Abstract
Introduction
Positive fluid balance has been associated with an increased risk for mortality in critically ill patients with acute kidney injury with or without renal replacement therapy (RRT). Data on fluid accumulation prior to RRT initiation and mortality are limited. We aimed to study the association between fluid accumulation at RRT initiation and 90-day mortality.
Methods
We conducted a prospective, multicenter, observational cohort study in 17 Finnish intensive care units (ICUs) during a five-month period. We collected data on patient characteristics, RRT timing, and parameters at RRT initiation. We studied the association of parameters at RRT initiation, including fluid overload (defined as cumulative fluid accumulation > 10% of baseline weight) with 90-day mortality.
Results
We included 296 RRT-treated critically ill patients. Of 283 patients with complete data on fluid balance, 76 (26.9%) patients had fluid overload. The median (interquartile range) time from ICU admission to RRT initiation was 14 (3.3 to 41.5) hours. The 90-day mortality rate of the whole cohort was 116 of 296 (39.2%; 95% confidence interval 38.6 to 39.8%). The crude 90-day mortality of patients with or without fluid overload was 45 of 76 (59.2%) vs. 65 of 207 (31.4%), P < 0.001. In logistic regression, fluid overload was associated with an increased risk for 90-day mortality (odds ratio 2.6) after adjusting for disease severity, time of RRT initiation, initial RRT modality, and sepsis. Of the 168 survivors with data on RRT use at 90 days, 34 (18.9%, 95% CI 13.2 to 24.6%) were still dependent on RRT.
Conclusions
Patients with fluid overload at RRT initiation had twice as high crude 90-day mortality compared to those without. Fluid overload was associated with increased risk for 90-day mortality even after adjustments.
Similar content being viewed by others
Introduction
Four to eight percent of intensive care unit (ICU) patients receive renal replacement therapy (RRT) for acute kidney injury (AKI) [1–4]. The outcome of these severely ill patients remains poor with reported 90-day mortality rates varying between 45 and 74% [2, 5–9]. The optimal timing of RRT initiation is unclear, although some studies suggest that early initiation might be beneficial [10, 11]. The importance of fluid balance as a timing parameter has been highlighted [12, 13]. An association of a greater degree of fluid accumulation at RRT initiation with higher mortality has been well documented in pediatric ICU patients [14, 15]. Among adults, more positive mean daily fluid balance during ICU stay [16] or after RRT initiation [17] has been associated with increased mortality. Higher degree of fluid accumulation based on data on fluid balance from three days preceding nephrologist consultation [18] and on weight gain at RRT initiation in a retrospective cohort [19] has been associated with increased risk for death.
No studies presenting cumulative fluid balance from ICU admission to RRT initiation exist. Therefore, we aimed to evaluate the association of factors at RRT initiation and especially cumulative fluid accumulation with 90-day mortality in critically ill adults.
Materials and methods
Patients
We performed a prospective, observational cohort study, the FINNAKI study, from 1 September 2011 to 1 February 2012, in 17 Finnish ICUs. The referral areas of these ICUs cover 85% of the Finnish adult population. The Ethics Committee of the Department of Surgery, Hospital District of Helsinki and Uusimaa approved the study protocol and the use of deferred consent with a signed, informed consent from the patient or a proxy obtained as soon as possible. The Finnish National Institute of Health approved the collection of data from medical records of deceased patients if an informed consent could not be obtained.
We included all adult patients with either emergency ICU admission or elective post-operative ICU admission with an expected ICU stay of more than 24 hours. We excluded patients 1) with end-stage renal disease (ESRD) on chronic dialysis 2) who had already participated in the FINNAKI study and had received RRT during that previous ICU admission 3) not permanently living in Finland or having insufficient language skills for giving an informed consent, and 4) on intermediate care (Figure 1). Of patients receiving RRT, we excluded those who received RRT only for intoxication or plasmapheresis for non-renal indications. For analyses regarding fluid accumulation, we excluded patients with incomplete data on fluid balance. The decision to initiate RRT and the choice of RRT modality were based on the judgment of the treating clinician.
