Abstract
In this review, the authors discuss the formation and structure of high-density lipoproteins (HDLs) and how those particles are altered in inflammatory or stress states to lose their capacity for reverse cholesterol transport and for antioxidant activity. In addition, abnormal HDLs can become proinflammatory (piHDLs) and actually contribute to oxidative damage. The assay by which piHDLs are identified involves studying the ability of test HDLs to prevent oxidation of low-density lipoproteins. Finally, the authors discuss the potential role of piHDLs (found in some 45% of patients with systemic lupus erythematosus and 20% of patients with rheumatoid arthritis) in the accelerated atherosclerosis associated with some chronic rheumatic diseases.
Similar content being viewed by others
Overview of the pathogenesis of atherosclerosis
Multiple factors play a role in the development of clinical atherosclerosis, including lipids, inflammation, physical sheer forces, and aging. This review is concerned with the role of high-density lipoproteins (HDLs) in both protecting and promoting atherosclerosis. In quick review then, low-density lipoproteins (LDLs) shuttle in and out of artery walls; when they are minimally or moderately oxidized within the wall (oxLDLs), they become proinflammatory. Endothelial cells are activated, monocytes are attracted into the artery wall, and monocyte/macrophages engulf oxLDLs, forming foam cells. Foam cells are the nidus of atherosclerotic plaque, and their formation is associated with the release of growth factors and proteinases that cause hypertrophy of arterial smooth muscle and destruction of normal tissue in the artery wall. Monocyte ingress into arterial walls attracts lymphocytes that recognize antigens released by damaged cells, such as heat shock proteins, and contributes to inflammation with release of cytokines. The endothelial cells can also be damaged by products of inflammation and immunity independently of pro-atherogenic lipids, including cytokines (particularly tumor necrosis factor-alpha [TNF-α], interleukin-1 [IL-1], and inter-feron-gamma), chemokines, pro-oxidants, circulating immune complexes (ICs), and antiendothelial antibodies. Finally, shear stress, hypertension, and aging contribute to points of increased pressure which favor plaque formation and gradual loss of elasticity, resulting in the gradual stiffening of major arteries. Recent reviews of these processes are available [1–5]. In the remainder of this review, we will focus on the interactions between LDLs, oxLDLs, and proinflammatory HDLs (piHDLs).
Overview of the role of apolipoprotein B- and apolipoprotein A-containing lipids in atherosclerosis
Some experts consider that the simplest way to classify the role of various lipids in promoting atherosclerosis is to compare levels of those carrying apolipoprotein B with those carrying apolipoprotein A (apoB and apoA, respectively). High levels of the proatherogenic apoB or low levels of antiatherogenic apoA predict accelerated atherosclerosis, manifested as coronary artery disease (CAD) or stroke [5–7]. The following lipids are rich in apoB: low-density lipoproteins (LDLs), very-low-density lipoproteins (VLDLs) (which are also rich in triglycerides), and intermediate-density lipoproteins (IDLs). In contrast, apoA-1 is carried primarily in high-density lipoproteins (HDLs). Thus, there is substantial evidence that high levels of LDLs in plasma are associated with increased risk for atherosclerosis whereas subnormal levels of HDLs are an independent risk factor for the same disease [7, 8].
Recently, it has become clear that simple quantitative analysis of HDL lipid/lipoproteins and their subfractions may be inadequate to estimate the role of HDLs in protecting against atherosclerosis. For example, in a controlled prospective trial of the HDL-raising CETP (cholesterol ester transfer protein) inhibitor torcetrapib added to a statin, compared with placebo plus statin, quantitative HDL levels increased 72.1% in 12 months in the torcetrapib/statin group, but atherosclerotic events were significantly more frequent [9]. The qualitative character of the increased HDLs was not measured in that study. In fact, in states of acute and chronic inflammation, the contents and functions of HDLs can change drastically, converting atheroprotective HDLs to atherogenic HDLs. The focus of this review is to discuss that change and to review data suggesting that altered atherogenic piHDLs may be products of inflammation in patients with rheumatic diseases which play an important role in their predisposition to accelerated atherosclerosis.
Low-density lipoproteins: mechanisms by which oxidized low-density lipoproteins predispose to atherosclerosis
LDLs are the major transporters of cholesterol in the body. They shuttle in and out of arterial walls, where they are major substrates for oxidation. In the artery wall, numerous oxidative molecules are available, including xanthine oxidase, myeloperoxidase, nitric oxide synthase (NOS), NAD(P)H, lipoxy-genases, and mitochondrial electron transport chains. LDLs are altered by these oxidants to contain reactive oxygen, nitrogen, and chlorine species as well as lipid-derived free radicals [5]. These are oxidized LDLs (oxLDLs), which are potent mediators of endothelial dysfunction and oxidative stress. The result of deposition of oxLDLs is inflammation and the formation of plaque in the artery. oxLDLs activate chemokine and cytokine receptors (such as monocyte chemotactic protein-1 [MCP-1]) on endothelial cells, and monocytes are trapped as they flow past; they enter the artery wall [10]. oxLDLs, in contrast to unmodified LDLs, are recognized by scavenger receptors on monocytes (thus triggering innate immunity). This results in phagocytosis of oxLDLs and formation of the lipid-rich foam cells that are the nidus of plaque. These activated macrophages release pro-inflammatory cytokines and chemokines, causing local tissue damage and stimulating hypertrophy of smooth muscle cells in the artery wall. Inflammation is also expanded by the influx of lymphocytes. As plaque matures, there is central inflammation around lipids, release of proteases and other pro-inflammatory molecules from the inflammatory cells, hypertrophy of smooth muscle, damage to endothelial cells, bulging of plaque into the lumen of the artery, and formation of a friable fibrous cap over the plaque. Exposure of circulating clotting factors and platelets to plaque is thrombogenic. Thus, the stage is set for impairment and even total blockage of blood flow in the area of plaque, leading ultimately to myocardial infarction, stroke, and tissue death.
High-density lipoproteins: characteristics, synthesis, degradation, and mechanisms by which normal high-density lipoproteins protect from atherosclerosis
Description of high-density lipoproteins and subsets
Plasma HDLs can also be viewed as part of the innate immune system – designed to prevent inflammation in baseline healthy situations and to enhance it when in danger [11]. As shown in Figures 1 and 2, HDLs are a collection of spherical or discoidal particles with high protein content (in the range of 30% by weight) that includes apolipoprotein A1 (apoA1) (approximately 70% of the total proteins) [5]. Their outer portion is a lipid monolayer of phospholipids and free cholesterol; larger HDLs have, in addition, a hydrophobic core consisting of cholesterol esters with small amounts of triglycerides. Proteins in HDLs in addition to apoA1 include apoE, apoA-IV, apoA-V, apoJ, apoC-I, apoC-II, and apoC-III [12, 13]. HDL particles also contain antioxidant enzymes paraoxonase (PON), lecithin cholesterol acyltransferase (LCAT), and platelet-activating acyl hydrolase (PAF-AH). Characteristics of a classical HDL molecule are shown in Figure 2a.
Overview of synthesis, maturation, and disposal of high-density lipoproteins (HDLs). Apolipoprotein A1 (apoA1) is synthesized by the action of ATP-binding cassette transporter AI (ABCA1) in the liver and small intestine and is secreted as immature HDL (imm HDL) particles with large amounts of protein and small amounts of free cholesterol. Macrophages and peripheral tissues also donate free cholesterol and phospholipids to apoA1 to form more immature HDL particles. The action of lecithin cholesterol acyltransferase (LCAT) adds esterified cholesterol to the core of HDLs, leading to mature HDL particles composed of lipoproteins (apoA1 being the most abundant), phospholipids, and cholesterol esters. Cholesterol esters are shuttled to apoB-rich low-density lipoproteins (LDLs) and very-low-density lipoproteins (VLDLs) by the actions of cholesterol ester transfer protein (CETP). Conversely, phospholipids are transferred from LDLs/VLDLs to HDLs by the action of phospholipid transfer protein (PLTP). HDLs, as they break down, donate phospholipids and cholesterol/cholesterol esters, which are bound by SR-B1 receptor on liver cells. LDLs are bound by LDL receptor (LDLR) on hepatocytes. ApoA1 can be reused or secreted by the liver. Cholesterol can be reused or secreted into the bile for disposal. Triangles = apoA1; diamond = apoB. CE, cholesterol esters; FC, free cholesterol; PL, phospholipids; TG, triglycerides. The figure is based, in part, on figures and data in [102] and [103].
