Abstract
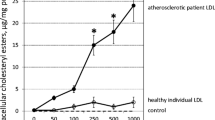
Disordered lipid accumulation in the arterial wall is a hallmark of atherosclerosis. Previous studies found that the expression of triggering receptor expressed on myeloid cells 2 (TREM2), a transmembrane receptor of the immunoglobulin family, is increased in mouse atherosclerotic aortic plaques. However, it remains unknown whether TREM2 plays a role in atherosclerosis. Here we investigated the role of TREM2 in atherosclerosis using ApoE knockout (ApoE−/−) mouse models, primary vascular smooth muscle cells (SMCs), and bone marrow-derived macrophages (BMDMs). In ApoE−/− mice, the density of TREM2-positive foam cells in aortic plaques increased in a time-dependent manner after the mice were fed a high-fat diet (HFD). Compared with ApoE−/− mice, the Trem2−/−/ApoE−/− double-knockout mice showed significantly reduced atherosclerotic lesion size, foam cell number, and lipid burden degree in plaques after HFD feeding. Overexpression of TREM2 in cultured vascular SMCs and macrophages exacerbates lipid influx and foam cell formation by upregulating the expression of the scavenger receptor CD36. Mechanistically, TREM2 inhibits the phosphorylation of p38 mitogen-activated protein kinase and peroxisome proliferator activated-receptor gamma (PPARγ), thereby increasing PPARγ nuclear transcriptional activity and subsequently promoting the transcription of CD36. Our results indicate that TREM2 exacerbates atherosclerosis development by promoting SMC- and macrophage-derived foam cell formation by regulating scavenger receptor CD36 expression. Thus, TREM2 may act as a novel therapeutic target for the treatment of atherosclerosis.
Graphical abstract








Similar content being viewed by others
Data availability
All the data supporting the findings of this study are available within the paper. Data will be made available on reasonable request, not applicable for material.
Abbreviations
- ApoE −/− :
-
Apolipoprotein E knockout
- AS:
-
Atherosclerosis
- BMDMs:
-
Bone marrow-derived macrophages
- BODIPY:
-
4,4-difluoro-1,3,5,7,8-pentamethyl-4-bora-3a,4a-diaza-s-indacene
- CD36:
-
Cluster of differentiation 36 Deh dehydrocorydaline
- DAPI:
-
4ʹ,6-diamidino-2-phenylindole
- DEGs:
-
Differentially expressed genes
- Deh:
-
Dehydrocorydaline
- DiI-oxLDL:
-
Dil-labeled oxLDL
- GEO:
-
Gene Expression Omnibus
- HFD:
-
High-fat diet
- IF:
-
Immunofluorescence
- MAPK:
-
Mitogen-activated protein kinase
- M-CSF:
-
Macrophage colony-stimulating factor
- Mfi:
-
Mean fluorescence intensity
- mSMCs:
-
Mouse primary aortic SMCs
- ORO:
-
Oil Red O
- OxLDL:
-
Oxidized low-density lipoprotein
- p-ERK1/2:
-
Phosphorylated ERK1/2
- p-JNK:
-
Phosphorylated JNK
- p-p38:
-
Phosphorylated p38
- PPARγ:
-
Peroxisome proliferator activated-receptor gamma
- SMCs:
-
Vascular smooth muscle cells
- t-ERK1/2:
-
Total ERK1/2
- t-JNK:
-
Total JNK
- t-p38:
-
Total p38
- TREM2:
-
Triggering receptor expressed on myeloid cells 2
- α-SMA:
-
α-Smooth muscle actin
References
Herrington W, Lacey B, Sherliker P, Armitage J, Lewington S (2016) Epidemiology of atherosclerosis and the potential to reduce the global burden of atherothrombotic disease. Circ Res 118:535–546. https://doi.org/10.1161/CIRCRESAHA.115.307611
Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R et al (2017) Heart disease and stroke statistics-2017 update: a report from the American Heart Association. Circulation 135:e146–e603. https://doi.org/10.1161/CIR.0000000000000485
Pi S, Mao L, Chen J, Shi H, Liu Y, Guo X et al (2021) The P2RY12 receptor promotes VSMC-derived foam cell formation by inhibiting autophagy in advanced atherosclerosis. Autophagy 17:980–1000. https://doi.org/10.1080/15548627.2020.1741202
Tabas I, Bornfeldt KE (2016) Macrophage phenotype and function in different stages of atherosclerosis. Circ Res 118:653–667. https://doi.org/10.1161/CIRCRESAHA.115.306256
Allahverdian S, Chehroudi AC, McManus BM, Abraham T, Francis GA (2014) Contribution of intimal smooth muscle cells to cholesterol accumulation and macrophage-like cells in human atherosclerosis. Circulation 129:1551–1559. https://doi.org/10.1161/CIRCULATIONAHA.113.005015
Feil S, Fehrenbacher B, Lukowski R, Essmann F, Schulze-Osthoff K, Schaller M et al (2014) Transdifferentiation of vascular smooth muscle cells to macrophage-like cells during atherogenesis. Circ Res 115:662–667. https://doi.org/10.1161/CIRCRESAHA.115.304634
Wang D, Yang Y, Lei Y, Tzvetkov NT, Liu X, Yeung AWK et al (2019) Targeting foam cell formation in atherosclerosis: therapeutic potential of natural products. Pharmacol Rev 71:596–670. https://doi.org/10.1124/pr.118.017178
Childs BG, Baker DJ, Wijshake T, Conover CA, Campisi J, van Deursen JM (2016) Senescent intimal foam cells are deleterious at all stages of atherosclerosis. Science 354:472–477. https://doi.org/10.1126/science.aaf6659
Deczkowska A, Weiner A, Amit I (2020) The physiology, pathology, and potential therapeutic applications of the TREM2 signaling pathway. Cell 181:1207–1217. https://doi.org/10.1016/j.cell.2020.05.003
Shi Y, Holtzman DM (2018) Interplay between innate immunity and Alzheimer disease: APOE and TREM2 in the spotlight. Nat Rev Immunol 18:759–772. https://doi.org/10.1038/s41577-018-0051-1
Kober DL, Brett TJ (2017) TREM2–ligand interactions in health and disease. J Mol Biol 429:1607–1629. https://doi.org/10.1016/j.jmb.2017.04.004
Zhang J, Liu Y, Zheng Y, Luo Y, Du Y, Zhao Y et al (2020) TREM-2-p38 MAPK signaling regulates neuroinflammation during chronic cerebral hypoperfusion combined with diabetes mellitus. J Neuroinflammation 17:2. https://doi.org/10.1186/s12974-019-1688-9
Jaitin DA, Adlung L, Thaiss CA, Weiner A, Li B, Descamps H et al (2019) Lipid-associated macrophages control metabolic homeostasis in a Trem2-dependent manner. Cell 178:686-698 e14. https://doi.org/10.1016/j.cell.2019.05.054
Zernecke A, Winkels H, Cochain C, Williams JW, Wolf D, Soehnlein O et al (2020) Meta-analysis of leukocyte diversity in atherosclerotic mouse aortas. Circ Res 127:402–426. https://doi.org/10.1161/CIRCRESAHA.120.316903
Damisah EC, Rai A, Grutzendler J (2020) TREM2: modulator of lipid metabolism in microglia. Neuron 105:759–761. https://doi.org/10.1016/j.neuron.2020.02.008
Depuydt MAC, Prange KHM, Slenders L, Ord T, Elbersen D, Boltjes A et al (2020) Microanatomy of the human atherosclerotic plaque by single-cell transcriptomics. Circ Res 127:1437–1455. https://doi.org/10.1161/CIRCRESAHA.120.316770
Cochain C, Vafadarnejad E, Arampatzi P, Pelisek J, Winkels H, Ley K et al (2018) Single-cell RNA-Seq reveals the transcriptional landscape and heterogeneity of aortic macrophages in murine atherosclerosis. Circ Res 122:1661–1674. https://doi.org/10.1161/CIRCRESAHA.117.312509
Kim K, Shim D, Lee JS, Zaitsev K, Williams JW, Kim KW et al (2018) Transcriptome analysis reveals nonfoamy rather than foamy plaque macrophages are proinflammatory in atherosclerotic murine models. Circ Res 123:1127–1142. https://doi.org/10.1161/CIRCRESAHA.118.312804
Reddick RL, Zhang SH, Maeda N (1994) Atherosclerosis in mice lacking apo E. Evaluation of lesional development and progression. Arterioscler Thromb 14:141–147. https://doi.org/10.1161/01.atv.14.1.141
Jawien J, Nastalek P, Korbut R (2004) Mouse models of experimental atherosclerosis. J Physiol Pharmacol 55:503–517
Feng B, Zhang D, Kuriakose G, Devlin CM, Kockx M, Tabas I (2003) Niemann-Pick C heterozygosity confers resistance to lesional necrosis and macrophage apoptosis in murine atherosclerosis. Proc Natl Acad Sci USA 100:10423–10428. https://doi.org/10.1073/pnas.1732494100
Niu X, Pi SL, Baral S, Xia YP, He QW, Li YN et al (2017) P2Y12 promotes migration of vascular smooth muscle cells through cofilin dephosphorylation during atherogenesis. Arterioscler Thromb Vasc Biol 37:515–524. https://doi.org/10.1161/ATVBAHA.116.308725
Le Guezennec X, Brichkina A, Huang YF, Kostromina E, Han W, Bulavin DV (2012) Wip1-dependent regulation of autophagy, obesity, and atherosclerosis. Cell Metab 16:68–80. https://doi.org/10.1016/j.cmet.2012.06.003
Xu S, Huang Y, Xie Y, Lan T, Le K, Chen J et al (2010) Evaluation of foam cell formation in cultured macrophages: an improved method with Oil Red O staining and DiI-oxLDL uptake. Cytotechnology 62:473–481. https://doi.org/10.1007/s10616-010-9290-0
Selvais CM, Davis-Lopez de Carrizosa MA, Nachit M, Versele R, Dubuisson N, Noel L et al (2023) AdipoRon enhances healthspan in middle-aged obese mice: striking alleviation of myosteatosis and muscle degenerative markers. J Cachexia Sarcopenia Muscle 14:464–478. https://doi.org/10.1002/jcsm.13148
Niu X, Pi SL, Baral S, Xia YP, He QW, Li YN et al (2017) P2Y(12) promotes migration of vascular smooth muscle cells through cofilin dephosphorylation during atherogenesis. Arterioscler Thromb Vasc Biol 37:515–524. https://doi.org/10.1161/ATVBAHA.116.308725
Livak KJ, Schmittgen TD (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods 25:402–408. https://doi.org/10.1006/meth.2001.1262
Cochain C, Saliba AE, Zernecke A (2018) Letter by cochain et al regarding article, “Transcriptome analysis reveals nonfoamy rather than foamy plaque macrophages are proinflammatory in atherosclerotic murine models.” Circ Res 123:e48–e49. https://doi.org/10.1161/CIRCRESAHA.118.314120
Yang S, Xia YP, Luo XY, Chen SL, Li BW, Ye ZM et al (2019) Exosomal CagA derived from Helicobacter pylori-infected gastric epithelial cells induces macrophage foam cell formation and promotes atherosclerosis. J Mol Cell Cardiol 135:40–51. https://doi.org/10.1016/j.yjmcc.2019.07.011
Yeh FL, Wang Y, Tom I, Gonzalez LC, Sheng M (2016) TREM2 binds to apolipoproteins, including APOE and CLU/APOJ, and thereby facilitates uptake of amyloid-beta by microglia. Neuron 91:328–340. https://doi.org/10.1016/j.neuron.2016.06.015
Wang H, Franco F, Tsui YC, Xie X, Trefny MP, Zappasodi R et al (2020) CD36-mediated metabolic adaptation supports regulatory T cell survival and function in tumors. Nat Immunol 21:298–308. https://doi.org/10.1038/s41590-019-0589-5
Zhang C, Luo X, Chen J, Zhou B, Yang M, Liu R et al (2019) Osteoprotegerin promotes liver steatosis by targeting the ERK-PPAR-gamma-CD36 pathway. Diabetes 68:1902–1914. https://doi.org/10.2337/db18-1055
Chen CH, Leu SJ, Hsu CP, Pan CC, Shyue SK, Lee TS (2021) Atypical antipsychotic drugs deregulate the cholesterol metabolism of macrophage-foam cells by activating NOX-ROS-PPARgamma-CD36 signaling pathway. Metabolism 123:154847. https://doi.org/10.1016/j.metabol.2021.154847
Cargnello M, Roux PP (2011) Activation and function of the MAPKs and their substrates, the MAPK-activated protein kinases. Microbiol Mol Biol Rev 75:50–83. https://doi.org/10.1128/MMBR.00031-10
Kim EK, Choi EJ (2015) Compromised MAPK signaling in human diseases: an update. Arch Toxicol 89:867–882. https://doi.org/10.1007/s00204-015-1472-2
Oppi S, Nusser-Stein S, Blyszczuk P, Wang X, Jomard A, Marzolla V et al (2020) Macrophage NCOR1 protects from atherosclerosis by repressing a pro-atherogenic PPARgamma signature. Eur Heart J 41:995–1005. https://doi.org/10.1093/eurheartj/ehz667
Haass C (2021) Loss of TREM2 facilitates tau accumulation, spreading, and brain atrophy, but only in the presence of amyloid pathology. Neuron 109:1243–1245. https://doi.org/10.1016/j.neuron.2021.03.029
Lee SH, Meilandt WJ, Xie L, Gandham VD, Ngu H, Barck KH et al (2021) Trem2 restrains the enhancement of tau accumulation and neurodegeneration by beta-amyloid pathology. Neuron 109:1283-1301 e6. https://doi.org/10.1016/j.neuron.2021.02.010
Park M, Yi JW, Kim EM, Yoon IJ, Lee EH, Lee HY et al (2015) Triggering receptor expressed on myeloid cells 2 (TREM2) promotes adipogenesis and diet-induced obesity. Diabetes 64:117–127. https://doi.org/10.2337/db13-1869
Nugent AA, Lin K, van Lengerich B, Lianoglou S, Przybyla L, Davis SS et al (2020) TREM2 regulates microglial cholesterol metabolism upon chronic phagocytic challenge. Neuron 105:837-854 e9. https://doi.org/10.1016/j.neuron.2019.12.007
Ulland TK, Song WM, Huang SC, Ulrich JD, Sergushichev A, Beatty WL et al (2017) TREM2 maintains microglial metabolic fitness in Alzheimer’s disease. Cell 170:649-663 e13. https://doi.org/10.1016/j.cell.2017.07.023
Willemsen L, de Winther MP (2020) Macrophage subsets in atherosclerosis as defined by single-cell technologies. J Pathol 250:705–714. https://doi.org/10.1002/path.5392
Xu YL, Liu XY, Cheng SB, He PK, Hong MK, Chen YY et al (2020) Geniposide enhances macrophage autophagy through downregulation of TREM2 in atherosclerosis. Am J Chin Med 48:1821–1840. https://doi.org/10.1142/S0192415X20500913
Do TH, Ma F, Andrade PR, Teles R, de Andrade Silva BJ, Hu C et al (2022) TREM2 macrophages induced by human lipids drive inflammation in acne lesions. Sci Immunol 7:eabo2787. https://doi.org/10.1126/sciimmunol.abo2787
Bartels ED, Christoffersen C, Lindholm MW, Nielsen LB (2015) Altered metabolism of LDL in the arterial wall precedes atherosclerosis regression. Circ Res 117:933–942. https://doi.org/10.1161/CIRCRESAHA.115.307182
Ouimet M, Marcel YL (2012) Regulation of lipid droplet cholesterol efflux from macrophage foam cells. Arterioscler Thromb Vasc Biol 32:575–581. https://doi.org/10.1161/ATVBAHA.111.240705
Matsuo M (2022) ABCA1 and ABCG1 as potential therapeutic targets for the prevention of atherosclerosis. J Pharmacol Sci 148:197–203. https://doi.org/10.1016/j.jphs.2021.11.005
Yu XH, Fu YC, Zhang DW, Yin K, Tang CK (2013) Foam cells in atherosclerosis. Clin Chim Acta 424:245–252. https://doi.org/10.1016/j.cca.2013.06.006
Platt N, Gordon S (2001) Is the class A macrophage scavenger receptor (SR-A) multifunctional?—The mouse’s tale. J Clin Invest 108:649–654. https://doi.org/10.1172/JCI13903
Shu H, Peng Y, Hang W, Nie J, Zhou N, Wang DW (2022) The role of CD36 in cardiovascular disease. Cardiovasc Res 118:115–129. https://doi.org/10.1093/cvr/cvaa319
Linnartz-Gerlach B, Bodea LG, Klaus C, Ginolhac A, Halder R, Sinkkonen L et al (2019) TREM2 triggers microglial density and age-related neuronal loss. Glia 67:539–550. https://doi.org/10.1002/glia.23563
Collot-Teixeira S, Martin J, McDermott-Roe C, Poston R, McGregor JL (2007) CD36 and macrophages in atherosclerosis. Cardiovasc Res 75:468–477. https://doi.org/10.1016/j.cardiores.2007.03.010
Tian K, Xu Y, Sahebkar A, Xu S (2020) CD36 in atherosclerosis: pathophysiological mechanisms and therapeutic implications. Curr Atheroscler Rep 22:59. https://doi.org/10.1007/s11883-020-00870-8
Hendrikx T, Porsch F, Kiss MG, Rajcic D, Papac-Milicevic N, Hoebinger C et al (2022) Soluble TREM2 levels reflect the recruitment and expansion of TREM2(+) macrophages that localize to fibrotic areas and limit NASH. J Hepatol. https://doi.org/10.1016/j.jhep.2022.06.004
Kim SM, Mun BR, Lee SJ, Joh Y, Lee HY, Ji KY et al (2017) TREM2 promotes Abeta phagocytosis by upregulating C/EBPalpha-dependent CD36 expression in microglia. Sci Rep 7:11118. https://doi.org/10.1038/s41598-017-11634-x
Tontonoz P, Nagy L, Alvarez JG, Thomazy VA, Evans RM (1998) PPARgamma promotes monocyte/macrophage differentiation and uptake of oxidized LDL. Cell 93:241–252. https://doi.org/10.1016/s0092-8674(00)81575-5
Huang CC, Chou CA, Chen WY, Yang JL, Lee WC, Chen JB et al (2021) Empagliflozin ameliorates free fatty acid induced-lipotoxicity in renal proximal tubular cells via the PPARgamma/CD36 pathway in obese mice. Int J Mol Sci. https://doi.org/10.3390/ijms222212408
Kotla S, Singh NK, Rao GN (2017) ROS via BTK-p300-STAT1-PPARgamma signaling activation mediates cholesterol crystals-induced CD36 expression and foam cell formation. Redox Biol 11:350–364. https://doi.org/10.1016/j.redox.2016.12.005
Wu L, Zhang S, Zhang Q, Wei S, Wang G, Luo P (2022) The molecular mechanism of hepatic lipid metabolism disorder caused by NaAsO2 through regulating the ERK/PPAR signaling pathway. Oxid Med Cell Longev 2022:6405911. https://doi.org/10.1155/2022/6405911
Nicholson AC (2004) Expression of CD36 in macrophages and atherosclerosis: the role of lipid regulation of PPARgamma signaling. Trends Cardiovasc Med 14:8–12. https://doi.org/10.1016/j.tcm.2003.09.004
Feng J, Han J, Pearce SF, Silverstein RL, Gotto AM Jr, Hajjar DP et al (2000) Induction of CD36 expression by oxidized LDL and IL-4 by a common signaling pathway dependent on protein kinase C and PPAR-gamma. J Lipid Res 41:688–696
Li H, Ruan XZ, Powis SH, Fernando R, Mon WY, Wheeler DC et al (2005) EPA and DHA reduce LPS-induced inflammation responses in HK-2 cells: evidence for a PPAR-gamma-dependent mechanism. Kidney Int 67:867–874. https://doi.org/10.1111/j.1523-1755.2005.00151.x
Lim HJ, Lee S, Lee KS, Park JH, Jang Y, Lee EJ et al (2006) PPARgamma activation induces CD36 expression and stimulates foam cell like changes in rVSMCs. Prostaglandins Other Lipid Mediat 80:165–174. https://doi.org/10.1016/j.prostaglandins.2006.06.006
Lu Y, Zhang M, Wang S, Hong B, Wang Z, Li H et al (2014) p38 MAPK-inhibited dendritic cells induce superior antitumour immune responses and overcome regulatory T-cell-mediated immunosuppression. Nat Commun 5:4229. https://doi.org/10.1038/ncomms5229
Han Y, Wang J, Jin M, Jia L, Yan C, Wang Y (2021) Shentong Zhuyu decoction inhibits inflammatory response, migration, and invasion and promotes apoptosis of rheumatoid arthritis fibroblast-like synoviocytes via the MAPK p38/PPARgamma/CTGF pathway. Biomed Res Int 2021:6187695. https://doi.org/10.1155/2021/6187695
Hua B, Liu Q, Gao S, Li W, Li H (2022) Protective role of activating PPARgamma in advanced glycation end products-induced impairment of coronary artery vasodilation via inhibiting p38 phosphorylation and reactive oxygen species production. Biomed Pharmacother 147:112641. https://doi.org/10.1016/j.biopha.2022.112641
Tian C, Jin X, Ye X, Wu H, Ren W, Zhang R et al (2014) