Abstract
Purpose
To evaluate the efficacy of transpyloric feeding (TPF) compared with gastric feeding (GF) with regard to the incidence of ventilator-associated pneumonia in severe traumatic brain injury patients (TBI).
Design and setting
Prospective, open-label, randomized study in an intensive care unit of a university hospital.
Patients
One hundred and four CHI adult patients admitted for TBI between April 2007 and December 2008. Patients were included within the first 24 h after ICU admission and were followed until discharge or 30 days after admission.
Intervention
Patients were randomized to TPF or GF groups. They received the same diet, with 25 kcal kg−1 day−1 of calculated energy requirements and a nitrogen intake of 0.2 g N kg−1 day−1. Primary outcome was the incidence of early and ventilatory-associated pneumonia. Secondary outcomes were enteral nutrition-related gastrointestinal complications (GIC), days on mechanical ventilation, length of ICU stay and hospital stay, and sequential organ failure assessment score (SOFA).
Results
The TPF group had a lower incidence of pneumonia, OR 0.3 (95% CI 0.1–0.7, P = 0.01). There were no significant differences in other nosocomial infections. The TPF group received higher amounts of diet compared to the GF group (92 vs. 84%, P < 0.01) and had lesser incidence of increased gastric residuals, OR 0.2 (95% CI 0.04–0.6, P = 0.003).
Conclusions
Enteral nutrition delivered through the transpyloric route reduces the incidence of overall and late pneumonia and improves nutritional efficacy in severe TBI patients.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Patients with severe traumatic brain injury (TBI) show an increased energy consumption and protein catabolism [1, 2] leading to a decreased immune response and higher incidence of nosocomial infections [3]. TBI patients fed early seem to have better outcomes in terms of survival and disability [4]. The enteral route is preferred due to its secretagogue and immunologic effects on the intestinal function and a decreased rate of nosocomial infections, particularly pneumonia episodes [5, 6]. Feeding tolerance must be continually assessed, particularly when poor gastric motility is suspected and there is an increased risk of gastroesophageal reflux. In fact, increased gastric residuals are the most frequent gastrointestinal complication of enteral nutrition with an incidence rate between 40 and 60% [7]. Usually, increased gastric residuals are checked periodically and a volume higher than 200 mL is considered for temporary discontinuation of the diet, but a recent study has demonstrated that 500 mL is a safer limit without significant changes in the incidence of nosocomial pneumonia [8].
Postpyloric feeding has theoretical advantages because it could reduce the risk of gastroesophageal reflux and the risk of aspiration pneumonia. ESPEN guidelines do not recommend the use of the transpyloric approach as a first choice [9]. Nevertheless, patients with severe TBI have an increased incidence of gastrointestinal complications (GIC), particularly increased gastric residuals (GR), due to brain trauma itself, the therapeutics used to control intracreaneal hypertension and measures of patient support. The final result is a significant decrease in nutritional intake, and the occurrence of regurgitation and bronchoaspiration episodes [10]. Transpyloric-administered enteral nutrition preserves gastrointestinal function, can normalize caloric intake, and reduces the incidence of bronchoaspiration episodes [11].
The aim of this study was to evaluate the nutritional efficacy of transpyloric route feeding and the incidence of overall pneumonia and late or ventilator-associated pneumonia in TBI patients, compared with the gastric route.
Materials and methods
Study design
This controlled, randomized, open trial was performed in the Intensive Care Unit of the University General Hospital of Alicante (Spain), a referral center for severe TBI patients. The study was approved by the ethics committee according to Spanish laws. All patients or their closest relative gave written informed consent.
Patients
Adult patients with severe TBI were eligible if they met the following inclusion criteria: age between 18 and 80 years; Glasgow coma scale (GCS) <9, Apache II between 15 and 30, sequential organ failure assessment (SOFA) index <6 (excluding the neurological variable), mechanical ventilation required on admission, and artificial nutrition required for at least 5 days. Exclusion criteria were chronic renal failure (plasma creatinin >2 mg/dL), hepatic failure (bilirubin >3 mg/dL), contraindication for enteral nutrition (intestinal inflammatory disease, past history of gastric resection, or abdominal surgery within the 2 months previous to inclusion, facial trauma), treatment with steroids or immunosuppressive drugs, traumatic spinal cord injury, pregnancy, body mass index (BMI) >35 kg/m2, severe malnutrition with BMI <18 kg/m2, life expectancy less than 5 days or encephalic death on admission, refusal to participate, or participation in another clinical study.
