appear to occur in the antral-pyloro region of the stomach [9]. Not only does increasing administration of nutrients have the potential to reduce mortality and length of stay, particularly in those patients at risk of critical illness malnutrition and its consequences [10], but delivery of nutrients into the small intestine has been reported to reduce the incidence of hospital-acquired pneumonia, possibly because episodes of gastro-oesophageal regurgitation occur less frequently [11, 12]. Intuitively, a reduction in pneumonia should shorten intensive care unit (ICU) and hospital length of stay and may reduce mortality [13].
Systematic reviews and meta-analysis have been published that evaluated small bowel and gastric feeding in the critically ill [14–17]. An update incorporating important recent studies [18–20] was published by Jiyong and colleagues [17]. However, a limitation of the latter review is that the authors included a study in which patients received care on the general hospital ward rather than a critical care environment. In addition, Jiyong and colleagues included studies of both adult and paediatric subjects. Finally, data from the ENTERIC study were not included, and we believe that this study is the pivotal study in the area [21]. For these reasons we sought to update previous reviews to determine whether small bowel, when compared to intragastric delivery of nutrition, is associated with improved outcomes in the critically ill.
The objectives of this study were to determine the effects of small bowel and gastric tube delivery of liquid nutrients on hospital-acquired pneumonia, duration of mechanical ventilation, length of ICU and hospital stay, mortality and nutritional intake in adult critically ill patients.
Methods
The meta-analysis was performed in line with the recommendations from the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [22].
Study identification
We conducted a systematic review of the published literature to identify all relevant randomised clinical trials. Using text word or MeSH headings containing: "randomized"; "blind"; "clinical trial"; "nutrition"; "enteral"; "small bowel"; "gastric"; "nasojejunal"; "nasoduodenal"; and "nasogastric" computerised searches for relevant articles on MEDLINE, EMBASE, BIIOSIS, CINAHL electronic databases Cochrane Controlled Trials Register from 1990 to March 2013 were performed. Reference lists of review articles and original studies were hand searched and relevant articles extracted.
Study eligibility criteria
All primary studies were retrieved and reviewed. Primary studies were eligible for inclusion if they: (1) studied adult patients with critical illness; (2) compared small bowel (delivered into the jejunum or duodenum) to gastric delivery; (3) included clinically important outcomes, such as mortality, infectious complications (including hospital-acquired pneumonia), length of stay or major nutritional endpoints; and (4) were randomised clinical trials (RCTs).
We defined patients with critical illness as those who were cared for in a critical care environment. Utilizing a scoring system that has been previously reported [23], RCTs were rated for methodological quality. Using previously piloted forms [23], two reviewers independently, and in duplicate, then abstracted data from these studies. Agreement was reached by consensus. We attempted to contact the authors of included studies and requested further information not contained in published articles.
Data synthesis
The primary outcome was the incidence of ICU-acquired pneumonia. Secondary outcomes were duration of mechanical ventilation, duration of ICU stay, duration of hospital stay, mortality, and nutritional intake. We used definitions of ICU-acquired pneumonia as defined by the original study investigators.
To quantify nutritional intake we included only studies that reported the mean (SD) percentage of calories or volume delivered when compared to the patients' energy expenditure or prescribed volume as estimated by weight-based or complex calculation. Data from all studies were combined to estimate the common risk ratio (RR) and associated 95% confidence intervals (CI) for mortality and hospital-acquired pneumonia. In the meta-analysis, we used maximum likelihood methods of combining risk ratios across all trials and examined the data for evidence of heterogeneity within groups. The Mantel-Haenszel method was used to test the significance of treatment effect. We used a random effects model to estimate the overall relative risk. Heterogeneity was determined using the Chi squared test and interclass correlation I2. We also analysed the effect of small bowel delivery on duration of mechanical ventilation, ICU stay and hospital stay; the weighted mean difference (WMD) was used to describe the standardised difference between mean duration of stay from small bowel and intragastric delivery, respectively. P-values < 0.05 were considered significant.
