Abstract
The clinical spectrum of the anti-phospholipid syndrome (APS) is not limited to vascular thrombosis or miscarriages but includes additional manifestations that cannot be explained solely by a thrombophilic state. Anti-cardiolipin, anti-beta2 glycoprotein I (anti-β2GPI) and lupus anticoagulant (LA) assays are not only the formal diagnostic and classification laboratory tools but also parameters to stratify the risk to develop the clinical manifestations of the syndrome. In particular, anti-β2GPI antibodies reacting with an immunodominant epitope on domain I of the molecule were reported as the prevalent specificity in APS patients, correlating with a more aggressive clinical picture. Several laboratory assays to improve the diagnostic and predictive power of the standard tests have been proposed. Plates coated with the phosphatidylserine-prothrombin complex for detecting antibodies represent a promising laboratory tool correlating with LA and with clinical manifestations. Anti-phospholipid antibodies can be found in patients with full-blown APS, in those with thrombotic events or obstetric complications only or in asymptomatic carriers. An inflammatory second hit is required to increase the presence of β2GPI in vascular tissues, eventually triggering thrombosis. Post-transcriptional modifications of circulating β2GPI, different epitope specificities or diverse anti-β2GPI antibody-induced cell signaling have all been suggested to affect the clinical manifestations and/or to modulate their occurrence.
Similar content being viewed by others
Review
The current clinical spectrum of anti-phospholipid syndrome
Formal clinical classification criteria
The revised classification criteria for anti-phospholipid syndrome (APS), commonly used as a diagnostic tools for the syndrome, include a history of venous or arterial thrombosis and/or of pregnancy morbidity in the presence of persistent anti-phospholipid antibody (aPL) positivity (Table 1) [1]. The most common vascular manifestations are deep venous thrombosis of lower limbs, pulmonary embolism and cerebral ischemic attack; early and late miscarriages are the major features of obstetric APS [1, 2]. In the catastrophic variant of APS, multiple small-vessel thrombotic events occur at different sites, in association with manifestations of the systemic inflammatory response syndrome [3].
Clinical manifestations not yet considered as classification criteria
From the first definition of the disease, the clinical spectrum of APS has notably extended and many other manifestations have been described [4]. Thrombocytopenia, heart valve disease (valve thickening, vegetations and regurgitation), nephropathy, livedo reticularis and skin ulcers are relatively common features of APS but are not included in the classification criteria because of their low specificity (Table 2) [5–9].
In addition to thrombo-occlusive events in the cerebral circulation, a wide range of 'non-criteria' neurological manifestations have been associated with aPL, even though in some cases such association is still controversial. Examples include untreatable headache and migraine, epilepsy, chorea, ocular manifestations such as amaurosis fugax and retinal vessel thrombosis [10, 11]. A clinical syndrome and/or magnetic resonance imaging resembling multiple sclerosis has also been described in APS, raising the issue of a correct differential diagnosis [10].
Persistent aPL positivity has been related to cognitive impairment in systemic lupus erythematosus (SLE) patients, even if recent studies in very large SLE cohorts have not confirmed such an association [11]. Although scant, studies in primary APS have reported a high predominance of cognitive deficits involving attention and verbal fluency [12, 13]. In addition, several authors reported the occurrence of chronic or recurrent ischemic events affecting small or large cerebral vessels and leading to multi-infarct dementia [1].
Further manifestations affecting different organs or tissues have been described in APS patients. However, their association with aPL is still a matter of research mainly because of the anecdotal nature of the reports or the presence of other underlying disorders (diffuse alveolar hemorrhage, myocardial dysfunction, transverse myelopathy, Guillain-Barré syndrome and multiple mononeuropathy, sensorineural hearing loss or vertigo due to middle ear involvement, splinter hemorrhages and anetoderma [1]).
Diagnostic laboratory tools
Classification laboratory assays
Laboratory criteria for formal APS classification currently include three aPL assays: one based on coagulation tests to reveal the presence of lupus anticoagulant (LA) and two solid phase assays to detect IgG/IgM antibodies targeting cardiolipin (CL)/beta2 glycoprotein I (β2GPI) complexes or β2GPI alone (Table 1). Persistent medium/high positivity (12 weeks apart) of at least one of these tests is mandatory [1].
Risk stratification
According to the revised classification criteria, APS patients should be divided into four categories: category I includes patients with more than one positive test in any combination, while patients with a single positive test should be classified in category II (IIA if LA-positive, IIb if positive for antibodies against CL (aCLs), IIc if positive for anti-β2GPI antibodies) [1]. Triple positivity, defined by the presence of LA and medium/high titers of aCL and anti-β2GPI antibodies (above the 99th percentile), is the most predictive profile for clinical manifestations and recurrences despite conventional treatment [14, 15].
There is growing evidence that patients in category II have a lesser risk to develop APS manifestations. LA was reported to be the most predictive test. LA can be mediated by both anti-β2GPI and anti-prothrombin (aPT) antibodies [16]. However, β2GPI-dependent LA was found to be a stronger risk factor for thrombosis and miscarriages than aPT-dependent LA [17, 18]. aCL positivity alone is not associated with an increased risk of thrombosis or pregnancy loss [16, 17, 19]. Data on anti-β2GPI antibodies are more controversial, maybe because the assay is less standardized [17]. Accordingly, Otomo and colleagues [20] have recently validated a scoring system to quantify the thrombotic or obstetric risk depending on aPL profiles.
Clinical events are more robustly associated with aPLs of the IgG isotype, an isolated positivity for aCLs or anti-β2GPI antibodies of the IgM isotype being rarely detected in APS cohorts. Patients carrying both aCL/anti-β2GPI antibody isotypes display a higher risk of developing clinical events [21]. Some investigators have recently proposed that aCLs and anti-β2GPI IgA antibodies be included in the APS laboratory criteria. However, this is not supported by available data: the detection of a single IgA aPL positivity is more commonly associated with non-criteria manifestations, while IgA testing has not been shown to increase the diagnostic accuracy for APS [22]. Interestingly, this is not consistent with in vivo findings, which are supportive for a pathogenic role of IgA β2GPI-dependent aPLs in mediating thrombus formation [23].
While it is well accepted that aPLs confer a prothrombotic susceptibility when at high titers, controversies have recently arisen about the clinical meaning of low-titer aPLs in pregnancy morbidity. A few studies have reported that women with persistent low-titer aPL positivity display an obstetric outcome comparable to the general population [17]. On the other hand, a recent study showed that low-titer aCL and anti-β2GPI antibody positivity (between the 95th and 99th percentiles) accurately identifies women with aPL-related pregnancy complications [24].
Risk stratification for thrombotic events should also take into account the presence of traditional cardiovascular factors such as systemic inflammatory conditions (infectious or autoimmune), inherited thrombophilia, arterial hypertension, cigarette smoking and dyslipidemia [1]. Risk-factors for pregnancy failure include low complement levels, decreased platelet counts and a previous history of thrombosis and pregnancy failure [15].
Non-classification laboratory assays
Additional laboratory tests to detect aPLs have been reported: the most important 'non-classification' tests still deal with the two major phospholipid (PL)-binding proteins thought to represent the true antigenic targets for aPL: β2GPI and prothrombin (PT) [16]. However, other autoantigens have been described that are a matter of debate and research (Table 3).