Patient’s status was assessed daily with the SOFA score [12] and the SOFA-corrected score (SOFAc), excluding the neurological score. The level of coma was assessed with the GCS. Trauma severity was assessed with the injury severity score [13]. Other severity variables included time to clinical stabilization, defined as the time needed to achieve optimal values in the following clinical variables: mean blood pressure >90 mm/Hg, heart rate <120 beats/min, capillary oxygen saturation >95%, arterial pH > 7.30, Hb > 8 g/dL, lactic acid <1.5 mMol/L, with or without vasoactive medication; length of treatment with vasoactive drugs; and administered volume of hemoderivates within the first 24 h. Intracranial hypertension (ICH) was defined as a pressure higher than 20 mmHg once general therapeutic measures had been optimized [14]. The length of mechanical ventilation, length of ICU and hospital stay, incidence of neurological sequel level [15], and mortality at 30 days were also recorded. Baseline data included total C-reactive protein (CRP), cholesterol, prealbumin, and albumin, measured using nephelometry techniques [16].
Intervention
After patient’s clinical stabilization, a 12 French tube was placed for gastric feeding (GF) group patients, and a double-lumen tube (Compat Stay-Put 9/18) was placed for transpyloric feeding (TPF) group patients in the jejunum, through spontaneous placement or in the radiology suite, within the first 24 h using a trans-nasal or a trans-oral approach. Basilar skull fractures were ruled out using cranial CT scans. An abdominal plain film was made before diet administration to confirm adequate enteral tube placement. Investigators were encouraged to maintain the patients in a semi-recumbent position (between 30° and 45°). Enteral nutrition was administered continuously with a 24 h infusion pump. All patients received the same diet (Isosource Protein, Nestle, Spain). Energy intake was set at 25 kcal kg−1 day−1, and nitrogen intake was 0.2 g N kg−1 day−1. Nutritional goal was to achieve a caloric intake equal to 50% of the calculated requirements on the first day, and full requirements on the second day. Gastric residuals were checked every 6 h the first day and every 12 h on subsequent days. Increased GR was defined when more than 200 mL were recovered from the NG tube. If GR met these criteria, enteral nutrition was discontinued for 6 h and restarted at the same previous rate. GF patients with two consecutive episodes of increased GR volumes received metoclopramide, 30 mg/day for 3 days. Insulin administration was started if the blood glucose level exceeded 150 mg/dL in two consecutive determinations according to a previously established protocol.
All patients get intracranial pressure monitoring [17]. Patients were sedated with midazolam at 0.3–0.5 mg kg−1 h−1 IV, until a level of 30 was achieved by bi-spectral analysis (BIS). Patients received 2 mg/h IV of morphine for analgesia. Muscle relaxants were used as the first measure to control intracranial hypertension.
Study outcomes
The primary outcome was the incidence of nosocomial pneumonia throughout the stay in ICU. Pneumonia was assessed using the CPIS criteria [18], with a score higher than 6 indicating pneumonia. Early pneumonia was defined as cases that developed within the first 48 h after admission, and late or mechanical ventilation-related (VAP) cases were those that appeared more than 48 h after admission [19]. All other episodes of hospital-acquired infection that occurred throughout the study period were also recorded, following the CDC criteria [20, 21]. Secondary outcomes were enteral feeding gastrointestinal complications, recorded prospectively, and defined as follows (a) abdominal distention: abdominal changes at physical exam with timpanism or/and the absence of bowel sounds, (b) increased gastric residual volume: gastric residuals were considered high when the recovered volume was higher than 200 mL, (c) vomiting: enteral formula ejected through the mouth, (d) diarrhea: at least five liquid stools in a 24 h period or an estimated volume of at least 2,000 mL/day, (e) aspiration: diet presence in the airway or respiratory tract (with or without exteriorization). Mean efficacious volume (mean volume of diet administered daily) and reasons for enteral feeding withdrawal were also recorded [22].