Subgroup and sensitivity analyses
There were substantial limitations when interpreting data from two of the included studies. Taylor and colleagues reported the effect of 'enhanced' enteral nutrition, that ideally was administered via a small intestinal feeding tube [24]. However, only 34% of the patients actually achieved feeding via the small bowel, which is markedly inferior to rates of successful small intestinal tube placement reported by other groups [25]. Minard and colleagues compared patients who received early immune-enhanced enteral nutrition via the small bowel to those receiving delayed immune-enhanced enteral nutrition via the stomach [26]. Accordingly, when indicated, meta-analyses of outcome data were performed with, and without, these two studies.
It should also be recognised that the diagnosis of ICU-acquired pneumonia can be subjective. For this reason, when evaluating the effect of small intestinal feeding on the incidence of pneumonia we also report the subgroup of studies that used microbiological data in association with clinical data [27].
Results
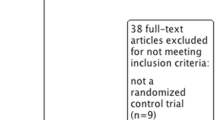
The literature search resulted in 22 RCTs. After reviewing these studies, four were excluded because they were systematic reviews [14–17], one had < 50% of enrolled patients admitted to an ICU [28], one did not report clinical outcomes [11] and one [29] was an analysis of data already included.
Studies
Results from these 15 level-2 RCTs were aggregated. None of the studies were able to blind treating health care providers to the route of delivery once patients were randomised, and only three studies included patients from more than one ICU (Kortbeek, n = 2; Montejo, n = 11; Davies, 2012, n = 17). Only two groups reported registration of their study [18, 21]. The characteristics of the studies are summarised in Table 1.
Placement of small intestinal feeding catheters
Various techniques were used to insert small intestinal tubes (Table 1).
Success - and time to successful placement - of small intestinal feeding tubes were not reported in all studies. When reported (n = 11), success rates varied between 34 and 100%, with the median time to placement ranging from 5 hours to 1.5 days (Table 1). Repeated testing to confirm that the feeding tube remained in either the stomach or small intestine throughout the patient's admission was not reported in any study.
Standardisation in the intragastrically-fed group
While the 'control' group in all studies was, at least initially, intragastric delivery, the use of gastrokinetic drugs was inconsistently reported (Table 1).
Outcomes
Pneumonia
Twelve studies reported the incidence of ICU-acquired pneumonia. The reported incidence of pneumonia ranged from 9% to 46% of patients studied. Pneumonia was diagnosed according to a variety of techniques (Table 1), with six studies incorporating microbiological and clinical data [20, 21, 30–33], four studies used clinical signs and radiological changes [18, 19, 34, 35] and two studies did not describe the technique used to make the diagnosis of pneumonia [24, 36]. In only four studies were the investigators blinded to treatment allocation when making the diagnosis of pneumonia [19, 21, 30, 31].
Small bowel feeding was associated with a reduced risk of ICU-acquired pneumonia when compared to gastric (relative risk (RR): small intestine vs. intragastric: 0.75 (0.60 to 0.93) P = 0.01; test for heterogeneity I2 = 11%; Figure 1A). The point estimate was unaffected when the studies by Taylor and Minard were removed (RR: 0.75 (0.56 to 1.00); P = 0.05; I2 = 21%). When analysing only studies that included microbiological diagnosis, these results remained similar (RR: 0.72 (0.55 to 0.93); P = 0.01; I2 = 0%; Figure 1B).
Length of stay
Nine studies reported on ICU length of stay. Although heterogeneity was present, length of stay appeared unaffected regardless of whether small intestine or intragastric tubes were used (weighted mean difference (WMD): 0.49 days (-1.36 to 2.33); P = 0.60; I2 = 81%; Figure 2A). Results were unchanged when the study by Minard was excluded (WMD: 0.04 days (-1.85 to 1.93); P = 0.97; I2 = 82%). Hospital length of stay was also unaffected by small bowel or intragastric administration of nutrients in the five studies that reported this outcome (WMD: 0.56 days (-3.60 to 4.73) P = 0.79; I2 = 24%; Figure 2B).
Small intestinal feeding and duration of ICU- and hospital admission and mechanical ventilation. (A) Nine studies reported the duration of admission into the Intensive Care Unit (ICU), (B) five studies reported hospital admission length-of-stay, and (C) six reported length of mechanical ventilation.
