Abstract
Supplementary oxygen is routinely administered to patients, even those with adequate oxygen saturations, in the belief that it increases oxygen delivery. But oxygen delivery depends not just on arterial oxygen content but also on perfusion. It is not widely recognized that hyperoxia causes vasoconstriction, either directly or through hyperoxia-induced hypocapnia. If perfusion decreases more than arterial oxygen content increases during hyperoxia, then regional oxygen delivery decreases. This mechanism, and not (just) that attributed to reactive oxygen species, is likely to contribute to the worse outcomes in patients given high-concentration oxygen in the treatment of myocardial infarction, in postcardiac arrest, in stroke, in neonatal resuscitation and in the critically ill. The mechanism may also contribute to the increased risk of mortality in acute exacerbations of chronic obstructive pulmonary disease, in which worsening respiratory failure plays a predominant role. To avoid these effects, hyperoxia and hypocapnia should be avoided, with oxygen administered only to patients with evidence of hypoxemia and at a dose that relieves hypoxemia without causing hyperoxia.
Similar content being viewed by others
... the aim of oxygen therapy should be to increase the delivery of oxygen rather than to reach any arbitrary concentration in the arterial blood.
EJM Campbell [1]
Is administration of oxygen, the most widely prescribed drug in the formulary, free of risks to nonhypoxemic patients with regional ischemia? Hyperoxia marginally increases the arterial blood oxygen content (CaO2), theoretically increasing tissue oxygen delivery (DO2) assuming no reduction in tissue blood flow. However, oxygen causes constriction of the coronary, cerebral, renal and other key vasculatures - and if regional perfusion decreases concomitantly with blood hyperoxygenation, one would have a seemingly paradoxical situation in which the administration of oxygen may place tissues at increased risk of hypoxic stress. Any tissue damage in the course of oxygen administration would plausibly be attributed to the underlying disease process. Ascribing hypoxic damage to oxygen administration is counter-intuitive and is difficult to accept without a receptive mindset. Considering the ubiquity of oxygen therapy, the continued low threshold for its administration, and the widespread belief that its use is justified and safe [2, 3], we believe it is important to revisit the arguments made to justify the status quo.
Owing to the vasoconstrictor effects on the coronary, cerebral, renal and other key vasculatures, there are many scenarios in which administration of oxygen decreases the perfusion to vital organs to a greater extent than the small increase in CaO2, thereby actually reducing DO2. The calculated CaO2 increases with normobaric hyperoxia (assuming all hemoglobin is already saturated) by only 0.03 ml/l per mmHg. With increases in alveolar PaO2 from 100 to 600 mmHg, CaO2 increases by 15 ml/l, or about ~7.5% assuming a hemoglobin concentration of 150 g/l.
In healthy adults, hyperoxia decreases cerebral blood flow by 11 to 33% [4, 5]. Administration of high oxygen concentrations is therefore likely to decrease brain DO2. Despite this known effect of hyperoxia on cerebral blood flow, and the published recommendations [6], patients with stroke - even those with satisfactory arterial saturations - are routinely administered oxygen [4]. Does this matter? Possibly. Although Singhal and colleagues reported transient improvement in patients with ischemic strokes [7], survival at 7 months for patients with mild or moderate strokes is significantly greater in those administered air than in those given 100% oxygen for the first 24 hours after the event [8].
Hyperoxia-induced decreases in regional DO2 are not confined to the brain. Normobaric hyperoxia reduces coronary blood flow by 8 to 29% in normal subjects and in patients with coronary artery disease or chronic heart failure [9]. The reduction in coronary artery flow is associated with a reduction in myocardial DO2 and oxygen consumption [10]. These effects may explain disturbing findings in patients with coronary artery disease. As early as 1950 Russek and colleagues reported that supplemental oxygen failed to reduce electrocardiographic signs of ischemia or reduce anginal pain in patients with myocardial infarction [11]. In 1969 Bourassa and colleagues proposed that hyperoxia-induced decreases in coronary blood flow provoke myocardial ischemia in patients with severe coronary artery disease [12]. Then in 1976, in a double-blind randomized controlled trial, Rawles and Kenmure reported greater serum aspartate aminotransferase levels, indicating increased infarct size, in patients with acute myocardial infarction receiving high-flow oxygen compared with room air [13]. They also observed a nonsignificant tripling of the death rate in those patients.