Data collection
We collected physiological data, laboratory values, Sequential Organ Failure Assessment (SOFA) [20] and Simplified Acute Physiology Score (SAPS) II [21] scores, Acute Physiology and Chronic Health Evaluation (APACHE) III diagnoses, and patients' baseline weight with the help of the Finnish Intensive Care Consortium database using electronic patient records. We collected data on patients' chronic illnesses, baseline creatinine (latest creatinine value a week to a year prior to ICU admission), and treatment prior to ICU admission. The patients' daily fluid balance was calculated in the electronic patient records by summing the amount of fluids given (maintenance and resuscitation fluids, blood products, drug infusions, and enteral and parenteral nutrition), from which losses (urine output, bleeding, output from drains, rectal and nasogastric tube, and surrogate for evaporation (1000 mL for normothermic patients, and an addition per each Celsius degree of fever per hour)) were subtracted. We recorded data on patients' daily fluid balance from ICU admission to day five and obtained data on cumulative fluid balance of patients with RRT initiated after day five. We collected data on the given RRT treatment daily during the first five days and, thereafter, twice a week. We recorded the RRT replacement fluid flow and dilution mode, dialysis fluid flow, and the blood flow once daily. We calculated the CRRT dose (mL/kg/hr) according to previous equations [22] and considered treatment modality, blood flow, dilution mode, hematocrit, replacement and dialysis fluid flow, and the patient's weight. We recorded hospital mortality, length of ICU and hospital stay, and patients' need for RRT at 90 days from admission. We obtained patients' vital status 90 days from ICU admission from the Finnish Population Register Centre.
Definitions
We calculated the total cumulative fluid balance from ICU admission to RRT initiation (including the day of RRT initiation) and defined the percentage of fluid accumulation by dividing the cumulative balance in liters by patient's baseline weight and multiplying by 100%. We then used the cutoff value of 10% of fluid accumulation as a definition of fluid overload [18, 23]. We assessed presence of sepsis on admission and on days one to five according to the American College of Chest Physicians/Society of Critical Care Medicine definition [24]. We defined renal recovery as RRT independency at 90 days from ICU admission [25].
Statistical methods
We report data as count and percentages or medians with interquartile range (IQR, 25th to 75th percentiles). We used Fisher's exact test to compare proportions and Mann-Whitney U-test to compare continuous data and calculated 95% confidence intervals (CI) for the main outcome. We studied factors associated with 90-day mortality with backwards logistic regression. We used stepwise elimination approach and a significance level of < 0.05 for entry and > 0.10 for removal. We entered the following variables: age, SAPS II score without age points, non-renal SOFA score on the day of RRT initiation, time from ICU admission to RRT initiation (days), initial RRT modality (continuous or intermittent), lactate (mmol/L), base excess (mmol/L), and plasma creatinine (umol/L) at RRT initiation, cumulative urine output on the day of RRT initiation, colloid use prior to RRT initiation (including data from ICU stay and 48 hours prior to ICU admission), presence of severe sepsis (yes/no) during the ICU admission, and fluid accumulation (%) at RRT initiation. We studied fluid overload (fluid accumulation > 10%) as a categorical variable in a separate model with all other covariates being the same as in the first model. We studied the potential interactions in separate models between degree of fluid accumulation (%) and 1) SAPS II score without age points, 2) day of RRT initiation, and 3) presence of severe sepsis 4) creatinine prior to RRT initiation and 5) urine output on the day of RRT initiation. We tested the goodness-of-fit with the Hosmer-Lemeshow test and calculated the area under the receiver operating characteristic curve (AUC) and correct classification rate. We examined the 90-day survival with Kaplan-Meier curves, and compared survival at 90 days between patients with and without fluid overload at RRT initiation with the log-rank test. We considered a two-sided P value lower than 0.05 as significant and made no corrections for multiple comparisons. In logistic regression, we set the significance level at 0.01. We performed the statistical analysis using the SPSS Statistics version 19.0 (SPSS Inc, Chicago, IL, USA).
Results
We included 296 patients in the study (Figure 1). Source of admission and APACHE III diagnosis groups are presented in Table 1. The median (IQR) number of underlying co-morbidities was 1 (0 to 2), hypertension in 156 (53%), diabetes in 111 (37%), and coronary artery disease and/or peripheral vascular disease in 48 (16%) patients being the most common. Chronic kidney disease without the need for maintenance dialysis was reported in 47 (16%) patients. Patient characteristics, parameters at RRT initiation, and length of stay of all patients and a comparison between survivors and non-survivors are presented in Table 2.
Of 283 patients with complete data on fluid balance, 76 (26.9%) patients had fluid overload (Figure 1). Patients with fluid overload were more often admitted because of sepsis (25.0% vs. 8.2%, P < 0.001), while patients without fluid overload had renal disease as APACHE III admission diagnosis (22.7% vs. 2.6%, P < 0.001) more frequently. Other baseline characteristics and parameters at RRT initiation stratified according to fluid overload status are presented in Table 3. Patients with fluid overload at RRT initiation had a trend for a more positive daily fluid balance after RRT initiation (Additional file 1, Figure S1). No statistically significant differences in fluid removal with RRT existed between the groups (Additional file 2, Figure S2).