Duration of mechanical ventilation
Administration of nutrients directly into the small intestine did not appear to influence duration of mechanical ventilation (WMD: -0.36 (-2.02 to 1.30); P = 0.67; I2 = 42%; Figure 2C).
Mortality
Thirteen studies reported mortality data. Feeding via small intestinal or intragastric tube did not affect mortality (RR: 1.01 (95% CI: 0.83 to 1.24); P = 0.92; I2 = 0%; Figure 3). When the studies by Taylor and Minard were excluded, data were unchanged (RR: 1.03 (0.84 to 1.27); P = 0.78; I2 = 0%).
Nutritional administration
Targets for nutritional delivery were based on formulae (n = 7) or weight-based calculations (n = 4), with a few studies either not, or inadequately, reporting how the nutrition target was derived (n = 4) (Table 2). Only eight studies reported the number of days of enteral nutrition provided, which varied from less than 4 days to more than 11 days (Table 2).
Nine studies reported the amount of nutrients administered to patients (calories ± protein). Of these studies, one reported small intestinal feeding reduced the amount of nutrients administered [18], four reported that it increased nutrient delivery [19, 20, 30, 34] and four reported that energy and protein delivered was unaffected by route of feeding [32, 33, 37] (Table 2).
Data from six studies that reported nutritional intake as mean ± SD could be aggregated. In these studies there was slight variation in the description of nutrient intake: it was specified as percentage of daily caloric intake, percentage of estimated energy requirements received, and 'mean efficacious volume of diet'. When these data were grouped, small bowel feeding compared to gastric feeding was associated with a significantly greater percentage of nutritional intake (WMD 11% of intake/amount prescribed [5, 16]; P = 0.0004, I2 = 88%; Figure 4A). Data from studies that reported the time to reach nutritional goal rate were aggregated (n = 4), and there was no effect detected (WMD -3.4 hours (-13.5 to 6.6); P = 0.51; I2 = 87%; Figure 4B).
Discussion
We conducted a systematic review and meta-analysis of all RCTs of gastric vs. small bowel feeding in the ICU setting, including the recently published ENTERIC study [21]. The main observations are that delivery of nutrients directly into the small intestine may be associated with a reduction in the incidence of ICU-acquired pneumonia when compared to intragastric delivery, but despite this, days of ventilation, ICU and hospital length of stay and mortality appear unaffected. In addition, while there were relatively few, and substantial heterogeneity between, studies that evaluated nutritional efficiency, there was a signal that feeding into the small intestine increased nutrient intake.
It is possible that our meta-analysis over-estimated any reduction in pneumonia caused by small intestinal feeding. In several studies the diagnosis of pneumonia was made while investigators were aware of treatment allocation. Moreover, nearly all studies were conducted at a single ICU and the number of subjects was relatively small. Biases, including publication and selection biases, are well known to occur in studies involving fewer subjects, thereby affecting point estimates calculated in meta-analyses [38]. To limit bias we also analysed studies that used quantitative microbiological assessment. When this was performed, the interpretation remained similar supporting the original observation. Nevertheless, a reduction in pneumonia was not apparent in the largest cohort studied (ENTERIC). Given that discrepancies between meta-analyses and the 'truth' occur frequently [39, 40], circumspect interpretation of these aggregate data related to the incidence of pneumonia is recommended.
While we report a reduction in ICU-acquired pneumonia, the number of days of ventilation, length of ICU and hospital stay, as well as mortality, were unaffected by the route of feeding. While the lack of effect on the latter outcomes may reflect an inadequate sample size or, as described, that our meta-analysis overestimated the effect of route of feeding on the risk of pneumonia, there are plausible mechanisms that may explain these seemingly discrepant findings. In several of the studies artificial nutrition was administered for only a short period and so-called 'early-onset' ventilator-associated pneumonia is often caused by susceptible organisms and responds rapidly to antibiotic therapy [41]. Accordingly, attributed outcomes, such as length of ventilation and mortality, may actually be unaffected by 'early-onset' hospital-acquired pneumonia. Indeed, other factors, such as depth of sedation [42], may be greater determinants of length of ventilation and ICU stay than development of pneumonia.