Comparison of normal protective anti-inflammatory high-density lipoproteins (HDLs) (a) to proinflammatory HDLs (b). Normal HDLs are rich in apolipoproteins (yellow ovals) and antioxidant enzymes (white squares). After exposure to pro-oxidants, oxidized lipids, and proteases, proinflammatory HDLs have less lipoprotein and some, such as the major transporter apolipoprotein A-1 (A-1 in the figure), are disabled by the addition of chlorine, nitrogen, and oxygen to protein moieties: A-1 can no longer stabilize paraoxonase-1 (PON1) so PON1 cannot exert its antioxidant enzyme activity. In addition, pro-oxidant acute-phase proteins are added to the particle (serum amyloid A [SAA] and ceruloplasmin) as are oxidized lipids. The figure is based on information in [2] and [41]. apoJ, apolipoprotein J; CE, cholesterol ester; CE-OOH, cholesteryl linoleate hydroperoxide; GSH, glutathione; HPETE, hydroxyeicosatetraenoic acid; HPODE, hydroperoxy-octadecadienoic acid; LCAT, lecithin cholesterol acyltransferase; PAF-AH, platelet-activating acyl hydrolase.
Depending on the method used to separate HDLs, there are as many as 10 subsets: some particles contain only apoA1 and others both apoA-I and apoA-II [14]. In general, small dense HDLs are lipid-poor and protein-rich discs, but the majority of HDL particles are spherical and rich in both lipid and protein. There has been dispute as to which of the HDL subsets are most important in protecting from atherosclerosis, with general agreement that high plasma levels of alpha1-HDLs and apoA-I are protective [13, 14]. The HDLs that are measured in routine service laboratories include primarily large, cholesterol-rich HDL particles [5].
Synthesis and degradation of high-density lipoproteins
As shown in Figure 1, small HDL precursors (lipid-free apoA-I or lipid-poor pre-beta-HDLs referred to as immature HDLs in Figure 1) are synthesized in liver and intestine through the action of the enzyme ATP-binding cassette transporter A1 (ABCA1) on precursor protein, then modified in the circulation by acquisition of lipids. Initial lipid acquisition occurs at cellular membranes (listed as macrophages and peripheral tissues in Figure 1) via the ABCA1-mediated efflux of cholesterol and phospholipids from cells onto HDLs [15, 16]. Genetic defects in ABCA1, as in Tangier disease, result in low HDL levels and premature atherosclerosis [1, 5, 16]. LCAT-mediated esterification of cholesterol then generates large spherical HDL particles with a lipid core of cholesterol esters and triglycerides [5]. These particles are remodeled and fused with other particles. Surface remnant transfer onto HDLs from LDLs and VLDLs is mediated by phospholipid transfer protein (PLTP) [17]. Smaller particles can be generated by the action of CETP, which transfers cholesterol esters from HDLs to apoB-containing lipoproteins (LDLs and VLDLs) [18]. This generates triglyceride-rich HDLs with little cholesterol ester, forming smaller particles of HDLs. The important protein apoA-I can be shed from these small HDLs and form new HDL particles via new interactions with ABCA1 in macrophages, cell membranes of other tissues, or liver. HDL lipids are degraded (a) by selective uptake into other particles, (b) via CETP transfer to LDLs/VLDLs, or (c) as holoparticles taken up by SR-B1 receptors on hepatocytes, primarily via apoE-containing HDLs, after which they are secreted into bile [5]. Another consequence of binding to SR-B1 is activation of endothelial NOS and nitric oxide production.
Mechanisms by which high-density lipoproteins prevent atherosclerosis
Numerous actions of normal anti-inflammatory HDLs contribute to their ability to protect against atherosclerosis (Table 1 and Figure 2a). The first major mechanism for this protection is that normal HDLs participate in reverse cholesterol transport. Reverse cholesterol transport is the shuttling of cholesterol out of cell membranes and cytoplasm (including tissue macrophages, foam cells, and artery walls; Figure 1) into the circulation and then to the liver. The cholesterol efflux is mediated by the interactions of apoA-I, apoA-II, and apoE in HDLs with ABCA1, ABCG1, or ABCG4 transporters and/or SR-BI receptor on cell membranes. The process is rapid, unidirectional, and LCAT-independent, removing both cholesterol and phospholipids from membranes [19]. The cholesterol is transferred to HDL particles in the circulation and from there is transported to the liver [20]. ApoA-I is probably the most important protein in promoting reverse cholesterol transport [21]; treatment with recombinant apoA-I (Milano) variant mobilized tissue cholesterol and reduced plaque lipid and macrophage content in aortas of apoE-/- mice [22]. In addition to reverse cholesterol transport mediated by HDLs, oxLDLs are removed from artery walls by engulfment by macrophages using scavenger receptors such as CD36 [23–26].
The second major mechanism for protective capacity of normal HDLs is their antioxidative function. Both proteins and lipids in LDLs are protected from accumulation of oxidation products in vivo in the presence of normal HDLs [27, 28]. The antioxidative capacity depends on several antioxidative enzymes and several apolipoproteins. Again, apoA-I plays a major role by removing oxidized phospholipids of many types from LDLs and from arterial wall cells [29] and by stabilizing PON – a major antioxidant enzyme in HDLs. ApoE also has antioxidant properties [30] and can promote regression of atherosclerosis [31]. ApoJ at low levels is also antioxidant via its hydrophobic-binding domains [32]. On the other hand, apoA-II may be proatherogenic in that it can displace apoA-I and PON from HDL particles [33]. The major HDL antioxidative enzymes are PON1, platelet-activating factor acylhydrolase (PAF-AH), lecithin/cholesterol acyltransferase (LCAT), and glutathione peroxidase [27, 29]. PON1 hydrolyzes LDL-derived short-chain oxidized phospholipids. PON1 can destroy biologically active oxLDLs and can protect LDLs from oxidation that is metal-ion-dependent. The association of HDLs with PON1 is required to maintain normal serum activity of the enzyme, possibly by stabilizing the secreted peptide [34, 35]. PAF-AH and LCAT can also hydrolyze LDL-derived short-chain oxidized phospholipids [36]. Local arterial expression of PAF-AH (separate from HDLs) also reduces accumulation of oxLDLs and inhibits inflammation, thrombosis, and neointima formation in rabbits [37]. The characteristics of normal HDL particles are illustrated in Figure 2a.
A third protective mechanism relates to HDL interactions with lipids in human arterial endothelial cells. Oxidized 1-palmitoyl-2-arachidonyl-sn-3-glycero-phosphorylcholine (ox-PAPC) and its component phospholipid, 1-palmitoyl-2-5,6 epoxyisoprostanoyl)-sn-glycero-e-phosphocholine (PEIPC), present in atherosclerotic lesions activate endothelial cells to induce inflammatory and pro-oxidant responses that involve induction of genes regulating chemotaxis, sterol biosynthesis, the unfolded protein response, and redox homeostasis. The addition of normal HDLs to the arterial endothelial cells in vitro reduced the induction of the proinflammatory responses, resulting in the reduction of chemotactic activity and monocyte binding. However, the antioxidant activities induced by ox-PAPC and PEIPC were preserved [38].
A fourth mechanism by which normal HDLs protect from atherosclerosis is by downregulating immune responses. This has several components. First, the oxidation of lipids is proinflammatory, as discussed above, and normal HDLs prevent that oxidation. Second, activation of endothelial cells, influx and activation of monocytes/macrophages, and damage to smooth muscle cells resulting from oxLDL deposition in artery walls are all suppressed, as discussed above. Third, cellular contact between stimulated T cells and monocytes is inhibited by HDL-associated apoA-I. This results in decreased activation of monocytes and decreased release of the highly proinflammatory cytokines IL-1β and TNF-α [39].
Transformation of normal, protective high-density lipoproteins to proinflammatory high-density lipoproteins
During acute or chronic inflammation, several changes occur in HDLs, as summarized in Table 1. As part of the acute-phase response, several plasma proteins carried in HDLs are decreased, including PON, LCAT, CETP, PLTP, hepatic lipase, and apoA-I. Acute-phase HDLs are depleted in cholesterol ester but enriched in free cholesterol, triglyceride, and free fatty acids – none of which can participate in reverse cholesterol transport or antioxidation [40, 41]. In these HDLs, levels of the pro-oxidant serum amyloid A (SAA) increase several-fold, as do levels of apoJ (also called clusterin) [42]. In fact, apoA-I is displaced from HDLs by SAA, which is associated not only with disabling HDLs as anti-inflammatory mediators, but with creating piHDLs. These HDLs can be defined as proinflammatory because they actually enhance the oxidation of LDLs and therefore attract monocytes to engulf those oxLDLs [42]. In fact, regulation of SAA, apoA-I, and PON1 is coordinated in murine hepatocytes; as SAA increases, the other two molecules decrease. These changes are promoted by nuclear factor-kappa-B and suppressed by the nuclear receptor peroxisome proliferator-activated receptor-alpha (PPAR-α) [43]. Acute-phase HDLs (including piHDLs) are much less effective than normal HDLs in removing cholesterol from macrophages [44] and delivering cholesterol esters to hepatocytes [45]. Lipids in the altered HDLs are themselves oxidized [46].
