Abstract
Introduction
Mammographically dense breast tissue is a strong predictor of breast cancer risk, and is influenced by both mitogens and mutagens. One enzyme that is able to affect both the mitogenic and mutagenic characteristics of estrogens is cytochrome P450 1A2 (CYP1A2), which is principally responsible for the metabolism of 17β-estradiol.
Methods
In a cross-sectional study of 146 premenopausal and 149 postmenopausal women, we examined the relationships between CYP1A2 activity, malondialdehyde (MDA) levels, and mammographic density. In vivo CYP1A2 activity was assessed by measuring caffeine metabolites in urine. Levels of serum and urinary MDA, and MDA–deoxyguanosine adducts in DNA were measured. Mammograms were digitized and measured using a computer-assisted method.
Results
CYP1A2 activity in postmenopausal women, but not in premenopausal women, was positively associated with mammographic density, suggesting that increased CYP1A2 activity after the menopause is a risk factor for breast cancer. In premenopausal women, but not in postmenopausal women, CYP1A2 activity was positively associated with serum and urinary MDA levels; there was also some evidence that CYP1A2 activity was more positively associated with percentage breast density when MDA levels were high, and more negatively associated with percentage breast density when MDA levels were low.
Conclusion
These findings provide further evidence that variation in the activity level of enzymes involved in estrogen metabolism is related to levels of mammographic density and potentially to breast cancer risk.
Similar content being viewed by others
Introduction
Increased amounts of stromal and epithelial tissue in the breast is a strong independent risk factor for breast cancer, and they appear as light areas on a mammogram because they are radiologically dense. These areas are referred to as 'mammographic density'. In contrast, fat appears dark on a mammogram because it is radiologically lucent [1].
Like breast cancer, epidemiologic evidence for breast density suggests that endocrine factors play a role [1]. Mammographic density levels decline with increasing age, onset of menopause, increasing body weight and parity, and younger age at first childbirth [1]. Density levels increase with hormone replacement therapy [2], and are reduced with tamoxifen [3] and a gonadotrophin release agonist [4].
In addition to mitogens, mammographic density may also be influenced by mutagens. Relationships between mammographic density and the mutagen malondialdehyde (MDA), an end product of lipid peroxidation, have been observed in two studies [5, 6], suggesting that breast density levels are also affected by mutagenic events that can lead to DNA damage [7, 8]. and increased cell proliferation [9]. The main DNA adduct is malondialdehyde–deoxyguanosine (dG-MDA), and this and other MDA adducts are twofold to threefold greater in breast tissue from patients with breast cancer than in breast tissue from those without breast cancer [10]. Increased levels of circulating MDA have also been detected in breast cancer patients compared with noncancer patients [11].
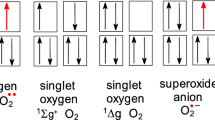
Of human P450s that are capable of oxidizing estradiol, cytochrome P450 1A2 (CYP1A2) has the highest catalytic activity, resulting in the production of 2-hydroxy and 4-hydroxy metabolites. The absolute level of 2-hydroxylation of estrone, which is mediated by CYP1A2, is six to seven times greater than the extent of 4-hydroxylation mediated by this enzyme [12]. Although CYP1A2 is a hepatic enzyme that is not expressed in the breast, it can potentially affect circulating estrogen levels. Circulating sex hormone levels, in turn, have been shown in prospective studies of postmenopausal women to be associated with future risk for developing breast cancer [13]. Differences in CYP1A2 mRNA levels in human liver have also been reported, and it has been suggested that these differences in CYP1A2 expression may play a role in various cancers [14, 15]. Figure 1 shows the estrogen metabolites resulting from CYP1A2 function and how these metabolites may potentially have an impact on breast density levels [16]. Of these metabolites, 4-hydroxyestrogens are known to be estrogenic and are thought to be carcinogenic. Most studies agree, however, that 2-hydroxyestrogens are not dangerous because the metabolite is nonestrogenic and has been determined to be non-tumorigenic in animal models [17]. Catecholestrogens can contribute to carcinogenesis by becoming a source of reactive oxygen species and entering into redox cycling (i.e. repeated cycles of oxidation and reduction between catechol and quinone estrogens). In particular, 4-hydroxyestrogens can become a source of potentially genotoxic and cytotoxic reactive oxygen species [16, 18] because they can be oxidized by numerous enzymes into compounds called 3, 4-semiquinones and 3, 4-quinones. These compounds are highly reactive and can bind to DNA to create depurinating adducts that induce gene mutations and may lead to tumor initiation. The 2-catecholestrogens, in contrast, are oxidized to form predominantly stable DNA adducts, which remain in DNA unless they are removed by repair processes [18].
Estrogen metabolism by cytochrome P450 1A2 (CYP1A2) and its postulated effects on catecholestrogen levels and mammographic density. aCYP1A2 is principally responsible for metabolizing 17β-estradiol after an initial conversion to estrone. The enzyme is primarily involved in 2- and 4-hydroxylations. bIn humans, between 40% and 50% of estrogens undergo 2-hydroxylation whereas 5–8% undergo 4-hydroxylation. cCatecholestrogens are deactivated by catechol-O-methyltransferase (COMT). dCatecholestrogens can potentially affect breast density levels through estrogen-receptor mediated mechanisms and/or oxidative mechanisms. 2-Hydroxyestrogens are nonestrogenic and nontumorigenic, but can be oxidized to form predominantly stable DNA adducts. 4-Hydroxyestrogens are estrogenic and carcinogenic. They form potentially genotoxic and cytotoxic reactive oxygen species (ROS) that can bind to DNA to create depurinating adducts. ROS can also participate in lipid peroxidation to create the mutagen malondialdehyde (MDA), which is a risk factor for mammographic density. These mechanisms are postulated to be inhibitory (-) or stimulatory (+) for development of mammographic density.
The goals of the present cross-sectional study of premenopausal and postmenopausal women were to determine whether CYP1A2 activity is associated with mammographic density, whether CYP1A2 activity is related to MDA levels (serum, urinary, and dG-MDA), and whether MDA levels are associated with breast density.
Methods
The methods for this study are published in detail elsewhere [19] and are only briefly described here. Ethical approval for the study protocol was given by the Human Subjects Review Committee at the University of Toronto, Canada.