There was a signal for increased nutritional intake when using small intestinal feeding tubes. There was, however, substantial statistical heterogeneity indicating that this observation should be interpreted with caution. The heterogeneity may reflect that placement of small intestinal tube can be technically difficult, requiring expertise and sophisticated methodologies [25]. Somewhat surprisingly, time-to-placement and placement success was not consistently reported. We suggest that the improvement in nutritional intake will only be generalisable to institutions that have the capacity to rapidly insert feeding tubes into the small intestine.
There were also inconsistencies between studies as to reporting concurrent gastrokinetic drug administration. This is likely to be important when trying to interpret the nutritional data, as gastrokinetic drugs can have potent effects on gastric emptying, but the response varies markedly between drug classes and regimens [4, 43, 44]. It should, therefore, be emphasised that data relating to nutritional intake do not extend to a comparison between small intestinal feeding and intragastric feeding with concurrent gastrokinetic drug administration.
While nutrient intake may have been 'improved', as discussed, mortality was unaffected. However, the optimal amount of calories and protein that should be administered to the critically ill is uncertain. Moreover, the benefits of nutrient administration may vary according to a number of factors specific to the individual patients. Those likely to benefit more from artificial nutrition compared to other ICU patients are those with a body mass index at either extreme [6], increased NUTRIC score [45], and anticipated prolonged length of stay in the ICU [10]. It should be emphasised that in some studies the period of nutrition required was relatively brief [18]. Hence, the power to detect any benefit from improved nutritional efficiency is markedly diminished [45]. It should also be noted that administration of more nutrient might have effects that are important to patients, but are not measured using data such as length of stay and mortality. Rice and colleagues reported that patients who received fewer calories were less likely to return to independent living on discharge [46]. Unfortunately, only one study reported longer-term function (neurological outcomes in this case) [24] and none measured muscle strength after ICU discharge. These functional outcomes may be very important to patients, and future studies of nutritional interventions would benefit from measuring such outcomes.
A further consideration is that the delivery of nutrients into the small intestine does not guarantee absorption, and it is absorption, rather than delivery of nutrients, which will improve patient outcomes, as undigested nutrients entering into the large intestine will lead to gas formation and abdominal distension, as well as diarrhoea [47]. Whether nutrients are administered proximal or distal to the pylorus does not, however, appear to affect absorption [48].
Although our search strategy was relatively comprehensive, and our methodology robust, there are several limitations to our findings. Statistical heterogeneity was modest and clinical heterogeneity was substantial. Some studies attempted to identify a cohort that was likely to have delayed gastric emptying [21], whereas others evaluated all patients requiring enteral nutrition at the beginning of their ICU stay [18]. There are no studies that include only patients with persistent feed-intolerance and/or those at the greatest risk of ICU-acquired pneumonia. This is important because while delayed gastric emptying occurs frequently in the critically ill [4, 5], the prevalence is probably no greater than 30% of all ICU patients that receive enteral nutrition. We suggest that patients with relatively 'normal' gastric emptying and oesophago-gastric motility are unlikely to benefit from small intestinal feeding. For this reason, we recommend against extrapolating this systematic review to patients with documented enteral feed-intolerance (as a marker of delayed gastric emptying) [49], particularly when feed-intolerance occurs during gastrokinetic drug use, and/or those at the greatest risk of ICU-acquired pneumonia - as these groups of patients may well benefit from small intestinal feeding.
Future studies should therefore target patients who develop feed-intolerance while receiving gastrokinetic drugs. In particular, targeting patients who are most likely to benefit from augmented nutritional delivery and who will require nutritional support for a substantial period of time will be a priority. In addition, these studies would also benefit from using a technique that affords rapidly and repeatedly successful placement of small intestinal feeding tubes as well as measuring longer-term functional outcomes.
Conclusions
Small bowel feeding may be associated with a reduction in ICU-acquired pneumonia and increases in nutrient delivery, but days of ventilation, ICU and hospital stay, and mortality were unaffected. Until further data are available, decisions as to whether to preferentially feed patients into the small intestine will need to be at an institutional level, incorporating the feasibility, safety and delays in obtaining access, while identifying patients most likely to benefit from this route of feeding.