We can thus envision the piHDLs as pictured in Figure 2b. In the spherical particles, apoA-I and antioxidative enzymes are partially replaced by the products of oxidation, including oxidized lipids and serum amyloid protein. Such changes have been shown to occur in acute infection, in acute 'trauma' of surgical interventions, and in chronic inflammation. If one measures total HDLs by standard service clinical laboratory methods, they are usually low during periods of acute infection as well as in chronic inflammatory states such as rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE) [47–50]. A population study of monocytes from individuals from the general population with low plasma concentrations of HDLs showed increased expression of a cluster of inflammatory genes (IL-1β, IL-8, and TNF-α) and decreased PPAR-γ and antioxidant metallothionein genes compared with controls [51]. It seems likely that there are at least two major factors determining whether an individual at any given time point has normal anti-inflammatory HDLs or nonprotective piHDLs, whether inflammation is present, and genetic background. Furthermore, it is likely that the measurement of HDL function shows a 'majority' activity. That is, HDLs consist of numerous particles of different sizes, contents, and activities. In assays for anti-inflammatory versus proinflammatory function of HDLs obtained from test serum, one detects a dominant activity that does not describe the exact distribution of these HDLs. These data would predict that the ratio of normal to proinflammatory HDLs would vary over time. In fact, as discussed below, in our data in patients with SLE, that was not true. piHDL activity in an individual was stable over time without relation to disease activity; normal HDLs were also found repeatedly in some individuals with SLE even during periods of marked disease activity. It is our idea that HDL functions are rooted in genetic susceptibility and influenced by the presence of chronic inflammation in rheumatic diseases.
What are the processes that account for modification of normal HDLs into piHDLs? These are probably complex and include (a) oxidation of lipids and lipoproteins in the HDL particle (by increased activities of peroxidases that occur during inflammation, for example), (b) decreased synthesis of the proteins that populate HDL particles (for example, apoA-I), (c) addition of proteins that may participate in inflammation, and (d) replacement of cholesterol-transporting proteins and antioxidant enzymes by pro-oxidants SAA and ceruloplasmin. This is probably a dynamic situation in which lipids and proteins interact with other lipids and transfer from one particle or lipid-containing membrane to another. Thus, chronic autoimmune inflammation, even if low-grade, in a permissive genetic background may determine a chronic composition of HDLs which is proinflammatory. A study of the protein content of HDLs from patients with CAD compared with HDLs from healthy individuals showed enrichment of CAD HDLs in complement regulatory proteins, serpins, and apoE [52]. It is not clear how this work relates to the piHDLs that are discussed in this review.
Measurement of proinflammatory versus normal high-density lipoproteins
The measurement of the qualitative function of HDLs relies on the ability of normal HDLs to prevent oxidation of LDLs [53–55]. Patient HDLs are isolated from cryopreserved plasma and added to a fluorochrome-releasing substrate, dichlorofluorescein (DCFH), following the addition of LDLs from a normal donor. In the absence of HDLs, the LDLs oxidize in vitro and in turn oxidize DCFH, which then gives off a fluorescent signal. In the presence of normal protective HDLs (isolated from a normal donor), oxidation of LDLs is reduced and fluorescence is quenched. Fluorescence released by normal HDLs plus normal LDLs is set as '1.0'. Protective HDLs give a reading of 1 or less and piHDLs give a reading of greater than 1 [55]. Another approach to measuring the inflammatory potential of HDLs is to measure monocyte migration in coculture with aortic or smooth muscle cells in the presence of LDLs and test HDLs [42], although our laboratory has experienced better reliability and reproducibility with the procedurally easier DCFH cell-free assay.
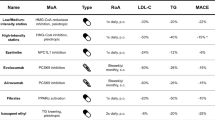
Lipid abnormalities and rheumatic diseases: overview
The prevalence of atherosclerosis is increased in several rheumatic diseases (Table 2), with the highest prevalence being in SLE, followed by RA. The usual lipid profiles (done in routine service laboratories) for SLE and RA, as well as other rheumatic diseases, are shown in Table 2[47–50, 55–59]. With regard to HDLs, the usual profile is for HDL cholesterol to be low in rheumatic diseases associated with systemic inflammation (and triglycerides to be high), although there is variation from study to study in this regard. Quantitative measures of HDLs have not been predictive of subclinical or clinical atherosclerosis in any studies of patients with rheumatic diseases, with major predictors being age and duration of disease with weaker correlations with smoking, high levels of homocysteine, hypertension, antibodies to phospholipids, and diabetes. The role of treatment with glucocorticoids has been variable [2, 47–50, 55–59]; most studies show a correlation with atherosclerosis but some show either no correlation or a protective effect. In our work, prednisone doses of greater than 7.5 mg daily were significantly associated with piHDLs [55].
Genetic factors predisposing to arterial thrombosis in SLE include homozygosity for variant alleles of mannose-binding lectin, as shown in a Danish cohort [60]. For dysfunctional HDLs in the general population, a polymorphism in apoA-1 (apoA-1 Milano) is associated with reduced clinical events [55, 61, 62]. Genetic variants of ABCA1 influence cholesterol efflux. Polymorphisms in LCAT, apoA-II, and apoE are all likely to alter the function of HDLs [63, 64]. Some genetic variants of PON1 influence levels of that enzyme and are also likely to alter HDL function; at least one also predisposes to SLE [65, 66].
Proinflammatory high-density lipoproteins and systemic lupus erythematosus
When qualitative rather than quantitative properties of HDLs are measured, the importance of HDLs to atherosclerosis in SLE and RA becomes apparent. In our studies [55], the presence of piHDLs was common in SLE and a strong predictor of subclinical atherosclerosis. A study of 154 women with SLE compared with 48 women with RA and 72 healthy women showed that piHDLs were present in 45% of patients with SLE, 20% of patients with RA, and 4% of healthy controls. Differences between each group were statistically significant at a P value of less than 0.006. The mean inflammatory indices (<1.0 is normal) were 1.02 ± 0.57 in SLE compared with 0.68 ± 0.28 in healthy controls (P < 0.001). Since piHDLs can arise and persist for approximately 2 weeks after surgeries, we originally proposed that piHDLs developed from peroxidation of HDLs caused by inflammation associated with active SLE. This hypothesis was supported by a positive correlation between piHDLs and Westergren erythrocyte sedimentation rate levels on multivariate analysis. However, the presence of piHDLs did not correlate with SLE disease activity measured by Selena-SLEDAI, and the presence of piHDLs or normal HDLs in any given patient was stable over time, regardless of disease activity. Therefore, it seems likely that genetic predisposition also contributes to whether a given individual produces persistent piHDLs. Genetic predisposition is also suggested by the observation that low activity of PON1 in SLE patients compared with a healthy population did not correlate with measures of disease activity/inflammation, although it did correlate with clinical atherosclerosis. The BB phenotype that correlates with high activity of PON1 was absent in all of the SLE patients [67].
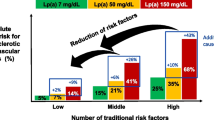
piHDLs occur in a larger proportion of patients with SLE compared with RA and also are significantly more frequent in SLE patients who had documented CAD. Recent work has shown that piHDLs are also significantly more frequent in SLE patients with carotid artery plaque [68]. In fact, the presence of piHDLs in an SLE patient increases the risk for carotid plaque several-fold. Thus, it is likely that identification of piHDLs is a valid biomarker for increased risk for atherosclerosis in patients with SLE. More importantly, understanding the biologic basis for maintaining piHDLs should provide important insights into the pathogenesis of accelerated atherosclerosis characteristic of some patients with SLE. The results of our initial study are summarized in Figure 3.
Comparison of the inflammatory indices of high-density lipoproteins (HDLs) isolated from healthy controls (left column) and patients with systemic lupus erythematosus (SLE) (middle column) and rheumatoid arthritis (RA) (right column). Numbers below 1.0 are normal; numbers greater than or equal to 1.0 are proinflammatory. Data are presented as box-and-whisker plots; the ends of each box represent the lowest and highest quartiles, the vertical lines show minimum and maximum values, and horizontal lines in each box indicate median values. Note that inflammatory indices are higher in SLE patients than in healthy controls or RA patients and are higher in RA patients than in healthy controls. Statistical analyses are as follows: SLE versus healthy controls, P < 0.0001; RA versus healthy controls, P = 0.004; and SLE versus RA, P = 0.005. There were 154 individuals in the SLE group, 45 in the RA group, and 74 healthy volunteers. All individuals are female. Data are from [55].