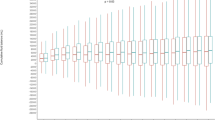
Renal replacement therapy
The median (IQR) number of reported indications for RRT was 3 (2 to 4). The most common indications were oliguria in 223 (78%), high creatinine in 196 (70%), acidosis in 181 (65%), and fluid accumulation in 116 (43%) patients. RRT was initiated on the first ICU treatment day in 124 (41.9%), on day two in 86 (29.1%), on day three in 37 (12.5%), and on day four or after in 49 (16.6%) patients. When patients were classified according to the day of RRT initiation, the degree of fluid accumulation increased until the day three (Additional file 3, Figure S3.) Of the 215 patients who initially received continuous RRT (CRRT), 111 (51.6%) received continuous veno-venous hemodialysis, 93 (43.3%) continuous veno-venous hemodiafiltration and 11 (5.1%) continuous veno-venous hemofiltration. The median (IQR) prescribed CRRT dose was 35.3 (31.2 to 40.6) mL/kg/hr (data from 205 of 215 patients). The median (IQR) daily duration of CRRT was 19.0 (9.3 to 24.0) hr (data from 680 CRRT treatment days), and CRRT dose adjusted for the treatment duration was 27.9 mL/kg/hr. The median (IQR) number of days patients who received CRRT (n = 230) was 3 (2 to 6) and number of intermittent RRT (n = 163) sessions 2 (1 to 4).
Outcomes
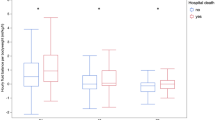
Of the 296 patients, 96 (32.4%; 95% CI 31.9 to 32.9%) died in hospital and 116 (39.2%; 95% CI 38.6 to 39.8%) before day 90. The SAPS II -based standardized mortality ratio (95% CI) was 0.64 (0.52 to 0.78). The hospital mortality of patients with or without fluid overload was 43 of 76 (56.6%) and 49 of 207 (23.7%), P < 0.001. The unadjusted 90-day survival of patients with fluid overload compared to those without is presented in Figure 2. The 90-day mortality rate increased as the degree of fluid accumulation increased (Figure 3). At 90 days, 34 of 168 (18.9%; 95% CI 13.2 to 24.6%) survivors (12 patients lost to follow-up) were dependent on RRT.
In logistic regression for 90-day mortality, no interactions between fluid accumulation percentage and 1) SAPS II score without age points, 2) time from ICU admission to RRT initiation, 3) presence of severe sepsis 4) creatinine prior to RRT initiation, or 5) urine output on the day of RRT initiation were present. The final model with fluid overload studied as categorical variable had Hosmer-Lemeshow chi-square 8.6 (P = 0.375), an AUC of 0.816 (95% CI 0.767 to 0.866), and correct classification rate of 74.4%. The results of the final model are presented in Table 4.
Discussion
In this prospective, observational, nationwide cohort study in critically ill patients with RRT, the 90-day mortality rate was 39%. Median time from ICU admission to RRT initiation was 14 hours. Patients with fluid overload at RRT initiation had twice as high crude 90-day mortality compared to those without. Additionally, fluid overload was independently associated with an increased risk for 90-day mortality. Of 90-day survivors, 19% were dependent on RRT at 90 days.
We demonstrated an association between cumulative fluid overload at RRT initiation and increased risk for 90-day mortality, which remained significant after adjustment for disease severity, time of RRT initiation, initial RRT modality, patient's sepsis status, and several other parameters. The majority of non-survivors with fluid overload died in the hospital within a short time period, implying a severe course of disease. Fluid overload has been proposed as a biomarker of critical illness [26]. The mortality rate increased as the degree of fluid accumulation increased, which speaks for a potential dose-response relationship. RRT was initiated later on patients with fluid overload, and potentially, initiating RRT earlier could have altered their outcome.
