Abstract
Androgens have important physiological effects in women while at the same time they may be implicated in breast cancer pathologies. However, data on the effects of androgens on mammary epithelial proliferation and/or breast cancer incidence are not in full agreement. We performed a literature review evaluating current clinical, genetic and epidemiological data regarding the role of androgens in mammary growth and neoplasia. Epidemiological studies appear to have significant methodological limitations and thus provide inconclusive results. The study of molecular defects involving androgenic pathways in breast cancer is still in its infancy. Clinical and nonhuman primate studies suggest that androgens inhibit mammary epithelial proliferation and breast growth while conventional estrogen treatment suppresses endogenous androgens. Abundant clinical evidence suggests that androgens normally inhibit mammary epithelial proliferation and breast growth. Suppression of androgens using conventional estrogen treatment may thus enhance estrogenic breast stimulation and possibly breast cancer risk. Addition of testosterone to the usual hormone therapy regimen may diminish the estrogen/progestin increase in breast cancer risk but the impact of this combined use on mammary gland homeostasis still needs evaluation.
Similar content being viewed by others
Introduction
Treatment of women with physiological testosterone supplementation to remedy hypoactive sexual desire disorder is an area of great interest at present [1]. While it seems evident that testosterone treatment increases sexual activity, the risk-benefit ratio for such treatment remains unclear. Androgen receptors are found in virtually every tissue in women as well as men, including breast, bone and brain, indicating that androgens and their metabolites may play an important role in normal tissue homeostasis and possibly in pathologies like breast cancer, osteoporosis, libido and cognitive decline. Thus, testosterone treatment to improve sexual function may have unintended effects in diverse tissues. A continuing area of concern is the notion that excess androgen exposure may increase the risk of breast cancer in women [2].
Experimental data suggest that conventional estrogen treatment regimens, both as oral contraceptives (OCs) and hormone therapy (HT) [3], upset the normal estrogen/androgen balance and promote 'unopposed' estrogenic stimulation of mammary epithelial proliferation and, hence, potentially breast cancer risk. This is due to suppression of gonadotropins by exogenous estrogen treatment, resulting in globally reduced ovarian steroidogenesis, so both endogenous estrogen and androgen production are reduced, but only estrogens are provided by the treatment regimens. Additionally, estrogens, particularly in oral form, stimulate the hepatic production of sex hormone binding globulin (SHBG), which binds testosterone with high affinity, reducing androgen bioavailability. As a result of this dual effect, total and bioavailable testosterone levels are significantly reduced in women taking oral contraceptives or estrogen supplementation for ovarian insufficiency [4].
This literature review compares the findings that androgens in women promote the risk for breast cancer versus the evidence that androgens protect the mammary gland from hormone-induced stimulation, increased proliferation and neoplasia.
Normal breast development: estrogens and androgens
Estrogens stimulate, while androgens inhibit breast development independently of genetic sex. Breast tissue is similar in prepubertal boys and girls. Pubertal rises in estrogen levels cause breast growth in girls and frequently in boys (transiently). Estradiol levels are significantly higher in girls with premature thelarche than in normal prepubertal girls. An association between expression of a high activity isoform of the testosterone metabolizing CYP3A4 and the early onset of thelarche has been documented, suggesting that decreasing testosterone levels may also trigger early breast growth [5]. Conversely, androgen excess due to adrenal tumor or hyperplasia suppresses normal breast development in girls, despite apparently adequate estrogen levels [6]. In castrated male-to-female transsexuals, feminizing estrogen therapy stimulates breast growth with full acinar and lobular formation and estrogen-treated genetically male breast tissue exhibits normal female histology. Estrogens taken to treat prostate cancer also lead to breast development in men with suppressed gonadal function and reduced testosterone levels. Conversely, androgen use by female athletes and female-to-male transsexuals leads to breast atrophy.
Supporting the normal inhibitory role of endogenous androgens on breast growth, androgen receptor (AR) blockade with flutamide causes gynecomastia and rarely breast adenocarcinoma [7]. Males may also develop gynecomastia when the estrogen/androgen ratio is increased due to decreased androgen production or increased aromatization.
The balance between stimulatory effects of the estrogens and inhibitory effects of the androgens is the critical factor that regulates mammary cell proliferation both in normal and in cancer tissues [8]. It has not been possible to identify specific estrogen/androgen ratios predictive of breast stimulation or inhibiting effects for several reasons. Estradiol and testosterone assays have not been very sensitive nor accurate in the lower ranges, while both hormones bind to SHBG, so total values may not be as informative as 'free' or bioavailable hormone [4]. Moreover, single hormone measurements may not be very informative about tissue exposure over time. Both estradiol and testosterone levels vary hourly in response to diurnal rhythm, diet, stress and exercise, so a single value may be inadequate to assess true tissue exposure. In addition, estradiol and testosterone may be synthesized locally in peripheral tissues from circulating precursors such as the sulfate of dehydroepiandrosterone (DHEA-S) and androstendione [9]. The conjugated products of steroid metabolism find their way into the circulation after peripheral action and provide evidence as to the proportion of the precursor pools of steroids utilized as androgen or estrogen. Analysis of these metabolites by Labrie and colleagues [9] and Sasano and colleagues [10] suggested that the major proportion of androgen effectors in women derive from such an endocrine mode of action, which will not be detected by assays of circulating testosterone or dihydrotestosterone (DHT). Interestingly, while circulating levels of testosterone and DHT are five - to ten-fold higher in men than women, the abundance of androgen metabolites is less than two-fold higher in men, suggesting that local tissue production and action of androgens in women may be more significant than historically suspected.
The mammary gland is capable of synthesizing both estradiol and testosterone. All the steroidogenic enzymes necessary for the formation of androgens and estrogens from steroid precursors - steroid sulfatase, 17β-hydroxysteroid dehydrogenases (17β-HSDs), 3β-HSDs, 5α-reductases and aromatase - have been reported in normal mammary tissues, breast cancer specimens or cell lines [10]. Androgens stimulate or inhibit the growth of breast cancer cells in vitro depending on the cell line and clone under study according to former data [11]. Breast cancer cell lines and tissue specimens express the enzymes involved in DHT as well as estradiol synthesis. In a histochemical study, expression of 5α-reductase was significantly correlated with androgen receptor expression and 17β-HSD and 3β-HSD immunoreactivities and the abundance of this androgenic molecular assembly was inversely correlated with tumor size, histological grade and proliferative index [12], suggesting an inhibitory role for DHT in tumor growth.
Androgen receptor
Androgen agonists such as testosterone and DHT function through binding to the intracellular AR. This is a member of the nuclear hormone receptor super-family comprising classic DNA-binding, hormone binding and activation domains (Figure 1). AR expression is abundant in normal mammary epithelium and in the majority of breast cancer specimens and cell lines. The AR is co-localized with estrogen and progesterone receptors in epithelial cells but not detected in mammary stroma or myoepithelium [13]. The co-expression of estrogen receptor (ER) and AR in mammary epithelial cells suggests that the effects of estrogen and androgen on mammary epithelial proliferation are integrated within the mammary epithelial cell. The AR gene is located on the X chromosome with no corresponding allele on the Y, so it functions solely as a single copy gene, as shown by the complete loss of androgen effect in XY individuals with an inactivating mutation of the AR [14].
Binding of testosterone or DHT triggers a cascade of signaling events, including phosphorylation and conformational changes in the receptor, which dissociates from cytoplasmic proteins and migrates to the cell nucleus. Ligand-activated AR regulates gene expression through binding to androgen response elements located in a gene's enhancer or promoter region. As with other similar receptors, the AR functions in transcriptional regulation in concert with a host of nuclear proteins, which may serve as co-activators or co-repressors. Interestingly, the BRCA1 gene product has been identified as an AR co-activator [15]. The BRCA1 protein binds to the AR and potentiates AR-mediated effects, suggesting that BRCA1 mutations may blunt androgen effects. However, other studies have not confirmed these findings [16].
AR has a highly polymorphic CAG repeat in exon 1 that encodes a polyglutamine stretch (Figure 1). There is evidence that longer CAG repeats are associated with earlier age of breast cancer onset [16]. However, other studies have not confirmed this finding [17]. In a study nested within the Nurses' Health Study cohort [18], no relation was found between AR genotype and breast cancer risk among post-menopausal Caucasian women overall, but an increased risk was observed when analysis was limited to those individuals with a first-degree family history of breast cancer. Germ-line mutations in the AR gene conferring variable degrees of androgen insensitivity have been associated with the occurrence of breast cancer in men [19]. Another study [20] provides evidence that the association with the long AR-CAG was observed only in postmenopausal and not premenopausal women, which may explain the insignificant results in studies restricted to young women. In other studies, reduced risk was observed with another trinucleotide repeat, GGC, in young women. AR repeat length might be partly responsible for the increased risk of early onset breast cancer in women using oral contraceptives or HT [21].
Emphasis should be given to the fact that none of these studies had sufficient statistical power to implicate or exclude specific AR defects in breast cancer risk. A recent epidemiological meta-analysis concludes that there is no association between AR genetic variations and breast cancer risk among Caucasian women [17].
AR-CAG repeat length was inversely associated with testosterone levels in both pre- and postmenopausal normal women [22]. Lillie and colleagues [23] evaluated the association between AR-CAG repeat length and mammographic density, a strong breast cancer risk factor. They found that in postmenopausal estrogen/progesterone users, carriers of the less active AR had a higher mean percentage of density than carriers of the more active AR. This suggests that AR genotype modifies hormone-induced proliferation as reflected in mammographic density and explains the mechanism by which estrogen/progesterone use increases breast cancer risk. However, the exact mechanisms and metabolic paths in which AR participates in normal tissues are still obscure. The role of AR in oncogenesis or breast tumor proliferation remains unclear. It is possible that the steroid receptor contributes differently in healthy compared to cancerous breast tissue; thus, a number of unanswered questions remain and further studies are needed before safe conclusions are drawn.
The hypothesis that androgens are directly involved in breast carcinogenesis is based on the presence of ARs in the majority of breast cancers. It is proposed that androgens, through binding to their receptors, act independently to produce tumors with specific clinical behaviors [24]. Clinical data support that a significant number of poorly differentiated breast carcinomas are ER-negative and progesterone receptor (PR)-negative but AR-positive, or patients with AR-positive tumors experience a better disease-free survival. These associations constitute important clinical and pathologic prognostic information. Recently, AR expression in a tumor is considered as an indicator of lower malignancy potential; this provides a new range of therapeutic targets for poorly differentiated cancers [25].
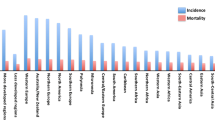
Androgens and breast cancer: epidemiological data
Long-term estrogen treatment increases the risk of breast cancer in both males and females through estrogenic stimulation of mammary epithelial proliferation. Additional carcinogenic effects by estrogen metabolites have been proposed [26]. The most widely accepted risk factor for breast cancer is the cumulative dose of estrogens that breast epithelium is exposed to over time. However, it has been difficult to correlate breast cancer risk with isolated serum estrogen levels in epidemiological studies, probably secondary to problems using single random hormone levels for the evaluation of tissue-specific exposure as discussed above.
Attempts to correlate adrenal precursor steroids with breast cancer incidence have been relatively successful, or at least consistent, perhaps reflecting the importance of local tissue conversion. Many years ago, reduced 17-ketosteroid excretion was noted in the urine of pre-menopausal women with breast cancer and subsequent studies have documented reduced DHEA and its sulfate (DHEA-S) in the serum of pre-menopausal breast cancer patients. In the first prospective study in this field, levels of androgen metabolites in urine were found to be abnormally reduced in premenopausal women who subsequently developed breast cancer [27], indicating a protective role of androgens on the breast. In contrast, in a recent prospective study of pre-menopausal women [28], no association was found between plasma adrenal androgen levels and risk of breast cancer. In the Nurses' Health Study II, no correlation between DHEA and DHEA-S levels and breast cancer risk overall was found but, interestingly, among premenopausal women there was a positive association, especially for tumors that express both ERs and PRs [29]. Also, among premenopausal women, higher levels of testosterone and androstendione were associated with increased risk of invasive ER+/PR+ tumors, although with a non-statistically significant increase in overall risk of breast cancer [29].
Several epidemiological studies have examined the correlation of circulating androgens, such as testosterone, and risk for breast cancer. A major limitation of these studies was that the androgen assays used were developed primarily to measure the higher levels found in men and lack reliability in the low ranges found in normal women [4]. Testosterone and androstenedione levels demonstrate substantial daily variability, while most of the epidemiological data are based on a single blood sample collected at non-standard times. Another problem using serum testosterone levels to gauge androgenic effects at the tissue level is that most of the circulating testosterone is tightly bound to SHBG, while only the free hormone is bioactive. SHBG, and thus total testosterone levels, vary widely based on genetic, metabolic and endocrine influences, and it is now accepted that measurement of free or bioavailable testosterone predicts androgenic effects more accurately than total testosterone levels [4]. Finally, most androgenic activity in women originates from the peripheral conversion of precursors such as DHEA into androgens within the cells of target tissues, and this activity will not be detected by measurement of circulating androgens.
In a recent study [30], levels of testosterone and DHEA-S in saliva were statistically significantly lower in breast cancer patients compared to controls and these differences were more profound in postmenopausal women. Breast cancer patients, when compared to controls, presented with an androgen insufficiency and a relative imbalance of sex steroid hormones in favor of estrogens.
Several studies have revealed, however, that adrenal androgens are increased in postmenopausal women with breast cancer [31]. A possible explanation regarding the divergence between pre- and postmenopausal findings is that one adrenal 'androgen', androstenediol, also known as 'hermaphrodol', is a weak ER agonist. In the presence of high estrogen levels in premenopausal women, androstendiol could exhibit anti-estrogenic effects, while in the hypoestrogenic postmenopausal milieu, the agonist effect may predominate. This view remains speculative, and other possibilities still exist. It is possible that the high estrogen environment in premenopausal women promotes androgenic enzyme and AR expression in mammary tissue, allowing androgenic effects by DHEA metabolites, while in postmenopausal women, an estrogen-deficient tissue microenvironment may favor estrogenic effects.
Genetic variation in CYP19 and SHBG genes was found to contribute to the variance in circulating hormone levels in postmenopausal women, but none was statistically significantly associated with breast cancer risk [32].
In some prospective epidemiological studies, age-adjusted mean values of total and free testosterone and estradiol were significantly higher pre-diagnostically in postmenopausal breast cancer cases compared with controls, and estradiol and total testosterone were elevated in other case-control studies of postmenopausal breast cancer. It was observed that elevated serum levels of both estrogens and androgens contribute to a greater risk of breast cancer [33] and a meta-analysis of nine prospective studies revealed that breast cancer risk increases with increasing concentrations of almost all sex hormones [34].
None of these studies manage, however, to disconnect the risk associated with increased estradiol levels from the androgen component, and since androgens are the obligate precursors for estradiol synthesis, this is a major confounding factor in assessing the role of androgen independently of the known cancer-promoting estrogen effect. In line with these observations, a recent study [35] concluded that increased breast cancer risk with increasing body mass index among postmenopausal women is largely the result of the associated increase in estrogens. The association of androgens with breast cancer risk did not persist after adjustment for estrone, the estrogen most strongly associated with the risk. Other authors conclude that conversion of DHEA to estrogens, particularly estradiol, is required to exert a mitogenic response [36]. These results suggest that the contribution of androgens to breast cancer risk is largely through their role as substrates for estrogen production.
Other studies have found no association between androgens and breast cancer [37, 38]. Recent epidemiological studies on the association between androgen levels and breast cancer risk are summarized in Table 1.
The above mentioned observations indicate the difficulty separating potential direct effects of circulating testosterone from its potential to be aromatized into estradiol. An interesting research topic would be to investigate levels of testosterone and DHT metabolites in these studies in order to assess more directly tissue exposure to androgens. As noted above, a single serum hormone measurement seems unlikely to be informative about a woman's true long-term exposure to that hormone or her specific risk of developing breast cancer. Nor does it seem to be a biologically plausible mechanism that androgens acting as androgens could promote breast cancer, since virtually all clinical data suggest just the opposite. If elevated androgen levels directly contribute to breast cancer, then women with clinically evident long-term hyperandrogenism - for example, polycystic ovary syndrome and congenital adrenal hyperplasia - should experience increased rates of breast cancer, but this is not the case [39]. Moreover, androgen levels are chronically elevated in men, who have a breast cancer risk less than 1% of that of women. This is despite the fact that lifetime estradiol levels are not much lower in men than in women. In fact, decreased androgen levels found, for example, in Kleinefelter's syndrome and other hypogonadal syndromes increase the risk of breast cancer in males [40]. Epidemiological studies in men indicate that low urinary androsterone and serum free testosterone levels are related to early onset of breast cancer, a much higher relapse rate and a worse response to endocrine therapy [41].
Hormone therapy and androgens
Exposure to endogenous and exogenous estrogens is thought to contribute to increased breast cancer risk. Since the introduction of combined OCs 40 years ago, many changes in doses and their biochemical structures have taken place and the possibility that OCs may increase the risk of breast cancer has been the subject of intense research. Although many epidemiological studies in the past have not linked OC use to breast cancer risk, several more recent studies have found an association, either overall or especially in subgroups of women. A large meta-analysis on previously published studies [42] calculated a small but significant increase in relative risk of breast cancer (RR = 1.24) in current OC users while other publications [43] have not associated current or former OC use with an increased risk of breast cancer. However, because pill users are young, this represents a very small increase in absolute risk. It is not yet known if lower dose and variable OC formulations are associated with a similar increase in risk, making comparisons very difficult.
The bulk of the currently available evidence supports a causal relationship between the use of HT and breast cancer. Recent and long-term users of HT are associated with higher risk. The effect of concurrent progestin use appears to further increase risk above that with estrogens alone. The most important randomized clinical trial providing information about this issue is the Women's Health Initiative (WHI) study [44] reporting increased risk of breast cancer in women who took estrogen plus progestin but not in women who took estrogen alone [45]. The results from observational studies are generally consistent with those of the WHI trial, reporting no significant variation in the risk of breast cancer with use of different estrogens, progestins, doses, or routes of administration.
A group of postmenopausal participants in the WHI study used testosterone combined with estrogens. In this group, testosterone addition for a period of a year had no statistically significant effect on breast cancer occurrence, suggesting at least that androgen induction did not increase the number of breast cancer cases in this trial [46]. In the same study, rates of breast cancer were lower in longer-term compared to shorter-term users of estrogen plus testosterone. On the other hand, in a prospective study of over a million person-years with 24 years of follow-up within the Nurses' Health Study, current users of estrogen plus testosterone have shown a 2.5-fold increased risk of developing breast cancer compared to menopausal women who used estrogen-only therapy or to women who never used postmenopausal hormone formulations [47].
If androgens are protective against breast cancer as many studies suggest, then conventional HT may promote breast cancer not only by increasing estrogen exposure but also by decreasing endogenous androgen activity. Oral estrogen therapy reduces free androgens by stimulating hepatic production of SHBG and through suppression of luteinizing hormone, thus inhibiting ovarian androgen production [4]. Thus, institution of pharmacological estrogen therapy at menopause may result in a drastic reduction in the testosterone/estradiol ratio, which is normally maintained at relatively high levels throughout a woman's lifespan (Figure 2).
Pertinent to these results, our published article [48] provides important information about the addition of testosterone to the HT regimen. In our evaluation of 508 postmenopausal women in Australia receiving testosterone in addition to usual HT, the incidence of breast cancer in testosterone users was substantially less than in women receiving estrogen/progestin in the WHI study and in the Million-woman study [49]. Breast cancer rates in the testosterone users was closer to that reported for HT never users, and their age-standardization rate was the same as for the general population in South Australia. These observations suggest that the addition of physiological doses of androgen to OCs and HT could protect the breast from 'unopposed' estrogenic effects.
Suppression of normal endogenous androgen may be an adverse consequence of pharmacological estrogen therapy, if androgens are indeed protective against estrogen-induced mammary proliferation. We have shown that addition of low physiological doses of testosterone (producing serum levels in the mid-normal range for women as well as rhesus monkeys) to estrogen therapy in ovariectomized rhesus monkeys significantly inhibits HT-induced mammary epithelial proliferation [3] (Figure 3). Additionally, testosterone treatment significantly reduced mammary epithelial estrogen receptor expression, thus suggesting a potential mechanism for the growth inhibitory effect. Moreover, we have found that treatment of intact cycling monkeys with the AR antagonist flutamide resulted in a significant increase in mammary epithelial proliferation [3], adding to the burden of evidence that endogenous androgens normally limit mammary proliferation and, hence, cancer risk. Other studies on primates also suggest that inclusion of testosterone with estrogen/progesterone use may counteract breast cell proliferation [50]. In a recent randomized, double-blind, placebo-controlled study, testosterone use inhibited exogenous estrogen-induced breast tissue proliferation in postmenopausal women [51]. There is also evidence that testosterone does not influence mammographic breast density like conventional HT [51, 52]. The antiproliferative effects of androgens on breast tissue may occur either indirectly, via downregulation of other receptors like PRs, or directly, through breast AR stimulation.
Mammary epithelial proliferation shown by Ki67 immunoreactivity (brown dots) in ovariectomized monkeys treated with (a) placebo (Con), (b) estradiol (E2), (c) E2 and progesterone (P4), (d) tamoxifen (Tam) and (e) E2 and testosterone (T). (f) Quantification of the Ki67 proliferation index. Proliferation is increased with E2 or E2 and P4 (E/P), while this increase is attenuated by the addition of T to E2 (E/T). All differences are statistically significant when compared to the placebo group. Data from Zhou and colleagues [53].
Women, and particularly postmenopausal women, have been treated with testosterone for female sexual dysfunction for almost six decades. The exact biological role of androgens in the restoration of libido in hypoactive sexual desire disorder in females is still unclear. The main safety concern for women who have undergone years of this therapy has been breast and endometrial cancer risk related to androgens. In a recent trial of 814 sexually hypoactive women, the results for breast cancer risk were inconclusive [1]. Nevertheless, current experience does not confirm a positive correlation between testosterone use and breast cancer occurrence; thus, androgens do have a place in female sexual dysfunction treatment.
Conclusion
This review focuses on the role of androgens with regard to breast growth and neoplasia. Measurement of circulating sex steroids and their metabolites demonstrates that androgen activity is normally abundant in healthy women throughout their entire lifetime. Epidemiological studies investigating testosterone levels and breast cancer risk have major theoretical and methodological limitations and do not provide consensus. The molecular epidemiology of defects in pathways involved in androgen synthesis and activity in breast cancer hold great promise, but investigation of these is still in the early stages. Clinical observations and experimental data indicate that androgens inhibit mammary growth, and they have been used in the past with success to treat breast cancer. It is of concern that current forms of estrogen treatment in OCs and for ovarian failure result in suppression of endogenous androgen activity considering that the addition of testosterone to the HT regimen ameliorates the stimulating effects of estrogen/progestin on the breast. Research addressing the role of androgens in breast cancer prevention and the efficacy of hormonal supplementation with physiological androgen to maintain estrogen/androgen ratios typical of normal women is warranted.
Abbreviations
- AR:
-
androgen receptor
- DHEA:
-
dehydroepiandrosterone
- DHEA-S:
-
DHEA sulfate
- DHT:
-
dihydrotestosterone
- ER:
-
estrogen receptor
- HSD:
-
hydroxysteroid dehydrogenase
- HT:
-
hormone therapy
- OC:
-
oral contraceptive
- PR:
-
progesterone receptor
- SHBG:
-
sex hormone binding globulin
- WHI:
-
Women's Health Initiative.
References
Davis SR, Moreau M, Kroll R, Bouchard C, Panay N, Gass M, Braunstein GD, Hirschberg AL, Rodenberg C, Pack S, Koch H, Moufarege A, Studd J, APHRODITE Study Team: Testosterone for low libido in postmenopausal women not taking estrogen. N Engl J Med. 2008, 359: 2005-2017. 10.1056/NEJMoa0707302.
Schover LR: Androgen therapy for loss of desire in women: is the benefit worth the breast cancer risk?. Fertil Steril. 2008, 90: 129-140. 10.1016/j.fertnstert.2007.05.057.
Dimitrakakis C, Zhou J, Wang J, Belanger A, LaBrie F, Cheng C, Powell D, Bondy C: A physiologic role for testosterone in limiting estrogenic stimulation of the breast. Menopause. 2003, 10: 292-298. 10.1097/01.GME.0000055522.67459.89.
Lobo RA: Androgens in postmenopausal women: production, possible role, and replacement options. Obstet Gynecol Surv. 2001, 56: 361-376. 10.1097/00006254-200106000-00022.
Kadlubar F, Berkowitz G, Delongchamp R, Green B, Wang C, Wolff MS: The putative high activity variant, CYP3A4*1B, predicts the onset of puberty in young girls. Proc Am Assoc Cancer Res. 2001, 42: 408-
Forsbach G, Guitron-Cantu A, Vazquez-Lara J, Mota-Morales M, Diaz-Mendoza ML: Virilizing adrenal adenoma and primary amenorrhea in a girl with adrenal hyperplasia. Arch Gynecol Obstet. 2000, 263: 134-136. 10.1007/s004040050012.
Karamanakos P, Mitsiades CS, Lembessis P, Kontos M, Trafalis D, Koutsilieris M: Male breast adenocarcinoma in a prostate cancer patient following prolonged anti-androgen monotherapy. Anticancer Res. 2004, 24: 1077-1081.
Labrie F: Dehydroepiandrosterone, androgens and the mammary gland. Gynecol Endocrinol. 2006, 22: 118-130. 10.1080/09513590600624440.
Labrie F, Luu-The V, Lin SX, Simard J, Labrie C, El-Alfy M, Pelletier G, Belanger A: Intracrinology: role of the family of 17 beta-hydroxysteroid dehydrogenases in human physiology and disease. J Mol Endocrinol. 2000, 25: 1-16. 10.1677/jme.0.0250001.
Sasano H, Suzuki T, Nakata T, Moriya T: New development in intracrinology of breast carcinoma. Breast Cancer. 2006, 13: 129-136. 10.2325/jbcs.13.129.
Birrell SN, Bentel JM, Hickey TE, Ricciardelli C, Weger MA, Horsfall DJ, Tilley WD: Androgens induce divergent proliferative responses in human breast cancer cell lines. J Steroid Biochem Mol Biol. 1995, 52: 459-467. 10.1016/0960-0760(95)00005-K.
Suzuki M, Ishida H, Shiotsu Y, Nakata T, Akinaga S, Takashima S, Utsumi T, Saeki T, Harada N: Expression level of enzymes related to in situ estrogen synthesis and clinicopathological parameters in breast cancer patients. J Steroid Biochem Mol Biol. 2009, 113: 195-201. 10.1016/j.jsbmb.2008.12.008.
Zhou J, Anderson K, Bievre M, Ng S, Bondy CA: Primate mammary gland insulin-like growth factor system: cellular localization and regulation by sex steroids. J Investig Med. 2001, 49: 47-55. 10.2310/6650.2001.34090.
Avila DM, Zoppi S, McPhaul MJ: The androgen receptor (AR) in syndromes of androgen insensitivity and in prostate cancer. J Steroid Biochem Mol Biol. 2001, 76: 135-142. 10.1016/S0960-0760(00)00158-8.
Park JJ, Irvine RA, Buchanan G, Koh SS, Park JM, Tilley WD, Stallcup MR, Press MF, Coetzee GA: Breast cancer susceptibility gene 1 (BRCAI) is a coactivator of the androgen receptor. Cancer Res. 2000, 60: 5946-5949.
Spurdle AB, Antoniou AC, Duffy DL, Pandeya N, Kelemen L, Chen X, Peock S, Cook MR, Smith PL, Purdie DM, Newman B, Dite GS, Apicella C, Southey MC, Giles GG, Hopper JL, Chenevix-Trench G, Easton DF, EMBRACE Study Collaborators: The androgen receptor CAG repeat polymorphism and modification of breast cancer risk in BRCA1 and BRCA2 mutation carriers. Breast Cancer Res. 2005, 7: R176-10.1186/bcr971.
Cox DG, Blanché H, Pearce CL, Calle EE, Colditz GA, Pike MC, Albanes D, Allen NE, Amiano P, Berglund G, Boeing H, Buring J, Burtt N, Canzian F, Chanock S, Clavel-Chapelon F, Feigelson HS, Freedman M, Haiman CA, Hankinson SE, Henderson BE, Hoover R, Hunter DJ, Kaaks R, Kolonel L, Kraft P, LeMarchand L, Lund E, Palli D, Peeters PH, Riboli E, et al: A comprehensive analysis of the androgen receptor gene and risk of breast cancer: results from the National Cancer Institute Breast and Prostate Cancer Cohort Consortium (BPC3). Breast Cancer Res. 2006, 8: R54-10.1186/bcr1602.
Haiman CA, Brown M, Hankinson SE, Spiegelman D, Colditz GA, Willett WC, Kantoff PW, Hunter DJ: The androgen receptor CAG repeat polymorphism and risk of breast cancer in the Nurses' Health Study. Cancer Res. 2002, 62: 1045-1049.
MacLean HE, Brown RW, Beilin J, Warne GL, Zajac JD: Increased frequency of long androgen receptor CAG repeats in male breast cancers. Breast Cancer Res Treat. 2004, 88: 239-246. 10.1007/s10549-004-0781-6.
Giguere Y, Dewailly E, Brisson J, Ayotte P, Laflamme N, Demers A, Forest VI, Dodin S, Robert J, Rousseau F: Short polyglutamine tracts in the androgen receptor are protective against breast cancer in the general population. Cancer Res. 2001, 61: 5869-5874.
Abbas S, Brauch H, Chang-Claude J, Dunnebier T, Flesch-Janys D, Hamann U, Hein R, Justenhoven C, Salazar R: Polymorphisms in genes of the steroid receptor superfamily modify post-menopausal breast cancer risk associated with menopausal hormone therapy. Int J Cancer. 2009,
Westberg L, Baghaei F, Rosmond R, Hellstrand M, Landen M, Jansson M, Holm G, Bjorntorp P, Eriksson E: Polymorphisms of the androgen receptor gene and the estrogen receptor beta gene are associated with androgen levels in women. J Clin Endocrinol Metab. 2001, 86: 2562-2568. 10.1210/jc.86.6.2562.
Lillie EO, Bernstein L, Ingles SA, Gauderman WJ, Rivas GE, Gagalang V, Krontiris T, Ursin G: Polymorphism in the androgen receptor and mammographic density in women taking and not taking estrogen and progestin therapy. Cancer Res. 2004, 64: 1237-1241. 10.1158/0008-5472.CAN-03-2887.
Nicolas Diaz-Chico B, German Rodriguez F, Gonzalez A, Ramirez R, Bilbao C, Cabrera de Leon A, Aguirre Jaime A, Chirino R, Navarro D, Diaz-Chico JC: Androgens and androgen receptors in breast cancer. J Steroid Biochem Mol Biol. 2007, 105: 1-15. 10.1016/j.jsbmb.2006.11.019.
Ogawa Y, Hai E, Matsumoto K, Ikeda K, Tokunaga S, Nagahara H, Sakurai K, Inoue T, Nishiguchi Y: Androgen receptor expression in breast cancer: relationship with clinicopathological factors and biomarkers. Int J Clin Oncol. 2008, 13: 431-435. 10.1007/s10147-008-0770-6.
Yager JD, Davidson NE: Estrogen carcinogenesis in breast cancer. N Engl J Med. 2006, 354: 270-282. 10.1056/NEJMra050776.
Bulbrook RD, Thomas BS, Utsunomiya J, Hamaguchi E: The urinary excretion of 11-deoxy-17-oxosteroids and 17-hydroxy-corticosteroids by normal Japanese and British women. J Endocrinol. 1967, 38: 401-406. 10.1677/joe.0.0380401.
Page JH, Colditz GA, Rifai N, Barbieri RL, Willett WC, Hankinson SE: Plasma adrenal androgens and risk of breast cancer in premenopausal women. Cancer Epidemiol Biomarkers Prev. 2004, 13: 1032-1036.
Eliassen AH, Missmer SA, Tworoger SS, Spiegelman D, Barbieri RL, Dowsett M, Hankinson SE: Endogenous steroid hormone concentrations and risk of breast cancer among pre-menopausal women. J Natl Cancer Inst. 2006, 98: 1406-1415. 10.1093/jnci/djj376.
Dimitrakakis C, Glaser RL, Zava DT, Tsigginou A, Marinopoulos S, Antsaklis A: The protective role of androgens: salivary hormone levels in newly diagnosed breast cancer patients. 26th Annual Miami Breast Cancer Conference: March 4-7, 2009; Miami, FL. 2009, [http://www.cancerlearning.com/index.cfm/fuseaction/conference.showOverview/id/5/conference_id/93]
Tworoger SS, Missmer SA, Eliassen AH, Spiegelman D, Folkerd E, Dowsett M, Barbieri RL, Hankinson SE: The association of plasma DHEA and DHEA sulfate with breast cancer risk in predominantly premenopausal women. Cancer Epidemiol Biomarkers Prev. 2006, 15: 967-971. 10.1158/1055-9965.EPI-05-0976.
Olson JE, Ingle JN, Ma CX, Pelleymounter LL, Schaid DJ, Pankratz VS, Vierkant RA, Fredericksen ZS, Wu Y, Couch FJ, Vachon CM, Sellers TA, Weinshilboum RM: A comprehensive examination of CYP19 variation and risk of breast cancer using two haplotype-tagging approaches. Breast Cancer Res Treat. 2007, 102: 237-247. 10.1007/s10549-006-9324-7.
Eliassen AH, Missmer SA, Tworoger SS, Hankinson SE: Endogenous steroid hormone concentrations and risk of breast cancer: does the association vary by a woman's predicted breast cancer risk?. J Clin Oncol. 2006, 24: 1823-1830. 10.1200/JCO.2005.03.7432.
Key T, Appleby P, Barnes I, Reeves G, Endogenous Hormones and Breast Cancer Collaborative Group: Endogenous sex hormones and breast cancer in postmenopausal women: reanalysis of nine prospective studies. J Natl Cancer Inst. 2002, 94: 606-616.
Key TJ, Appleby PN, Reeves GK, Roddam A, Dorgan JF, Longcope C, Stanczyk FZ, Stephenson HE, Falk RT, Miller R, Schatzkin A, Allen DS, Fentiman IS, Key TJ, Wang DY, Dowsett M, Thomas HV, Hankinson SE, Toniolo P, Akhmedkhanov A, Koenig K, Shore RE, Zeleniuch-Jacquotte A, Berrino F, Muti P, Micheli A, Krogh V, Sieri S, Pala V, Venturelli E, et al: Body mass index, serum sex hormones, and breast cancer risk in post-menopausal women. J Natl Cancer Inst. 2003, 95: 1218-1226. 10.1093/jnci/djg022.
Schmitt M, Klinga K, Schnarr B, Morfin R, Mayer D: Dehydroepiandrosterone stimulates proliferation and gene expression in MCF-7 cells after conversion to estradiol. Mol Cell Endocrinol. 2001, 173: 1-13. 10.1016/S0303-7207(00)00442-1.
Adly L, Hill D, Sherman ME, Sturgeon SR, Fears T, Mies C, Ziegler RG, Hoover RN, Schairer C: Serum concentrations of estrogens, sex hormone-binding globulin, and androgens and risk of breast cancer in postmenopausal women. Int J Cancer. 2006, 119: 2402-2407. 10.1002/ijc.22203.
Beattie MS, Costantino JP, Cummings SR, Wickerham DL, Vogel VG, Dowsett M, Folkerd EJ, Willett WC, Wolmark N, Hankinson SE: Endogenous sex hormones, breast cancer risk, and tamoxifen response: an ancillary study in the NSABP Breast Cancer Prevention Trial (P-1). J Natl Cancer Inst. 2006, 98: 110-115. 10.1093/jnci/djj011.
Gadducci A, Gargini A, Palla E, Fanucchi A, Genazzani AR: Polycystic ovary syndrome and gynecological cancers: is there a link?. Gynecol Endocrinol. 2005, 20: 200-208. 10.1080/09513590400021201.
Giordano SH, Buzdar AU, Hortobagyi GN: Breast cancer in men. Ann Intern Med. 2002, 137: 678-687.
Bulbrook RD, Thomas BS: Hormones are ambiguous risk factors for breast cancer. Acta Oncol. 1989, 28: 841-847. 10.3109/02841868909092319.
Breast cancer and hormonal contraceptives: collaborative reanalysis of individual data on 53 297 women with breast cancer and 100 239 women without breast cancer from 54 epidemiological studies. Collaborative Group on Hormonal Factors in Breast Cancer. Lancet. 1996, 347: 1713-1727. 10.1016/S0140-6736(96)90806-5.
Marchbanks PA, McDonald JA, Wilson HG, Folger SG, Mandel MG, Daling JR, Bernstein L, Malone KE, Ursin G, Strom BL, Norman SA, Wingo PA, Burkman RT, Berlin JA, Simon MS, Spirtas R, Weiss LK: Oral contraceptives and the risk of breast cancer. N Engl J Med. 2002, 346: 2025-2032. 10.1056/NEJMoa013202.
Rossouw JE, Anderson GL, Prentice RL, LaCroix AZ, Kooperberg C, Stefanick ML, Jackson RD, Beresford SA, Howard BV, Johnson KC, Kotchen JM, Ockene J, Writing Group for the Women's Health Initiative Investigators: Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results From the Women's Health Initiative randomized controlled trial. JAMA. 2002, 288: 321-333. 10.1001/jama.288.3.321.
Anderson GL, Limacher M, Assaf AR, Bassford T, Beresford SA, Black H, Bonds D, Brunner R, Brzyski R, Caan B, Chlebowski R, Curb D, Gass M, Hays J, Heiss G, Hendrix S, Howard BV, Hsia J, Hubbell A, Jackson R, Johnson KC, Judd H, Kotchen JM, Kuller L, LaCroix AZ, Lane D, Langer RD, Lasser N, Lewis CE, Manson J, Margolis K, Ockene J, et al: Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the Women's Health Initiative randomized controlled trial. JAMA. 2004, 291: 1701-1712. 10.1001/jama.291.14.1701.
Ness RB, Albano JD, McTiernan A, Cauley JA: Influence of estrogen plus testosterone supplementation on breast cancer. Arch Intern Med. 2009, 169: 41-46. 10.1001/archinternmed.2008.507.
Tamimi RM, Hankinson SE, Chen WY, Rosner B, Colditz GA: Combined estrogen and testosterone use and risk of breast cancer in postmenopausal women. Arch Intern Med. 2006, 166: 1483-1489. 10.1001/archinte.166.14.1483.
Dimitrakakis C, Jones RA, Liu A, Bondy CA: Breast cancer incidence in postmenopausal women using testosterone in addition to usual hormone therapy. Menopause. 2004, 11: 531-535. 10.1097/01.GME.0000119983.48235.D3.
Beral V: Breast cancer and hormone-replacement therapy in the Million Women Study. Lancet. 2003, 362: 419-427. 10.1016/S0140-6736(03)14596-5.
Somboonporn W, Davis SR: Testosterone effects on the breast: implications for testosterone therapy for women. Endocr Rev. 2004, 25: 374-388. 10.1210/er.2003-0016.
Hofling M, Hirschberg AL, Skoog L, Tani E, Hagerstrom T, von Schoultz B: Testosterone inhibits estrogen/progestogen-induced breast cell proliferation in postmenopausal women. Menopause. 2007, 14: 183-190. 10.1097/01.gme.0000232033.92411.51.
Conner P: Breast response to menopausal hormone therapy - aspects on proliferation, apoptosis and mammographic density. Ann Med. 2007, 39: 28-41. 10.1080/07853890601039842.
Zhou J, Ng S, Adesanya-Famuiya O, Anderson K, Bondy CA: Testosterone inhibits estrogen-induced mammary epithelial proliferation and suppresses estrogen receptor expression. Faseb J. 2000, 14: 1725-1730. 10.1096/fj.99-0863com.
Micheli A, Meneghini E, Secreto G, Berrino F, Venturelli E, Cavalleri A, Camerini T, Di Mauro MG, Cavadini E, De Palo G, Veronesi U, Formelli F: Plasma testosterone and prognosis of post-menopausal breast cancer patients. J Clin Oncol. 2007, 25: 2685-2690. 10.1200/JCO.2006.09.0118.
Suzuki T, Darnel AD, Akahira JI, Ariga N, Ogawa S, Kaneko C, Takeyama J, Moriya T, Sasano H: 5alpha-reductases in human breast carcinoma: possible modulator of in situ androgenic actions. J Clin Endocrinol Metab. 2001, 86: 2250-2257. 10.1210/jc.86.5.2250.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
About this article
Cite this article
Dimitrakakis, C., Bondy, C. Androgens and the breast. Breast Cancer Res 11, 212 (2009). https://doi.org/10.1186/bcr2413
Published:
DOI: https://doi.org/10.1186/bcr2413