Source of study subjects
Between 1994 and 1997, potential participants were identified from the mammographic units of Mount Sinai, Women's College, and St. Michael's Hospital in Toronto. The extent of mammographic density for all patients was visually estimated by a radiologist and expressed as a percentage of breast area on a five-point scale. The number of patients recruited into each of the five categories of radiological density were as follows: <10%, n = 101; 10% to <25%, n = 62; 25% to <50%, n = 60; 50% to <75%, n = 60; and ≥ 75%, n = 99.
Recruitment
Potential participants were sent a letter and subsequently telephoned about the study. Premenopausal women were eligible if they were menstruating regularly, not pregnant or breast-feeding, and had not had a hysterectomy or oophorectomy. Postmenopausal women were eligible if they had spontaneous amenorrhea for at least 12 months, or had had a hysterectomy and were 50 years of age or older, or had had a bilateral oophorectomy at any age. A woman was excluded if she was taking any type of exogenous hormone preparation, had breast augmentation or reduction, or had a personal history of breast cancer or was being investigated for breast cancer. In total, 382 women agreed to participate in the study, representing 88% of those who were contacted and found to be eligible.
Measurements
Blood samples were collected after a 12-hour overnight fast, and during the luteal phase of the menstrual cycle (days 20–24) for premenopausal women. The mammogram closest to the time of the blood draw was used (mean difference 32 weeks). Twenty-four hour urine samples were also collected.
Obtaining consent for the phenotyping study
Because examination of CYP1A2 activity in relation to mammographic density was not a goal of the original study, patients were subsequently mailed a letter describing the goals of the phenotypic component of this study, and written consent was obtained to phenotype CYP1A2 activity. Information on ethnicity was also obtained at this time. Of 382 eligible women (193 premenopausal and 189 postmenopausal), 357 (93%) gave consent. Eight women could not be contacted because they had moved and could not be traced through either telephone directories or their physicians. Sixteen women were nonresponders after a minimum of four telephone reminders, and one did not provide consent.
Of the 357 women, 40 (11.2%; 29 premenopausal and 11 postmenopausal) did not have urine samples and 22 (6.2%; seven premenopausal and 15 postmenopausal) had insufficient excretion of caffeine metabolites for estimating CYP1A2 activity, leaving 146 postmenopausal and 149 postmenopausal women in whom CYP1A2 activity was measurable. This represented 93% of women with urine samples and 82% of eligible women who provided consent. The overall participation rate for this portion of the study was 77% (295/382).
Ethnicity
By questionnaire, each participant was asked their country of birth as well as the countries of birth for each of their parents and grandparents. They were also asked the question, 'What is your ethnic or cultural background?' and were given instructions to mark all appropriate categories. They were classified as follows: black; white (e.g. British, French, European, Latin/South American of European background); native/aboriginal people of North America (North American Indian, Inuit, Métis); East Asian (e.g. Chinese, Japanese, Korean, Vietnamese); South Asian (e.g. Indian from India, Pakistani, Punjabi, Tamil); other, with specification; and 'don't know'. Because of low numbers in groups other than Caucasians, the categories were collapsed and described as Caucasian (white), East Asians, Jewish, and other.
Epidemiologic and anthropometric data
Information about epidemiologic risk factors for breast density and breast cancer was collected by questionnaire, and dietary information was obtained using a list-based food frequency questionnaire developed by Block and coworkers [20]. Each woman was weighed and measured for height, and waist and hip circumference.
CYP1A2 activity
Caffeine (1, 3, 7-trimethylxanthine) is metabolized by CYP1A2 and has been used to evaluate CYP1A2 activity in vivo [21]. The best urinary metabolic ratio appears to be [5-acetylamino-6-formylamino-3-methyluracil (AFMU) + 1-methylurate (1U) + 1-methylxanthine (1X)]/1,7-dimethylurate (1, 7U), which is referred to as the caffeine metabolic ratio (CMR) [22]. The CMR is not dependent on renal flow [23], and is based only on metabolic end products of caffeine metabolism, thus making the amount and timing of urine collection relatively unimportant [24]. Measurement of the CMR in 24-hour urine samples has been shown to be a viable method for assessing CYP1A2 intake in populations with widespread caffeine use [25]. In the present study, 93% of women consumed sufficient levels of caffeine to estimate CMR. Because daily caffeine intake is relatively constant, urinary recovery of caffeine metabolites over a 24-hour period reflects CMRs observed with standardized dosing [25].
Urinary caffeine metabolites were measured by HPLC as previously described [21], except for a modification of the composition of the mobile phase. The mobile phase was composed of 1.3% isopropanol, 0.2% isonitrile, and 0.1% phosphoric acid. The caffeine metabolites were eluted at 1 ml/min and detected by ultraviolet absorbance (0.05) at 280 nm. The retention times of 1U, 1X and 1, 7U and the internal standard (N-acetyl-p-aminophenol) were 9.9, 11.9, 29.8, and 14.2 min, respectively.
Urinary AFMU was first deformylated to stable 5-acetylamino-6-amino-3-methyluracil (AAMU) and then measured using the HPLC method reported by Tang and coworkers [21]. The mobile phase consisted of 0.075% acetic acid and 0.075% phosphoric acid. AAMU and the internal standard (hydrobenzyl alcohol) were eluted at a flow of 0.9 ml/min and monitored by ultraviolet absorbance (0.04) at 263 nm. The retention times of AAMU and the internal standard were 13 and 36 min, respectively.
A standard urine sample with known caffeine metabolite concentrations was analyzed across all days of sample analyses with an interassay coefficient of variation of 9%. Accuracy of the CYP1A2 measurement did not vary with caffeine intake. After adjustment for smoking status, age, body mass index (BMI), waist–hip ratio (WHR), and ethnicity, coefficients of variation associated with mean CYP1A2 function across quartiles of caffeine intake were 56.8%, 55.3%, 57.0%, and 46.9% for premenopausal women, and 39.8%, 44.1%, 43.5%, and 42.4% for postmenopausal women. Kashuba and coworkers [26] investigated the intraindividual variability in CYP1A2 activity over a 3-month period and the median coefficient of variation was 16.8% (range 4.5–49.3%).
Serum antioxidants
Serum levels of α-tocopherol, retinol, and five commonly reported carotenoids (α- and β-carotene, lutein, lycopene and cryptoxanthin) were extracted using hexane and analyzed by reverse phase HPLC, C18 column, and absorbance detector. Peaks were identified and quantified by using their respective standards [27].