It is also interesting that measurements of some of the lipoproteins and antioxidant enzymes associated with HDLs are also associated with increased risk for atherosclerosis in SLE. For example, plasma levels of PON1 are reduced in SLE patients [67], as one would expect if HDLs were pro-inflammatory instead of protective (Table 1 and Figure 2b). Enhanced lipid peroxidation, including high levels of oxLDLs, is associated with atherosclerosis in patients with SLE [69]. The increase in oxidation is associated, in part, with the presence of piHDLs rather than antioxidant normal HDLs.
Processes in addition to proinflammatory high-density lipoproteins that may accelerate atherosclerosis in systemic lupus erythematosus
Antibodies may also play a role in the pathogenesis of atherosclerosis, particularly in conditions such as SLE. Elevated levels of antibodies against oxLDLs have been described in the general population and in some studies are predictive of myocardial infarction and the progression of atherosclerosis [70, 71]. Other studies, however, have not found any such correlations [72]. Similarly, the presence of antibodies to oxLDLs has uncertain significance in subjects with SLE. Anti-oxLDLs have been described in up to 80% of patients with SLE and antiphospholipid antibody syndrome [73–76]. Titers of antibodies to oxLDLs have also been associated with disease activity in SLE [77]. At least one study has demonstrated that autoantibodies to oxLDLs are more common in SLE patients who have a history of cardiovascular disease than in SLE controls or normal subjects [78], although in two other studies, anti-oxLDLs and arterial disease were not associated [79, 80]. There is some speculation that the increased risk of thrombotic and atherosclerotic events seen in patients with SLE and antiphos-pholipid antibodies may be due, in part, to a crossreactivity between anticardiolipin and oxLDLs [74]. Cardiolipin is a component of LDLs [81], and indeed, a crossreactivity between anticardiolipin and anti-oxLDL antibodies has been demonstrated [74]. Additionally, beta2-glycoprotein I (β2-GPI), the protein recognized by most antibodies to cardiolipin, binds directly and stably to oxLDLs [82]. These oxLDL-β2-GPI complexes have been found in patients with SLE and antiphospholipid antibody syndrome and are associated with a risk of arterial thrombosis [83]. Interestingly, there is enhanced uptake of oxLDL-β2-GPI complexes by macrophages, probably mediated by macrophage Fc-γ receptors [84]. Thus, oxLDL-β2-GPI complexes may contribute to atherosclerosis by increasing formation of foam cells.
ICs have also been described as a risk factor for atherosclerosis in the general population. In one prospective study of 257 healthy men, the levels of circulating ICs at age 50 correlated with the future development of myocardial infarction [85]. In vitro studies have also suggested that LDL-containing ICs may play a role in atherogenesis. Macrophages that ingest LDL-ICs become activated and release TNF-α, IL-1, oxygen-activated radicals, and matrix metallo-proteinase-1 [86]. LDL-containing ICs have been examined in several studies of SLE subjects, with varying results. In one study of a pediatric SLE population, there was an increase in levels of IgG LDL-ICs in SLE subjects compared with healthy controls, although there was no association with endothelial dysfunction [76]. Another study of an adult SLE population, however, demonstrated no difference from controls in levels of IgG or IgM LDL-containing ICs [69].
In addition to piHDLs, autoantibodies, and ICs, inflammation itself probably contributes to accelerated atherosclerosis in patients with chronic rheumatic diseases. Infiltration of arterial walls with T lymphocytes that recognize various autoantigens and contribute to the release of proinflammatory cytokine and chemokines, and to the pro-oxidative molecules that arise, also accelerates clinical disease [87]. Furthermore, at the adventitial side of the artery, lipokines, cytokines, and chemokines promote inflammation in arteries, particularly the neurtrophil-attractant IL-8 and the monocyte-attractant MCP-1 [88]. Discussion of these risk factors is beyond the scope of this article: they are reviewed elsewhere in more detail [2, 89] and their interplay is illustrated in Figure 4.
An overview of the pathogenesis of atherosclerosis. The influence of high-density lipoprotein (HDL) and oxidized low-density lipoprotein (oxLDL) on atherosclerosis is one part of the story, as shown in the open circle on the right. However, many other processes impact on arterial health, including additional factors influencing inflammation, oxidation, and the immune response. Proinflammatory HDLs (piHDLs) play a role in each of these processes. EC, endothelial cell; IFNγ, interferon-gamma; IL, interleukin; iNOS, inducible nitric oxide synthase; L, lymphocyte; M, monocyte; MCP-1, monocyte chemotactic protein-1; OxPL, oxidized phospholipid; TNFα, tumor necrosis factor-alpha.
Proinflammatory high-density lipoproteins and nonrheumatic diseases
Other diseases in which dysfunctional, presumably pro-inflammatory, HDLs have been found include metabolic syndrome [90], poorly controlled diabetes mellitus [91], solid organ transplantation [92], and chronic kidney disease [93]. All of these disorders are characterized by accelerated atherosclerosis, and all have many abnormalities promoting arterial damage – similar to the situation in SLE and RA.
Therapeutic options to restore proinflammatory high-density lipoproteins to normal protective high-density lipoproteins
Several ideas and preliminary studies have been advanced for methods to alter piHDLs and render them more protective against atherosclerosis. It would be ideal in the therapy of rheumatic diseases (a) to be able to identify patients at high risk for accelerated atherosclerosis and (b) to have available effective, safe therapies. With this in mind, a few trials of statins have been undertaken in an attempt to affect piHDLs. Statins decrease plasma levels of apoB-containing lipoproteins, particularly LDLs, IDLs, VLDLs, and VLDL remnants. HDL levels rise a small amount, as does apoA-I production. Statins increase the activity of PON1 and reduce LDLs. Recombinant HDL administered intravenously enhances cholesterol efflux and reducs oxidative damage in dys-lipidemic subjects. This has been effective in a small trial to stabilize vulnerable unstable atherosclerotic plaque [94]. In the Ansell series, patients with CAD and piHDLs were treated with simvastatin 40 mg/day for 6 weeks. The mean decrease in the inflammatory index of their piHDLs was 38%, but this was not enough to restore piHDLs to normal range in most patients [95]. In RA, Charles-Schoeman and colleagues [96] treated 30 patients with RA with atorvastatin 80 mg or placebo for 12 weeks. The inflammatory index of patient HDLs fell 15% in statin-treated patients and rose 7% in those on placebo (P < 0.026) [96]. Diet and exercise in patients with metabolic syndrome dropped piHDL levels toward normal as the patients lost weight [97].
Amphipathic peptides based on the structures of apoA-1 or apoJ can be administered orally in their D forms. In animal studies, an 18-amino-acid peptide, D-4F, removed lipid oxidation products from HDLs and promoted cholesterol efflux [98]. In monkeys with piHDLs, the inflammatory index of 1.2 fell to 0.5 two hours after administration of D-4F [28], the best studied of these peptides to date. Levels of lipid hydroperoxides fell in both LDLs and HDLs. Preliminary data in patients with coronary disease showed improvement in HDL inflammatory index after administration of D-4F, without any lowering of total HDLs [99]. D-(113–122)apoJ is a nine-amino-acid sequence mimetic that also improves HDL function and inhibits atherosclerosis in animals [100].
Other potential therapies that might alter piHDLs toward more protective particles include decreasing plasma triglyceride levels to increase cholesterol esters in HDL cores or decreasing oxidative stress and inflammation hoping to replace SAA with functional apoA-1. Although a recent CETP inhibitor study failed to prevent cardiovascular events (and actually increased them) even though quantities of HDLs rose [9], other CETP inhibitors are under study. It may be that they should be combined with niacin or statins or both. Niacin functions to reduce triglycerides, with a concomitant increase in quantities of HDLs and apoA-1. Fibrate therapy increases HDLs by a small amount and also increases levels of apo-AI and apo-AII [5].
For now, in 2008, physicians caring for patients predisposed to atherosclerosis by SLE or RA or other rheumatic disease, especially with accompanying risk factors like metabolic syndrome, hypertension, diabetes, and older age, should follow standard guidelines for preventing atherosclerosis. This would include statin therapies for high LDLs, niacin for hypertriglyceridemia, control of hyperglycemia and hypertension, and cessation of smoking. Furthermore, it is likely that the better we control inflammation from the rheumatic disease, the less the patient is predisposed to atherosclerosis and to piHDLs. For example, treatment of RA with methotrexate reduced mortality overall, particularly mortality from cardiovascular disease [101]. Since that was not true of other disease-modifying antirheumatic drugs used for RA in the same study population, the situation is probably more complex than simply reducing the inflammatory 'load' in a given patient. Hopefully, in the next few years, measurement of piHDLs will be established as a routine biomarker of patients at high risk; therapies that correct HDLs from dysfunctional to normal will be improved by new biologics, and currently available therapies that partially correct HDL dysfunction will be more widely used.