In critically ill children, a strong association between fluid overload at CRRT initiation and mortality has been found [14, 15]. In adults, a conservative fluid management strategy compared to a liberal strategy in patients with acute lung injury increased neither the incidence of AKI nor the need for RRT [27]. Among those with AKI, more positive fluid balance after AKI diagnosis was associated with higher adjusted mortality [28]. In a secondary analysis of the randomized evaluation of normal vs. augmented level (RENAL) study, positive mean daily fluid balance after RRT initiation was associated with worse outcome [6]. Payen et al. [16] demonstrated an association between higher mean daily fluid balance among AKI patients with and without RRT and 60-day mortality. Bagshaw et al. [29] found fluid accumulation over 5% of weight from 24 hours preceding RRT initiation to be associated with hospital mortality with an adjusted odds ratio (OR) of 2.31. Another study found fluid accumulation over 10% to be associated with 60-day mortality after adjusting for disease severity and RRT modality with an OR of 2.07 [18]. The calculations of cumulative balance were based on data from three days preceding nephrologist consultation, and neither the time point of the consultation nor the time between consultation and RRT initiation were specified [18, 30]. A retrospective study also including patients treated outside ICUs [19] and a small prospective study [31] used weight at RRT initiation compared to baseline weight to determine fluid accumulation, and found that fluid accumulation was associated with an increased risk for mortality. A more positive fluid balance has been associated with increased risk for developing AKI after cardiovascular surgery [32] and a trend for increased need for RRT among septic shock patients with higher cumulative fluid balance has been noted [33]. Our results join the growing body of evidence showing an association between fluid overload and increased risk for mortality [14–19, 29].
The 90-day mortality found in this study was lower compared to previous reports. In the RENAL study the 90-day mortality rate was 45% [6]. Randomization took place two days from ICU admission [6] and RRT was initiated later compared to our study. Furthermore, patients expected to die within 24 hours were excluded [6]. A prospective study also including patients treated outside ICUs reported a 90-day mortality rate of 48% [9]. In a large, retrospective cohort study, the 90-day mortality rate was 50%, with no disease severity score reported, but 85% of the patients initially received CRRT [5]. Several studies with higher disease severity scores have reported higher mortality rates from 56% [2, 34] to 72% [35]. The early initiation of RRT in our study may be one plausible explanation for the lower 90-day mortality observed.
Hydroxyethyl starch solutions have been shown to increase mortality among patients with severe sepsis in the 6S trial [36]. In our study, 90% of patients with fluid accumulation received colloids prior to RRT initiation. Difference in colloid use was significant both between patients with or without fluid overload and survivors and non-survivors. However, colloid use did not remain significant in the logistic regression model for 90-day mortality. Moreover, the separation of the survival curves of patients with and without fluid overload occurred early after ICU admission, while the in the 6S trial the starch group separated from the Ringer's acetate group later [36].
The indications for RRT were in line with previous studies [6, 37]. In few reports RRT has been initiated as early in terms of ICU treatment days [29, 38], most studies reporting a median time from ICU admission to RRT initiation or randomization for RRT from two to seven days [6, 7, 39, 40]. The proportion of patients initially receiving CRRT was higher than in a U.S. cohort with 56% [30] but corresponding to reports from Canada [29] and Taiwan [7] and slightly lower compared to a multinational study [38]. The initial CRRT dose adjusted for daily duration of CRRT was in line with the current recommendations [13].
Our study has some limitations. First, we were not able to record the fluid balance preceding ICU admission. However, in contrast to other studies [18, 29] we recorded data on cumulative balance from ICU admission to RRT initiation day. Second, we could not relate the degree of fluid accumulation to physiologic parameters such as pulmonary capillary wedge pressure or stroke volume variation index. Third, regrettably, we did not collect data regarding the colloid type administered. Thus, we cannot separate to which extent the use of starch accounted for the worse outcome among patients with fluid overload. However, the use of any type of colloid did not remain significant in the logistic regression model. Fourth, the power of this study did not allow us to study the association between fluid accumulation and renal recovery. Finally, as this was an observational study, there may be factors that we did not measure that affected outcome, and the observed association does not imply causation. However, we reported data from a nationwide, non-selected patient cohort, with meticulously recorded prospective data about RRT timing.
Conclusions
In this observational cohort study, the 90-day mortality of critically ill patients treated with RRT was 39%. Patients with fluid overload had twice as high 90-day mortality compared to those without. Fluid overload was associated with a markedly increased risk for 90-day mortality even after adjustments.
Key messages
-
AKI patients treated with RRT had a 90-day mortality of 39%.
-
RRT was initiated early, a median of 14 hours after ICU admission.
-
Patients with fluid overload (> 10% of weight) at RRT initiation had higher crude mortality compared to those without and had an increased risk for 90-day mortality after adjusting for disease severity, time of RRT initiation, RRT modality, and presence of severe sepsis.