Serum MDA, urinary MDA, dG-MDA adducts
MDA in serum and urine was measured in triplicate by HPLC determination of thiobarbituric acid derivatives, as described by Bird and coworkers [28]. The sample was extracted with trichloroacetic acid and then heated with thiobarbituric acid. The thiobarbituric acid–MDA complex was separated using HPLC and the absorbance measured at 535 nm. Total urinary MDA level excreted over a 24-hour period was calculated as concentration of urinary MDA multiplied by total urinary volume collected. Study results with total urinary MDA were similar to those obtained when total urinary MDA levels were expressed per millimole creatinine. Results shown here are those obtained with total urinary MDA levels unadjusted for creatinine.
Precipitated DNA was treated with RNase A and RNase T1 to remove RNA contamination. Isolated DNA was hydrolyzed using nuclease P1 and alkaline phosphatase, and the amount of dG-MDA adducts were determined by reverse-phase HPLC, C18 column, and fluorescence detection (340 nm excitation, 518 nm emission) using 30% as the mobile phase, as previously described [29].
Serum estradiol
Serum estradiol levels in premenopausal women were measured at the London Regional Cancer Center in Ontario, Canada in the laboratory of Geoffrey Hammond [30]. Serum estradiol levels in postmenopausal women were measured by Esoterix Center for Clinical Trials (Calabasas Hills, California, USA) [19].
Mammographic density
Breast density measurements were made using a randomly selected, craniocaudal (viewing from above, down) mammographic view of one breast from each woman. Mammograms were digitized using a Lumisys model 85 (Eastman Kodak Company, Rochester, NY, USA) and randomly ordered for analysis. The observer (NFB) selected a threshold gray value to separate the image of the breast from the background. A second threshold was selected to identify the edges of regions representative of radiographically dense tissue. Summation of pixels within these areas gave a measure of the area of density in the breast. The percentage of radiographic density is the area of dense tissue divided by the entire projected area of the breast multiplied by 100. Further details of this method are given elsewhere [31].
Statistical methods
Data analyses were carried out using the SAS statistical software package (version 6.12; SAS Institute Inc., Cary, NC, USA) [32]. Data were inspected for normality and, when necessary, transformed to approximate a normal distribution. This included square root transformation of percentage breast density, and natural log transformation of CYP1A2 activity, BMI, and MDA levels. Because of differences in results between premenopausal and postmenopausal women, all data are presented stratified by menopausal status.
Partial correlations were used to control for potential confounders when relationships between serum, urinary, and dG-MDA levels were assessed.
Relationships between CYP1A2 phenotype, MDA levels, and breast density were assessed using multiple regression analysis. For descriptive purposes, relationships across quartiles were also provided with a test for trend. Although these results are based on analyses of transformed data, they are presented in their original units with 95% confidence intervals. Age, BMI, WHR, ethnicity, and smoking status were included in all models unless indicated. Age and body size were included as potential confounders because increased oxidant status and lipid peroxidation is related to advancing age, central obesity, hyperinsulinemia, insulin resistance, dyslipidemia, and blood glucose [33–36]. In the present study, serum MDA levels were positively associated with BMI measurements in both premenopausal and postmenopausal women (P ≤ 0.005). Age and body size are also important determinants of breast density levels [1]. Adjustments were made for smoking status because tobacco smoke is inversely associated with mammographic density [37] and is a known inducer of CYP1A2 activity [38]. Associations between CYP1A2 and MDA levels, as well as associations between MDA levels and mammographic density, were further adjusted for serum antioxidant levels.
To illustrate interactions between CYP1A2 activity and MDA levels (i.e. two continuous variables) on percentage density, relationships (simple slopes) between CYP1A2 activity and percentage density were determined for (conditional on) three levels of oxidative stress: at mean level, at one standard deviation above the mean, and one standard deviation below the mean [39].
Of 295 women with CYP1A2 results, 251 (85%) were non-Jewish Caucasians, 10 were East Asians, 15 were Jewish, and 19 were from other ethnic groups. To assess the possibility that ethnicity may be a potential confounder of findings, all analyses were performed on the 295 women with CYP1A2 results, with and without adjustment for ethnicity. All analyses were then repeated with only the 251 non-Jewish Caucasians. Findings from all three sets of analyses were similar, suggesting that ethnicity was not a strong confounder in the study. Results shown in this report are those performed on the 295 women with adjustment for ethnicity.
Results
Study subject characteristics
There were 146 premenopausal and 149 postmenopausal women with CYP1A2 phenotype data, for whom selected characteristics are shown in Table 1. Of the participants 85% were Caucasian, 3.4% were East Asian, 5.1% were Jewish, and 6.4% were from other ethnic groups. The mean age was 45 years in premenopausal and 56 years in postmenopausal women. The two groups were similar in age at menarche, age at first birth, and total number of livebirths. Postmenopausal women were slightly heavier, with higher average BMI and WHR. They also had lower levels of percentage mammographic density, and higher serum and urinary MDA levels.
Compared with Caucasians, premenopausal and postmenopausal East Asian women and premenopausal Jewish women were lighter, with lower mean BMIs and greater levels of percentage breast density. Among premenopausal women, East Asians had higher levels of urinary MDA than did Caucasians. In postmenopausal women, compared with Caucasians, East Asians were older at age of first birth, and had higher levels of CYP1A2 activity and urinary MDA. Jewish women had lower CYP1A2 activity than did Caucasians.
In premenopausal women, those without CYP1A2 data had higher urinary MDA levels than did those with phenotype data. In postmenopausal women, those without CYP1A2 results weighed less, and had lower mean BMI and urinary MDA levels. Percentage density was on average 14% higher in these patients than in women with CYP1A2 results.
CYP1A2 activity
The CMR in premenopausal women ranged from 0.8 to 23.5, with a mean ± standard deviation of 6.2 ± 2.9 and a median of 5.8. In postmenopausal women the ratio ranged from 1.8 to 17.1, with a mean ± standard deviation of 5.9 ± 2.3, and median of 5.4. This magnitude of interindividual variation is similar to those in previous reports showing up to a 30-fold variation in enzyme activity [40, 41]).). The population distribution of CMR in the present study was log-normal, which is similar to findings of other studies using the same urinary ratio [25, 38, 40, 41].