Given these concerns, the Emergency Oxygen Guideline Group of the British Thoracic Society called for 'large randomised trials of oxygen therapy for non-hypoxaemic patients with acute cardiac and cerebral ischaemia' [14]. Conti, in a recent editorial [15], reminded readers that that there is only level C evidence for the administration of supplemental oxygen to patients with uncomplicated ST elevation in myocardial infarction during the first 6 hours [16]. Based on currently available evidence, the UK National Institute for Health and Clinical Excellence guidelines have recently emphasized that 'supplementary oxygen should not be routinely administered to patients with acute chest pain of suspected cardiac origin, but that oxygen saturation levels should be monitored and used to guide its administration' [17]. Similar cautions have been expressed about the use of oxygen for the treatment of traumatic brain injury [18].
The mechanisms by which hyperoxia causes systemic vasoconstriction remain uncertain. Recent work focuses on the inhibition of vasodilators (prostaglandins, nitric oxide) by reactive oxygen species generated as a result of the hyperoxia [19–23]. Other work suggests that reactive oxygen species activate brainstem respiratory neurons [24], but this suggestion needs to be established as occurring under normobaric conditions. The role of hyperoxia-induced hypocapnia (that is, the reverse Haldane effect) remains contentious [3, 25]. Regardless of the underlying mechanism(s), the importance of considering the effects of both PaO2 and PaCO2 on vascular tone is evident in a study in which both hyperoxia and hypocapnia independently increased cerebrovascular resistance and reduced cerebral blood flow [5]. Indeed, in some situations, the vasoconstrictive effects of hyperoxia may be predominantly due to the concomitant hypocapnia [25, 26]. Positron emission tomography provides similar results: the reduction of cerebral blood flow and the increase in oxygen extraction during inhalation of 100% oxygen is completely reversed when subjects breathe carbogen (5% carbon dioxide, 95% oxygen) [27]. These observations emphasize the importance of independent control of arterial PCO2 and PO2 - possibly using dynamic forcing of alveolar gases (for example [28]) or sequential gas delivery (for example [29]) - when studying the independent effects of PO2 and PCO2 on regional perfusions. These observations also suggest that adding carbon dioxide to oxygen may offset the vasoconstriction due to hyperoxia or hypoxia-induced hypocapnia.
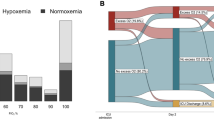
There are other clinical situations in which the routine administration of high-concentration oxygen may lead to worse outcomes, although primarily through mechanisms other than changes in regional perfusion. Austin and colleagues recently reported in a randomized controlled trial that patients with acute exacerbations of chronic obstructive pulmonary disease have a twofold to fourfold increased mortality when treated with high-flow oxygen compared with oxygen titrated to result in an arterial oxygen saturation between 88 and 92% [30]. Although several mechanisms may account for these findings [31], worsening respiratory failure is probably the predominant mechanism. Of the patients whose arterial blood gases were measured within 30 minutes of presentation to hospital, those who received high-concentration oxygen were more likely to have hypercapnia (mean difference PaCO2 34 mmHg) or respiratory acidosis (mean difference pH 0.12).
Adverse outcomes with hyperoxia have also been reported in critically ill patients admitted to the intensive care unit; a high PaO2 in the first 24 hours after admission is independently associated with in-hospital mortality [32]. In this study a U-shaped curve of mortality with PaO2 was observed, illustrating the risks of both hypoxia and hyperoxia. Kilgannon and colleagues recently reported that patients administered high-concentration oxygen resulting in hyperoxia (PaO2 >300 mmHg) following cardiac arrest have increased in-hospital mortality, a finding they attributed to increased oxidative stress associated with hyperoxia [33]. However, because a subsequent study was unable to replicate these findings [34], randomized controlled trials will be required to resolve the clinical uncertainty.
Neonatal resuscitation is the clinical situation in which administration of 100% oxygen has most clearly been demonstrated to increase the risk of death [35, 36]. This has resulted in a radical change in practice whereby room air rather than oxygen is now the recommended resuscitation regime [36].