Data management and statistical analysis
After inclusion and exclusion criteria were verified, and informed consent was obtained, patients were randomized in a 1:1 ratio to one of two treatment groups. Study power was set at 80% in order to detect a difference between the two types of enteral routes of at least 25% in absolute terms or a risk reduction of 0.3 for the development of nosocomial pneumonia during stay in the ICU with an alpha error of 5%. That gives a sample size of 104, 52 for each group with continuity correction. We did an intention-to-treat analysis and not an analysis based on the treatment administered, to avoid the misleading effect of failures of the TPG that were nourished by the gastric route. Continuous data were assessed for normality, two-tailed Student’s t test was performed for normal data, and the Mann-Whitney U test for non-normal distributions, with a 95% confidence interval, and a < 0.05 significance level. Two-tailed chi-squared test with Fisher test correction was applied for proportions. Odds ratio with 95% confidence interval was calculated for the incidence of nosocomial infections and gastrointestinal complications.
Results
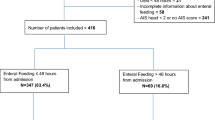
From April 2007 to January 2009, 264 patients with severe TBI were admitted and consecutively assessed for inclusion. Of these, 160 patients did not meet the inclusion criteria, and the remaining 104 patients were randomized. Fifty patients were assigned to the TPF group and 54 to the GF group. Four patients died within the first 5 days of study, two in the TPF group and two in the GF group. Three patients assigned to the TPF group were subsequently reassigned to the GF group, due to unsuccessful transpyloric tube placement (Fig. 1). Baseline demographic data were similar between groups and only the time to clinical stabilization was 2 h longer in the GF group, achieving statistical significance (P < 0.05). Nutritional parameters were similar in both groups (Table 1).
Infectious complications
Forty-seven patients (45%) had pneumonia, 16 (32%) in the TPF group and 31 (57%) in the GF group with an OR of 0.3 (95% CI 0.1–0.7; P < 0.01). Early pneumonia was present in nine patients, five (10%) in the TPF group, and four (7%) in the GF group, without significant differences between the two groups. Thirty-eight patients (36%) had late pneumonia, 11 of them (24%) in the TPF group and 27 of them (48%) in the GF group, with OR 0.2 (95% CI; 0.1–0.9; P = 0.02). Mean time to the occurrence of late pneumonia was 5 ± 2 days. No differences between groups were observed in the incidence of other infections (Table 2). Isolates from patients with pneumonia are shown in Table 3.
Nutritional efficacy
Mean efficacious volume of diet was significantly higher in the TPF group (92 ± 7 vs. 84 ± 15%, P < 0.01). Seven patients (14%) had GIC in the TF group, and 27 patients (50%) in the GF group (OR: 0.2, 95% CI 0.06–0.4; P = 0.001). Only 3 patients (7%) of the TPF group had increased gastric residuals and 15 (28%) in the GF group (OR 0.2, 95% CI 0.04–0.6; P = 0.003). Enteral feeding was withdrawn in 3 patients (7%) in the TPF group and in 10 patients (18%) in the GF group, without significant differences. The incidence of other gastrointestinal complications was similar in both groups (Table 4).
Prognostic variables
On day 5, the SOFAc was significantly higher in the GN group (1.5 ± 1.5 vs. 2 ± 2, P < 0.05), due to respiratory and hemodynamic variables. We found no significant differences in the length of ICU stay, hospital stay, or length of mechanical ventilation. The incidence of ICH was similar in both groups. Of the 104 included patients, 4 patients died within the first 5 days and 15 patients died within the first 30 days (Table 5).
Discussion
Our study shows that the early use of postpyloric feeding instead of gastric feeding in patients with severe traumatic brain injury is associated with a decrease in the incidence of ventilator-associated pneumonia with a low rate of gastrointestinal complications and postpyloric tube malfunction. The two groups of patients were well matched in terms of injury severity, prognostic scores, and nutritional parameters. We use a transpyloric approach with gastric decompression to overcome the risk of bronchoaspiration of large volumes of gastric residuals. Also, prokinetics were used in both groups when gastric residuals were elevated. After clinical stabilization, patients received early enteral nutrition with strict control of blood glucose levels and GIC [23, 24].