Abbreviations
- ABCA1:
-
= ATP-binding cassette transporter AI
- apo:
-
= apolipoprotein
- b2-GPI:
-
= beta2-glycoprotein I
- CAD:
-
= coronary artery disease
- CETP:
-
= cholesterol ester transfer protein
- DCFH:
-
= dichlorofluorescein
- HDL:
-
= high-density lipoprotein
- IC:
-
= immune complex
- IDL:
-
= intermediate-density lipoprotein
- IL:
-
= interleukin
- LCAT:
-
= lecithin cholesterol acyltransferase
- LDL:
-
= low-density lipoprotein
- MCP-1:
-
= monocyte chemotactic protein-1
- NOS:
-
= nitric oxide synthase
- oxLDL:
-
= oxidized low-density lipoprotein
- ox-PAPC:
-
= oxidized 1-palmitoyl-2-arachidonyl-sn-3-glycero-phosphoryl-choline
- PAF-AH:
-
= platelet-activating acyl hydrolase
- PEIPC:
-
= 1-palmitoyl-2-5, 6 epoxyisoprostanoyl)-sn-glycero-e-phosphocholine
- piHDL:
-
= proin-flammatory high-density lipoprotein
- PLTP:
-
= phospholipid transfer protein
- PON:
-
= paraoxonase
- PPAR:
-
= peroxisome proliferator-activated receptor
- RA:
-
= rheumatoid arthritis
- SAA:
-
= serum amyloid A
- SLE:
-
= systemic lupus erythematosus
- TNF-α:
-
= tumor necrosis factor-alpha
- VLDL:
-
= very-low-density lipoprotein.
References
Rosenson RS: Lipoprotein classification; metabolism; and role in atherosclerosis. UpToDate, version 15.3; 2008. Searched 3 March 2008.
Hahn BH, Grossman J, Chen WC, McMahon M: The pathogenesis of atherosclerosis in autoimmune rheumatic diseases: roles of inflammation and dyslipidemia. J Autoimmunity. 2007, 28: 69-75. 10.1016/j.jaut.2007.02.004.
O'Rourke MF: Arterial aging: pathophysiological principles. Vasc Med. 2007, 12: 329-341. 10.1177/1358863X07083392.
Blann AD, Woywodt A, Bertolini F, Bull TM, Buyon JP, Clancy RM, Haubitz M, He RP, Lip GY, Mancuso P, Sampol J, Solovey A, Dignat-George F: Circulating endothelial cells. Biomarker of vascular disease. Thromb Haemost. 2005, 93: 228-235.
Kontush A, Chapman MJ: Functionally defective high-density lipoprotein: a new therapeutic target at the crossroads of dys-lipidemia, inflammation and atherosclerosis. Pharmacol Rev. 2006, 58: 342-374. 10.1124/pr.58.3.1.
Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, McQueen M, Budaj A, Pais P, Varigos J, Lisheng L: Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004, 364: 937-952. 10.1016/S0140-6736(04)17018-9.
Rosenson R, Maron DJ: The epidemiology of low levels of high-density lipoprotein cholesterol in patients with and without coronary artery disease. Am J Cardiol. 2000, 86: 11L-14L. 10.1016/S0002-9149(00)01462-4.
Sharette AR, Ballantyne CM, Coady SA, Yeiss G, Sorlie PD, Catellier D, Patsch W: Coronary heart disease prediction from lipoprotein cholesterol levels, triglycerides, lipoprotein (a), apolipoproteins A-1 and B, and HDL density subfractions. The Atherosclerosis Risk in Communities (ARIC) Study. Circulation. 2001, 104: 1108-1113. 10.1161/hc3501.095214.
Barter PJ, Caulfield M, Eriksson M, Grundy SM, Kastelein JJP, Komajda M, Lopez-Sendon J, Mosca L, Tardif J-C, Waters DD, Shear CL, Revkin JH, Buhr KA, Fisher MR, Tall AR, Brewer B, for the ILLUMINATE Investigators: Effects of torcetapib in patients at high risk for coronary events. N Eng J Med. 2007, 357: 2109-2122. 10.1056/NEJMoa0706628.
Lusis AJ: Atherosclerosis. Nature (London). 2000, 407: 233-241. 10.1038/35025203.
Van Lenten BJ, Reddy ST, Navab M, Fogelman A: Understanding changes in high density lipoproteins during the acute phase response. Arterioscler Thromb Vasc Biol. 2006, 26: 1687-1688. 10.1161/01.ATV.0000232522.47018.a6.
Rosenson R, Karlsson H, Leanderson P, Tagesson C, Lindahl M: Lipoproteomics II: mapping of proteins in high-density lipoprotein using two-dimensional gel electrophoresis and mass spectrometry. Proteomics. 2005, 5: 1431-1445. 10.1002/pmic.200401010.
Duriez P, Fruchart JC: High-density lipoprotein subclasses and apolipoprotein A-I. Clin Chem Acta. 1999, 286: 97-114. 10.1016/S0009-8981(99)00096-0.
Asztalos BF, Collins D, Cupples LA, Demissie S, Horvath KV, Bloomfield HE, Robins SJ, Schaefer EJ: Value of high-density lipoprotein (HDL) subpopulations in predicting recurrent cardiovascular events in the Veterans Affairs HDL Intervention Trial. Arterioscler Thromb Vasc Biol. 2005, 25: 2185-2191. 10.1161/01.ATV.0000183727.90611.4f.
Oram JF: The cholesterol mobilizing transporter ABCA1 as a new therapeutic target for cardiovascular disease. Trends Cardiovasc Med. 2002, 12: 170-175. 10.1016/S1050-1738(02)00159-7.
Rye KA, Barter PJ: Formation and metabolism of prebeta-migrating, lipid-poor apolipoprotein A-I. Arterioscler Thromb Vasc Biol. 2004, 24: 421-428. 10.1161/01.ATV.0000104029.74961.f5.
van Tol A: Phospholipid transfer protein. Curr Opin Lipidol. 2002, 13: 135-139. 10.1097/00041433-200204000-00004.
Le Goff W, Guerin M, Chapman JM: Pharmacological modulation of cholesteryl ester transfer protein, a new therapeutic target in atherogenic dyslipidemia. Pharmacol Ther. 2004, 101: 17-38. 10.1016/j.pharmthera.2003.10.001.
Lewis GF, Rader DJ: New insights into the regulation of HDL metabolism and reverse cholesterol transport. Circ Res. 2005, 96: 1221-1232. 10.1161/01.RES.0000170946.56981.5c.
Nanjee MN, Cooke CJ, Wong JS, Hamilton RL, Olszewski WL, Miller NE: Composition and ultrastructure of size subclasses of normal human peripheral lymph lipoproteins: quantification of cholesterol uptake by HDL in tissue fluids. J Lipid Res. 2001, 42: 639-648.
Zhang Y, Zanotti I, Reilly MP, Glick JM, Rothblat GH, Rader DJ: Overexpression of apolipoprotein A-I promotes reverse transport of cholesterol from macrophages to feces in vivo. Circulation. 2003, 108: 661-663. 10.1161/01.CIR.0000086981.09834.E0.
Shah PK, Yano J, Reyes O, Chuy KY, Kaul S, Bisgaier CL, Drake S, Cercek B: High-dose recombinant apolipoprotein A-I (Milano) mobilizes tissue cholesterol and rapidly reduces plaque lipid and macrophage content in apolipoprotein e-deficient mice. Potential implications for acute plaque stabilization. Circulation. 2001, 103: 3047-3050. 10.1161/hc2501.092494.
Podrez EA, Poliakov E, Shen Z, Zhang R, Deng Y, Sun M, Finton PJ, Shan L, Gugiu B, Fox PL, Hoff HF, Salomon RG, Hazen SL: Identification of a novel family of oxidized phospholipids that serve as ligands for the macrophage scavenger receptor CD36. J Biol Chem. 2002, 277: 38503-38516. 10.1074/jbc.M203318200.
Berliner J, Leitinger N, Watson A, Huber J, Fogelman A, Navab M: Oxidized lipids in atherogenesis: formation, destruction and action. Thromb Haemost. 1997, 78: 195-199.
Miller YI, Chang MK, Binder CJ, Shaw PX, Witztum JL: Oxidized low density lipoprotein and innate immune receptors. Curr Opin Lipidol. 2003, 14: 437-445. 10.1097/00041433-200310000-00004.
Miller YI, Viriyakosol S, Binder CJ, Feramisco JR, Kirkland TN, Witztum JL: Minimally modified LDL binds to CD14, induces macrophage spreading via TLR4/MD-2, and inhibits phagocytosis of apoptotic cells. J Biol Chem. 2003, 278: 1561-1568. 10.1074/jbc.M209634200.