-
At 90 days, 19% of survivors were still dependent on RRT.
Abbreviations
- AKI:
-
acute kidney injury
- APACHE:
-
Acute Physiology and Chronic Health Evaluation
- AUC:
-
area under the receiver operating characteristic curve
- CI:
-
confidence interval
- CRRT:
-
continuous renal replacement therapy
- ICU:
-
intensive care unit
- IQR:
-
interquartile range
- OR:
-
odds ratio
- RRT:
-
renal replacement therapy
- SAPS:
-
Simplified Acute Physiology Score
- SOFA:
-
Sequential Organ Failure Assessment.
References
Uchino S, Kellum JA, Bellomo R, Doig GS, Morimatsu H, Morgera S, Schetz M, Tan I, Bouman C, Macedo E, Gibney N, Tolwani A, Ronco C: Acute renal failure in critically ill patients: a multinational, multicenter study. JAMA 2005, 294: 813-818. 10.1001/jama.294.7.813
Bagshaw SM, Laupland KB, Doig CJ, Mortis G, Fick GH, Mucenski M, Godinez-Luna T, Svenson LW, Rosenal T: Prognosis for long-term survival and renal recovery in critically ill patients with severe acute renal failure: a population-based study. Crit Care 2005, 9: R700-9. 10.1186/cc3879
Vaara ST, Pettilä V, Reinikainen M, Kaukonen KM, for the Finnish Intensive Care Consortium: Population-based incidence, mortality and quality of life in critically ill patients treated with renal replacement therapy: a nationwide retrospective cohort study in Finnish intensive care units. Crit Care 2012, 16: R13. 10.1186/cc11158
Piccinni P, Cruz DN, Gramaticopolo S, Garzotto F, Dal Santo M, Aneloni G, Rocco M, Alessandri E, Giunta F, Michetti V, Iannuzzi M, Belluomo Anello C, Brienza N, Carlini M, Pelaia P, Gabbanelli V, Ronco C: Prospective multicenter study on epidemiology of acute kidney injury in the ICU: a critical care nephrology Italian collaborative effort (NEFROINT). Minerva Anestesiol 2011, 77: 1072-1083.
Bell M, Swing , Granath F, Schon S, Ekbom A, Martling CR: Continuous renal replacement therapy is associated with less chronic renal failure than intermittent haemodialysis after acute renal failure. Intensive Care Med 2007, 33: 773-780. 10.1007/s00134-007-0590-6
The RENAL replacement study investigators: Intensity of continuous renal-replacement therapy in critically ill patients. N Engl J Med 2009, 361: 1627-1638.
Lin YF, Ko WJ, Chu TS, Chen YS, Wu VC, Chen YM, Wu MS, Chen YW, Tsai CW, Shiao CC, Li WY, Hu FC, Tsai PR, Tsai TJ, Wu KD, NSARF Study Group: The 90-day mortality and the subsequent renal recovery in critically ill surgical patients requiring acute renal replacement therapy. Am J Surg 2009, 198: 325-332. 10.1016/j.amjsurg.2008.10.021
Saudan P, Niederberger M, De Seigneux S, Romand J, Pugin J, Perneger T, Martin PY: Adding a dialysis dose to continuous hemofiltration increases survival in patients with acute renal failure. Kidney Int 2006, 70: 1312-1317. 10.1038/sj.ki.5001705
Prescott GJ, Metcalfe W, Baharani J, Khan IH, Simpson K, Smith WC, MacLeod AM: A prospective national study of acute renal failure treated with RRT: incidence, aetiology and outcomes. Nephrol Dial Transplant 2007, 22: 2513-2519. 10.1093/ndt/gfm264
Seabra VF, Balk EM, Liangos O, Sosa MA, Cendoroglo M, Jaber BL: Timing of renal replacement therapy initiation in acute renal failure: a meta-analysis. Am J Kidney Dis 2008, 52: 272-284. 10.1053/j.ajkd.2008.02.371
Karvellas CJ, Farhat MR, Sajjad I, Mogensen SS, Leung AA, Wald R, Bagshaw SM: A comparison of early versus late initiation of renal replacement therapy in critically ill patients with acute kidney injury: a systematic review and meta-analysis. Crit Care 2011, 15: R72. 10.1186/cc10061
Ostermann M, Dickie H, Barrett NA: Renal replacement therapy in critically ill patients with acute kidney injury - when to start. Nephrol Dial Transplant 2012, 27: 2242-2248. 10.1093/ndt/gfr707
Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group: KDIGO Clinical Practice Guideline for Acute Kidney Injury. Kidney Int Suppl 2012, 2: 1-138.
