Abstract
Introduction
Androgens have been hypothesised to influence risk of breast cancer through several possible mechanisms, including their conversion to estradiol or their binding to the oestrogen receptor and/or androgen receptor (AR) in the breast. Here, we report on the results of a large and comprehensive study of the association between genetic variation in the AR gene and risk of breast cancer in the National Cancer Institute Breast and Prostate Cancer Cohort Consortium (BPC3).
Methods
The underlying genetic variation was determined by first sequencing the coding regions of the AR gene in a panel of 95 advanced breast cancer cases. Second, a dense set of markers from the public database was genotyped in a panel of 349 healthy women. The linkage disequilibrium relationships (blocks) across the gene were then identified, and haplotype-tagging single nucleotide polymorphisms (htSNPs) were selected to capture the common genetic variation across the locus. The htSNPs were then genotyped in the nested breast cancer cases and controls from the Cancer Prevention Study II, European Prospective Investigation into Cancer and Nutrition, Multiethnic Cohort, Nurses' Health Study, and Women's Health Study cohorts (5,603 breast cancer cases and 7,480 controls).
Results
We found no association between any genetic variation (SNP, haplotype, or the exon 1 CAG repeat) in the AR gene and risk of breast cancer, nor were any statistical interactions with known breast cancer risk factors observed.
Conclusion
Among postmenopausal Caucasian women, common variants of the AR gene are not associated with risk of breast cancer.
Similar content being viewed by others
Introduction
The effects of testosterone activity in the breast are still unknown, showing both proliferative and anti-proliferative effects in vitro [1–3]. Levels of testosterone, which is produced in the ovaries, adrenal gland, and peripherally in adipose tissue, either change little or decline slightly after menopause [4–9]. In both pre- and postmenopausal women, circulating testosterone levels are associated with increased risk of breast cancer [10–17].
The androgen receptor (AR) protein exists as two isoforms, both arising from the same DNA sequence on the X chromosome (Xq11-q12). The shorter form of the AR protein lacks the N-terminal region, which is coded by exon 1. Within exon 1 is a tri-nucleotide CAG repeat. Although this polymorphism is associated with AR transactivation activity [18–21] and prostate cancer risk in some studies [22–28], no clear association has been shown with breast cancer risk [29–34]. The 3' UTR (untranslated region) of the AR contains sequence elements that bind to proteins involved in regulation of mRNA stability. This and other sequence-specific characteristics of AR mRNA, including putative function of the repeats in exon 1, have recently been reviewed [35]. The AR is expressed in the normal breast, as well as in primary and metastatic breast cancer tumours, and both the expression and protein levels are correlated with tumour invasiveness [36].
We hypothesised that inherited polymorphisms in genes related to sex steroid hormone synthesis, metabolism, and cell signaling could alter the function of these genes and the proteins they encode, therefore altering breast cancer risk; in this report, we present results for the AR. We used a haplotype-tagging approach, which aims to capture common variants in the AR gene. Here, we present these haplotypes and describe their association with breast cancer risk in a pooled analysis of nested case control studies from a large collaborative study, the Breast and Prostate Cancer Cohort Consortium (BPC3) [37], which includes 5,603 cases of breast cancer and 7,480 controls.
Materials and methods
Study population
The BPC3 has been described in detail elsewhere [37]. Briefly, the consortium includes five large well-established cohorts assembled in the U.S. and Europe which have both DNA samples and extensive questionnaire information (the American Cancer Society Cancer Prevention Study II [38], the European Prospective Investigation into Cancer and Nutrition [EPIC] cohort [39], the Harvard Nurses' Health Study [NHS] [40] and Women's Health Study [WHS] [41], and the Hawaii-Los Angeles Multiethnic Cohort [MEC] [42]). Most women in these cohorts, with the exception of the MEC, were Caucasians of U.S. and European descent. Breast cancer cases were identified in each cohort by self-report with subsequent confirmation of the diagnosis from medical records or tumour registries and/or from linkage with population-based tumour registries (method of confirmation varied by cohort). Controls were matched to cases by ethnicity and age and, in some cohorts, additional criteria (such as country of residence in EPIC).
Genotyping
Coding regions of AR were sequenced in a panel of 95 advanced breast cancer cases from the MEC (19 of each ethnic group: African-American, Latino, Japanese, Native Hawaiian, and white). Thirty-two single nucleotide polymorphisms (SNPs) with minor allele frequency greater than 5% in any of the five ethnic groups or greater than 1% overall were selected from this resequencing as well as any SNP available in dbSNP to be used to select haplotype-tagging SNPs (htSNPs). These SNPs were genotyped in a reference panel of 349 healthy women from the MEC populations (including 70 whites) at the Broad Institute (Cambridge, MA, USA) using the Sequenom, Inc. (San Diego, CA, USA) and Illumina, Inc. (San Diego, CA, USA) platforms, and six htSNPs were selected to maximise R2 H (a measure of correlation between SNPs genotyped and the haplotypes they describe) among Caucasians, using the method of Stram et al. [43]. Genotyping of the six htSNPs in the breast cancer cases and controls was performed in three laboratories (University of Southern California, Los Angeles, CA, USA; Harvard School of Public Health, Boston, MA, USA; and International Agency for Research on Cancer, Lyon, France) using a fluorescent 5' endonuclease assay and the ABI-PRISM 7900 for sequence detection (Taqman) (Applied Biosystems, Foster City, CA). Initial quality control checks of the SNP assays were performed at the manufacturer (Applied Biosystems); an additional 500 test reactions were run by the BPC3. Assay characteristics for the six htSNPs for AR are available on a public website [44]. Sequence validation for each SNP assay was performed and 100% concordance was observed [45]. To assess inter-laboratory variation, each genotyping centre ran assays on a designated set of 94 samples from the Coriell Biorepository (Camden, NJ, USA), showing completion and concordance rates of greater than 99% [45]. The internal quality of genotype data at each genotyping centre was assessed by typing 5%–10% blinded samples in duplicate or triplicate (depending on the study); the resulting concordance was greater than 99%. The genotyping success rate was 94% or greater for each of the six SNPs at each genotyping centre. No deviation from Hardy-Weinberg equilibrium was observed among the controls in each cohort (at the p < 0.01 level) for any given assay. An association among the exon 1 CAG repeat in AR, family history of breast cancer, and breast cancer risk was previously reported (1990–96 follow-up in the NHS, 617 cases and 960 controls [46]). The exon 1 CAG repeat was genotyped in an additional 376 cases and 540 controls from the NHS as well as 669 cases and 674 controls from the WHS, as previously described [46]. Given that there is no association between the CAG repeat and breast cancer risk, and the interaction between this polymorphism and family history was not observed in this larger combined sample set (1,662 cases and 2,174 controls), we decided not to expend the resources necessary to genotype the repeat in the remaining data sets.
Statistical analysis
We used conditional multivariate logistic regression to estimate odds ratios (ORs) for disease in subjects with a linear (additive) scoring for zero, one, or two copies of the minor allele of each SNP. We also used conditional logistic regression with additive scoring and the most common haplotype as the referent to estimate haplotype-specific ORs, using an expectation-substitution approach to assign haplotypes based on the unphased genotype data and to account for uncertainty in assignment [47, 48]. Haplotype frequencies and expected subject-specific haplotype indicators were calculated separately for each cohort (as well as by country within EPIC and race in the MEC). To test the global null hypothesis of no association between variation in AR haplotypes and htSNPs and risk of breast cancer (or subtypes defined by receptor status), we used a likelihood ratio test comparing a model with additive effects for each common haplotype (treating the most common haplotype as the referent) to the intercept-only model. We combined rare haplotypes (those with estimated individual frequencies less than 5% in all cohorts) into a single category that comprised less than 1.5% of the controls.
We considered both unadjusted conditional models and conditional models adjusting for known breast cancer risk factors. The covariates included to account for breast cancer risk factors were age at menarche (≤12 years, 13–14 years, 15+ years), menopausal status (pre-, peri-, and postmenopausal), parity (ever/never full-term pregnancy), body mass index (BMI) (in kg/m2 as a continuous variable), and use of postmenopausal hormones (ever/never). Other common risk factors, including family history of breast cancer, personal history of benign breast disease, and age at menopause, were unavailable for large numbers of women and therefore were not included in the models. Because the results remained essentially unchanged regardless of the model used, we present results using the unadjusted conditional model. We also evaluated these covariates, restricting analyses of interaction to only those subjects with information available for variables such as family history, with categorical variables divided into quintiles. Interaction effects were evaluated using likelihood ratio testing, comparing models with the main effects of the genetic and risk variable to the model with these main effects and a multiplicative interaction term. Lastly, we tested whether the association between AR and breast cancer differed by menopausal status at diagnosis and tumour receptor (oestrogen receptor [ER] and progesterone receptor [PR]) status.
The exon 1 CAG repeat was analysed as previously reported [44]. Interaction p values between number of repeats and family history were calculated using likelihood ratio tests comparing the model with main effects for carrying at least one long repeat (cutoffs of ≥22, 23, 25, and 27 repeats) and family history with the model containing these main effects, and an additional interaction term, with homozyotes of the ≥22 allele with no family history as the reference.
Results
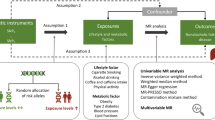
Figure 1 shows the genomic structure of the region around AR. One very common (approximately 70%) haplotype exists, with six lower-prevalence haplotypes being defined each by the htSNPs. The minimum R2 H for these six SNPs was 0.77 in the Japanese, white, and Latina samples from the SNP selection panel. However, these SNPs do not describe haplotype diversity among African-Americans (minimum R2 H = 0.03).
Linkage disequilibrium (LD) at androgen receptor (AR). Linkage disequilibrium plot generated by Haploview [50] showing correlation between all pairs of single nucleotide polymorphisms (SNPs) genotyped to select haplotype-tagging SNPs (ht-SNPs). The 32 SNPs genotyped among the 349 Multiethnic Cohort samples are shown in their physical position along the X chromosome (solid black horizontal line) and relative to the AR gene (depicted above the X chromosome plot). htSNPs selected are shown by arrows. Although two LD blocks are shown (black outline in LD plot), high correlation between the blocks allowed for the analysis of the htSNPs as one block.
A total of 5,603 cases and 7,480 controls were available for genotyping. Table 1 shows some of the baseline characteristics of these cases and controls. Genotyping success for each polymorphism was greater than 94%, and samples not yielding a genotype for a given SNP were removed from analyses for that SNP. Samples not yielding at least one genotype were removed from haplotype analyses, for a total of 5,584 cases and 7,459 controls. No associations with breast cancer or heterogeneity of risk estimates across the participating cohorts were observed for any individual SNP (Table 2) or haplotype tagged by these SNPs (Table 3). No differences in haplotype distribution were observed between ER+ (n = 2,543) and ER- (n = 590) cases (global p value = 0.61), PR+ (n = 2,158) and PR- (n = 860) cases (global p value = 0.51), or localised (n = 2,964) and metastatic (n = 1,646) cases (global p value = 0.43). No statistically significant interactions were observed between haplotypes and common breast cancer risk factors such as family history (yes/no), BMI (≤25, >25), age at first full-term pregnancy (nulliparous, ≤24, >24), or alcohol consumption (non-drinkers, ≤5 g/day, >5 g/day) (p interaction = 0.13, 0.16, 0.14, and 0.28, respectively). These results were not materially different after excluding African-American women from the MEC (344 cases and 426 controls).
Data from further follow-up of the NHS and the WHS did not support the previous findings of interaction between the AR CAG repeat and family history on breast cancer risk in the NHS with follow-up to 1996 [46]. No statistically significant interactions between longer AR CAG repeat length and positive family history were observed in either the further NHS follow-up or the WHS. The decrease in risk associated with shorter repeats among family history positive cases as previously reported [46] was not observed (Table 4).
Discussion
One of the main aims of the BPC3 was to overcome limitations of prior studies by increasing sample size and, therefore, power of the study. By choosing genes involved in the synthesis, metabolism, and signaling of sex hormones, we aimed to maximise the possibility of finding alleles that predispose to breast cancer. Although the AR gene is a likely candidate gene, no association between polymorphisms in the AR gene and breast cancer risk was observed, despite the large sample size (5,603 cases and 7,480 controls) and systematic approach of this study.
In a previous study [46], shorter alleles of the CAG repeat polymorphism in exon 1 of the AR gene were associated with decreased risk of disease in women with a family history of breast cancer in the NHS. Adding samples from further follow-up cycles of the NHS, as well as samples from the WHS, we were unable to confirm this initial finding.
Mutations in genes such as BRCA1 (breast cancer 1, early onset) and BRCA2, although highly penetrant, are of low prevalence in the general population. Very few common polymorphisms have been shown to be associated with breast cancer risk. Using a candidate gene approach to select genes of possible interest in breast cancer etiology has also yielded very few breast cancer-susceptibility loci. One possible explanation for the lack of consistent association between common polymorphisms and breast cancer risk in individual studies is that the change in risk associated with common variants is too low to detect in individual studies and results that are reported may reflect publication bias.
The 95% confidence intervals in our study were narrow and exclude a substantial association between common variants in the AR gene with breast cancer risk. A concern that is more specific to the AR gene is that, due to the gene's location on the X chromosome, X chromosome inactivation could bias risk estimates associated with a causal allele toward the null. Such bias would be especially likely if the same X chromosome (either maternal or paternal) were inactivated in all breast tissue within each woman. However, X chromosome inactivation occurs very early in embryonic development and differs between lobes within the same breast [49]. Assuming a low-penetrance allele (as hypothesised here), women who are heterozygous for a putative risk allele on the X chromosome are still at approximately half the risk of developing breast cancer as women who are homozygous for the same allele, as approximately half (from random inactivation) of the breast cells would not express or be exposed to the risk allele, compared with all breast cells expressing the risk allele among homozygotes. This somewhat limits the possibility that X chromosome inactivation patterns could bias risk estimates toward the null. Optimally, tumour tissue from heterozygous women would be analysed to determine which allele is inactivated; however, this is not possible in the present study, because tumour specimens are not available.
Due to the low numbers of premenopausal women in our study, we cannot exclude the AR gene as a susceptibility locus for breast cancer occurring before menopause. Additionally, although the MEC does provide information from non-Caucasian individuals, there are not a sufficient number of samples, and htSNPs selected to describe genetic variation in Caucasians is not sufficient among African-Americans to definitively exclude polymorphisms in the AR gene as breast cancer-susceptibility alleles except in Caucasians. Among the latter, neither common variants nor the CAG repeat in exon 1 of the AR gene is associated with risk of postmenopausal breast cancer.
Conclusion
Common polymorphisms in the AR gene are not associated with breast cancer risk among postmenopausal Caucasian women.
Abbreviations
- AR:
-
androgen receptor
- BMI:
-
body mass index
- BPC3:
-
Breast and Prostate Cancer Cohort Consortium
- EPIC:
-
European Prospective Investigation into Cancer and Nutrition
- ER:
-
oestrogen receptor
- htSNP:
-
haplotype-tagging single nucleotide polymorphism
- MEC:
-
Multiethnic Cohort
- NHS:
-
Nurses' Health Study
- OR:
-
odds ratio
- PR:
-
progesterone receptor
- SNP:
-
single nucleotide polymorphism
- WHS:
-
Women's Health Study.
References
Birrell SN, Bentel JM, Hickey TE, Ricciardelli C, Weger MA, Horsfall DJ, Tilley WD: Androgens induce divergent proliferative responses in human breast cancer cell lines. J Steroid Biochem Mol Biol. 1995, 52: 459-467. 10.1016/0960-0760(95)00005-K.
Marugo M, Bernasconi D, Miglietta L, Fazzuoli L, Ravera F, Cassulo S, Giordano G: Effects of dihydrotestosterone and hydroxyflutamide on androgen receptors in cultured human breast cancer cells (EVSA-T). J Steroid Biochem Mol Biol. 1992, 42: 547-554. 10.1016/0960-0760(92)90268-N.
Ortmann J, Prifti S, Bohlmann MK, Rehberger-Schneider S, Strowitzki T, Rabe T: Testosterone and 5 alpha-dihydrotestosterone inhibit in vitro growth of human breast cancer cell lines. Gynecol Endocrinol. 2002, 16: 113-120.
Rannevik G, Jeppsson S, Johnell O, Bjerre B, Laurell-Borulf Y, Svanberg L: A longitudinal study of the perimenopausal transition: altered profiles of steroid and pituitary hormones, SHBG and bone mineral density. Maturitas. 1995, 21: 103-113. 10.1016/0378-5122(94)00869-9.
Zumoff B, Strain GW, Miller LK, Rosner W: Twenty-four-hour mean plasma testosterone concentration declines with age in normal premenopausal women. J Clin Endocrinol Metab. 1995, 80: 1429-1430. 10.1210/jc.80.4.1429.
Longcope C, Franz C, Morello C, Baker R, Johnston CC: Steroid and gonadotropin levels in women during the peri-menopausal years. Maturitas. 1986, 8: 189-196. 10.1016/0378-5122(86)90025-3.
Bancroft J, Cawood EH: Androgens and the menopause: a study of 40–60-year-old women. Clin Endocrinol (Oxf). 1996, 45: 577-587. 10.1046/j.1365-2265.1996.00846.x.
Labrie F, Belanger A, Cusan L, Gomez JL, Candas B: Marked decline in serum concentrations of adrenal C19 sex steroid precursors and conjugated androgen metabolites during aging. J Clin Endocrinol Metab. 1997, 82: 2396-2402. 10.1210/jc.82.8.2396.
Burger HG, Dudley EC, Cui J, Dennerstein L, Hopper JL: A prospective longitudinal study of serum testosterone, dehydroepiandrosterone sulfate, and sex hormone-binding globulin levels through the menopause transition. J Clin Endocrinol Metab. 2000, 85: 2832-2838. 10.1210/jc.85.8.2832.
Cauley JA, Lucas FL, Kuller LH, Stone K, Browner W, Cummings SR: Elevated serum estradiol and testosterone concentrations are associated with a high risk for breast cancer. Study of Osteoporotic Fractures Research Group. Ann Intern Med. 1999, 130: 270-277.
Hankinson SE, Willett WC, Manson JE, Colditz GA, Hunter DJ, Spiegelman D, Barbieri RL, Speizer FE: Plasma sex steroid hormone levels and risk of breast cancer in postmenopausal women. J Natl Cancer Inst. 1998, 90: 1292-1299. 10.1093/jnci/90.17.1292.
Zeleniuch-Jacquotte A, Bruning PF, Bonfrer JM, Koenig KL, Shore RE, Kim MY, Pasternack BS, Toniolo P: Relation of serum levels of testosterone and dehydroepiandrosterone sulfate to risk of breast cancer in postmenopausal women. Am J Epidemiol. 1997, 145: 1030-1038.
Thomas HV, Key TJ, Allen DS, Moore JW, Dowsett M, Fentiman IS, Wang DY: A prospective study of endogenous serum hormone concentrations and breast cancer risk in post-menopausal women on the island of Guernsey. Br J Cancer. 1997, 76: 401-405.
Berrino F, Muti P, Micheli A, Bolelli G, Krogh V, Sciajno R, Pisani P, Panico S, Secreto G: Serum sex hormone levels after menopause and subsequent breast cancer. J Natl Cancer Inst. 1996, 88: 291-296.
Dorgan JF, Longcope C, Stephenson HE, Falk RT, Miller R, Franz C, Kahle L, Campbell WS, Tangrea JA, Schatzkin A: Relation of prediagnostic serum estrogen and androgen levels to breast cancer risk. Cancer Epidemiol Biomarkers Prev. 1996, 5: 533-539.
Garland CF, Friedlander NJ, Barrett-Connor E, Khaw KT: Sex hormones and postmenopausal breast cancer: a prospective study in an adult community. Am J Epidemiol. 1992, 135: 1220-1230.
Wysowski DK, Comstock GW, Helsing KJ, Lau HL: Sex hormone levels in serum in relation to the development of breast cancer. Am J Epidemiol. 1987, 125: 791-799.
Chamberlain NL, Driver ED, Miesfeld RL: The length and location of CAG trinucleotide repeats in the androgen receptor N-terminal domain affect transactivation function. Nucleic Acids Res. 1994, 22: 3181-3186.
Kazemi-Esfarjani P, Trifiro MA, Pinsky L: Evidence for a repressive function of the long polyglutamine tract in the human androgen receptor: possible pathogenetic relevance for the (CAG)n-expanded neuronopathies. Hum Mol Genet. 1995, 4: 523-527.
Tut TG, Ghadessy FJ, Trifiro MA, Pinsky L, Yong EL: Long polyglutamine tracts in the androgen receptor are associated with reduced trans-activation, impaired sperm production, and male infertility. J Clin Endocrinol Metab. 1997, 82: 3777-3782. 10.1210/jc.82.11.3777.
Irvine RA, Ma H, Yu MC, Ross RK, Stallcup MR, Coetzee GA: Inhibition of p160-mediated coactivation with increasing androgen receptor polyglutamine length. Hum Mol Genet. 2000, 9: 267-274. 10.1093/hmg/9.2.267.
Giovannucci E, Stampfer MJ, Krithivas K, Brown M, Dahl D, Brufsky A, Talcott J, Hennekens CH, Kantoff PW: The CAG repeat within the androgen receptor gene and its relationship to prostate cancer. Proc Natl Acad Sci USA. 1997, 94: 3320-3323. 10.1073/pnas.94.7.3320.
Irvine RA, Yu MC, Ross RK, Coetzee GA: The CAG and GGC microsatellites of the androgen receptor gene are in linkage disequilibrium in men with prostate cancer. Cancer Res. 1995, 55: 1937-1940.
Ingles SA, Ross RK, Yu MC, Irvine RA, La Pera G, Haile RW, Coetzee GA: Association of prostate cancer risk with genetic polymorphisms in vitamin D receptor and androgen receptor. J Natl Cancer Inst. 1997, 89: 166-170. 10.1093/jnci/89.2.166.
Stanford JL, Just JJ, Gibbs M, Wicklund KG, Neal CL, Blumenstein BA, Ostrander EA: Polymorphic repeats in the androgen receptor gene: molecular markers of prostate cancer risk. Cancer Res. 1997, 57: 1194-1198.
Hakimi JM, Schoenberg MP, Rondinelli RH, Piantadosi S, Barrack ER: Androgen receptor variants with short glutamine or glycine repeats may identify unique subpopulations of men with prostate cancer. Clin Cancer Res. 1997, 3: 1599-1608.
Ekman P, Gronberg H, Matsuyama H, Kivineva M, Bergerheim US, Li C: Links between genetic and environmental factors and prostate cancer risk. Prostate. 1999, 39: 262-268. 10.1002/(SICI)1097-0045(19990601)39:4<262::AID-PROS6>3.0.CO;2-P.
Hsing AW, Gao YT, Wu G, Wang X, Deng J, Chen YL, Sesterhenn IA, Mostofi FK, Benichou J, Chang C: Polymorphic CAG and GGN repeat lengths in the androgen receptor gene and prostate cancer risk: a population-based case-control study in China. Cancer Res. 2000, 60: 5111-5116.
Rebbeck TR, Kantoff PW, Krithivas K, Neuhausen S, Blackwood MA, Godwin AK, Daly MB, Narod SA, Garber JE, Lynch HT, et al: Modification of BRCA1-associated breast cancer risk by the polymorphic androgen-receptor CAG repeat. Am J Hum Genet. 1999, 64: 1371-1377. 10.1086/302366.
Spurdle AB, Antoniou AC, Duffy DL, Pandeya N, Kelemen L, Chen X, Peock S, Cook MR, Smith PL, Purdie DM, et al: The androgen receptor CAG repeat polymorphism and modification of breast cancer risk in BRCA1 and BRCA2 mutation carriers. Breast Cancer Res. 2005, 7: R176-R183. 10.1186/bcr971.
Spurdle AB, Dite GS, Chen X, Mayne CJ, Southey MC, Batten LE, Chy H, Trute L, McCredie MR, Giles GG, et al: Androgen receptor exon 1 CAG repeat length and breast cancer in women before age forty years. J Natl Cancer Inst. 1999, 91: 961-966. 10.1093/jnci/91.11.961.
Dunning AM, McBride S, Gregory J, Durocher F, Foster NA, Healey CS, Smith N, Pharoah PD, Luben RN, Easton DF, et al: No association between androgen or vitamin D receptor gene polymorphisms and risk of breast cancer. Carcinogenesis. 1999, 20: 2131-2135. 10.1093/carcin/20.11.2131.
Giguere Y, Dewailly E, Brisson J, Ayotte P, Laflamme N, Demers A, Forest VI, Dodin S, Robert J, Rousseau F: Short polyglutamine tracts in the androgen receptor are protective against breast cancer in the general population. Cancer Res. 2001, 61: 5869-5874.
Kadouri L, Easton DF, Edwards S, Hubert A, Kote-Jarai Z, Glaser B, Durocher F, Abeliovich D, Peretz T, Eeles RA: CAG and GGC repeat polymorphisms in the androgen receptor gene and breast cancer susceptibility in BRCA1/2 carriers and non-carriers. Br J Cancer. 2001, 85: 36-40. 10.1054/bjoc.2001.1777.
Yeap BB, Wilce JA, Leedman PJ: The androgen receptor mRNA. Bioessays. 2004, 26: 672-682. 10.1002/bies.20051.
Brys M, Wojcik M, Romanowicz-Makowska H, Krajewska WM: Androgen receptor status in female breast cancer: RT-PCR and Western blot studies. J Cancer Res Clin Oncol. 2002, 128: 85-90. 10.1007/s004320100294.
Hunter DJ, Riboli E, Haiman CA, Albanes D, Altshuler D, Chanock SJ, Haynes RB, Henderson BE, Kaaks R, Stram DO, et al: A candidate gene approach to searching for low-penetrance breast and prostate cancer genes. Nat Rev Cancer. 2005, 5: 977-985. 10.1038/nrc1754.
Calle EE, Rodriguez C, Jacobs EJ, Almon ML, Chao A, McCullough ML, Feigelson HS, Thun MJ: The American Cancer Society Prevention Study II Nutrition Cohort: rationale, study design and baseline characteristics. Cancer. 2002, 94: 2490-2501. 10.1002/cncr.101970.
Riboli E, Hunt KJ, Slimani N, Ferrari P, Norat T, Fahey M, Charrondiere UR, Hemon B, Casagrande C, Vignat J, et al: European Prospective Investigation into Cancer and Nutrition (EPIC): study populations and data collection. Public Health Nutr. 2002, 5: 1113-1124. 10.1079/PHN2002394.
Colditz GA, Hankinson SE: The Nurses' Health Study: lifestyle and health among women. Nat Rev Cancer. 2005, 5: 388-396. 10.1038/nrc1608.
Rexrode KM, Lee IM, Cook NR, Hennekens CH, Buring JE: Baseline characteristics of participants in the Women's Health Study. J Womens Health Gend Based Med. 2000, 9: 19-27. 10.1089/152460900318911.
Kolonel LN, Henderson BE, Hankin JH, Nomura AM, Wilkens LR, Pike MC, Stram DO, Monroe KR, Earle ME, Nagamine FS: A multiethnic cohort in Hawaii and Los Angeles: baseline characteristics. Am J Epidemiol. 2000, 151: 346-357.
Stram DO, Haiman CA, Hirschhorn JN, Altshuler D, Kolonel LN, Henderson BE, Pike MC: Choosing haplotype-tagging SNPS based on unphased genotype data using a preliminary sample of unrelated subjects with an example from the Multiethnic Cohort Study. Hum Hered. 2003, 55: 27-36. 10.1159/000071807.
USC/Norris MEC Genetics homepage. [http://www.uscnorris.com/mecgenetics/CohortGCKView.aspx]
Packer BR, Yeager M, Staats B, Welch R, Crenshaw A, Kiley M, Eckert A, Beerman M, Miller E, Bergen A, et al: SNP500 Cancer: a public resource for sequence validation and assay development for genetic variation in candidate genes. Nucleic Acids Res. 2004, D528-D532. 10.1093/nar/gkh005. 32 Database
Haiman CA, Brown M, Hankinson SE, Spiegelman D, Colditz GA, Willett WC, Kantoff PW, Hunter DJ: The androgen receptor CAG repeat polymorphism and risk of breast cancer in the Nurses' Health Study. Cancer Res. 2002, 62: 1045-1049.
Kraft P, Cox DG, Paynter RA, Hunter D, De Vivo I: Accounting for haplotype uncertainty in association studies: a comparison of simple and flexible techniques. Genet Epidemiol. 2005, 28: 261-272. 10.1002/gepi.20061.
Zaykin DV, Westfall PH, Young SS, Karnoub MA, Wagner MJ, Ehm MG: Testing association of statistically inferred haplotypes with discrete and continuous traits in samples of unrelated individuals. Hum Hered. 2002, 53: 79-91. 10.1159/000057986.
Tsai YC, Lu Y, Nichols PW, Zlotnikov G, Jones PA, Smith HS: Contiguous patches of normal human mammary epithelium derived from a single stem cell: implications for breast carcinogenesis. Cancer Res. 1996, 56: 402-404.
Barrett JC, Fry B, Maller J, Daly MJ: Haploview: analysis and visualization of LD and haplotype maps. Bioinformatics. 2005, 21: 263-265. 10.1093/bioinformatics/bth457.
Acknowledgements
We thank the participants in the component cohort studies and the expert contributions of Hardeep Ranu, Craig Labadie, Lisa Cardinale, Shamika Ketkar (Harvard University), Robert Welch, Cynthia Glaser, Laurie Burdett (National Cancer Institute), Loreall Pooler (University of Southern California), and Laure Dossus and James McKay (EPIC).
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
DGC, H Blanché, CLP, EEC, GAC, and MCP made up the writing committee for this work and were responsible for data analyses, manuscript preparation, and editing. NB and MF performed the htSNP selection and contributed substantially to manuscript editing. SC, FC, CAH, PK, DOS, and MY provided expertise in genotyping and results analyses, as well as manuscript editing. DA, NEA, PA, GB, H Boeing, JB, FC-C, HSF, SEH, BEH, RH, DJH, RK, LK, LL, EL, DP, PP, ER, MT, AT, and DT contributed substantially to sample collection and manuscript editing. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Cox, D.G., Blanché, H., Pearce, C.L. et al. A comprehensive analysis of the androgen receptor gene and risk of breast cancer: results from the National Cancer Institute Breast and Prostate Cancer Cohort Consortium (BPC3). Breast Cancer Res 8, R54 (2006). https://doi.org/10.1186/bcr1602
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/bcr1602