Van Lenten BJ, Navab M, Shih D, Fogelman AM, Lusis AJ: The role of high-density lipoproteins in oxidation and inflammation. Trends Cardiovasc Med. 2001, 11: 155-161. 10.1016/S1050-1738(01)00095-0.
Navab M, Ananthramaiah GM, Reddy ST, Van Lenten BJ, Ansell BJ, Fonarow GC, Vahabzadeh K, Hama S, Hough G, Kamranpour N, Berliner JA, Lusis AJ, Fogelman AM: The oxidation hypothesis of atherogenesis: the role of oxidized phospholipids and HDL. J Lipid Res. 2004, 45: 993-1007. 10.1194/jlr.R400001-JLR200.
Navab M, Hama SY, Anantharamaiah GM, Hassan K, Hough GP, Watson AD, Reddy ST, Sevanian A, Fonarow GC, Fogelman AM: Normal high density lipoprotein inhibits three steps in the formation of mildly oxidized low density lipoprotein: steps 2 and 3. J Lipid Res. 2000, 41: 1481-1494.
Miyata M, Smith JD: Apolipoprotein E allele-specific antioxidant activity and effects on cytotoxicity by oxidative insults and beta-amyloid peptides. Nat Genet. 1996, 14: 555-561. 10.1038/ng0996-55.
Raffai RL, Loeb SM, Weisgraber KH: Apolipoprotein E promotes the regression of atherosclerosis independently of lowering plasma cholesterol levels. Arterioscler Thromb Vasc Biol. 2005, 22: 483-487.
Trougakos IP, Lourda M, Agiostratidou G, Kleetsas D, Gonos ES: Differential effects of clusterin/apolipoprotein J on cellular growth and survival. Free Radi Biol Med. 2005, 38: 436-449. 10.1016/j.freeradbiomed.2004.10.038.
Ribas V, Sanchez-Quesada JL, Anton R, Camacho M, Julve J, Escola-Gil JC, Fila L, Ordonez-Llanos J, Blanco-Vaca F: Human apoliprotein A-II enrichment displaces paraoxonase from HDL and impairs its antioxidant properties: a new mechanism linking HDL protein composition and antiatherogenic potential. Circ Res. 2004, 95: 789-797. 10.1161/01.RES.0000146031.94850.5f.
James RW, Deakin SP: The importance of high-density lipoproteins for paraoxonase-1 secretion, stability and activity. Free Radic Biol Med. 2004, 37: 1986-1994. 10.1016/j.freeradbiomed.2004.08.012.
Gaidukov L, Tawfik DS: High affinity, stability and lactonase activity of serum paraoxonase PON1 anchored on HDL with ApoA-I. Biochemistry. 2005, 44: 11843-11854. 10.1021/bi050862i.
Marathe GK, Zimmerman GA, McIntyre TM: Platelet-activating factor acetylhydrolase, and not paraoxonase-1, is the oxidized phospholipid hydrolase of high density lipoprotein particles. J Biol Chem. 2003, 278: 3937-3947. 10.1074/jbc.M211126200.
Arakawa H, Qian J-Y, Baatar D, Karasawa K, Asada Y, Sasaguri Y, Miller ER, Witztum JL, Ueno H: Local expression of platelet-activating factor-acetylhydrolase reduces accumulation of oxidized lipoproteins and inhibits inflammation, shear stress-induced thrombosis, and neointima formation in balloon-injured carotid arteries in nonhyperlipidemic rabbits. Circulation. 2005, 111: 3302-3309. 10.1161/CIRCULATIONAHA.104.476242.
Gharavi NM, Gargalovic PS, Chang I, Araujo JA, Clark MJ, Szeto WL, Watson AD, Lusis AJ, Berliner JA: High-density lipoprotein modulates oxidized phospholipids signaling in human endothelial cells from proinflammatory to anti-inflammatory. Arterioscler Thromb Vasc Biol. 2007, 27: 1346-1353. 10.1161/ATVBAHA.107.141283.
Hyka N, Dayer J-M, Modoux C, Kohno T, Edwards CK, Roux-Lombard P, Burger D: Apolipoprotein A-I inhibits the production of IL-1beta and tumor necrosis factor-alpha by blocking contact-mediated activation of monocytes by T lymphocytes. Blood. 2001, 97: 2381-2389. 10.1182/blood.V97.8.2381.
Khovidhunkit W, Memon RA, Feingold KR, Funfeld C: Infection and inflammation-induced proatherogenic changes of lipoproteins. J Infect Dis. 2000, 181: S462-S472. 10.1086/315611.
Navab M, Berliner JA, Subbanagounder G, Hama S, Lusis AJ, Castellani LW, Reddy ST, Shih D, Shi W, Watson AD, ven Lenten BJ, Vora D, Fogelman AM: HDL and the inflammatory response induced by LDL-derived oxidized phospholipids. Arterioscler Thromb Vasc Biol. 2001, 21: 481-488.
Van Lenten BJ, Wagner AC, Nayak DP, Hama S, Navab M, Fogelman AM: HDL loses its anti-inflammatory properties during acute influenza A infection. Circulation. 2001, 103: 2283-2288.
Han CY, Chiba T, Campbell JS, Faust N, Chaisson M, Orasanu G, Plutzky J, Chait A: Reciprocal and co-ordinate regulation of serum amyloid A versus apolipoprotein A-I and paraoxonase-1 by inflammation in murine hepatocytes. Arterioscler Thromb Vasc Biol. 2006, 26: 1806-1813. 10.1161/01.ATV.0000227472.70734.ad.
Artl A, Marsche G, Lestavel S, Sattler W, Malle E: Role of serum amyloid A during metabolism of acute-phase HDL by macrophages. Arterioscler Thromb Vasc Biol. 2000, 10: 763-772.
Artle A, Marsche GP, Pussinen P, Knipping G, Sattler W, Malle E: Impaired capacity of acute-phase high density lipoprotein particles to deliver cholesteryl ester to the human HUH-7 hepatoma cell line. Int J Biochem Cell Biol. 2002, 34: 370-381. 10.1016/S1357-2725(01)00132-7.
Navab M, Anantharamaiah GM, Reddy ST, Van Lenten BJ, Ansell BJ, Fogelman AM: Mechanisms of disease: proatherogenic HDL – an evolving field. Nat Clin Pract Endocrinol Metab. 2006, 2: 504-511. 10.1038/ncpendmet0245.
Park YB, Choi HK, Kim MY, Lee WK, Song J, Dim DK, Lee SK: Effects of antirheumatic therapy on serum lipid levels in patients with rheumatoid arthritis: a prospective study. Am J Med. 2002, 15: 188-198. 10.1016/S0002-9343(02)01186-5.
Yoo WH: Dyslipoproteinemia in patients with active rheumatoid arthritis: effects of disease activity, sex and menopausal status on lipid profiles. J Rheumatol. 2004, 31: 1746-1753.
Georgiadis AN, Papvasiloiou EC, Lourida ES, Alamanos Y, Kostara C, Tselepis AD, Drosos AA: Atherogenic lipid profile is a feature characteristic of patients with early rheumatoid arthritis: effect of early treatment – a prospective, controlled study. Arthritis Res Ther. 2006, 8: R82-10.1186/ar1952.
de Carvalho JF, Bonfa E, Borba EF: Systemic lupus erythematosus and lupus dyslipoproteinemia. Autoimmun Rev. 2008, 7: 246-250. 10.1016/j.autrev.2007.11.016.
Sarov-Blat L, Kiss RS, Haidar B, Kavaslar N, Jaye M, Bertiaux M, Steplewski K, Hurle MR, Sprecher D, McPherson R, Marcel YL: Predominance of a proinflammatory phenotype in monocyte-derived macrophages from subjects with low plasma HDL-cholesterol. Arterioscler Thromb Vasc Biol. 2007, 27: 1115-1122. 10.1161/ATVBAHA.106.138990.
Vaisar T, Pennathur S, Green PS, Gharib SA, Hoofnagle AN, Cheung MC, Byun J, Vuletic S, Kassim S, Singh P, Chea H, Knopp RH, Brunzell J, Geary R, Chait A, Zhao XQ, Elkon K, Marcovina S, Ridker P, Oram JF, Heinecke JW: Shotgun proteomics implicates protease inhibition and complement activation in the anti-inflammatory properties of HDL. J Clin Invest. 2007, 117: 746-756. 10.1172/JCI26206.
Navab M, Imes SS, Hama SY, Hough GP, Ross LA, Bork RW, Valente AJ, Berliner JA, Drinkwater DC, Laks H, Fogelman AM: Monocyte transmigration induced by modification of low density lipoprotein in cocultures of human aortic wall cells is due to induction of monocyte chemotactic protein 1 synthesis and is abolished by high density lipoprotein. J Clin Invest. 1991, 88: 2039-2046. 10.1172/JCI115532.
Navab M, Hama SY, Hough GP, Subbanagounder G, Reddy ST, Fogelman AM: A cell-free assay for detecting HDL that is dysfunctional in preventing the formation of or inactivating oxidized phospholipids. J Lipid Res. 2001, 42: 1308-1317.
McMahon M, Grossman J, FitzGerald J, Dahlin-Lee E, Wallace DJ, Thong BY, Badsha H, Kalunian K, Charles C, Navab M, Fogelman AM, Hahn BH: Proinflammatory high-density lipoprotein as a biomarker for atherosclerosis in patients with systemic lupus erythematosus and rheumatoid arthritis. Arthritis Rheum. 2006, 54: 2541-2549. 10.1002/art.21976.
del Rincón ID, Williams K, Stern MP, Freeman GL, Escalante A: High incidence of cardiovascular events in a rheumatoid arthritis cohort not explained by traditional cardiac risk factors. Arthritis Rheum. 2001, 44: 2737-2745. 10.1002/1529-0131(200112)44:12<2737::AID-ART460>3.0.CO;2-#.
Roman MJ, Moeller E, Davis A, Paget SA, Crow MK, Lockshin MD, Sammaritano L, Devereux RB, Schwartz JE, Levine DM, Salmon JE: Preclinical carotid atherosclerosis in patients with rheumatoid arthritis. Ann Intern Med. 2006, 144: 249-256.
Roman MJ, Crow MK, Lockshin MD, Devereux RB, Paget SA, Sammaritano L, Levine DM, Davis A, Salmon JE: Rate and determinants of progress of atherosclerosis in systemic lupus erythematosus. Arthritis Rheum. 2007, 56: 3412-3419. 10.1002/art.22924.
Urowitz MB, Gladman D, Ibanez D, Fortin P, Sanchez-Guerrero J, Bae S, Clarke A, Bernatsky S, Gordon C, Hanly J, Wallace D, Isenberg D, Ginzler E, Merrill J, Alarcon GS, Steinsson K, Petri M, Dooley MA, Bruce I, Manzi S, Khamasta M, Ramsey-Goldman R, Zoma A, Sturfelt G, Nived O, Maddison P, Fong J, van Vollenhoven R, Aranow C, Kalunian K, Stoll T: Accumulation of coronary artery disease risk factors over three years: data from an international inception cohort. Arthritis Rheum. 2008, 59: 176-180. 10.1002/art.23353.
Ohlenschlaeger T, Garred P, Madsen HO, Jacobsen S: Mannose-binding lectin variant alleles and the risk of arterial thrombosis in systemic lupus erythematosus. N Engl J Med. 2004, 351: 260-267. 10.1056/NEJMoa033122.
Sirtori SR, Calabresi L, Franceschini G, Baldassarre D, Amato M, Johansson J, Salvetti M, Monteduro C, Zulli R, Muiesan ML, Agabiti-Rosei E: Cardiovascular status of carriers of the apolipoprotein A-l Milano mutant: the Limone sul Garda Study. Circulation. 2001, 103: 1949-1954.
Li D, Weng S, Yang B, Zander DS, Saldeen T, Nichols WW, Khan S, Mehta JL: Inhibition of arterial thrombus formation by ApoA1 Milano. Arterioscler Thromb Vasc Biol. 1999, 19: 378-383.
Singaraja RR, Visscher H, James ER, Chroni A, Coutinho JM, Brunham LR, Kang MH, Zannis VI, Chimini G, Hayden MR: Specific mutations in ABCA1 have discrete effects on ABCA1 function and lipid phenotypes both in vivo and in vitro. Circ Res. 2006, 99: 389-397. 10.1161/01.RES.0000237920.70451.ad.
Sviridov D, Nesterl PJ: Genetic factors affecting HDL levels, structure, metabolism and function. Curr Opin Lipidol. 2007, 18: 157-163. 10.1097/MOL.0b013e32803dbdd6.
Gaidukov L, Rosenblat M, Aviram M, Tawfik DS: The 192 R/Q polymorphs of serum paraoxonase PON1 differ in HDL binding, lipolactonase stimulation and cholesterol efflux. J Lipid Res. 2006, 47: 2492-2502. 10.1194/jlr.M600297-JLR200.
Tripi LM, Manzi S, Chen Q, Kenney M, Shaw P, Kao A, Bontempo F, Kammereer C, Kamboh MI: Relationship of serum paraoxonase 1 activity and paraoxonase 1 genotype to risk of systemic lupus erythematosus. Arthritis Rheum. 2006, 54: 1928-1939. 10.1002/art.21889.
Kiss E, Seres I, Tarr T, Kocsis Z, Szedgei G, Paragh G: Reduced paraoxonase1 activity is a risk for atherosclerosis in patients with systemic lupus erythematosus. Ann NY Acad Sci. 2007, 1108: 83-91. 10.1196/annals.1422.009.
McMahon M, Grossman J, FitzGerald J, Hahn BH: The novel bio-marker pro-inflammatory HDL is associated with carotid artery plaque in women with SLE [abstract]. Arthritis Rheum. 2006, 54: S522-10.1002/art.21976.
Frostegard J, Svenungsson E, Wu R, Gunnarsson I, Lundgerg IE, Klareskog L, Horkko S, Witztum JL: Lipid peroxidation is enhanced in patients with systemic lupus erythematosus and is associated with arterial and renal disease manifestations. Arthritis Rheum. 2005, 52: 192-200. 10.1002/art.20780.
Wu R, Nityanand S, Berglund L, Lithell H, Homm G, Lefvert AK: Antibodies against cardiolipin and oxidatively modified LDL in 50-year-old men predict myocardial infarction. Arteriosclero Thromb Vasc Biol. 1997, 17: 3159-3163.
Salonen JT, Yla-Herttuala S, Yamamoto R, Butler S, Korpela H, Salonen R, Nyssonen K, Palinski W, Witztum JL: Autoantibody against oxidised LDL and progression of carotid atherosclerosis. Lancet. 1992, 339: 883-887. 10.1016/0140-6736(92)90926-T.
Hansson GK: Immune mechanisms in atherosclerosis. Arterioscler Thromb Vasc Biol. 2001, 21: 1685-1690. 10.1161/hq1201.100220.
Tsimikas S, Brilakis ES, Miller ER, McConnell JP, Lennon RJ, Kornman KS, Witztum JL, Berger PBL: Oxidized phospholipids, Lp(a) lipoprotein and coronary artery disease. N Eng J Med. 2005, 353: 46-57. 10.1056/NEJMoa043175.
Vaarala O, Alfthan G, Jauhiainen M, Leirisalo-Repo M, Aho K, Palusuo T: Cross reaction between antibodies to oxidised low-density lipoprotein and to cardiolipin in systemic lupus erythematosus. Lancet. 1993, 341: 923-925. 10.1016/0140-6736(93)91213-6.
Aho K, Vaaral O, Tenkanen L, Julkunen H, Jouhikainen T, Alfthan G, Palusuo T: Antibodies binding to anionic phospholipids but not to oxidized low-density lipoprotein are associated with thrombosis in patients with systemic lupus erythematosus. Clin Exp Rheumatol. 1996, 14: 499-506.
Soep JB, Mietus-Snyder M, Malloy MJ, Witztum JL, von Scheven E: Assessment of atherosclerotic risk factors and endothelial function in children and young adults with pediatric-onset systemic lupus erythematosus. Arthritis Rheum. 2004, 51: 451-457. 10.1002/art.20392.
Gomez-Zumaquero JM, Tinahones FJ, De Ramon E, Camps M, Garrido L, Sorguer FJ: Association of biological markers of activity of systemic lupus erythematosus with levels of anti-oxidized low-density lipoprotein antibodies. Rheumatology (Oxford). 2004, 43: 510-513. 10.1093/rheumatology/keh109.
Svenungsson E, Jensen-Urstad K, Heimburger M, Silveira A, Hamsten A, de Faire U, Witzgum JL, Frostegard J: Risk factors for cardiovascular disease in systemic lupus erythematosus. Circulation. 2001, 104: 1887-1893. 10.1161/hc4101.097518.
Romero FI, Amengual OK, Atsumi T, Khamashta MA, Tinahones FJ, Hughes GR: Arterial disease in lupus and secondary antiphospholipid syndrome: association with anti-beta2-gly-coprotein 1 antibodies but not with antibodies against oxidized low-density lipoprotein. Br J Rheumatol. 1998, 37: 883-888. 10.1093/rheumatology/37.8.883.
Hayem G, Nicaise-Roland P, Palazzo E, de Bandt M, Tuback F, Weber M, Meyer OI: Anti-oxidized low-density lipoprotein (OxLDL) antibodies in systemic lupus erythematosus with and without antiphospholipid syndrome. Lupus. 2001, 10: 346-351. 10.1191/096120301667475689.
Deguchi H, Fernandez JA, Hackeng RM, Banka CL, Griffin JH: Cardiolipin is a normal component of human plasma lipoproteins. Proc Natl Acad Sci USA. 2000, 97: 1743-1748. 10.1073/pnas.97.4.1743.
Hasunuma Y, Matsuura E, Makita Z, Katahira T, Nishi S, Koike T: Involvement of beta 2-glycoprotein 1 and anticardiolipin antibodies in oxidatively modified low-density lipoprotein uptake by macrophages. Clin Exp Immunol. 1997, 107: 569-573. 10.1046/j.1365-2249.1997.d01-948.x.
Kobayashi K, Kishi M, Atsumi T, Bertolaccini ML, Makino H, Sakairi N, Yamamoto I, Yasuda T, Khamashta MA, Hughes GR, Koike T, Voelker DR, Matsuura E: Circulating oxidized LDL forms complexes with beta2-glycoprotein 1: implication as an atherogenic autoantigen. J Lipid Res. 2003, 44: 716-726. 10.1194/jlr.M200329-JLR200.
Kobayashi K, Matsuura E, Liu Q, Furukawa J, Kaihara K, Inagaki J, Atsumi T, Sakairi N, Yasuda T, Voelker DR, Koike T: A specific legan for beta(2)-glycoprotein 1 mediates autoantibody-dependent uptake of oxidized low density lipoprotein by macrophages. J Lipid Res. 2001, 42: 697-709.
Mustafa A, Nityanand S, Berglund L, Lithell H, Lefvert AK: Circulating immune complexes in 50-year-old men as a strong and independent risk factor for myocardial infarction. Circulation. 2000, 102: 2576-2581.
Virella G, Atchley D, Koskinen S, Zheng D, Lopes-Virella MF: Proatherogenic and proinflammatory properties of immune complexes prepared with purified human oxLDL antibodies and human oxLDL. Clin Immunol. 2002, 105: 81-92. 10.1006/clim.2002.5269.
Sherer Y, Shoenfeld Y: Mechanisms of disease: atherosclerosis in autoimmune diseases. Nat Clin Pract Rheumatol. 2006, 2: 3337-3347. 10.1038/ncprheum0092.
Henrichot E, Juge-Aubry CE, Pernin A, Pache JC, Velebit V, Dayer JM, Meda P, Chizzolini C, Meier CA: Production of chemokines by perivascular adipose tissue: a role in the pathogenesis of atherosclerosis?. Arterioscler Thromb Vasc Biol. 2005, 25: 2594-2599. 10.1161/01.ATV.0000188508.40052.35.
McMahon , Maureen , Hahn BH: Atherosclerosis and systemic lupus erythematosus – mechanistic basis of the association. Curr Opin Immunol. 2007, 19: 633-639. 10.1016/j.coi.2007.11.001.
Ansell BJ, Fonarow GC, Fogelman AM: The paradox of dysfunctional high-density lipoprotein. Curr Opin Lipidol. 2007, 18: 427-434. 10.1097/MOL.0b013e3282364a17.
Gowri MS, Westhuyzen Van der DR, Bridges SR, Anderson JW: Decreased protection by HDL from poorly controlled type 2 diabetic subjects against LDL oxidation may be due to the abnormal composition of HDL. Arterioscler Thromb Vasc Biol. 1999, 19: 2226-2233.
Sviridov D, Chin-Dusting J, Nestel P, Kingwell B, Hoang A, Olchawa B, Starr J, Dart A: Elevated HDL Cholesterol is functionally ineffective in cardiac transplant recipients: evidence for impaired reverse cholesterol transport. Transplantation. 2006, 81: 361-366. 10.1097/01.tp.0000197556.83675.a6.
Kaysen GA: Disorders in high-density metabolism with insulin resistance and chronic kidney disease. J Ren Nutr. 2007, 17: 4-8. 10.1053/j.jrn.2006.10.002.
Nissen SE, Tsunoda T, Tuzcu EM, Schoenhagen P, Cooper CJ, Yasin M, Eaton GM, Lauer MA, Sheldon WS, Grines CL, Halpern S, Crowe T, Blankenship JC, Kerensky R: Effect of recombinant ApoA-I Milano on coronary atherosclerosis in patients with acute coronary syndromes: a randomized controlled trial. JAMA. 2003, 290: 2292-2300. 10.1001/jama.290.17.2292.
Ansell BJ, Navab M, Hama S, Kamranpour N, Fonarow G, Hough G, Rahmani S, Mottahedeh R, Dave R, Reddy ST, Fogelman AM: Inflammatory/anti-inflammatory properties of high-density lipoprotein distinguish patients from control subjects better than high-density lipoprotein cholesterol levels and are favorably affected by simvastatin treatment. Circulation. 2003, 108: 2751-2756. 10.1161/01.CIR.0000103624.14436.4B.
Charles-Schoeman C, Khanna D, Furst DE, McMahon M, Reddy ST, Fogelman AM, Paulus HE, Park GS, Gong T, Ansell BJ: Effects of high-dose atorvastatin on HDL anti-inflammatory/pro-inflammatory function and disease activity in patients with rheumatoid arthritis. Results of the Statin Anti-Rheumatic Activity (SARA) pilot study. J Rheumatol. 2007, 34: 1459-1464.
Roberts CK, Ng C, Hama S, Eliseo AJ, Barnard RJ: Effect of a short-term diet and exercise intervention on inflammatory/anti-inflammatory properties of HDL in overweight/obese men with cardiovascular risk factors. J Appl Physiol. 2006, 101: 1727-1732. 10.1152/japplphysiol.00345.2006.
Navab M, Anantharamaiah GM, Reddy ST, Hama S, Hough G, Grijalva VR, Wagner AC, Frank JS, Datta G, Garber D, Fogelman AM: Oral D-4F causes formation of prebeta high-density lipoprotein and improves high-density lipoprotein-mediated cholesterol efflux and reverse cholesterol transport from macrophages in apolipoprotein E-null mice. Circulation. 2004, 109: 3215-3220. 10.1161/01.CIR.0000134275.90823.87.
Bloedon LT, Dunbar R, Duffy D, Pinell-Salles P, Norris R, DeGroot BJ, Movva R, Navab M, Fogelman AM, Rader DJ: Safety, pharmacokinetics, and pharmacodynamics of oral apoA-I mimetic peptide D-4F in high-risk cardiovascular patients. J Lipid Res. 2008, 49: 1344-1352. 10.1194/jlr.P800003-JLR200.
Navab M, Anantharamaiah GM, Reddy ST, Van Lenten BH, Wagner AC, Hama S, Hough G, Bachini E, Garger DW, Mishra VK, Palgunachari MN, Fogelman AM: An oral apoJ peptide renders HDL anti-inflammatory in mice and monkeys and dramatically reduces atherosclerosis in apolipoprotein E-null mice. Arterioscler Thromb Vasc Biol. 2005, 25: 1932-1937. 10.1161/01.ATV.0000174589.70190.e2.
Choi HK, Hernan MA, Seeger JD, Robins JM, Wolfe F: Methotrexate and mortality in patients with rheumatoid arthritis: a prospective study. Lancet. 2002, 360: 1096-1097. 10.1016/S0140-6736(02)11161-5.
Hausenloy DJ, Yellon DM: Targeting residual cardiovascular risk: raising high-density lipoprotein cholesterol levels. Heart. 2008, 94: 706-714. 10.1136/hrt.2007.125401.
Tall AR: Cholesterol efflux pathways and other potential mechanisms involved in the atheroprotective effect of high density lipoproteins. J Intern Med. 2008, 263: 256-273. 10.1111/j.1365-2796.2007.01898.x.
Acknowledgements
Studies referenced in this manuscript were supported by grants from the Lupus Research Institute (to BHH), the Alliance for Lupus Research (to BHH), the American College of Rheumatology/Lupus Research Institute Lupus Fellowship (to MM), a Kirkland Award (to BHH), and an award from the National Institute of Arthritis, Skin and Musculoskeletal Diseases (1K23AR053864-01A1) (to MM).
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
About this article
Cite this article
Hahn, B.H., Grossman, J., Ansell, B.J. et al. Altered lipoprotein metabolism in chronic inflammatory states: proinflammatory high-density lipoprotein and accelerated atherosclerosis in systemic lupus erythematosus and rheumatoid arthritis. Arthritis Res Ther 10, 213 (2008). https://doi.org/10.1186/ar2471
Published:
DOI: https://doi.org/10.1186/ar2471