Goldstein SL, Somers MJ, Baum MA, Symons JM, Brophy PD, Blowey D, Bunchman TE, Baker C, Mottes T, McAfee N, Barnett J, Morrison G, Rogers K, Fortenberry JD: Pediatric patients with multi-organ dysfunction syndrome receiving continuous renal replacement therapy. Kidney Int 2005, 67: 653-658. 10.1111/j.1523-1755.2005.67121.x
Sutherland SM, Zappitelli M, Alexander SR, Chua AN, Brophy PD, Bunchman TE, Hackbarth R, Somers MJ, Baum M, Symons JM, Flores FX, Benfield M, Askenazi D, Chand D, Fortenberry JD, Mahan JD, McBryde K, Blowey D, Goldstein SL: Fluid overload and mortality in children receiving continuous renal replacement therapy: the prospective pediatric continuous renal replacement therapy registry. Am J Kidney Dis 2010, 55: 316-325. 10.1053/j.ajkd.2009.10.048
Payen D, de Pont AC, Sakr Y, Spies C, Reinhart K, Vincent JL, Sepsis Occurrence in Acutely Ill Patients (SOAP) investigators: A positive fluid balance is associated with a worse outcome in patients with acute renal failure. Crit Care 2008, 12: R74. 10.1186/cc6916
The RENAL replacement study investigators, Bellomo R, Cass A, Cole L, Finfer S, Gallagher M, Lee J, Lo S, McArthur C, McGuiness S, Norton R, Myburgh J, Scheinkestel C, Su S: An observational study fluid balance and patient outcomes in the randomized evaluation of normal vs. augmented level of replacement therapy trial. Crit Care Med 2012, 40: 1753-1760.
Bouchard J, Soroko SB, Chertow GM, Himmelfarb J, Ikizler TA, Paganini EP, Mehta RL: Fluid accumulation, survival and recovery of kidney function in critically ill patients with acute kidney injury. Kidney Int 2009, 76: 422-427. 10.1038/ki.2009.159
Heung M, Wolfgram DF, Kommareddi M, Hu Y, Song PX, Ojo AO: Fluid overload at initiation of renal replacement therapy is associated with lack of renal recovery in patients with acute kidney injury. Nephrol Dial Transplant 2012, 27: 956-961. 10.1093/ndt/gfr470
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonca A, Bruining H, Reinhart CK, Suter PM, Thijs LG: The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. Intensive Care Med 1996, 22: 707-10. 10.1007/BF01709751
Le Gall JR, Lemeshow S, Saulnier F: A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA 1993, 270: 2957-2963. 10.1001/jama.1993.03510240069035
Clark WR, Turk JE, Kraus MA, Gao D: Dose determinants in continuous renal replacement therapy. Artificial organs 2003, 27: 815-820. 10.1046/j.1525-1594.2003.07288.x
Brierley J, Carcillo JA, Choong K, Cornell T, Decaen A, Deymann A, Doctor A, Davis A, Duff J, Dugas MA, Duncan A, Evans B, Feldman J, Felmet K, Fisher G, Frankel L, Jeffries H, Greenwald B, Gutierrez J, Hall M, Han YY, Hanson J, Hazelzet J, Hernan L, Kiff J, Kissoon N, Kon A, Irazuzta J, Lin J, Lorts A, et al.: Clinical practice parameters for hemodynamic support of pediatric and neonatal septic shock: 2007 update from the American College of Critical Care Medicine. Crit Care Med 2009, 37: 666-688. 10.1097/CCM.0b013e31819323c6
Bone RC, Balk RA, Cerra FB, Dellinger RP, Fein AM, Knaus WA, Schein RM, Sibbald WJ: Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. The ACCP/SCCM Consensus Conference Committee. American College of Chest Physicians/Society of Critical Care Medicine. Chest 1992, 101: 1644-1655. 10.1378/chest.101.6.1644
Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P, Acute Dialysis Quality Initiative workgroup: Acute renal failure - definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care 2004, 8: R204-12. 10.1186/cc2872
Bagshaw SM, Brophy PD, Cruz D, Ronco C: Fluid balance as a biomarker: impact of fluid overload on outcome in critically ill patients with acute kidney injury. Crit Care 2008, 12: 169. 10.1186/cc6948
Wiedemann HP, Wheeler AP, Bernard GR, Thompson BT, Hayden D, deBoisblanc B, Connors AF Jr, Hite RD, Harabin AL: Comparison of two fluid-management strategies in acute lung injury. N Engl J Med 2006, 354: 2564-2575.
Grams ME, Estrella MM, Coresh J, Brower RG, Liu KD: Fluid balance, diuretic use, and mortality in acute kidney injury. Clin J Am Soc Nephrol 2011, 6: 966-973. 10.2215/CJN.08781010
Bagshaw SM, Wald R, Barton J, Burns KE, Friedrich JO, House AA, James MT, Levin A, Moist L, Pannu N, Stollery DE, Walsh MW: Clinical factors associated with initiation of renal replacement therapy in critically ill patients with acute kidney injury-A prospective multicenter observational study. J Critical Care 2012, 27: 268-275. 10.1016/j.jcrc.2011.06.003
Mehta RL, Pascual MT, Soroko S, Savage BR, Himmelfarb J, Ikizler TA, Paganini EP, Chertow GM: Spectrum of acute renal failure in the intensive care unit: the PICARD experience. Kidney Int 2004, 66: 1613-1621. 10.1111/j.1523-1755.2004.00927.x
Fulop T, Pathak MB, Schmidt DW, Lengvarszky Z, Juncos JP, Lebrun CJ, Brar H, Juncos LA: Volume-related weight gain and subsequent mortality in acute renal failure patients treated with continuous renal replacement therapy. ASAIO J 2010, 56: 333-337.
Dass B, Shimada M, Kambhampati G, Ejaz NI, Arif AA, Ejaz AA: Fluid balance as an early indicator of acute kidney injury in CV surgery. Clin Nephrol 2012, 77: 438-444.
Smith SH, Perner A: Higher vs. lower fluid volume for septic shock: clinical characteristics and outcome in unselected patients in a prospective, multicenter cohort. Crit Care 2012, 16: R76. 10.1186/cc11333
Delannoy B, Floccard B, Thiolliere F, Kaaki M, Badet M, Rosselli S, Ber CE, Saez A, Flandreau G, Guerin C: Six-month outcome in acute kidney injury requiring renal replacement therapy in the ICU: a multicentre prospective study. Intensive Care Med 2009, 35: 1907-1915. 10.1007/s00134-009-1588-z
Vinsonneau C, Camus C, Combes A, Costa de Beauregard MA, Klouche K, Boulain T, Pallot JL, Chiche JD, Taupin P, Landais P, Dhainaut JF, Hemodiafe Study Group: Continuous venovenous haemodiafiltration versus intermittent haemodialysis for acute renal failure in patients with multiple-organ dysfunction syndrome: a multicentre randomised trial. Lancet 2006, 368: 379-385. 10.1016/S0140-6736(06)69111-3
Perner A, Haase N, Guttormsen AB, Tenhunen J, Klemenzson G, Aneman A, Madsen KR, Moller MH, Elkjaer JM, Poulsen LM, Bendtsen A, Winding R, Steensen M, Berezowicz P, Soe-Jensen P, Bestle M, Strand K, Wiis J, White JO, Thornberg KJ, Quist L, Nielsen J, Andersen LH, Holst LB, Thormar K, Kjaeldgaard AL, Fabritius ML, Mondrup F, Pott FC, Moller TP, et al.: Hydroxyethyl starch 130/0.4 versus Ringer's acetate in severe sepsis. N Engl J Med 2012, 367: 124-34. 10.1056/NEJMoa1204242
Uchino S, Bellomo R, Morimatsu H, Morgera S, Schetz M, Tan I, Bouman C, Macedo E, Gibney N, Tolwani A, Oudemans-van Straaten H, Ronco C, Kellum JA: Continuous renal replacement therapy: a worldwide practice survey. The beginning and ending supportive therapy for the kidney (BEST kidney) investigators. Intensive Care Med 2007, 33: 1563-1570. 10.1007/s00134-007-0754-4
Bagshaw SM, Uchino S, Bellomo R, Morimatsu H, Morgera S, Schetz M, Tan I, Bouman C, Macedo E, Gibney N, Tolwani A, Oudemans-van Straaten HM, Ronco C, Kellum JA: Timing of renal replacement therapy and clinical outcomes in critically ill patients with severe acute kidney injury. J Critical Care 2009, 24: 129-140. 10.1016/j.jcrc.2007.12.017
Palevsky PM, Zhang JH, O'Connor TZ, Chertow GM, Crowley ST, Choudhury D, Finkel K, Kellum JA, Paganini E, Schein RM, Smith MW, Swanson KM, Thompson BT, Vijayan A, Watnick S, Star RA, Peduzzi P: Intensity of renal support in critically ill patients with acute kidney injury. N Engl J Med 2008, 359: 7-20.
Maccariello E, Soares M, Valente C, Nogueira L, Valenca RV, Machado JE, Rocha E: RIFLE classification in patients with acute kidney injury in need of renal replacement therapy. Intensive Care Med 2007, 33: 597-605. 10.1007/s00134-007-0535-0
Acknowledgements
The study has been supported by the Academy of Finland, Helsinki University Central Hospital EVO grants (T 102010070 and TYH 2010109 and 2011210), and a grant from the Finnish Society of Intensive Care. STV has received a grant from the Finnish Kidney Foundation and the Instrumentarium Foundation.
We thank all members of the FINNAKI study group in participating hospitals and Tieto Healthcare and Welfare Ltd for database management.
The FINNAKI study group
Central Finland Central Hospital: Raili Laru-Sompa, Anni Pulkkinen, Minna Saarelainen, Mikko Reilama, Sinikka Tolmunen, Ulla Rantalainen, Marja Miettinen; East Savo Central Hospital: Markku Suvela, Katrine Pesola, Pekka Saastamoinen, Sirpa Kauppinen; Helsinki University Central Hospital: Ville Pettilä, Kirsi-Maija Kaukonen, Anna-Maija Korhonen, Sara Nisula, Suvi Vaara, Raili Suojaranta-Ylinen, Leena Mildh, Mikko Haapio, Laura Nurminen, Sari Sutinen, Leena Pettilä, Helinä Laitinen, Heidi Syrjä, Kirsi Henttonen, Elina Lappi, Hillevi Boman; Jorvi Central Hospital: Tero Varpula, Päivi Porkka, Mirka Sivula, Mira Rahkonen, Anne Tsurkka, Taina Nieminen, Niina Pirttinen; Kanta-Häme Central hospital: Ari Alaspää, Ville Salanto, Hanna Juntunen, Teija Sanisalo; Kuopio University Hospital: Ilkka Parviainen, Ari Uusaro, Esko Ruokonen, Stepani Bendel, Niina Rissanen, Maarit Lång, Sari Rahikainen, Saija Rissanen, Merja Ahonen, Elina Halonen, Eija Vaskelainen; Lapland Central Hospital: Meri Poukkanen, Esa Lintula, Sirpa Suominen; Länsi-Pohja Central Hospital: Jorma Heikkinen, Timo Lavander, Kirsi Heinonen, Anne-Mari Juopperi; Middle Ostrobothnia Central Hospital: Tadeusz Kaminski, Fiia Gäddnäs, Tuija Kuusela, Jane Roiko; North Karelia Central Hospital: Sari Karlsson, Matti Reinikainen, Tero Surakka, Helena Jyrkönen, Tanja Eiserbeck, Jaana Kallinen; Oulu University Hospital: Tero Ala-Kokko, Jouko Laurila, Sinikka Sälkiö; Satakunta Hospital District: Vesa Lund, Päivi Tuominen, Pauliina Perkola, Riikka Tuominen, Marika Hietaranta, Satu Johansson; South Karelia Central Hospital: Seppo Hovilehto, Anne Kirsi, Pekka Tiainen, Tuija Myllärinen, Pirjo Leino, Anne Toropainen; Tampere University Hospital: Anne Kuitunen, Jyrki Tenhunen, Ilona Leppänen, Markus Levoranta, Sanna Hoppu, Jukka Sauranen, Atte Kukkurainen, Samuli Kortelainen, Simo Varila; Turku University Hospital: Outi Inkinen, Niina Koivuviita, Jutta Kotamäki, Anu Laine.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
STV carried out the data analysis and drafted the manuscript. AMK, KMK and SN participated in designing the study. OI, SH, JL, LM, MR, VL and IP critically revised the manuscript. VP designed the study and helped to draft the manuscript. All authors participated in the data collection and read and approved the final manuscript.
Electronic supplementary material
13054_2012_926_MOESM3_ESM.PDF
Additional file 3: Figure S3: Percentage of fluid accumulation prior to RRT initiation according to RRT initiation day. (PDF 58 KB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Vaara, S.T., Korhonen, AM., Kaukonen, KM. et al. Fluid overload is associated with an increased risk for 90-day mortality in critically ill patients with renal replacement therapy: data from the prospective FINNAKI study. Crit Care 16, R197 (2012). https://doi.org/10.1186/cc11682
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/cc11682