Considering the ubiquity of the administration of supplemental oxygen, there are surprisingly few randomized clinical trials that demonstrate its beneficial role when hypoxemia is absent. This may reflect the fact that its usage is so embedded in clinical practice that it is accepted as safe [2]. Nevertheless, there are some situations in which supplemental oxygen administration is useful: treatment of cluster headache [37], reducing the oxidative stress associated with colon surgery [38], and the prevention of desaturation during endoscopy [39, 40]. Supplemental oxygen administration can, however, have the unintended side effect of delaying recognition by oximetry of hypoventilation [41, 42]. Until recently many studies had indicated that supplementary oxygen reduced postoperative nausea and vomiting, but the current status is ambiguous (for example [43–46]). Similarly, oxygen was thought to reduce postsurgical infections - but more recent studies (see [47] for a partial summary) have cast doubt on the original findings. Moreover, ventilation with high inspired oxygen concentrations during surgery leads to subsequent impairment of pulmonary gas exchange [48–50] that may be of clinical significance [50]. Traumatic injury and compartment syndrome may appear to be obvious applications for supplementary oxygen - an increased PO2 would help overcome the reductions in perfusion - but hyperbaric rather than normobaric oxygen is the treatment of choice [51–53]. Oxygen is used for the treatment of carbon monoxide poisoning [54], but this is probably less effective than it should be if the accompanying hypocapnia is not prevented [26]. In the case of breathlessness, which has long been treated with supplementary oxygen, a recent randomized double-blind controlled trial established that nasal oxygen was no better than air in relieving breathlessness and improving quality of life in palliative care patients with refractory breathlessness [55].
In conclusion, NASA managers demanded in 1986 that their counterparts at Martin-Thiokol prove that it was not safe to launch the Space Shuttle Challenger despite concerns expressed by engineers about the integrity at low temperatures of the O-rings joining the segments of the solid rocket boosters [56]. The correct question would have been: can you prove that it is safe? In the case of supplementary oxygen, failure to ask the right question reinforces complacency about its use in patients who may have regional hypoxia or ischemia but are not hypoxemic.
Abbreviations
- CaO2:
-
arterial blood oxygen content
- DO2:
-
oxygen delivery
- PaCO2:
-
arterial partial pressure of carbon dioxide
- PaO2:
-
arterial partial pressure of oxygen
- PCO2:
-
partial pressure of carbon dioxide
- PO2:
-
partial pressure of oxygen.
References
Campbell EJM: Foreword. In Acute Respiratory Failure in Chronic Obstructive Pulmonary Disease. Edited by: Derenne J-P, Whitelaw WA, Similowski T. New York: Marcel Dekker; 1996:v-vi.
Burls A, Emparanza JI, Quinn T, Cabello JB: Oxygen use in acute myocardial infarction: an online survey of health professionals' practice and beliefs. Emerg Med J 2010, 27: 283-286. 10.1136/emj.2009.077370
Forkner IF, Piantadosi CA, Scafetta N, Moon RE: Hyperoxia-induced tissue hypoxia: a danger? Anesthesiology 2007, 106: 1051-1055. 10.1097/01.anes.0000265167.14383.44
Johnston AJ, Steine LA, Gupta AK, Menon DK: Cerebral oxygen vasoreactivity and cerebral tissue oxygen reactivity. Br J Anaesth 2003, 90: 774-786. 10.1093/bja/aeg104
Floyd TF, Clark JM, Gelfand R, Detre JA, Ratcliffe S, Guvakov D, Lambertsen CJ, Eckenhoff RG: Independent cerebral vasoconstrictive effects of hyperoxia and accompanying arterial hypocapnia at 1 ATA. J Appl Physiol 2003, 95: 2453-2461.
Adams HP Jr, del Zoppo G, Alberts MJ, Bhatt DL, Brass L, Furlan A, Grubb RL, Higashida RT, Jauch EC, Kidwell C, Lyden PD, Morgenstern LB, Qureshi AI, Rosenwasser RH, Scott PA, Wijdicks EF: Guidelines for the early management of adults with ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council, Clinical Cardiology Council, Cardiovascular Radiology and Intervention Council, and the Atherosclerotic Peripheral Vascular Disease and Quality of Care Outcomes in Research Interdisciplinary Working Groups: the American Academy of Neurology affirms the value of this guideline as an educational tool for neurologists. Circulation 2007, 115: e478-e534. 10.1161/CIRCULATIONAHA.107.181486
Singhal AB, Benner T, Roccatagliata L, Koroshetz WJ, Schaefer PW, Lo EH, Buonanno FS, Gonzalez RG, Sorensen AG: A pilot study of normobaric oxygen therapy in acute ischemic stroke. Stroke 2005, 36: 797-802. 10.1161/01.STR.0000158914.66827.2e
Ronning OM, Guldvog B: Should stroke victims routinely receive supplemental oxygen? A quasi-randomized controlled trial. Stroke 1999, 30: 2033-2037. 10.1161/01.STR.30.10.2033
Farquhar H, Weatherall M, Wijesinghe M, Perrin K, Ranchord A, Simmonds M, Beasley R: Systematic review of studies of the effect of hyperoxia on coronary blood flow. Am Heart J 2009, 158: 371-377. 10.1016/j.ahj.2009.05.037
Bodetoft S, Carlsson M, Arheden H, Ekelund U: Effects of oxygen inhalation on cardiac output, coronary blood flow and oxygen delivery in healthy individuals, assessed with MRI. Eur J Emerg Med 2011, 18: 25-30. [Epub ahead of print] 10.1097/MEJ.0b013e32833a295e
Russek HI, Regan FD, Naegele CF: One hundred percent oxygen in the treatment of acute myocardial infarction and severe angina pectoris. J Am Med Assoc 1950, 144: 373-375.