Key messages
-
In the critically ill, small intestinal feeding when compared to intragastric may reduce the incidence of ICU-acquired pneumonia.
-
In the critically ill, small intestinal feeding when compared to intragastric may increase nutritional intake.
-
The route of enteral nutrient administration (intragastric or small intestinal) does not appear to be a major determinant of mortality or length of stay in unselected critically ill patients.
Abbreviations
- CI:
-
Confidence interval
- ICU:
-
Intensive care Unit
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RCT:
-
Randomised control trial
- RR:
-
Relative risk
- SD:
-
Standard deviation
- WMD:
-
Weighted mean difference.
References
Martindale RG, McClave SA, Vanek VW, McCarthy M, Roberts P, Taylor B, Ochoa JB, Napolitano L, Cresci G: Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of Critical Care Medicine and American Society for Parenteral and Enteral Nutrition: Executive Summary. Crit Care Med. 2009, 37: 1757-1761. 10.1097/CCM.0b013e3181a40116.
Kreymann KG, Berger MM, Deutz NE, Hiesmayr M, Jolliet P, Kazandjiev G, Nitenberg G, van den Berghe G, Wernerman J, Ebner C, Heymann C, Spies C: ESPEN Guidelines on Enteral Nutrition: Intensive care. Clin Nutr. 2006, 25: 210-223. 10.1016/j.clnu.2006.01.021.
Heyland DK, Dhaliwal R, Drover JW, Gramlich L, Dodek P: Canadian clinical practice guidelines for nutrition support in mechanically ventilated, critically ill adult patients. JPEN J Parenter Enteral Nutr. 2003, 27: 355-373. 10.1177/0148607103027005355.
Spapen HD, Duinslaeger L, Diltoer M, Gillet R, Bossuyt A, Huyghens LP: Gastric emptying in critically ill patients is accelerated by adding cisapride to a standard enteral feeding protocol: results of a prospective controlled trial. Crit Care Med. 1995, 23: 481-485. 10.1097/00003246-199503000-00011.
Chapman MJ, Fraser RJ, Matthews G, Russo A, Bellon M, Besanko LK, Jones KL, Butler R, Chatterton B, Horowitz M: Glucose absorption and gastric emptying in critical illness. Crit Care. 2009, 13: R140-10.1186/cc8021.
Alberda C, Gramlich L, Jones N, Jeejeebhoy K, Day AG, Dhaliwal R, Heyland DK: The relationship between nutritional intake and clinical outcomes in critically ill patients: results of an international multicenter observational study. Intensive Care Med. 2009, 35: 1728-1737. 10.1007/s00134-009-1567-4.
Hiesmayr M, Schindler K, Pernicka E, Schuh C, Schoeniger-Hekele A, Bauer P, Laviano A, Lovell AD, Mouhieddine M, Schuetz T, Schneider SM, Singer P, Pichard C, Howard P, Jonkers C, Grecu I, Ljunggvist O, NutritionDay Audit Team: Decreased food intake is a risk factor for mortality in hospitalised patients: the NutritionDay survey 2006. Clin Nutr. 2009, 28: 484-491. 10.1016/j.clnu.2009.05.013.
Allingstrup MJ, Esmailzadeh N, Wilkens Knudsen A, Espersen K, Hartvig Jensen T, Wiis J, Perner A, Kondrup J: Provision of protein and energy in relation to measured requirements in intensive care patients. Clin Nutr. 2012, 31: 462-468. 10.1016/j.clnu.2011.12.006.
Deane A, Chapman MJ, Fraser RJ, Bryant LK, Burgstad C, Nguyen NQ: Mechanisms underlying feed intolerance in the critically ill: implications for treatment. World J Gastroenterol. 2007, 13: 3909-3917.
Heyland DK, Cahill N, Day AG: Optimal amount of calories for critically ill patients: depends on how you slice the cake!. Crit Care Med. 2011, 39: 2619-2626.
Heyland DK, Drover JW, MacDonald S, Novak F, Lam M: Effect of postpyloric feeding on gastroesophageal regurgitation and pulmonary microaspiration: results of a randomized controlled trial. Crit Care Med. 2001, 29: 1495-1501. 10.1097/00003246-200108000-00001.