Anti-prothrombin antibodies
To be antigenically recognized, human PT has to be either coated on activated plates or exposed to immobilized anionic phosphatidylserine (PS) via calcium ions. ELISAs to detect antibodies against the PS/PT complex (aPS/PT antibodies) identify a partially different autoantibody population from the assay using PT as the only antigen [25]. A contentious issue concerns the potential cross-reactivity between aPS/PT and anti-β2GPI antibodies; however, human anti-β2GPI monoclonals or affinity-purified anti-β2GPI polyclonal IgG antibodies obtained from a serum reacting with both β2GPI and PS/PT have been shown to react towards β2GPI only [26].
In vitro experimental findings suggest that aPTs exert thrombogenic effects interfering with fluid phase components of coagulation and activating endothelial cells (ECs). Evidence from animal models is rather weak, however, mainly because of the lack of cross-reactivity of human aPTs with animal PT [25].
The wide variability in epitope specificities and detection methods drives a disparity across available studies about the prevalence and clinical significance of aPTs. The prevalence of antibodies targeting PT depends also on selection of study populations: when considering solely individuals with LA, the positivity rate increases up to 85% and 88% for aPTs and aPS/PTs, respectively [25]. Similarly, the clinical significance of aPTs in both primary and secondary APS is still a matter of debate. Some studies showed that aPTs are an independent risk factor for either venous or arterial thrombosis, while others have failed to demonstrate such an association. On the other hand, most of the studies addressing the clinical significance of aPS/PTs have highlighted a significant association with aPL-associated manifestations, in particular venous thrombosis. Consistently, a systematic review did not find any correlation between aPTs and clinical events, while a more recent one found that aPS/PTs are a stronger risk factor for arterial and venous thrombosis than aPTs [27]. Much more controversial remains the association of aPTs and aPL-related pregnancy morbidity (Tables 4 and 5).
aPS/PTs have been proposed as a surrogate test for LA and as an additional serological marker of APS, to be performed with other aPL tests to improve diagnosis. Noteworthy, LA together with aβ2GPI and aPS/PT antibodies has recently been identified to display the best diagnostic accuracy for both vascular and obstetric APS among 23 possible combinations of six aPL assays (LA, aCLs, anti-β2GPI antibodies, aPTs, aPS/PTs, and anti-phosphatidylethanolamine antibodies (aPEs)) [66]. However, the bulk of evidence is still not solid enough to recommend routine testing for antibodies targeting PT as shown by a summary of all studies available in the literature (Tables 4 and 5).
New assays for anti-β2GPI antibodies: the anti-domain antibodies
β2GPI is a relatively large plasma glycoprotein of 70 kDa with good immunogenic properties. Thus, it is not surprising that APS patients can produce antibodies against several epitopes of the molecule as demonstrated using different experimental approaches. Although the epitope specificity using linear peptides was not originally reported to be associated with specific clinical manifestations of the syndrome, more recently a close association between anti-domain (D)I reactivity and vascular events has been suggested [67].
The reactivity against DI of β2GPI was described for the first time in 2002 but its importance was revealed when a two-step technique was used to characterize β2GPI-dependent aPLs [68]. Specifically, β2GPI coated on hydrophilic but not hydrophobic microtiter plates displays conformational changes that expose DI to the surface, making it more accessible for autoantibody binding. Anti-β2GPI antibodies with DI specificity were found in the majority of APS patients and were significantly associated with LA and vascular thrombosis (mostly venous) [69]. Only in a subsequent multicenter study were they also found to be associated with the obstetric manifestations of the syndrome, although to a lesser extent than with thrombosis [70]. However, some data from the multicenter study are controversial. In fact, no correlation between LA and miscarriages was found, in contrast to several previous publications and the known clinical LA predictive value for miscarriages [17]. High levels of antibodies with comparable specificity and detected by a research ELISA kit have been recently associated with an increased risk for thrombotic events in a prospective cohort of SLE or aPL patients by the same group [71].
Recent studies have demonstrated that patients with multiple positive test results (that is, LA, aCLs and anti-β2GPI autoantibodies particularly of the IgG isotype) display a much higher risk for developing clinical complications [17]. In line with the hypothesis that anti-DI IgG may represent a more predictive aPL profile, these patients tend to have a higher prevalence and higher titers of anti-β2GPI-DI antibodies [72, 73].
Anti-β2GPI-DI IgG antibodies have been found as the most prevalent antibodies not only in primary APS with thrombosis but also in primary APS with pure obstetric disease. Comparable positivity rates were detectable in patients with SLE or undifferentiated connective tissue diseases, while antibodies against DIV or DV were less frequent in the same populations [73]. aPL positive asymptomatic carriers display a less polarized profile, suggesting that anti-DI antibodies may cluster in patients with systemic autoimmune diseases [73]. Interestingly, the two techniques for anti-DI antibodies used in the study (that is, standard ELISA and chemiluminescence immunoassay (CIA)) have been reported to display the same specificity but different sensitivities [74].
Additional epidemiological studies apparently support the diagnostic/predictive value of anti-DI antibodies. IgG reacting with β2GPI in sera from aPL-positive asymptomatic carriers, individuals with leprosy or children with atopic dermatitis have been shown to preferentially recognize epitopes on DIV or DV [68]. Recent studies have suggested that the ratio between anti-β2GPI-DI and anti-β2GPI-DIV/V IgG antibody reactivities can provide important information to discriminate between anti-β2GPI antibodies linked to an autoimmune disease such as APS and antibodies occurring in association with other pathologies [73]. If confirmed in larger studies, this finding would suggest the use of tests for antibodies against the different domains to discriminate between predictive versus non predictive anti-β2GPI antibodies.
In any case, it is difficult to draw definite conclusions on the diagnostic and prognostic value of anti-DI antibodies at this stage. The high prevalence of anti-DI IgG antibodies in patients with medium-high titers of aPLs and multiple positivities in the formal diagnostic tests supports the role of DI as the immunodominant epitope of β2GPI. However, a small but consistent proportion of full-blown APS patients have autoantibodies reacting with different epitopes, suggesting that the assay for the whole molecule cannot be substituted yet [73]. The discrepancies in the clinical associations can be related to the different methodologies used. Besides the two-step assay, three ELISA studies and a CIA employing different DI molecules or peptides have been reported [74, 75]. Although preliminary data seem to indicate that the solid phase assays by two different ELISAs or CIA are comparable, there is no information on the comparison with the two-step assay and the additional ELISAs. Confirmatory studies using multi-center setups and larger prospective patient cohorts are needed to confirm the data.
The fact that the anti-DI antibodies are directed against the immunodominant epitope of β2GPI is supported also by pathogenic studies in animal models. Passive infusion of a synthetic antigenic target peptide DI was shown to protect naïve mice from the thrombogenic effects of human polyclonal aPL IgG fractions [76]. Although the inhibition of thrombus formation as well as expression of adhesion molecule on aortic ECs and tissue factor expression on macrophages were not complete, this finding was thought to represent a proof of concept of the pathogenic role of anti-DI antibodies [76]. More recently, a human monoclonal IgG, specifically reacting with DI, was shown to induce clotting and fetal loss in naïve mice, offering the first direct demonstration of the pathogenic effect of anti-DI antibodies [77]. Interestingly, the anti-DI monoclonal induced clotting via complement activation and only after the concomitant administration of small amounts of lipopolysaccharide. This finding is in line with previous results obtained using polyclonal IgG anti-β2GPI fractions from APS patients and further supports the potential pathogenic role of anti-DI antibodies.
The main epitope of DI has been suggested to be a cryptic and conformation-dependent structure involving different residues located in the proximity of the junction between DI and DII. Fine epitope mapping using short synthetic peptide fragments and mutation experiments have demonstrated that the main epitope on β2GPI-DI is located around amino acid 40 of the molecule with R39-R43 representing the key constituent of the discontinuous epitope [68]. DI of β2GPI is usually hidden, being linked with DII in the circular form of the molecule, the most abundant variant in the circulation. After interaction with anionic PL monolayers or when bound to endotoxin, β2GPI is opened and DI can be presented to the afferent limb of the immune system [69]. In other words, it could be speculated that, unlike the other domains, which can induce tolerance at high antigen concentrations, DI does not. So, even a small amount of DI presented to the immune system can break the tolerance and easily induce specific antibodies.
Antibodies against phosphatidylethanolamine
Phosphatidylethanolamine (PE) is a zwitterionic PL, mainly located in the inner leaflets of biological membranes. Subpopulations of aPE bind to high molecular weight kininogen, leading to the formation of antibody-PE-kininogen trimolecular complexes that enhance thrombin-induced platelet aggregation. PE promotes thrombosis by activating factor X and PT, and works as an anticoagulant potentiating activated protein C activity. The finding that PE in the hexagonal phase inhibits the prolongation of clotting time led to the hypothesis that aPEs might be responsible for the LA phenomenon, despite a lack of a significant association between the two assays [78]. A clear in vivo demonstration of the pathogenic role of aPEs in mediating vascular and obstetric events is lacking.
Antibodies against PE have been described in up to 43% of APS patients, a higher positivity rate compared to healthy controls [78]. In particular, aPE prevalence among women experiencing recurrent pregnancy loss (RPL) has been reported to range between 23 and 31.7% [79]. Overall, available evidence on the clinical role of aPEs is inconsistent and comes from a limited number of studies, being flawed by the small sample size and poor ELISA standardization [78]. Therefore, aPE testing is currently not recommended, with these autoantibodies not yielding increased accuracy in diagnosing APS. Nevertheless, some authors have proposed aPEs as serological markers of seronegative APS, a debated nosological entity characterized by a clinical picture highly suggestive of APS despite persistent aPL undetectability. In patients with otherwise unexplained thrombotic events, the prevalence of aPEs was 18% when detected by ELISA, rising to 30.5% when tested using thin-layer immunostaining [78, 80]. Further, in a multicenter study on 270 thrombotic patients, 63% of 40 aPE-positive subjects had no additional aPL laboratory tests [78].
Antibodies against anionic phospholipids other than cardiolipin
The diagnostic and prognostic roles of several autoantibodies targeting negatively charged PLs other than CL have been evaluated, though not extensively, in the setting of APS.
PS, phosphatidylinositol and phosphatidic acid, three anionic PLs found in the inner and outer membranes of most cells, are among the best-characterized antigens. Noteworthy, in the 1980s aCLs were shown to broadly cross-react with antibodies targeting both PS and phosphatidylinositol. The cross-reactivity was mostly supported by the recognition of the complex of β2GPI with the different anionic PLs. In fact, being a cationic molecule, β2GPI binds efficiently to negatively charged PLs. Hence, the largest part of the cross-reactivity is actually due to the same family of autoantibodies, namely those reacting with β2GPI [81]. As a whole, testing for antibodies against PS (aPSs), phosphatidylinositol and phosphatidic acid does not improve the likelihood of diagnosing APS compared with criteria tests, being therefore not recommended in international guidelines [1].
Nevertheless, aPSs were reported to be promising, with a particular relevance in obstetric APS. In a study on 872 women with RPL, aPSs were the only detectable aPLs in 3.6% of subjects [82]. However, contradictory data have recently emerged: in one study, aPSs were not related to RPL, while other authors identified IgG but not IgM aPSs as associated with RPL. On the other hand, there is no evidence for an association between aPSs and vascular events [82].
Two murine monoclonal antibodies targeting PS (one reacting with both CL and PS and one with PS only) inhibited the development and invasion by trophoblasts, decreased human chorionic gonadotropin levels and retarded syncytiotrophoblast formation. Unfortunately there is no information whether they recognized β2GPI or not [82]. Conversely, the β2GPI dependence was shown to be important in another study in which active immunization with β2GPI-dependent polyclonal human IgG but not IgM aPSs induced fetal resorption via the production of murine β2GPI-dependent IgG aPSs [83]. Discrepancies across available studies justify why APS criteria do not include aPS assays among laboratory tools.
A novel ELISA kit detecting antibodies against a mixture of negatively charged PLs comprising PS, phosphatidic acid and β2GPI (APhL) has been recently introduced to the market. This commercial immunoassay has been suggested to overcome the issue of the low specificity of aCLs, which are frequently detected in infectious conditions such as chronic hepatitis C, leprosy, syphilis, and parvovirus B19 infection among others. Furthermore, the APhL assay displays higher positive and negative predictive values for APS diagnosis compared to two commercially available aCL assays [84]. In a cohort of 158 SLE patients, multivariate analysis revealed an association between APhL and thrombotic events, particularly arterial [85].
Antibodies against vimentin
Proteomic analysis of endothelial-surface membrane proteins in sera from patients with so-called seronegative APS led to the identification of vimentin as a strong autoantigen. Vimentin, a ubiquitous cytoskeleton intermediate filament protein, has been shown to bind CL in vitro. In one cohort of patients, antibodies against vimentin/CL were described in 55% of seronegative APS and 92% of full-blown APS patients [82]. However, antibodies against vimentin/CL have also been reported in aPL-negative SLE and rheumatoid arthritis subjects without any clinical manifestation suggestive of APS, thus weakening the specificity of such a diagnostic marker [82].
Annexins: annexin A5 resistance assay and autoantibodies against annexin A5 and annexin A2
Annexins are a family of ubiquitous calcium-dependent PL-binding proteins. Annexin (Ann)A5 is a potent anticoagulant protein mainly found in trophoblasts and vascular ECs. Upon binding to anionic PLs, it undergoes oligomerization to form a protective shield against coagulation enzymes. β2GPI-dependent aPLs have been shown to interfere with the protective binding of AnnA5 to the endothelium, hence leading to thrombosis. A novel two-stage coagulation assay to establish the AnnA5 resistance has been developed; patients with coagulation time lower than the reference are considered AnnA5-resistant [81, 82]. Data from five studies revealed that 52% of APS patients were AnnA5-resistant, in comparison with 2 to 5% of controls and seronegative subjects [81]. Resistance to AnnA5 anticoagulant activity was found to inversely correlate with titers of IgG antibodies targeting DI in both thrombotic and obstetric APS [81]. Future studies will assess whether this functional test may allow the identification of specific subsets of pathogenic anti-β2GPI antibodies. The clinical significance of serum autoantibodies against AnnA5 has also been investigated: in one study, no association was reported between these autoantibodies and vascular events, while inconsistencies emerged across different studies in obstetric APS [81, 82].
AnnA2, a cofactor for plasmin generation and cell-surface localization of fibrinolytic activity, has been identified as a receptor mediating β2GPI binding to ECs. Autoantibodies against AnnA2 have been demonstrated to exert a prothrombotic activity by activating ECs, inducing tissue factor expression and blocking tissue plasminogen activator-induced plasminogen activation in vitro. A high prevalence of AnnA2 antibodies has been described in patients with APS, but also in some other autoimmune conditions, thus lowering the specificity of this biomarker [86].
More than just autoantibodies
The presence of aPLs, even if persistent over time, does not explain the full spectrum of APS. For example, a comparable aPL profile can be associated with vascular but not obstetric manifestations and, in some cases, women with APS and previous miscarriages do not display any vascular events [1, 4]. In other words, autoantibodies with the same autoantigen specificity and titers have been associated with different clinical pictures and found to support diverse pathogenic mechanisms in experimental models [16].
β2GPI-dependent aPL IgG fractions were reported to affect signaling pathways in monocytes and trophoblast cell lines in different ways depending on whether they were obtained from patients with vascular thrombosis or from women with aPL-related miscarriages only [87]. Hence, the eventual clinical picture has been linked to autoantibodies with the same antigen specificity but different biological effects: induction of a pro-thrombotic and inflammatory phenotype in monocytes by β2GPI-dependent IgG antibodies from vascular APS patients and inhibition of trophoblast development by β2GPI-dependent IgG antibodies from obstetric APS patients [87].
It is still unclear whether these different effects can be related to diverse IgG epitope specificity. The use of these IgG fractions in animal models of aPL-induced thrombosis or fetal loss could further support such an elegant hypothesis in vivo.
Vascular and the obstetric APS have been suggested to represent two different variants of the syndrome [88]. The most striking difference is represented by the need of a second hit for triggering thrombosis in naive animals passively infused with human aPLs, while this is not apparently required in models of fetal loss. In fact, the infusion of aPL IgG fractions in pregnant naive mice can itself induce fetal loss and growth retardation. It has been recently demonstrated that β2GPI displays a peculiar tissue distribution in resting naive animals, being detectable only at the level of uterine endothelium but not in other vascularized tissues [89]. So the presence of anti-β2GPI antibodies can affect pregnancy outcome in resting animals but it does not trigger any vascular thrombosis. Animal pre-treatment with small amounts of lipopolysaccharide may induce the presence of β2GPI in vascularized tissues and only then can aPLs react with the target, activate the complement cascade and induce thrombosis [89]. Accordingly, it has been suggested that the modulation of β2GPI tissue distribution by inflammatory stimuli may represent an additional variable able to affect the ability of the antibodies to induce the vascular manifestations of the syndrome [16, 89].
Post-transcriptional modifications of β2GPI, such as oxidation, have been shown to affect autoantibody binding [90]. For example, autoimmune anti-β2GPI IgG antibodies react more strongly with plates coated with oxidized β2GPI than antibodies obtained after active immunization in naive animals. Moreover, plasma levels of oxidized β2GPI have been found to be increased in sera of APS patients. Altogether, these findings suggest that increased levels of post-transcriptionally modified β2GPI and the higher antibody reactivity against the modified molecule may affect the biological consequences of aPL binding [90].
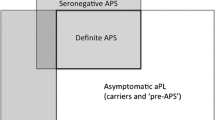
In addition, aPLs can be detected in so-called asymptomatic positive carriers who display the persistent presence of medium to high levels of antibodies but in whom no clinical events can be documented. It has been suggested that the second hit cannot take place in these subjects or that their antibodies display different antigen specificity. In line with the last hypothesis, the epitope specificity of the β2GPI-dependent IgG antibodies in these subjects was found to be more frequently directed against DIV or DV than against DI as in full-blown APS sera [68, 74]. Since the DI epitope is available for the autoantibodies on the open molecule only (for example, when bound to anionic PL monolayers), it has been hypothesized that only these antibodies may be pathogenic. Figure 1 presents a schematic view of the above discussed pathogenic mechanisms.
Schematic views of anti-phospholipid syndrome pathogenic mechanisms. (a) Vascular anti-phospholipid syndrome (APS). Anti-phospholipid antibodies (aPLs) may target different cell types and soluble coagulations factors. Pathogenic aPLs are beta2 glycoprotein I (β2GPI)-dependent and activate complement after an inflammatory stimulus (second hit). Additional variables may affect aPL pathogenicity, such as the ability of antibodies to modulate different cell signaling and to display diverse epitope specificity and reactivity with modified β2GPI. (b) Obstetric APS. β2GPI-dependent aPLs may target trophoblast and decidual cells. β2GPI can be present at the uterine level even in non-pregnant animals and it binds to trophoblast cells (syncytiotrophoblasts). A second hit is not apparently required, and female hormones or the pregnancy itself may be the equivalent of the second hit described for the vascular manifestations. As in vascular APS, the ability of antibodies to modulate different cell signaling and to display diverse epitope specificity and reactivity with modified β2GPI may be additional variables that can affect aPL pathogenicity. APC, activated protein C; C?S, Protein C/S; FII, Factor II; FIXa, Factor IXa, FVIIa, Factor VIIa; FXa, Factor Xa; PT, prothrombin; TF, tissue factor; tPA, tissue plasminogen factor.
Conclusion
The clinical spectrum of APS is more polymorphic than it was thought in the past, making the syndrome much closer to a systemic autoimmune disease. Additional laboratory tests have been proposed in order to improve diagnostic and predictive power, but promising findings have been reported only for anti-PS/PT and anti-DI antibodies.
aPLs play a major pathogenic role in inducing clinical manifestations; however, there is growing evidence that inflammatory stimuli are pivotal for triggering thrombosis, while tissue distribution of the major antigenic target (β2GPI) as well as its post-transcriptional modifications or the fine epitope specificity of anti-β2GPI antibodies may influence the type of clinical events or even their occurrence.
Abbreviations
- β2GPI:
-
beta2 glycoprotein I
- aCL:
-
Anti-cardiolipin antibody
- Ann:
-
Annexin
- aPE:
-
Anti-phosphatidylethanolamine antibody
- aPL:
-
Anti-phospholipid antibody
- aPS:
-
Anti-phosphatidylserine antibody
- APS:
-
Anti-phospholipid syndrome
- aPT:
-
Anti-prothrombin antibody
- CIA:
-
Chemiluminescence immunoassay
- CL:
-
Cardiolipin
- D:
-
Domain
- EC:
-
Endothelial cell
- ELISA:
-
Enzyme-linked immunosorbent assay
- Ig:
-
Immunoglobulin
- LA:
-
Lupus anticoagulant
- PE:
-
Phosphatidylethanolamine
- PL:
-
Phospholipid
- PS:
-
Phosphatidylserine
- PT:
-
Prothrombin
- RPL:
-
Recurrent pregnancy loss
- SLE:
-
Systemic lupus erythematosus.
References
Miyakis S, Lockshin MD, Atsumi T, Branch DW, Brey RL, Cervera R, Derksen RH, DE Groot PG, Koike T, Meroni PL, Reber G, Shoenfeld Y, Tincani A, Vlachoyiannopoulos PG, Krilis SA: International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS). J Thromb Haemost. 2006, 4: 295-306. 10.1111/j.1538-7836.2006.01753.x.
Cervera R, Khamashta MA, Shoenfeld Y, Camps MT, Jacobsen S, Kiss E, Zeher MM, Tincani A, Kontopoulou-Griva I, Galeazzi M, Bellisai F, Meroni PL, Derksen RH, de Groot PG, Gromnica-Ihle E, Baleva M, Mosca M, Bombardieri S, Houssiau F, Gris JC, Quéré I, Hachulla E, Vasconcelos C, Roch B, Fernández-Nebro A, Piette JC, Espinosa G, Bucciarelli S, Pisoni CN, Bertolaccini ML: Euro-Phospholipid Project Group (European Forum on Antiphospholipid Antibodies). Morbidity and mortality in the antiphospholipid syndrome during a 5-year period: a multicentre prospective study of 1000 patients. Ann Rheum Dis. 2009, 68: 1428-1432.
Cervera R, Espinosa G: Update on the catastrophic antiphospholipid syndrome and the 'CAPS Registry'. Semin Thromb Hemost. 2012, 38: 333-338.
Shoenfeld Y, Meroni PL, Toubi E: Antiphospholipid syndrome and systemic lupus erythematosus: are they separate entities or just clinical presentations on the same scale?. Curr Opin Rheumatol. 2009, 21: 495-500. 10.1097/BOR.0b013e32832effdd.
Erkan D, Lockshin MD: Non-criteria manifestations of antiphospholipid syndrome. Lupus. 2010, 19: 424-427. 10.1177/0961203309360545.
Atsumi T, Furukawa S, Amengual O, Koike T: Antiphospholipid antibody associated thrombocytopenia and the paradoxical risk of thrombosis. Lupus. 2005, 14: 499-504. 10.1191/0961203305lu2145rr.
Frances C: Dermatological manifestations of Hughes' antiphospholipid antibody syndrome. Lupus. 2010, 19: 1071-1077. 10.1177/0961203310370343.
Zuily S, Huttin O, Mohamed S, Marie PY, Selton-Suty C, Wahl D: Valvular heart disease in antiphospholipid syndrome. Curr Rheumatol Rep. 2013, 15: 320-
Tektonidou MG: Renal involvement in the antiphospholipid syndrome (APS)-APS nephropathy. Clin Rev Allergy Immunol. 2009, 36: 131-140. 10.1007/s12016-008-8112-z.
Brey RL, Muscal E, Chapman J: Antiphospholipid antibodies and the brain: a consensus report. Lupus. 2011, 20: 153-157. 10.1177/0961203310396748.
Hanly JG, Urowitz MB, Su L, Gordon C, Bae SC, Sanchez-Guerrero J, Romero-Diaz J, Wallace DJ, Clarke AE, Ginzler E, Merrill JT, Isenberg DA, Rahman A, Petri M, Fortin PR, Gladman D, Bruce IN, Steinsson K, Dooley M, Khamashta MA, Alarcón GS, Fessler BJ, Ramsey-Goldman R, Manzi S, Zoma AA, Sturfelt GK, Nived O, Aranow C, Mackay M, Ramos-Casals M: Seizure disorders in systemic lupus erythematosus results from an international, prospective, inception cohort study. Ann Rheum Dis. 2012, 71: 1502-1509.
Tektonidou MG, Varsou N, Kotoulas G, Antoniou A, Moutsopoulos HM: Cognitive deficits in patients with antiphopholipid syndrome. Arch Intern Med. 2006, 166: 2278-2284. 10.1001/archinte.166.20.2278.
Gerosa M, Poletti B, Pregnolato F, Lafronza A, Silani V, Meroni PL, Riboldi P: Antiphospholipid syndrome and systemic lupus erythematosus: what’s new about cognitive impairment. J Neurol. 2009, 256: S190-
Pengo V, Ruffatti A, Legnani C, Testa S, Fierro T, Marongiu F, De Micheli V, Gresele P, Tonello M, Ghirarduzzi A, Bison E, Denas G, Banzato A, Padayattil Jose S, Iliceto S: Incidence of a first thromboembolic event in asymptomatic carriers of high-risk antiphospholipid antibody profile: a multicenter prospective study. Blood. 2011, 118: 4714-4718. 10.1182/blood-2011-03-340232.
Ruffatti A, Tonello M, Visentin MS, Bontadi A, Hoxha A, De Carolis S, Botta A, Salvi S, Nuzzo M, Rovere-Querini P, Canti V, Mosca M, Mitic G, Bertero MT, Pengo V, Boffa MC, Tincani A: Risk factors for pregnancy failure in patients with anti-phospholipid syndrome treated with conventional therapies: a multicentre case–control study. Rheumatology. 2011, 50: 1684-1689. 10.1093/rheumatology/ker139.
Meroni PL, Borghi MO, Raschi E, Tedesco F: Pathogenesis of antiphospholipid syndrome: understanding the antibodies. Nat Rev Rheum. 2011, 7: 330-339. 10.1038/nrrheum.2011.52.
Pengo V, Banzato A, Denas G, Jose SP, Bison E, Hoxha A, Ruffatti A: Correct laboratory approach to APS diagnosis and monitoring. Autoimmun Rev. 2013, 12: 832-834. 10.1016/j.autrev.2012.11.008.
De Laat HB, Derksen RHWM, Urbanus RT, Roest M, de Groot PG: B2-glycoprotein I dependent lupus anticoagulant highly correlates with thrombosis in the antiphospholipid syndrome. Blood. 2004, 104: 3598-3602. 10.1182/blood-2004-03-1107.
Ruffatti A, Del Ross T, Ciprian M, Bertero MT, Sciascia S, Scarpato S, Montecucco C, Rossi S, Caramaschi P, Biasi D, Doria A, Rampudda M, Monica N, Fischetti F, Picillo U, Brucato A, Salvan E, Vittorio P, Meroni P, Tincani A, Antiphospholipid Syndrome Study Group of Italian Society of Rheumatology: Risk factors for a first thrombotic event in antiphospholipid antibody carriers: a prospective multicentre follow-up study. Ann Rheum Dis. 2011, 70: 1083-1086. 10.1136/ard.2010.142042.
Otomo K, Atsumi T, Amengual O, Fujieda Y, Kato M, Oku K, Horita T, Yasuda S, Koike T: Efficacy of the antiphospholipid score for the diagnosis of antiphospholipid syndrome and its predictive value for thrombotic events. Arthritis Rheum. 2012, 64: 504-512. 10.1002/art.33340.
Devreese KM: Antiphospholipid antibodies: evaluation of the thrombotic risk. Thrombosis Res. 2012, 130: S37-S40.
Meijide H, Sciascia S, Sanna G, Khamashta MA, Bertolaccini ML: The clinical relevance of IgA anticardiolipin and IgA anti-β2 glycoprotein I antiphospholipid antibodies. A systematic review. Autoimmun Rev. 2013, 12: 421-425. 10.1016/j.autrev.2012.08.002.
Murthy V, Willis R, Romay-Penabad Z, Ruiz-Limon P, Martinez-Martinez LA, Jatwani S, Jajoria P, Seif A, Alarcon GS, Papalardo E, Liu J, Vilà LM, McGwin G, McNearney TA, Maganti R, Sunkureddi P, Parekh T, Tarantino M, Akhter E, Fang H, Gonzalez EB, Binder WB, Norman GL, Shums Z, Teodorescu M, Reveille JD, Petri M, Pierangeli SP: Value of isolated IgA anti-β2-glycoprotein I positivity in the diagnosis of the antiphospholipid syndrome. Arthritis Rheum. 2013, 65: 3186-3193. 10.1002/art.38131.
Gardiner C, Hills J, Machin SJ, Cohen H: Diagnosis of antiphospholipid syndrome in routine clinical practice. Lupus. 2013, 22: 18-25. 10.1177/0961203312460722.
Pregnolato F, Chighizola C: Phospholipid autoantibodies (non-anticardiolipin)-anti-prothrombin antibodies. The Autoantibodies. Edited by: Shoenfeld Y, Gershwin E, Meroni PL. 2014, New York: Elsevier, 741-749. 3
Pregnolato F, Chighizola CB, Encabo S, Shums Z, Norman GL, Tripodi A, Chantarangkul V, Bertero T, De Micheli V, Borghi MO, Meroni PL: Anti-phosphatidylserine/prothrombin antibodies: an additional diagnostic marker for APS?. Immunologic Res. 2013, 56: 432-438. 10.1007/s12026-013-8421-z.
Sciascia S, Sanna G, Murru V, Roccatello D, Khamashta M, Bertolaccini ML: Anti-prothrombin (aPT) and anti-phosphatidylserine/prothrombin (aPS/PT) antibodies and the risk of thrombosis in the antiphospholipid syndrome: a systematic review. Thromb Haemost. 2014, 111: 354-364.
Fleck RA, Rapaport SI, Rao LVM: Anti-prothrombin antibodies and the lupus anticoagulant. Blood. 1988, 72: 512-519.
Pengo V, Biasiolo A, Brocco T, Tonetto S, Ruffatti A: Autoantibodies to phospholipid-binding plasma proteins in patients with thrombosis and phospholipid-reactive antibodies. Thromb Haemost. 1996, 75: 721-724.
Horback DA, van Oort E, Donders RC, Derksen RH, de Groot PG: Lupus anticoagulant is the strongest risk factor for both venous and arterial thrombosis in patients with systemic lupus erythematosus. Comparison between different assays for the detection of antiphospholipid antibodies. Thromb Haemost. 1996, 76: 916-924.
Puurunen M, Vaarala O, Julkunen H, Aho K, Palosuo T: Antibodies to phospholipid-binding plasma proteins and occurrence of thrombosis in patients with systemic lupus erythematosus. Clin Immunol Immunopathol. 1996, 80: 16-22. 10.1006/clin.1996.0089.
Swadzba J, De Clerck LS, Stevens WJ, Bridts CH, van Cotthem KA, Musial J, Jankowski M, Szczeklik A: Anti-cardiolipin, antibeta2glycoprotein I, antiprothrombin antibodies, and lupus anticoagulant in patients with systemic lupus erythematosus with a history of thrombosis. J Rheumatol. 1997, 24: 1710-1715.
Galli M, Beretta G, Daldossi M, Bevers EM, Barbui T: Different anticoagulant and immunological properties of anti-prothrombin antibodies in patients with antiphospholipid antibodies. Thromb Haemost. 1997, 77: 486-491.
Bertolaccini ML, Atsumi T, Khamashta MA, Amengual O, Hughes GR: Autoantibodies to human prothrombin and clinical manifestations in 207 patients with systemic lupus erythematosus. J Rheumatol. 1998, 25: 1104-1108.
Forastiero R, Martinuzzo ME, Adamczuk Y, Carreras LO: Occurrence of anti-prothrombin antibodies and anti-beta2glycoprotein I antibodies in patients with a history of thrombosis. J Lab Clin Med. 1999, 134: 610-615. 10.1016/S0022-2143(99)90101-4.
Munoz-Rodriguez FJ, Reverter JC, Font J, Tàssies D, Cervera R, Espinosa G, Carmona F, Balasch J, Ordinas A, Ingelmo M: Prevalence and clinical significance of anti-prothrombin antibodies in patients with systemic lupus erythematosus or with primary anti-phospholipid syndrome. Haematologica. 2000, 85: 632-637.
Atsumi T, Ieko M, Bertolaccini ML, Ichikawa K, Tsutsumi A, Matsuura E, Koike T: Association of autoantibodies against the phosphatidylserine-prothrobin complex with manifestations of the antiphospholipid syndrome and in the presence of lupus anticoagulant. Arthritis Rheum. 2000, 43: 1982-1993. 10.1002/1529-0131(200009)43:9<1982::AID-ANR9>3.0.CO;2-2.
Galli M, Dlott J, Norbis F, Ruggeri L, Cler L, Triplett DA, Barbui T: Lupus anticoagulants and thrombosis: clinical association of different coagulation and immunologic tests. Thromb Haemost. 2000, 84: 1012-1016.
Nojima H, Kuratsune H, Suehisa E, Futsukaichi Y, Yamanishi H, Machii T, Kitani T, Iwatani Y, Kanakura Y: Anti-prothrombin antibodies combined with lupus anticoagulant activity is an essential risk factor for venous thromboembolism in patients with systemic lupus erythematosus. Br J Haematol. 2001, 114: 647-654. 10.1046/j.1365-2141.2001.02950.x.
Nojima J, Kuratsune H, Suehisa E, Futsukaichi Y, Yamanishi H, Machii T, Iwatani Y, Kanakura Y: Association between the prevalence of antibodies to beta(2)-glycoprotein I, prothrombin, protein C, protein S, and annexin V in patients with systemic lupus erythematosus and thrombotic and thrombocytopenic complications. Clin Chem. 2001, 47: 1008-1015.
Simmelink MJA, De Groot PG, Derksen RHWM: A study on associations between antiprothrombin antibodies, antiplasminogen antibodies and thrombosis. J Thromb Haemost. 2002, 1: 735-739.
Salcido-Ochoa F, Cabiedes J, Alarcón-Segovia D, Cabral AR: Antiprothrombin antibodies in patients with systemic lupus erythematosus or with primary antiphospholipid syndrome. J Clin Rheumatol. 2002, 8: 251-255. 10.1097/00124743-200210000-00004.
Von Landenberg P, Matthias T, Zaech J, Schultz M, Lorber M, Blank M, Shoenfeld Y: Anti-prothrombin antibodies are associated with pregnancy loss in patients with the antiphospholipid syndrome. Am J Reprod Med. 2003, 49: 51-56.
Musial J, Swadzba J, Motyl A, Iwaniec T: Clinical significance of antiphospholipid protein antibodies. Receiver operating characteristics plot analysis. J Rheumatol. 2003, 30: 723-730.
Ishikura K, Wada H, Kamikura Y, Hattori K, Fukuzawa T, Yamada N, Nakamura M, Nobori T, Nakano T: High prevalence of anti-prothrombin antibody in patients with deep vein thrombosis. Am J Hematol. 2004, 76: 338-742. 10.1002/ajh.20124.
Koskenmies S, Vaarala O, Widen E, Kere J, Palosuo T, Julkunen H: The association of antibodies to cardiolipin, beta 2-glycoprotein I, prothrombin, and oxidized low-density lipoprotein with thrombosis in 292 patients with familial and sporadic systemic lupus erythematosus. Scand J Rheumatol. 2004, 33: 246-252. 10.1080/03009740410005386.
Bertolaccini ML, Atsumi T, Koike T, Hughes GR, Khamashta MA: Antiprothrombin antibodies detected in two different assay systems. Prevalence and clinical significance in systemic lupus erythematosus. Thromb Haemost. 2005, 93: 289-297.
Bizzaro N, Tonutti E, Villalta D, Tampoia M, Tozzoli R: Prevalence and clinical correlation of anti-phospholipid binding protein antibodies in anti-cardiolipin negative patients with systemic lupus erythematosus and women with unexplained recurrent miscarriages. Arch Pathol Lab Med. 2005, 129: 61-68.
Forastiero R, Martinuzzo M, Pombo G, Puente D, Rossi A, Celebrin L, Bonaccorso S, Aversa L: A prospective study of antibodies to beta2-glycoprotein I and prothrombin, and risk of thrombosis. J Thromb Haemost. 2005, 3: 1231-1238. 10.1111/j.1538-7836.2005.01295.x.
Gould T, Tikly M, Asherson R, Loizou S, Singh S: Prevalence and clinical correlates of anti-phospholipid antibodies in South Africans with systemic lupus erythematosus. Scand J Rheumatol. 2006, 35: 29-34. 10.1080/03009740510026913.
Tsutumi A, Hayashi T, Chino Y, Mamura M, Goto D, Matsumoto I, Ito S, Sumida T: Significance of anti-prothrombin antibodies in patients with systemic lupus erythematosus: clinical evaluation of the antiprothrombin assay and the anti-phosphatidylserine/prothrombin assay, and comparison with other antiphospholipid antibody assays. Mod Rheumatol. 2006, 16: 158-164. 10.3109/s10165-006-0481-7.
Nojima J, Iwatani Y, Suehisa E, Suehisa E, Kuratsune H, Kanakura Y: The presence of anti-phosphatidylserine/prothrombin antibodies as risk factor for both arterial and venous thrombosis in patients with systemic lupus erythematosus. Haematologica. 2006, 91: 699-702.
Bizzaro N, Ghirardello A, Zampieri S, Iaccarino L, Tozzoli R, Ruffatti A, Villalta D, Tonutti E, Doria A: Anti-prothrombin antibodies predict thrombosis in patients with systemic lupus erythematosus: a 15 year longitudinal study. J Thromb Haemost. 2007, 5: 1158-1164. 10.1111/j.1538-7836.2007.02532.x.
Sailer T, Vormittag R, Zoghlami C, Koder S, Quehenberger P, Male C, Pabinger I: The clinical significance of anti-prothrombin antibodies for risk assessment of thromboembolism in patients with lupus anticoagulant. Thromb Res. 2007, 120: 295-302. 10.1016/j.thromres.2007.01.001.
Bardin N, Alessi MC, Dignat-George F, Vague IJ, Sampol J, Harlé JR, Sanmarco M: Does the anti-prothrombin antibodies measurement provide additional information in patients with thrombosis?. Immunobiology. 2007, 212: 557-565. 10.1016/j.imbio.2007.02.001.
Jakowski TD, Wilson AR, Hill HR, Branch WD, Tebo AE: Autoantibodies against phosphatidylserine, prothrombin and phosphatidylserine-prothrombin complex: identical or distinct diagnostic tools for antiphospholipid syndrome?. Clin Chim Acta. 2009, 410: 19-24. 10.1016/j.cca.2009.09.006.
Szodoray P, Tarr T, Tumpek J, Kappelmayer J, Lakos G, Poor G, Szegedi G, Kiss E: Identification of rare anti-phospholipid/protein co-factor autoantibodies in patients with systemic lupus erythematosus. Autoimmunity. 2009, 42: 497-506. 10.1080/08916930902882731.
Pengo V, Denas G, Bison E, Banzato A, Jose SP, Gresele P, Marongiu F, Erba N, Veschi F, Ghirarduzzi A, De Candia E, Montaruli B, Marietta M, Testa S, Barcellona D, Tripodi A: Prevalence and significance of anti-prothrombin antibodies in patients with lupus anticoagulant (LA). Thromb Res. 2010, 126: 150-153. 10.1016/j.thromres.2010.05.018.
Marozio L, Curti A, Botta G, Canuto EM, Salton L, Tavella AM, Benedetto C: Anti-prothrombin antibodies are associated with adverse pregnancy outcome. Am J Reprod Immunol. 2011, 66: 404-409. 10.1111/j.1600-0897.2011.01031.x.
Hoxha A, Ruffatti A, Pittoni M: The clinical significance of autoantibodies directed against prothrombin in primary antiphospholipid syndrome. Clin Chim Acta. 2012, 413: 911-913. 10.1016/j.cca.2012.02.004.
Sater MS, Finan RR, Abu-Hijleh FM, Abu-Hijleh TM, Almawi WY: Anti-phosphatidylserine, anti-cardiolipin, anti-beta2glycoprotein I and anti-prothrombin antibodies in recurrent miscarriage at 8–12 gestational weeks. Eur J Obstet Gynecol Reprod Biol. 2012, 163: 170-174. 10.1016/j.ejogrb.2012.04.001.
Nojima J, Kuratsune H, Suehisa E, Kitani T, Iwatani Y, Kanakura Y: Strong correlation between the prevalence of cerebral infarction and the presence of anti-cardiolipin/antibeta2-glycoprotein I and anti-phosphatidylserine/prothrombin antibodies. Co-existence of these antibodies enhance ADP-induced platelet activation. Thromb Haemost. 2004, 91: 967-976.
Atsumi T, Koike T: Anti-prothrombin antibody: why do we need more assays?. Lupus. 2010, 19: 436-439. 10.1177/0961203310361487.
Žigon P, Ambrožič A, Čučnik S, Kveder T, Rozman B, Božič B: Modified phosphatidylserine-dependent antithrombin ELISA enables identification of patients negative for other antiphospholipid antibodies and also detects low avidity antibodies. Clin Chem Lab Med. 2011, 49: 1011-1018.
Vlagea A, Gil A, Cuesta MV, Arribas F, Diez J, Lavilla P, Pascual-Salcedo D: Antiphosphatidylserine/prothrombin antibodies (aPS/PT) as potential markers of antiphospholipid syndrome. Clin Appl Thromb Hemost. 2013, 19: 289-296.
Sciascia S, Murru V, Sanna G, Roccatello D, Khamashta MA, Bertolaccini ML: Clinical accuracy for diagnosis of antiphospholipid syndrome in systemic lupus erythematosus: evaluation of 23 possible combinations of antiphospholipid antibody specificities. J Thromb Haemost. 2012, 10: 2512-2518. 10.1111/jth.12014.
Shoenfeld Y, Krause I, Kvapil F, Sulkes J, Lev S, von Landenberg P, Font J, Zaech J, Cervera R, Piette JC, Boffa MC, Khamashta MA, Bertolaccini ML, Hughes GR, Youinou P, Meroni PL, Pengo V, Alves JD, Tincani A, Szegedi G, Lakos G, Sturfelt G, Jönsen A, Koike T, Sanmarco M, Ruffatti A, Ulcova-Gallova Z, Praprotnik S, Rozman B, Lorber M, Vriezman VB, Blank M: Prevalence and clinical correlations of antibodies against six beta2-glycoprotein-I-related peptides in the antiphospholipid syndrome. J Clin Immunol. 2003, 23: 377-383. 10.1023/A:1025321617304.
Mahler M, Norman GL, Meroni PL, Khamashta M: Autoantibodies to domain 1 of beta 2 glycoprotein 1: a promising candidate biomarker for risk management in antiphospholipid syndrome. Autoimmun Rev. 2012, 12: 313-317. 10.1016/j.autrev.2012.05.006.
de Laat B, de Groot PG: Autoantibodies directed against domain I of beta2-glycoprotein I. Curr Rheumatol Rep. 2011, 13: 70-76. 10.1007/s11926-010-0144-8.
de Laat B, Pengo V, Pabinger I, Musial J, Voskuyl AE, Bultink IE, Ruffatti A, Rozman B, Kveder T, de Moerloose P, Boehlen F, Rand J, Ulcova-Gallova Z, Mertens K, de Groot PG: The association between circulating antibodies against domain I of beta2-glycoprotein I and thrombosis: an international multicenter study. J Thromb Haemost. 2009, 7: 1767-1773. 10.1111/j.1538-7836.2009.03588.x.
Zuily S, De Laat B, Regnault V, Guillemin F, Kaminsky P, Albesa R, Norman G, De Groot PG, Lecompte T, Wahl D: Autoantibodies against domain I of beta2-glycoprotein indicate an increased risk for thrombosis in antiphospholipid patients, A prospective cohort study. J Thromb Haemost. 2013, 11: S3-
Agmon-Levin N, Seguro L, Rosario C, Mahler M, Gatto M, Tomer N, Leon E, Doria A, Kovács L, Costedoat-Chalumeau N, Gilburd B, Shoenfeld Y: Anti-β2GPI-DI antibodies are a marker of APS severity. Arthritis Rheum. 2013, 65: S1-
Andreoli L, Nalli C, Borghi MO, Pregnolato F, Grossi C, Zangola A, Allegri F, Gerosa M, Mahler M, Norman GL, Meroni PL, Tincani A: Domain I is the main specificity of anti-beta2 GPI in systemic autoimmune diseases. Arthritis Rheum. 2013, 65: S4-10.1002/acr.21904.
Chighizola CB, Gerosa M, Meroni PL: New tests to detect antiphospholipid antibodies: anti-domain I beta-2-glycoprotein-I antibodies. Curr Rheumatol Rep. 2014, 16: 402-
Willis R, Mahler M, Pregnolato F, Pericleous C, Rahman A, Ioannou J, Giles I, Lakos G, Albesa R, Zohoury N, Meroni PL, Pierangeli S: Clinical evaluation of two anti-Beta2glycoprotein I Domain 1 autoantibody assays to aid in the diagnosis and risk assessment of the antiphospholipid syndrome. Arthritis Rheum. 2013, 65: S3-
Ioannou Y, Pericleous C, Giles I, Latchman DS, Isenberg DA, Rahman A: Binding of antiphospholipid antibodies to discontinuous epitopes on domain I of human beta(2)-glycoprotein I: mutation studies including residues R39 to R43. Arthritis Rheum. 2007, 56: 280-290. 10.1002/art.22306.
Agostinis C, Durigutto P, Sblattero D, Borghi M, Grossi C, Bulla R, Macor P, Meroni PL, Tedesco F: A human monoclonal antibody against domain I of β2-glycoprotein I prevents clotting and fetal loss induced by polyclonal anti-phospholipid antibodies in animal models. Arthritis Rheum. 2013, 65: S245-
Staub HL, Bertolaccini ML, Khamashta MA: Anti-phosphatidylethanolamine antibody, thromboembolic events and the antiphospholipid syndrome. Autoimmun Rev. 2012, 12: 230-234. 10.1016/j.autrev.2012.07.008.
Sugi T, Matsubayashi H, Inomo A, Dan L, Makino T: Antiphosphatidylethanolamine antibodies in recurrent early pregnancy loss and mid-to-late pregnancy loss. J Obstet Gynaecol Res. 2004, 30: 326-332. 10.1111/j.1447-0756.2004.00206.x.
Conti F, Alessandri C, Sorice M, Capozzi A, Longo A, Garofalo T, Misasi R, Bompane D, Hughes GR, Khamashta MA, Valesini G: Thin-layer chromatography immunostaining in detecting anti-phospholipid antibodies in seronegative anti-phospholipid syndrome. Clin Exp Immunol. 2012, 167: 429-437. 10.1111/j.1365-2249.2011.04532.x.
Bertolaccini ML, Amengual O, Atsumi T, Binder WL, de Laat B, Forastiero R, Kutteh WH, Lambert M, Matsubayashi H, Murthy V, Petri M, Rand JH, Sanmarco M, Tebo AE, Pierangeli SS: 'Non-criteria' aPL tests: report of a task force and preconference workshop at the 13th International Congress on Antiphospholipid Antibodies, Galveston, TX, USA, April 2010. Lupus. 2011, 20: 191-205. 10.1177/0961203310397082.
Nayfe R, Uthman I, Aoun J, Saad Aldin E, Merashli M, Khamashta MA: Seronegative antiphospholipid syndrome. Rheumatology. 2013, 52: 1358-1367. 10.1093/rheumatology/ket126.
Yodfat O, Blank M, Krause I, Shoenfeld Y: The pathogenic role of anti-phosphatidylserine antibodies: active immunization with the antibodies leads to the induction of antiphospholipid syndrome. Clin Immunol Immunopathol. 1996, 78: 14-20. 10.1006/clin.1996.0003.
Grossi C, Borghi MO, Papaardo E, Pierangeli SS, Meroni PL: A more specific immunoassay for the diagnosis of APS. Arthritis Rheum. 2013, 65: S5-10.1002/acr.21811.
Sciascia S, Sanna G, Murru V, Khamashta MA, Bertolaccini ML: The clinical value of testing for Aphl, a new ELISA kit with a unique phospholipid mixture in patients with systemic lupus erythematosus (SLE). Arthritis Rheum. 2013, 65: S1-
Cesarman-Maus G, Ríos-Luna NP, Deora AB, Huang B, Villa R, Cravioto Mdel C, Alarcón-Segovia D, Sánchez-Guerrero J, Hajjar KA: Autoantibodies against the fibrinolytic receptor, annexin 2, in antiphospholipid syndrome. Blood. 2006, 107: 4375-4382. 10.1182/blood-2005-07-2636.
Lambrianides A, Carroll CJ, Pierangeli SS, Pericleous C, Branch W, Rice J, Latchman DS, Townsend P, Isenberg DA, Rhaman A, Giles IP: Effects of polyclonal IgG derived from patients with different clinical types of the antiphospholipid syndrome on monocyte signaling pathways. J Immunol. 2010, 184: 6622-6628. 10.4049/jimmunol.0902765.
Meroni PL, Raschi E, Grossi C, Pregnolato F, Trespidi L, Acaia B, Borghi MO: Obstetric and vascular APS: same autoantibodies but different diseases?. Lupus. 2012, 21: 708-710. 10.1177/0961203312438116.
Agostinis C, Biffi S, Garrovo C, Durigutto P, Lorenzon A, Bek A, Bulla R, Grossi C, Borghi MO, Meroni P, Tedesco F: In vivo distribution of β2 glycoprotein I under various pathophysiologic conditions. Blood. 2011, 118: 4231-4238. 10.1182/blood-2011-01-333617.
Passam FH, Giannakopoulos B, Mirarabshahi P, Krilis SA: Molecular pathophysiology of the antiphospholipid syndrome: the role of oxidative post-translational modification of beta 2 glycoprotein I. J Thromb Haemost. 2011, 9: 275-282.
Acknowledgements
CBC is supported by a Research Grant co-financed by University of Milan and Dote Ricerca: FSE, Regione Lombardia.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Meroni, P.L., Chighizola, C.B., Rovelli, F. et al. Antiphospholipid syndrome in 2014: more clinical manifestations, novel pathogenic players and emerging biomarkers. Arthritis Res Ther 16, 209 (2014). https://doi.org/10.1186/ar4549
Published:
DOI: https://doi.org/10.1186/ar4549