Bourassa MG, Campeau L, Bois MA, Rico O: The effects of inhalation of 100 percent oxygen on myocardial lactate metabolism in coronary heart disease. Am J Cardiol 1969, 24: 172-177. 10.1016/0002-9149(69)90400-7
Rawles JM, Kenmure AC: Controlled trial of oxygen in uncomplicated myocardial infarction. Br Med J 1976, 1: 1121-1123. 10.1136/bmj.1.6018.1121
O'Driscoll BR, Howard LS, Davison AG: BTS guideline for emergency oxygen use in adult patients. Thorax 2008, 63: vi1-vi68. 10.1136/thx.2008.102947
Conti CR: Oxygen therapy-use and abuse in acute myocardial infarction patients. Clin Cardiol 2009, 32: 480-481. 10.1002/clc.20678
Antman EM, Anbe DT, Armstrong PW, Bates ER, Green LA, Hand M, Hochman JS, Krumholz HM, Kushner FG, Lamas GA, Mullany CJ, Ornato JP, Pearle DL, Sloan MA, Smith SC Jr: ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction - executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to revise the 1999 guidelines for the management of patients with acute myocardial infarction). J Am Coll Cardiol 2004, 44: 671-719. 10.1016/j.jacc.2004.07.002
Chest Pain of Recent Onset: Assessment and Diagnosis of Recent Onset Chest Pain or Discomfort of Suspected Cardiac Origin[http://www.nice.org.uk/nicemedia/live/12947/47931/47931.pdf]
Diringer MN: Hyperoxia: good or bad for the injured brain? Curr Opin Crit Care 2008, 14: 167-171. 10.1097/MCC.0b013e3282f57552
Rousseau A, Tesselaar E, Henricson J, Sjoberg F: Prostaglandins and radical oxygen species are involved in microvascular effects of hyperoxia. J Vasc Res 2010, 47: 441-450. 10.1159/000282667
Mak S, Egri Z, Tanna G, Colman R, Newton GE: Vitamin C prevents hyperoxia-mediated vasoconstriction and impairment of endothelium-dependent vasodilation. Am J Physiol Heart Circ Physiol 2002, 282: H2414-H2421.
McNulty PH, King N, Scott S, Hartman G, McCann J, Kozak M, Chambers CE, Demers LM, Sinoway LI: Effects of supplemental oxygen administration on coronary blood flow in patients undergoing cardiac catheterization. Am J Physiol Heart Circ Physiol 2005, 288: H1057-H1062.
Yamazaki F: Hyperoxia attenuates endothelial-mediated vasodilation in the human skin. J Physiol Sci 2007, 57: 81-84. 10.2170/physiolsci.SC011006
Zhilyaev SYu, Moskvin AN, Platonova TF, Gutsaeva DR, Churilina IV, Demchenko IT: Hyperoxic vasoconstriction in the brain is mediated by inactivation of nitric oxide by superoxide anions. Neurosci Behav Physiol 2003, 33: 783-787. 10.1023/A:1025145331149
Dean JB, Mulkey DK, Henderson RA, Potter SJ, Putnam RW: Hyperoxia, reactive oxygen species, and hyperventilation: oxygen sensitivity of brain stem neurons. J Appl Physiol 2004, 96: 784-791.
Iscoe S, Fisher JA: Hyperoxia-induced hypocapnia: an underappreciated risk. Chest 2005, 128: 430-433. 10.1378/chest.128.1.430
Rucker J, Tesler J, Fedorko L, Takeuchi A, Mascia L, Vesely A, Slutsky AS, Volgyesi GA, Iscoe S, Fisher JA: Normocapnia improves cerebral O 2 delivery during conventional O 2 therapy in CO-exposed subjects. Ann Emerg Med 2002, 40: 611-618. 10.1067/mem.2002.129723
Ashkanian M, Borghammer P, Gjedde A, Østergaard L, Vafaee M: Improvement of brain tissue oxygenation by inhalation of carbogen. Neuroscience 2008, 156: 932-938. 10.1016/j.neuroscience.2008.08.016
Wise RG, Pattinson KT, Bulte DP, Chiarelli PA, Mayhew SD, Balanos GM, O'Connor DF, Pragnell TR, Robbins PA, Tracey I, Jezzard P: Dynamic forcing of end-tidal carbon dioxide and oxygen applied to functional magnetic resonance imaging. J Cereb Blood Flow Metab 2007, 27: 1521-1532. 10.1038/sj.jcbfm.9600465
Slessarev M, Han J, Mardimae A, Prisman E, Preiss D, Volgyesi G, Ansel C, Duffin J, Fisher JA: Prospective targeting and control of end-tidal CO 2 and O 2 concentrations. J Physiol 2007, 581: 1207-1219. 10.1113/jphysiol.2007.129395
Austin MA, Wills KE, Blizzard L, Walters EH, Wood-Baker R: Effect of high flow oxygen on mortality in chronic obstructive pulmonary disease patients in prehospital setting: randomised controlled trial. BMJ 2010, 341: c5462. 10.1136/bmj.c5462
O'Driscoll BR, Beasley R: Avoidance of high concentration oxygen in chronic obstructive pulmonary disease. BMJ 2010, 341: c5549. 10.1136/bmj.c5549
de Jonge E, Peelen L, Keijzers P, Joore H, de Lange D, van der Voort P, Bosman R, de Waal R, Wesselink R, de Keizer N: Association between administered oxygen, arterial partial oxygen pressure and mortality in mechanically ventilated intensive care unit patients. Crit Care 2008, 12: R156. 10.1186/cc7150
Kilgannon JH, Jones AE, Shapiro NI, Angelos MG, Milcarek B, Hunter K, Parrillo JE, Trzeciak S: Association between arterial hyperoxia following resuscitation from cardiac arrest and in-hospital mortality. JAMA 2010, 303: 2165-2171. 10.1001/jama.2010.707
Bellomo R, Bailey M, Eastwood GM, Nichol A, Pilcher D, Hart GK, Reade MC, Egi M, Cooper DJ, the Study of Oxygen in Critical Care (SOCC) Group: Arterial hyperoxia and in-hospital mortality after resuscitation from cardiac arrest. Crit Care 2011, 15: R90. 10.1186/cc10090
Saugstad OD, Ramji S, Soll RF, Vento M: Resuscitation of newborn infants with 21% or 100% oxygen: an updated systematic review and meta-analysis. Neonatology 2008, 94: 176-182. 10.1159/000143397
Saugstad OD: Resuscitation of newborn infants: from oxygen to room air. Lancet 2010, 376: 1970-1971. 10.1016/S0140-6736(10)60543-0
Bennett MH, French C, Schnabel A, Wasiak J, Kranke P: Normobaric and hyperbaric oxygen therapy for migraine and cluster headache. Cochrane Database Syst Rev 2008, 3: CD005219.
Garcia de la Asuncion J, Belda FJ, Greif R, Barber G, Vina J, Sastre J: Inspired supplemental oxygen reduces markers of oxidative stress during elective colon surgery. Br J Surg 2007, 94: 475-477. 10.1002/bjs.5497
al-Qorain A, du-Gyamfi Y, Larbi EB, al-Shedokhi F: The effect of supplemental oxygen in sedated and unsedated patients undergoing upper gastrointestinal endoscopy. J Int Med Res 1993, 21: 165-170.
Crantock L, Cowen AE, Ward M, Roberts RK: Supplemental low flow oxygen prevents hypoxia during endoscopic cholangiopancreatography. Gastrointest Endosc 1992, 38: 418-420. 10.1016/S0016-5107(92)70468-4
Fu ES, Downs JB, Schweiger JW, Miguel RV, Smith RA: Supplemental oxygen impairs detection of hypoventilation by pulse oximetry. Chest 2004, 126: 1552-1558. 10.1378/chest.126.5.1552
Beasley R, Aldington S, Robinson G: Is it time to change the approach to oxygen therapy in the breathless patient? Thorax 2007, 62: 840-841. 10.1136/thx.2006.068866
McKeen DM, Arellano R, O'Connell C: Supplemental oxygen does not prevent postoperative nausea and vomiting after gynecological laparoscopy. Can J Anaesth 2009, 56: 651-657. 10.1007/s12630-009-9136-4
Purhonen S, Niskanen M, Wustefeld M, Hirvonen E, Hynynen M: Supplemental 80% oxygen does not attenuate post-operative nausea and vomiting after breast surgery. Acta Anaesthesiol Scand 2006, 50: 26-31. 10.1111/j.1399-6576.2005.00866.x
Sadrolsadat SH, Shoroghi M, Farahbakhsh F, Moharreri RS, Sheikhvatan M, Abbasi A: The effect of supplemental 70% oxygen on postoperative nausea and vomiting in patients undergoing inguinal hernia surgery. Hernia 2008, 12: 167-171. 10.1007/s10029-007-0303-7
Turan A, Apfel CC, Kumpch M, Danzeisen O, Eberhart LH, Forst H, Heringhaus C, Isselhorst C, Trenkler S, Trick M, Vedder I, Kerger H: Does the efficacy of supplemental oxygen for the prevention of postoperative nausea and vomiting depend on the measured outcome, observational period or site of surgery? Anaesthesia 2006, 61: 628-633. 10.1111/j.1365-2044.2006.04703.x
Rothen HU: Oxygen: avoid too much of a good thing! Eur J Anaesthesiol 2010, 27: 493-494. 10.1097/EJA.0b013e3283396360
Zoremba M, Dette F, Hunecke T, Braunecker S, Wulf H: The influence of perioperative oxygen concentration on postoperative lung function in moderately obese adults. Eur J Anaesthesiol 2010, 27: 501-507.
Register SD, Downs JB, Stock MC, Kirby RR: Is 50% oxygen harmful? Crit Care Med 1987, 15: 598-601. 10.1097/00003246-198706000-00012
Sinha PK, Neema PK, Unnikrishnan KP, Varma PK, Jaykumar K, Rathod RC: Effect of lung ventilation with 50% oxygen in air or nitrous oxide versus 100% oxygen on oxygenation index after cardiopulmonary bypass. J Cardiothorac Vasc Anesth 2006, 20: 136-142. 10.1053/j.jvca.2005.11.017
Greensmith JE: Hyperbaric oxygen therapy in extremity trauma. J Am Acad Orthop Surg 2004, 12: 376-384.
Garcia-Covarrubias L, McSwain NE Jr, Van Meter K, Bell RM: Adjuvant hyperbaric oxygen therapy in the management of crush injury and traumatic ischemia: an evidence-based approach. Am Surg 2005, 71: 144-151.
Sahni T, Singh P, John MJ: Hyperbaric oxygen therapy: current trends and applications. J Assoc Physicians India 2003, 51: 280-284.
Weaver LK: Clinical practice. Carbon monoxide poisoning. N Engl J Med 2009, 360: 1217-1225. 10.1056/NEJMcp0808891
Abernethy AP, McDonald CF, Frith PA, Clark K, Herndon JE II, Marcello J, Young IH, Bull J, Wilcock A, Booth S, Wheeler JL, Tulsky JA, Crockett AJ, Currow DC: Effect of palliative oxygen versus room air in relief of breathlessness in patients with refractory dyspnoea: a double-blind, randomised controlled trial. Lancet 2010, 376: 784-793. 10.1016/S0140-6736(10)61115-4
Report of the Presidential Commission on the Space Shuttle Challenger Accident[http://science.ksc.nasa.gov/shuttle/missions/51-l/docs/rogers-commission/table-of-contents.html]
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
SI and JAF have participated in the development of devices suitable for increasing the efficiency of oxygen delivery. The protection of the related intellectual property and distribution of income from sales (if any) follow the guidelines set by the University Health Network.
Rights and permissions
About this article
Cite this article
Iscoe, S., Beasley, R. & Fisher, J.A. Supplementary oxygen for nonhypoxemic patients: O2 much of a good thing?. Crit Care 15, 305 (2011). https://doi.org/10.1186/cc10229
Published:
DOI: https://doi.org/10.1186/cc10229