MDA measures
Postmenopausal women had higher serum (F = 18.08, P < 0.0001) and urinary (F = 24.05, P < 0.0001) MDA levels than did premenopausal women, but dG-MDA levels were not different between the two groups (P = 0.41). These findings were not altered when further adjusted for age, BMI, and WHR. The coefficient of variation associated with each MDA measure (untransformed values) was higher in premenopausal than in postmenopausal women (41.4 versus 37.0 for serum MDA; 52.1 versus 44.6 for urinary MDA; and 76.2 versus 56.0 for dG-MDA).
In premenopausal women, serum and urinary MDA levels were weakly correlated before (r = 0.15, P = 0.08) and after (r = 0.21, P = 0.02) adjustment for age, BMI, and WHR. Neither measure, however, was correlated with dG-MDA levels (P > 0.28). In postmenopausal women, serum MDA levels were positively associated with urinary (r = 0.17, P = 0.03) and dG-MDA (r = 0.17, P = 0.04) levels. After adjustment for age, BMI, and WHR, serum MDA continued to be associated with dG-MDA (r = 0.19, P = 0.02), but it was only weakly associated with urinary MDA levels (r = 0.14, P = 0.09). Urinary and dG-MDA levels were not correlated (P ≥ 0.13).
CYP1A2 activity and mammographic density
Relationships between CYP1A2 activity and percentage mammographic density levels are shown in Table 2. Results were initially adjusted for age, ethnicity, and smoking. Findings were then further adjusted for total estrogen levels to determine whether CYP1A2 function was independently associated with breast density levels without the influence of estrogen. Finally, findings were further adjusted for age at menarche, age at menopause (in postmenopausal women only), number of livebirths, BMI, WHR, family history of breast cancer, and smoking status.
CMR, as an indicator of CYP1A2 activity, was not related to percentage density in premenopausal women after adjustment for age, ethnicity, and smoking (P = 0.58), total estrogen (P = 0.49), and other common covariates (P = 0.68). In contrast, CMR in postmenopausal women was positively related to percentage breast density after adjustment for age, ethnicity, and smoking (β = 1.57 ± 0.60, F = 6.89, P = 0.01) as well as total estrogen (β = 1.30 ± 0.64, F = 4.05, P = 0.05). The relationship was attenuated and no longer significant when further adjusted for other risk factors for breast density (β = 0.94 ± 0.64, F = 2.36, P = 0.13), although the P trend remained significant across quartiles of CMR (P = 0.05). The positive association between CMR and breast density was primarily due to a lower mean percentage density level in the first quartile of CMR.
CYP1A2 activity and malondialdehyde levels
Relationships between CYP1A2 activity and MDA levels are shown in Table 3. CYP1A2 activity was positively associated with serum (P = 0.03) and urinary (P = 0.04) MDA levels in premenopausal but not in postmenopausal women (P ≥ 0.58). These relationships in premenopausal women were not altered when further adjusted for serum levels of the antioxidants tocopherol, retinol, β-carotene, β-cryptoxanthin, lycopene, and lutein (serum MDA: P = 0.04; urinary MDA: P = 0.04). No relationships were observed between CYP1A2 activity and dG-MDA levels in either menopausal group before (P ≥ 0.34) or after adjustment (P ≥ 0.32) for serum antioxidant levels.
MDA levels and mammographic density
Relationships between MDA levels and percentage breast density are shown in Table 4. No associations were observed between serum, urinary, or dG-MDA levels and percentage breast density in either premenopausal or postmenopausal women after adjustment for age, ethnicity, BMI, WHR, and smoking status. Further adjustments for serum antioxidant levels did not alter these findings. However, in premenopausal and postmenopausal women combined, we observed a positive association between urinary MDA levels and percentage mammographic density when adjusted for age, ethnicity, weight (instead of BMI), WHR, smoking status, and menopausal status (β = 0.47 ± 0.22, F = 4.45, P = 0.04). With further adjustment for serum antioxidant levels, however, the relationship was no longer significant (β = 0.35 ± 0.23, F = 2.29, P = 0.13). The relationship was also attenuated slightly when height was further added to the model (β = 0.35 ± 0.22, F = 2.62, P = 0.11). If all women who participated in the original study were included, including those without CYP1A2 results, then the positive association observed between urinary MDA levels and breast density after adjustment for age, weight, smoking status, WHR, and menopausal status was significant (n = 335; β = 0.53 ± 0.22, F = 5.67, P = 0.02), even after adjustment for height (β = 0.44 ± 0.22, F = 3.97, P = 0.05), but not with further adjustment for serum antioxidant levels (β = 0.31 ± 0.23, F = 1.85, P = 0.18). Similarly, among all women there was a positive association between urinary MDA and breast density if adjustment was for waist circumference (the anthropometric variable most closely associated with breast density levels), smoking status, height, and menopausal status (β = 0.44 ± 0.22, F = 4.06, P = 0.04). The relationship was attenuated by further adjustment for serum antioxidant levels (β = 0.32 ± 0.22, F = 2.10, P = 0.15).
Interaction between CYP1A2 activity and MDA levels
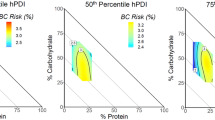
Although not originally hypothesized, we tested for possible interactions between CYP1A2 function and MDA levels with respect to mammographic density. Relationships between CYP1A2 activity and mammographic density according to MDA levels are shown in Fig. 2. Although not statistically significant, interactions in premenopausal women were suggested for urinary MDA (F = 2.14, P = 0.15) and dG-MDA adducts (F = 2.97, P = 0.09) after adjusting for age, ethnicity, BMI, WHR, and smoking status. The interaction between dG-MDA adducts and CYP1A2 activity was statistically significant if an adjustment was made for weight instead of BMI (F = 4.67, P = 0.03). This interaction was slightly attenuated if a further adjustment was made for height (F = 3.36, P = 0.07). For both MDA measures, the associations between CYP1A2 activity and breast density were more negative at low levels of MDA, and became more positive as MDA levels increased. At low dG-MDA adduct levels (illustrated at -1 standard deviation), for example, there was a negative nonsignificant relationship between CYP1A2 activity and percentage breast density (β = -0.77 ± 0.50, F = 2.36, P = 0.13). At mean MDA level CYP1A2 activity was not associated with breast density (β = -0.03 ± 0.40, F = 0.00, P = 0.95), and at high levels of dG-MDA (illustrated at +1 standard deviation) there was a positive nonsignficant association between CYP1A2 activity and breast density (β = 0.72 ± 0.66, F = 1.16, P = 0.28). A similar but nonsignificant (P = 0.29) pattern of interaction between CYP1A2 function and serum MDA levels were observed for postmenopausal women, although in the instance of urinary MDA the pattern was reversed. Those with lower MDA levels showed more positive associations between CYP1A2 function and breast density levels (P = 0.35).
Relationships between cytochrome P450 1A2 (CYP1A2) activity and percentage breast density according to (a) serum and (b) urinary malondialdehyde (MDA) levels, and (c) malondialdehyde–deoxyguanosine (dG-MDA) levels. All analyses are adjusted for age, ethnicity, body mass index (BMI), waist–hip ratio (WHR), and smoking status. Confounders were set at mean values and determined for Caucasian nonsmokers to illustrate relationships between CYP1A2 activity and percentage density according to MDA levels. Number of women in each group: premenopausal, n = 146 for serum MDA and n = 141 for urinary MDA and dG-MDA; and postmenopausal, n = 149 for serum and urinary MDA and n = 145 for dG-MDA. CMR, caffeine metabolic ratio.
Discussion
In premenopausal women, CYP1A2 activity, as estimated by the CMR, was not associated with breast density levels but was positively related to serum and urinary MDA levels. In postmenopausal women, higher CYP1A2 activity was consistently associated with higher levels of breast density, suggesting that increased CYP1A2 activity in this group is a risk factor for breast cancer. No associations, however, were observed between CYP1A2 activity and MDA levels.
In postmenopausal women, relationships were consistently positive between CYP1A2 activity and breast density levels. These observations are consistent with the findings of Riza and coworkers [42], who found that postmenopausal women with dense parenchymal breast patterns had 58% higher levels of 2-hydroxyestrone than did women with no density. Prospectively, however, both a higher [43] and a lower [44] ratio of 2-hydroxyestrone to 16α-hydroxyestrone have been associated with increased risk for breast cancer in postmenopausal women.
The positive relationship between CYP1A2 function and breast density levels in postmenopausal women was slightly attenuated by adjustment for total estradiol levels, but it remained statistically significant. This finding suggests that the relationship between CYP1A2 function and breast density is partially mediated by circulating estradiol levels, but that other factors are also important, such as catecholestrogens and other products of CYP1A2 activity. CYP1A2 is known to activate several heterocyclic and aromatic amine promutagens [15, 45, 46] as well as tobacco smoke-specific nitrosamines [47]. The enzyme is also inducible, and previous studies have shown variation in activity by sex, race, age, smoking status, body mass index, coffee and alcohol consumption, and exposure to various combustion products and contaminants [15, 38, 48–52].
Although CYP1A2 activity was not associated with breast density levels in premenopausal women, there was some evidence that the relationship may be modulated by oxidative burden. CYP1A2 activity was positively associated with breast density when urinary and dG-MDA levels were high and negatively associated when MDA levels were low. These relationships, however, did not reach statistical significance because of small sample size and the choice of confounders included in the statistical model. The interaction between dG-MDA adduct levels and CYP1A2 activity on breast density levels, for instance, was statistically significant when adjusted for weight instead of BMI.
An interaction between CYP1A2 activity and oxidative stress is biologically plausible because CYP1A2 metabolism of endogenous and exogenous substrates produce reactive oxygenated metabolites [53]. In premenopausal but not in postmenopausal women, we observed positive associations between CYP1A2 activity and serum and urinary MDA levels, as measures of lipid peroxidation. CYP1A2 function has also been positively associated with urinary excretion of 8-oxo-7,8-dihydro-2'-deoxyguanosine which is a biomarker of oxidative DNA damage [54–56].
In premenopausal women, the observed interaction between CYP1A2 activity and oxidative burden may result from competing consequences. Against a background of low oxidative burden, increased CYP1A2 function may reflect the advantages of estrogen inactivation [17], with attendant increases in reactive oxygen species being inactivated by protective antioxidant systems. Against a background of high oxidative stress, however, the disadvantages associated with further increases in pro-oxidant levels may outweigh the benefits of increased estradiol inactivation.
An association between urinary MDA levels and mammographic density has been reported in two separate studies [5, 6]. We, however, did not replicate the observation when premenopausal and postmenopausal women were considered separately [5]. This was due to our choice of confounders and to our limited sample size. A statistically significant association was observed when premenopausal and postmenopausal women were combined and results were adjusted for weight or waist circumference instead of BMI. The association was slightly attenuated by further adjustment for height as a potential confounder and remained significant if sample size was maximized to include all women in the original study. Further adjustments for serum antioxidant levels, however, attenuated these relationships.
The weak and null associations observed between MDA measures and breast density may be partly due to confounding by correlates of body size. Increased pro-oxidant activity is related to central obesity, hyperinsulinemia, insulin resistance, dyslipidemia, and blood glucose levels [33–36]. In this study, both serum and urinary MDA levels were positively associated with BMI and weight. BMI and WHR, however, are inversely associated with breast density levels [1]. Thus, MDA and mammographic density may seem inversely related if not properly adjusted for body size and its correlates. In our study, serum MDA levels after adjustment for age and ethnicity was inversely associated with mammographic density levels in both premenopausal (β = -1.07 ± 0.61, F = 3.08, P = 0.08) and postmenopausal (β = -1.29 ± 0.58, F = 5.02, P = 0.03) women. With further adjustments for body size (BMI and WHR) and smoking status, the relationship between MDA levels and breast density became more positive in both premenopausal (β = 0.57 ± 0.46, F = 1.52, P = 0.22) and postmenopausal (β = -0.33 ± 0.49, F = 0.47, P = 0.49) women, although neither was statistically significant.
Weak correlations between various MDA measurements may in part explain why these measures show different findings. This is consistent with previous observations that markers of oxidative DNA damage and lipid peroxidation may not be strongly correlated, and suggests that no single measure can be used as an indicator of in vivo oxidative stress [57]. MDA levels are determined by a number of factors apart from endogenous lipid peroxidation. Exogenous dietary intake, for instance, is estimated to represent 10–18% [58] and as high as 50–60% [59] of urinary MDA levels [60, 61], and is difficult to adjust for in data analysis because the MDA content of foods varies widely and is affected by lipid type, storage, and cooking methods. Regarding dG-MDA levels, it has recently been demonstrated that these adducts can be formed independently of lipid peroxidation through direct DNA oxidation [62]. Low correlations between dG-MDA levels and lipid peroxidation rates may also arise if MDA adduct levels are low enough for complete repair [63], and it has further been suggested that the relationship between circulating MDA concentrations and MDA adducts may be relatively weak because MDA is generated predominantly in cell membranes, some distance from cellular DNA [64].
Limitations of the present study include small sample size, which reduced our ability to detect interaction effects. Another limitation of the study was that catecholestrogen levels were not measured, therefore preventing examination of individual catecholestrogen levels along with levels of oxidative stress and breast density.
Conclusion
Results from the present study suggest that CYP1A2 activity is related to mammographic density levels and oxidative stress, but that the nature of the relationship depends on menopausal status. These findings provide further evidence that variation in the level of activity of enzymes involved in estrogen metabolism is related to breast density levels and potentially breast cancer risk [65].
Abbreviations
- AAMU:
-
5-acetylamino-6-amino-3-methyluracil
- AFMU:
-
5-acetylamino-6-formylamino-3-methyluracil
- BMI:
-
body mass index
- CMR:
-
caffeine metabolic ratio
- CYP1A2:
-
cytochrome P450 1A2
- dG-MDA:
-
malondialdehyde–deoxyguanosine (adducts)
- HPLC:
-
high-performance liquid chromatography
- MDA:
-
malondialdehyde
- 1U:
-
1-methylurate
- 1:
-
7U = 1,7-dimethylurate
- 1X:
-
1-methylxanthine
- WHR:
-
waist–hip ratio.
References
Boyd NF, Lockwood GA, Byng J, Tritchler DL, Yaffe M: Mammographic densities and breast cancer risk. Cancer Epidemiol Biomarkers Prev. 1998, 7: 1133-1144.
Greendale GA, Reboussin BA, Sie A, Singh R, Olson LK, Gatewood O, Bassett LW, Wasilauskas C, Bush T, Barrett-Connor E: Effects of estrogen and estrogen-progestin on mammographic parenchymal density. Ann Intern Med. 1999, 130: 262-269.
Brisson J, Brisson B, Coté G, Maunsell E, Bérubé S, Robert J: Tamoxifen and mammographic breast densities. Cancer Epidemiol Biomarkers Prev. 2000, 9: 911-915.
Gram IT, Ursin G, Spicer DV, Pike MC: Reversal of gonadotropin-releasing hormone agonist induced reductions in mammographic densities on stopping treatment. Cancer Epidemiol Biomarkers Prev. 2001, 10: 1117-1120.
Boyd NF, Connelly P, Byng J, Yaffe M, Draper H, Little L, Jones D, Martin LJ, Lockwood G, Tritchler D: Plasma lipids, lipoproteins, and mammographic densities. Cancer Epidemiol Biomarkers Prev. 1995, 4: 727-733.
Boyd NF, McGuire V: Evidence of lipid peroxidation in premenopausal women with mammographic dysplasia. Cancer Lett. 1990, 50: 31-37. 10.1016/0304-3835(90)90175-W.
Basu AK, Marnett LJ: Unequivocal demonstration that malondialdehyde is a mutagen. Carcinogenesis. 1983, 4: 331-333.
Vaca CE, Wilhelm J, Harms-Ringdahl M: Interaction of lipid peroxidation products with DNA. A review. Mutat Res. 1988, 195: 137-149. 10.1016/0165-1110(88)90022-X.
Burdon RH, Alliangana D, Gill V: Endogenously generated active oxygen species and cellular glutathione levels in relation to BHK-21 cell proliferation. Free Radic Res. 1994, 21: 121-133.
Vaca CE, Fang JL, Mutanen M, Valsta L: 32 P-Postlabelling determination of DNA adducts of malonaldehyde in humans: total white blood cells and breast tissue. Carcinogenesis. 1995, 16: 1847-1851.
Gonenc A, Ozkan Y, Torun M, Simsek B: Plasma malondialdehyde (MDA) levels in breast and lung cancer patients. J Clin Pharm Ther. 2001, 26: 141-144. 10.1046/j.1365-2710.2001.00334.x.
Yamazaki H, Shaw PM, Guengerich FP, Shimada T: Roles of cytochromes P450 1A2 and 3A4 in the oxidation of estradiol and estrone in human liver microsomes. Chem Res Toxicol. 1998, 11: 659-665. 10.1021/tx970217f.
The Endogenous Hormones and Breast Cancer Collaborative Group: Endogenous sex hormones and breast cancer in postmenopausal women: reanalysis of nine prospective studies. J Natl Cancer Inst. 2002, 94: 606-616. 10.1093/jnci/94.8.606.
Ikeya K, Jaiswal AK, Owens RA, Jones JE, Nebert DW, Kimura S: Human CYP1A2: sequence, gene structure, comparison with the mouse and rat orthologous gene, and differences in liver 1A2 mRNA expression. Mol Endocrinol. 1989, 3: 1399-408.
Kadlubar FF, Butler MA, Kaderlik KR, Chou HC, Lang NP: Polymorphisms for aromatic amine metabolism in humans: relevance for human carcinogenesis. Environ Health Perspect. 1992, 98: 69-74.
Yager JD, Liehr JG: Molecular mechanisms of estrogen carcinogenesis. Annu Rev Pharmacol Toxicol. 1996, 36: 203-232. 10.1146/annurev.pa.36.040196.001223.
Zhu BT, Conney AH: Is 2-methoxyestradiol an endogenous estrogen metabolite that inhibits mammary carcinogenesis?. Cancer Res. 1998, 58: 2269-2277.
Cavalieri EL, Rogan EG: A unified mechanism in the initiation of cancer. Ann N Y Acad Sci. 2002, 959: 341-354.
Boyd NF, Stone J, Martin LJ, Jong R, Fishell E, Yaffe M, Hammond G, Minkin S: The association of breast mitogens with mammographic densities. Br J Cancer. 2002, 87: 876-882. 10.1038/sj.bjc.6600537.
Block G, Thompson FE, Hartman AM, Larkin FA, Guire KE: Comparison of two dietary questionnaires validated against multiple dietary records collected during a 1-year period. J Am Diet Assoc. 1992, 92: 686-693.
Tang BK, Kadar D, Qian L, Iriah J, Yip J, Kalow W: Caffeine as a metabolic probe: validation of its use for acetylator phenotyping. Clin Pharmacol Ther. 1991, 49: 648-657.
Streetman DS, Bertino JS, Nafziger AN: Phenotyping of drug-metabolizing enzymes in adults: a review of in-vivo cytochrome P450 phenotyping probes. Pharmacogenetics. 2000, 10: 187-216. 10.1097/00008571-200004000-00001.
Tang BK, Zhou Y, Kadar D, Kalow W: Caffeine as a probe for CYP1A2 activity: potential influence of renal factors on urinary phenotypic trait measurements. Pharmacogenetics. 1994, 4: 117-124.
Kalow W, Tang BK: The use of caffeine for enzyme assays: a critical appraisal. Clin Pharmacol Ther. 1993, 53: 503-514.
Nordmark A, Lundgren S, Cnattingius S, Rane A: Dietary caffeine as a probe agent for assessment of cytochrome P4501A2 activity in random urine samples. Br J Clin Pharmacol. 1999, 47: 397-402. 10.1046/j.1365-2125.1999.00918.x.
Kashuba AD, Bertino JS, Kearns GL, Leeder JS, James AW, Gotschall R, Nafziger AN: Quantitation of three-month intraindividual variability and influence of sex and menstrual cycle phase on CYP1A2, N-acetyltransferase-2, and xanthine oxidase activity determined with caffeine phenotyping. Clin Pharmacol Ther. 1998, 63: 540-551.
Handelman GJ, Packer L, Cross CE: Destruction of tocopherols, carotenoids, and retinol in human plasma by cigarette smoke. Am J Clin Nutr. 1996, 63: 559-565.
Bird RP, Hung SSO, Hadley M, Draper HH: Determination of malondialdehyde in biological materials by high pressure liquid chromatography. Anal Biochem. 1983, 128: 240-244.
Agarwal S, Draper HH: Isolation of a malondialdehyde-deoxyguanosine adduct from rat liver DNA. Free Radic Biol Med. 1992, 13: 695-699. 10.1016/0891-5849(92)90043-G.
Boyd NF, Stone J, Martin LJ, Jong R, Fishell E, Yaffe M, Hammond G, Minkin S: The association of breast mitogens with mammographic densities. Br J Cancer. 2002, 87: 876-882. 10.1038/sj.bjc.6600537.
Byng JW, Boyd NF, Fishell E, Jong RA, Yaffe MJ: The quantitative analysis of mammographic densities. Phys Med Biol. 1994, 39: 1629-1638. 10.1088/0031-9155/39/10/008.
SAS Institute Inc: SAS/STAT User's Guide, version 6. 1989, Cary, NC: SAS Institute Inc
Ceballos-Picot I, Trivier JM, Nicole A, Sinet PM, Thevenin M: Age-correlated modifications of copper-zinc superoxide dismutase and glutathione-related enzyme activities in human erythrocytes. Clin Chem. 1992, 38: 66-70.
Van Gaal LF, Zhang A, Steijaert MM, De Leeuw IH: Human obesity: from lipid abnormalities to lipid oxidation. Int J Obes Relat Metab Disord. 1995, Suppl 3: S21-S26.
Sabuncu T, Vural H, Harma M, Harma M: Oxidative stress in polycystic ovary syndrome and its contribution to the risk of cardiovascular disease. Clin Biochem. 2001, 34: 407-413. 10.1016/S0009-9120(01)00245-4.
Garg R, Kumbkarni Y, Aljada A, Mohanty P, Ghanim H, Hamouda W, Dandona P: Troglitazone reduces reactive oxygen species generation by leukocytes and lipid peroxidation and improves flow-mediated vasodilatation in obese subjects. Hypertension. 2000, 36: 430-435.
Vachon CM, Kuni CC, Anderson K, Anderson VE, Sellers TA: Association of mammographically defined percent breast density with epidemiologic risk factors for breast cancer (United States). Cancer Causes Control. 2000, 11: 653-662. 10.1023/A:1008926607428.
Kalow W, Tang BK: Use of caffeine metabolite ratios to explore CYP1A2 and xanthine oxidase activities. Clin Pharmacol Ther. 1991, 50: 508-519.
Aiken LS, West SG: Multiple Regression: Testing and Interpreting Interactions. 1991, Newbury Park: Sage Publications Inc
Vistisen K, Poulsen HE, Loft S: Foreign compound metabolism capacity in man measured from metabolites of dietary caffeine. Carcinogenesis. 1992, 13: 1561-1568.
Schrenk D, Brockmeier D, Morike K, Bock KW, Eichelbaum M: A distribution study of CYP1A2 phenotypes among smokers and non-smokers in a cohort of healthy Caucasian volunteers. Eur J Clin Pharmacol. 1998, 53: 361-367. 10.1007/s002280050394.
Riza E, dos Santos Silva I, De Stavola B, Bradlow HL, Sepkovic DW, Linos D, Linos A: Urinary estrogen metabolites and mammographic parenchymal patterns in postmenopausal women. Cancer Epidemiol Biomarkers Prev. 2001, 10: 627-634.
Muti P, Bradlow HL, Micheli A, Krogh V, Freudenheim JL, Schünemann HJ, Stanulla M, Yang J, Sepkovic DW, Trevisan M, Berrino F: Estrogen metabolism and risk of breast cancer: a prospective study of the 2:16α-hydroxyestrone ratio in pre- and postmenopausal women. Epidemiology. 2000, 11: 635-640. 10.1097/00001648-200011000-00004.
Meilahn EN, De Stavola B, Allen DS, Fentiman IS, Bradlow HL, Sepkovic DW, Kuller LH: Do urinary oestrogen metabolites predict breast cancer? Guernsey III cohort follow-up. Br J Cancer. 1998, 78: 1250-1255.
McManus ME, Burgess W, Snyderwine E, Stupans I: Specificity of rabbit cytochrome P-450 isozymes involved in the metabolic activation of the food derived mutagen 2-amino-3-methylimidazo[4,5-f] quinoline. Cancer Res. 1988, 48: 4513-4519.
Yamazoe Y, Abu-Zeid M, Manabe S, Toyama S, Kato R: Metabolic activation of a protein pyrolysate promutagen 2-amino-3,8-dimethylimidazo[4,5-f]quinoxaline by rat liver microsomes and purified cytochrome P-450. Carcinogenesis. 1988, 9: 105-109.
Butler MA, Iwasaki M, Guengerich FP, Kadlubar FF: Human cytochrome P-450PA (P-450IA2), the phenacetin O-deethylase, is primarily responsible for the hepatic 3-demethylation of caffeine and N-oxidation of carcinogenic arylamines. Proc Natl Acad Sci USA. 1989, 86: 7696-7700.
Butler MA, Lang NP, Young JF, Caporaso NE, Vineis P, Hayes RB, Teitel CH, Massengill JP, Lawsen MF, Kadlubar FF: Determination of CYP1A2 and NAT2 phenotypes in human populations by analysis of caffeine urinary metabolites. Pharmacogenetics. 1992, 2: 116-127.
Tantcheva-Poor I, Zaigler M, Rietbrock S, Fuhr U: Estimation of cytochrome P-450 CYP1A2 activity in 863 healthy Caucasians using a saliva-based caffeine test. Pharmacogenetics. 1999, 9: 131-144.
Le Marchand L, Franke AA, Custer L, Wilkens LR, Cooney RV: Lifestyle and nutritional correlates of cytochrome CYP1A2 activity: inverse associations with plasma lutein and alpha-tocopherol. Pharmacogenetics. 1997, 7: 11-19.
Kall MA, Vang O, Clausen J: Effects of dietary broccoli on human in vivo drug metabolizing enzymes: evaluation of caffeine, oestrone and chlorzoxazone metabolism. Carcinogenesis. 1996, 17: 793-799.
Horn EP, Tucker MA, Lambert G, Silverman D, Zametkin D, Sinha R, Hartge T, Landi MT, Caporaso NE: A study of gender-based cytochrome P4501A2 variability: a possible mechanism for the male excess of bladder cancer. Cancer Epidemiol Biomarkers Prev. 1995, 4: 529-533.
Nebert DW, Roe AL, Dieter MZ, Solis WA, Yang Y, Dalton TP: Role of the aromatic hydrocarbon receptor and [Ah] gene battery in the oxidative stress response, cell cycle control, and apoptosis. Biochem Pharmacol. 2000, 59: 65-85. 10.1016/S0006-2952(99)00310-X.
Poulsen HE, Loft S, Prieme H, Vistisen K, Lykkesfeldt J, Nyyssonen K, Salonen JT: Oxidative DNA damage in vivo: relationship to age, plasma antioxidants, drug metabolism, glutathione-S-transferase activity and urinary creatinine excretion. Free Radic Res. 1998, 29: 565-571.
Prieme H, Nyyssonen K, Gronbaek K, Klarlund M, Loft S, Tonnesen P, Salonen JT, Poulsen HE: Randomized controlled smoking cessation study: transient increase in plasma high density lipoprotein but no change in lipoprotein oxidation resistance. Scand J Clin Lab Invest. 1998, 58: 11-18. 10.1080/00365519850186788.
Prieme H, Loft S, Klarlund M, Gronbaek K, Tonnesen P, Poulsen HE: Effect of smoking cessation on oxidative DNA modification estimated by 8-oxo-7,8-dihydro-2'-deoxyguanosine excretion. Carcinogenesis. 1998, 19: 347-351. 10.1093/carcin/19.2.347.
England T, Beatty E, Rehman A, Nourooz-Zadeh J, Pereira P, O'Reilly J, Wiseman H, Geissler C, Halliwell B: The steady-state levels of oxidative DNA damage and of lipid peroxidation (F2-isoprostanes) are not correlated in healthy human subjects. Free Radic Res. 2000, 32: 355-362.
Siu GM, Draper HH: Metabolism of malonaldehyde in vivo and in vitro. Lipids. 1982, 17: 349-355.
Jacobson EA, Newmark H, Bird R, Bruce WR: Increased excretion of malonaldehyde equivalents in the urine after consumption of cooked, stored meats. Nutr Rep Int. 1983, 28: 509-517.
Lasheras C, Gonzalez S, Huerta JM, Lombardia C, Ibanez R, Patterson AM, Fernandez S: Food habits are associated with lipid peroxidation in an elderly population. J Am Diet Assoc. 2003, 103: 1480-1487.
Dhanakoti SN, Draper HH: Response of urinary malondialdehyde to factors that stimulate lipid peroxidation in vivo. Lipids. 1987, 22: 643-646.
Dedon PC, Plastaras JP, Rouzer CA, Marnett LJ: Indirect mutagenesis by oxidative DNA damage: formation of the pyrimidopurinone adduct of deoxyguanosine by base propenal. Proc Natl Acad Sci USA. 1998, 95: 11113-11116. 10.1073/pnas.95.19.11113.
Halliwell B: Establishing the significance and optimal intake of dietary antioxidants: the biomarker concept. Nutr Rev. 1999, 57: 104-113.
Everett SM, Singh R, Leuratti C, White KL, Neville P, Greenwood D, Marnett LJ, Schorah CJ, Forman D, Shuker D, Axon AT: Levels of malondialdehyde-deoxyguanosine in the gastric mucosa: relationship with lipid peroxidation, ascorbic acid, and Helicobacter pylori. Cancer Epidemiol Biomarkers Prev. 2001, 10: 369-376.
Hong CC, Thompson HJ, Jiang C, Hammond GL, Tritchler D, Yaffe M, Boyd NF: Val158Met Polymorphism in catechol-O-methyltransferase gene associated with risk factors for breast cancer. Cancer Epidemiol Biomarkers Prev. 2003, 12: 838-847.
Acknowledgements
The authors thank Stefany Michel for data collection. This research was funded in part by the Canadian Breast Cancer Research Initiative (CBCRI 009065), and by Health Canada through a National Health Research and Development Program (NHRDP) Research Training Award.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
None declared.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
About this article
Cite this article
Hong, CC., Tang, BK., Rao, V. et al. Cytochrome P450 1A2 (CYP1A2) activity, mammographic density, and oxidative stress: a cross-sectional study. Breast Cancer Res 6, R338 (2004). https://doi.org/10.1186/bcr797
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/bcr797