Postpyloric feeding in critically ill patients has theoretical advantages because impaired gastric emptying is relatively frequent. Compared with gastric feeding, it may reduce the risks associated with high gastric residuals such as aspiration pneumonia [22]. Several studies and meta-analyses have compared these issues in critically ill patients. Based on a lower incidence of pulmonary aspiration, the American Chest Society Consensus Document recommended the use of TPF [25]. However, two consecutive studies conducted in critically ill patients evaluated the protective effect of TPF versus GF in the incidence of pneumonia and showed no significant differences between them [26, 27]. Three consecutive meta-analyses gave different results [6, 28, 29]. Only one of them showed significant differences in the incidence of pneumonia and concluded that the use of TPF should be reserved for patients with repeated CIG episodes, in particular in case of increased GR [28]. Nevertheless, the number of patients with TBI or neurological impairment included was limited. Only one of two studies that addressed this question in TBI patients showed an increased incidence of GIC, in particular increased GR; the other two meta-analyses that compared the two methods for EN administration did not reach a conclusive result [30, 31].
These contradictory findings are explained when looking at the incidence of tube feeding-related gastrointestinal complications. The incidence of GIC in critical patients ranges from 45 to 60% within the first days after injury, matching the period of maximum seriousness and the use of vital support measures [32, 33]. Abnormalities in the gastrointestinal transit may be observed in TBI patients, including decreased peristalsis or a reduction of the antral contraction [34]. This effect can be occasional or persistent during the first days after injury or can match acute episodes of ICH. In fact, patients with increased ICH have as much as an 80% increase in the incidence of gastric residuals [7]. Another study has shown greater incidence rates of GIC in ICH patients, mainly within the first 2 weeks or following barbiturate administration, despite the use of prokinetic drugs [35]. Our group has analyzed gastric emptying in TBI patients using the acetaminophen test, and lower plasma levels of acetaminophen were observed among those patients with intracranial hypertension. This factor was associated with a greater incidence rate of GIC (40%), significantly increased gastric residuals, and higher occurrence of pneumonia [36, 37].
The causality among increased gastric residuals, high rates of aspiration, and the development of pneumonia remains unclear. Nevertheless, several measures are recommended assuming this connection: backrest elevation up to 45°, administration of motility agents, and monitoring gastric residual volume [6, 38]. The general practice is to hold feedings for gastric residual volumes between 200 and 500 mL, but this amount is not standardized, and there are no studies to date that can predict an actual “safe” amount for gastric residual volume. In our study, early administration of TPF was associated with a decrease in high gastric residuals. Our results differ from previous study results, in which mean efficacious volume decreases and GIC increases have been described [30, 39]. Nevertheless, a more detailed analysis of our study shows a 48.1% incidence rate of GIC in the GF group, similar to those described. GF patients with good tolerability and no GIC complications within the first 3 days maintained adequate volumes of feeding throughout the study. On the contrary, some of the GF group patients experienced multiple episodes of increased GR, none of which resulted in EN withdrawal. These episodes did not appear to be related to GCS score or to ICH episodes, which were not significantly different. We only used metoclopramide when high gastric residuals were detected and not to prevent them, because it has no advantage there [40]. Our results showed that postpyloric feeding was not associated with other gastrointestinal complications such as diarrhea, and the procedure of inserting the tube was very safe. Tube placement was impossible only in three patients, and there was no delay in the time or amount of enteral nutrition delivery.
There were no significant differences between groups in secondary outcomes. The between-groups difference in SOFA scores should be attributed to a worsening of the respiratory variable in the GF group due to a higher incidence of pneumonia in this group. The greater length of the vasoactive medication period in the GF group was not related to a worsening of the hemodynamic condition but to the need for maintaining an appropriate brain perfusion, as a result of the slightly higher incidence of intracranial hypertension. Moreover, respiratory and hemodynamic variables most influenced SOFA scores throughout the study.
We may conclude that TBI patients fed early through a transpyloric tube and treated with a set of measures to reduce the incidence of bronchoaspiration, including strict control of the head position, early use of prokinetic drugs, and strict application of feeding guidelines, particularly for GR, had lesser incidence of late pneumonia with a significant probability that this was due to a lesser incidence of GIC, particularly increased gastric residuals.