Metheny NA, Stewart BJ, McClave SA: Relationship between feeding tube site and respiratory outcomes. JPEN J Parenter Enteral Nutr. 2011, 35: 346-355. 10.1177/0148607110377096.
Metheny NA, Clouse RE, Chang YH, Stewart BJ, Oliver DA, Kollef MH: Tracheobronchial aspiration of gastric contents in critically ill tube-fed patients: frequency, outcomes, and risk factors. Crit Care Med. 2006, 34: 1007-1015. 10.1097/01.CCM.0000206106.65220.59.
Heyland DK, Drover JW, Dhaliwal R, Greenwood J: Optimizing the benefits and minimizing the risks of enteral nutrition in the critically ill: role of small bowel feeding. JPEN J Parenter Enteral Nutr. 2002, 26 (6 Suppl): S51-55. 10.1177/014860710202600608. discussion S56-57
Marik PE, Zaloga GP: Gastric versus post-pyloric feeding: a systematic review. Crit Care. 2003, 7: R46-51. 10.1186/cc2190.
Ho KM, Dobb GJ, Webb SA: A comparison of early gastric and post-pyloric feeding in critically ill patients: a meta-analysis. Intensive Care Med. 2006, 32: 639-649. 10.1007/s00134-006-0128-3.
Jiyong J, Tiancha H, Huiqin W, Jingfen J: Effect of gastric versus post-pyloric feeding on the incidence of pneumonia in critically ill patients: observations from traditional and Bayesian random-effects meta-analysis. Clin Nutr. 2013, 32: 8-15. 10.1016/j.clnu.2012.07.002.
White H, Sosnowski K, Tran K, Reeves A, Jones M: A randomised controlled comparison of early post-pyloric versus early gastric feeding to meet nutritional targets in ventilated intensive care patients. Crit Care. 2009, 13: R187-10.1186/cc8181.
Hsu CW, Sun SF, Lin SL, Kang SP, Chu KA, Lin CH, Huang HH: Duodenal versus gastric feeding in medical intensive care unit patients: a prospective, randomized, clinical study. Crit Care Med. 2009, 37: 1866-1872. 10.1097/CCM.0b013e31819ffcda.
Acosta-Escribano J, Fernandez-Vivas M, Grau Carmona T, Caturla-Such J, Garcia-Martinez M, Menendez-Mainer A, Solera-Suarez M, Sanchez-Paya J: Gastric versus transpyloric feeding in severe traumatic brain injury: a prospective, randomized trial. Intensive Care Med. 2010, 36: 1532-1539. 10.1007/s00134-010-1908-3.
Davies AR, Morrison SS, Bailey MJ, Bellomo R, Cooper DJ, Doig GS, Finfer SR, Heyland DK: A multicenter, randomized controlled trial comparing early nasojejunal with nasogastric nutrition in critical illness. Crit Care Med. 2012, 40: 2342-2348. 10.1097/CCM.0b013e318255d87e.
Moher D, Liberati A, Tetzlaff J, Altman DG: Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009, 6: e1000097-10.1371/journal.pmed.1000097.
Heyland DK, MacDonald S, Keefe L, Drover JW: Total parenteral nutrition in the critically ill patient: a meta-analysis. JAMA. 1998, 280: 2013-2019. 10.1001/jama.280.23.2013.
Taylor SJ, Fettes SB, Jewkes C, Nelson RJ: Prospective, randomized, controlled trial to determine the effect of early enhanced enteral nutrition on clinical outcome in mechanically ventilated patients suffering head injury. Crit Care Med. 1999, 27: 2525-2531. 10.1097/00003246-199911000-00033.
Deane AM, Fraser RJ, Young RJ, Foreman B, O'Conner SN, Chapman MJ: Evaluation of a bedside technique for postpyloric placement of feeding catheters. Crit Care Resusc. 2009, 11: 180-183.
Minard G, Kudsk KA, Melton S, Patton JH, Tolley EA: Early versus delayed feeding with an immune-enhancing diet in patients with severe head injuries. JPEN J Parenter Enteral Nutr. 2000, 24: 145-149. 10.1177/0148607100024003145.
Lisboa T, Rello J: Diagnosis of ventilator-associated pneumonia: is there a gold standard and a simple approach?. Curr Opin Infect Dis. 2008, 21: 174-178. 10.1097/QCO.0b013e3282f55dd1.
Eatock FC, Chong P, Menezes N, Murray L, McKay CJ, Carter CR, Imrie CW: A randomized study of early nasogastric versus nasojejunal feeding in severe acute pancreatitis. Am J Gastroenterol. 2005, 100: 432-439. 10.1111/j.1572-0241.2005.40587.x.
Huang HH, Chang SJ, Hsu CW, Chang TM, Kang SP, Liu MY: Severity of illness influences the efficacy of enteral feeding route on clinical outcomes in patients with critical illness. J Acad Nutr Diet. 2012, 112: 1138-1146. 10.1016/j.jand.2012.04.013.
Montecalvo MA, Steger KA, Farber HW, Smith BF, Dennis RC, Fitzpatrick GF, Pollack SD, Korsberg TZ, Birkett DH, Hirsch EF, Craven DE: Nutritional outcome and pneumonia in critical care patients randomized to gastric versus jejunal tube feedings. The Critical Care Research Team. Crit Care Med. 1992, 20: 1377-1387. 10.1097/00003246-199210000-00004.
Kortbeek JB, Haigh PI, Doig C: Duodenal versus gastric feeding in ventilated blunt trauma patients: a randomized controlled trial. J Trauma. 1999, 46: 992-996. 10.1097/00005373-199906000-00002. discussion 996-998
Davies AR, Froomes PR, French CJ, Bellomo R, Gutteridge GA, Nyulasi I, Walker R, Sewell RB: Randomized comparison of nasojejunal and nasogastric feeding in critically ill patients. Crit Care Med. 2002, 30: 586-590. 10.1097/00003246-200203000-00016.
Montejo JC, Grau T, Acosta J, Ruiz-Santana S, Planas M, García-De-Lorenzo A, Mesejo A, Cervera M, Sánchez-Alvarez C, Núñez-Ruiz R, López-Martínez J, Nutritional and Metabolic Working Group of the Spanish Society of Intensive Care Medicine and Coronary Units: Multicenter, prospective, randomized, single-blind study comparing the efficacy and gastrointestinal complications of early jejunal feeding with early gastric feeding in critically ill patients. Crit Care Med. 2002, 30: 796-800. 10.1097/00003246-200204000-00013.
Kearns PJ, Chin D, Mueller L, Wallace K, Jensen WA, Kirsch CM: The incidence of ventilator-associated pneumonia and success in nutrient delivery with gastric versus small intestinal feeding: a randomized clinical trial. Crit Care Med. 2000, 28: 1742-1746. 10.1097/00003246-200006000-00007.
Minard G, Kudsk KA: Effect of route of feeding on the incidence of septic complications in critically ill patients. Semin Respir Infect. 1994, 9: 228-231.
Day L, Stotts NA, Frankfurt A, Stralovich-Romani A, Volz M, Muwaswes M, Fukuoka Y, O'Leary-Kelley C: Gastric versus duodenal feeding in patients with neurological disease: a pilot study. J Neurosci Nurs. 2001, 33: 148-149. 10.1097/01376517-200106000-00007. 155-159
Esparza J, Boivin MA, Hartshorne MF, Levy H: Equal aspiration rates in gastrically and transpylorically fed critically ill patients. Intensive Care Med. 2001, 27: 660-664. 10.1007/s001340100880.
Sterne JA, Gavaghan D, Egger M: Publication and related bias in meta-analysis: power of statistical tests and prevalence in the literature. J Clin Epidemiol. 2000, 53: 1119-1129. 10.1016/S0895-4356(00)00242-0.
Cook DJ, Guyatt GH, Laupacis A, Sackett DL, Goldberg RJ: Clinical recommendations using levels of evidence for antithrombotic agents. Chest. 1995, 108 (4 Suppl): 227S-230S.
LeLorier J, Gregoire G, Benhaddad A, Lapierre J, Derderian F: Discrepancies between meta-analyses and subsequent large randomized, controlled trials. N Engl J Med. 1997, 337: 536-542. 10.1056/NEJM199708213370806.
Valles J, Pobo A, Garcia-Esquirol O, Mariscal D, Real J, Fernandez R: Excess ICU mortality attributable to ventilator-associated pneumonia: the role of early vs late onset. Intensive Care Med. 2007, 33: 1363-1368. 10.1007/s00134-007-0721-0.
Kress JP, Pohlman AS, O'Connor MF, Hall JB: Daily interruption of sedative infusions in critically ill patients undergoing mechanical ventilation. N Engl J Med. 2000, 342: 1471-1477. 10.1056/NEJM200005183422002.
Nguyen NQ, Chapman MJ, Fraser RJ, Bryant LK, Holloway RH: Erythromycin is more effective than metoclopramide in the treatment of feed intolerance in critical illness. Crit Care Med. 2007, 35: 483-489. 10.1097/01.CCM.0000253410.36492.E9.
MacLaren R, Kiser TH, Fish DN, Wischmeyer PE: Erythromycin vs metoclopramide for facilitating gastric emptying and tolerance to intragastric nutrition in critically ill patients. JPEN J Parenter Enteral Nutr. 2008, 32: 412-419. 10.1177/0148607108319803.
Heyland DK, Dhaliwal R, Jiang X, Day AG: Identifying critically ill patients who benefit the most from nutrition therapy: the development and initial validation of a novel risk assessment tool. Crit Care. 2011, 15: R268-10.1186/cc10546.
Rice TW, Mogan S, Hays MA, Bernard GR, Jensen GL, Wheeler AP: Randomized trial of initial trophic versus full-energy enteral nutrition in mechanically ventilated patients with acute respiratory failure. Crit Care Med. 2011, 39: 967-974. 10.1097/CCM.0b013e31820a905a.
Deane AM, Wong GL, Horowitz M, Zaknic AV, Summers MJ, Di Bartolomeo AE, Sim JA, Maddox AF, Bellon MS, Rayner CK, Chapman MJ, Fraser RJ: Randomized double-blind crossover study to determine the effects of erythromycin on small intestinal nutrient absorption and transit in the critically ill. Am J Clin Nutr. 2012, 95: 1396-1402. 10.3945/ajcn.112.035691.
Di Bartolomeo AE, Chapman MJ, VZaknic A, Summers MJ, Jones KL, Nguyen NQ, Rayner CK, Horowitz M, Deane AM: Comparative effects on glucose absorption of intragastric and post-pyloric nutrient delivery in the critically ill. Crit Care. 2012, 16: R167-10.1186/cc11522.
Chapman MJ, Besanko LK, Burgstad CM, Fraser RJ, Bellon M, O'Connor S, Russo A, Jones KL, Lange K, Nguyen NQ, Bartholomeusz F, Chatterton B, Horowitz M: Gastric emptying of a liquid nutrient meal in the critically ill: relationship between scintigraphic and carbon breath test measurement. Gut. 2011, 60: 1336-1343. 10.1136/gut.2010.227934.
Acknowledgements
Prof Daren Heyland was awarded the 2012 Royal Adelaide Hospital Nimmo Professorship. The Nimmo Professorship facilitated collaboration required for this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
AD contributed to acquisition, analysis and interpretation of data, and was responsible for drafting, editing and submission of the manuscript. RD contributed to study conception and design. She was responsible for acquisition, analysis and interpretation of data and contributed to revision of the manuscript for important intellectual content. ADay contributed to study conception and design, as well as acquisition, analysis and interpretation of data. ER contributed to study conception and design, as well as acquisition, analysis and interpretation of data. ADavies contributed to study conception and design, acquisition, analysis and interpretation of data, and revision of the manuscript for important intellectual content. DH was responsible for conception and design, acquisition, and revising the manuscript for important intellectual content. All authors have read and approved the final manuscript.
An erratum to this article is available at http://dx.doi.org/10.1186/cc13961.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Deane Adam, M., Rupinder, D., Day Andrew, G. et al. Comparisons between intragastric and small intestinal delivery of enteral nutrition in the critically ill: a systematic review and meta-analysis. Crit Care 17, R125 (2013). https://doi.org/10.1186/cc12800
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/cc12800