Abbreviations
- BMI:
-
Body mass index
- CIPS:
-
Clinical infection pulmonary score
- GCS:
-
Glasgow coma score
- GIC:
-
Enteral nutrition-related gastrointestinal complications
- ICH:
-
Intracranial hypertension
- SOFA:
-
Sequential organ failure assessment
References
Chandra RK (1983) Nutrition, immunity and infection: present knowledge and future directions. Lancet 1:688–691
Dempsey DT, Mullen JL, Buzby GP (1988) The link between nutritional status and clinical outcome: can nutritional intervention modify it? Am J Clin Nutr 47:351–356
Apelgren K, Rombeau J, Twomey P, Miller R (1982) Comparison of nutritional indices and outcome in critically ill patients. Crit Care Med 10:305–3077
Perel P, Yanagawa T, Bunn F, Roberts I, Wentz R, Pierro A (2006) Nutritional support for head-injured patients. Cochrane Database Syst Rev 4:CD001530
Braunschweig C, Levy P, Sheean PM, Wang X (2001) Enteral compared with parenteral nutrition: a meta-analysis. Am J Clin Nutr 74:534–542
Marik PE, Zaloga GP (2003) Gastric versus post-pyloric feeding: a systematic review. Crit Care 7:R46–R51
Nguyen NQ, Chapman MJ, Fraser RJ, Bryant LK, Burgstad C, Ching K, Bellon M, Holloway RH (2008) The effects of sedation on gastric emptying and intra-gastric meal distribution in critical illness. Intensive Care Med 34:454–460
Montejo-Gonzalez JC, Minambres E, Bordeje ML, Mesejo A, Acosta J, Heras A et al (2008) Gastric residual volume during enteral nutrition in ICU patients. The REGANE study. Preliminary results. Intensive Care Med. doi:10.1007/s00134-010-1856-y
Kreymann KG, Berger MM, Deutz NE, Hiesmayrd M, Jolliete P, Kazandjiev G, Nitenberg G, van den Berghe G, Wernerman J, Ebner C, Hartl W, Heymann C, Spies C (2006) ESPEN guidelines on enteral nutrition: intensive care. Clin Nutr 25:210–223
Heyland DK, Drover JW, Macdonald S, Novak F, Lam M (2001) Effect of postpyloric feeding on gastroesophageal regurgitation and pulmonary microaspiration: results of a randomized trial. Crit Care Med 29:1495–1501
Montejo JC, Grau T, Acosta J, Ruiz-Santana S, Planas M, García-De-Lorenzo A, Mesejo A, Cervera M, Sánchez-Alvarez C, Núñez-Ruiz R, López-Martínez J, Nutritional and Metabolic Working Group of the Spanish Society of Intensive Care Medicine and Coronary Units (2002) Multicenter, prospective, randomized, single-blind study comparing the efficacy and gastrointestinal complications of early jejunal feeding with early gastric feeding in critically ill patients. Crit Care Med 30:796–800
Vincent JL, Ferreira F, Moreno R (2000) Scoring systems for assessing organ dysfunction and survival. Crit Care Clin 16:353–366
Moylan JA, Detmer DE, Rose J, Schulz R (1976) Evaluation of the quality of hospital care for major trauma. J Trauma 16:517–523
Bratton S, Bullock R, Carney N et al (2005) Guidelines for the management of severe traumatic brain injury. J Neurotrauma 24:S1–106
Kaye AH, Andrewas D (2000) Glasgow outcome scale: research scale or blunt instrument? Lancet 356:1541–1543
Bloom M, Hjorne N (1975) Immunochemical determination of serum albumin with a centrifugal analyser. Clin Chem 21:195–198
Andrews PJ, Citerio G, Longhi L, Polderman K, Sahuquillo J, Vajkoczy P (2008) NICEM consensus on neurological monitoring in acute neurological diseases. Intensive Care Med 34:1362–1370
Hubmayr RD (2002) Statement of the 4th International Consensus Conference in Critical Care on ICU-acquired pneumonia—Chicago, IIlinois, May 2002. Intensive Care Med 28:1521–1536
Valles J, Pobo A, Garcia-Esquirol O, Mariscal D, Real J, Fernandez R (2007) Excess ICU mortality attributable to ventilator-associated pneumonia: the role of early versus delayed onset. Intensive Care Med 33:1363–1368
Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM (1988) CDC definitions for nosocomial infections. Am J Infect Control 16:128–140
Calandra T, Cohen J (2005) The international sepsis forum consensus conference on definitions of infections in the intensive care unit. Crit Care Med 33:1538–1548
Montejo JC, Nutritional and Metabolic Working Group of the Spanish Society of Intensive Care Medicine and Coronary Units (1999) Enteral nutrition-related gastrointestinal complications in critically ill patients. A multicenter study. Crit Care Med 27:1447–1453
Jeremitsky E, Omert LA, Dunham CM, Wilberger J, Rodriguez A (2005) The impact of hyperglycemia on patients with severe brain injury. J Trauma 58:47–50
Laird AM, Miller PR, Kilgo PD, Meredith JW, Chang MC (2004) Relationship of early hyperglycemia to mortality in trauma patients. J Trauma 56:1058–1062
American Thoracic Society Ad Hoc Committee of the Scientific Assembly on Microbiology Tuberculosis and Pulmonary Infections (1995) Hospital acquired pneumonia in adults: diagnosis, assessment of severity, initial antimicrobial therapy and preventive strategies: a consensus statement. Am J Respir Crit Care Med 153:1711–1725
Strong R, Condon S, Solinger M, Namihas BN, Ito-Wong LA, Leuty JE (1992) Equal aspiration rates from postpylorus and intragastric-placed small-bore nasoenteric feeding tubes: a randomized, prospective study. JPEN 16:59–63
Kearns PJ, Chin D, Mueller L, Wallace K, Jensen WA, Kirsch CM (2000) The incidence of ventilator associated pneumonia and success in nutrient delivery with gastric versus small intestinal feeding: a randomized clinical trial. Crit Care Med 28:1742–1746
Heyland DK, Dhaliwal, Drover JW, Gramlich L, Dodek P (2003) Canadian clinical practice guidelines for nutrition support in mechanically ventilated, critically ill adult patients. JPEN 27:255–273
Ho KM, Dobb GJ, Webb SA (2006) A comparison of early gastric and post-pyloric feeding in critically ill patients: a meta-analysis. Intensive Care Med 32:639–649
Norton JA, Ott LG, McClain C, Adams L, Dempsey RJ, Haack D, Tibbs PA, Young AB (1988) Intolerance to enteral feeding in the brain injured patient. J Neurosurgery 68:62–68
Taylor SJ, Fettes SB, Jewkes C, Nelson RJ (1999) Prospective, randomized, controlled trial to determine the effect of early enhanced enteral nutrition on clinical outcome in mechanically ventilated patients suffering head injury. Crit Care Med 27:2525–2531
Ravasco P, Camilo M (2003) Tube feeding in mechanically ventilated critically ill patients: a prospective clinical audit. Nutr Clin Pract 18:427–433
Grau T, Bonet A, The Nutrition and Metabolism Working Group of the Spanish Society of Ctirical Care (SEMICYUC) (2005) Multicenter study on incidence of total parenteral nutrition complications in the critically-ill patient. ICOMEP study. Part II. Nutr Hosp 20:278–285
DeMeo M, Bruninga K (2002) Physiology of the aerodigestive system and aberrations in that system resulting in aspiration. JPEN 26:S9–S17
Bochicchio GV, Bochicchio K, Nehman S, Casey C, Andrews P, Scalea TM (2006) Tolerance and efficacy of enteral nutrition in traumatic brain-injured patients induced into barbiturate coma. JPEN 30:503–506
Tarling MM, Toner CC, Withington PS, Baxter MK, Whelpton R, Goldhill DR (1997) A model of gastric emptying using paracetamol absorption in intensive care patients. Intensive Care Med 23:256–260
Acosta JA, Carrasco R, Fernández M et al (2001) Intolerancia enteral gástrica en pacientes con lesión cerebral de origen traumático, ventilados mecánicamente. Nutr Hosp 6:262–267
Martindale RG, McClave SA, Vanek VW, McCarthy M, Roberts P, Taylor B, Ochoa JB, Napolitano L, Cresci G, American College of Critical Care Medicine, A.S.P.E.N. Board of Directors (2009) Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of Critical Care Medicine and American Society for Parenteral and Enteral Nutrition: executive summary. Crit Care Med 37:1757–1761
Hadley MN, Grahm TW, Harrington T, Schiller WR, McDermott MK, Posillico DB (1986) Nutritional support and neurotrauma: a critical review of early nutrition in forty-five acute head injury patients. Neurosurgery 19:367–373
Yavagal DR, Karnad DR, Oak JL (2000) Metoclopramide for preventing pneumonia in critically ill patients receiving enteral tube feeding: a randomized controlled trial. Crit Care Med 28:1408–1411
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Acosta-Escribano, J., Fernández-Vivas, M., Grau Carmona, T. et al. Gastric versus transpyloric feeding in severe traumatic brain injury: a prospective, randomized trial. Intensive Care Med 36, 1532–1539 (2010). https://doi.org/10.1007/s00134-010-1908-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-010-1908-3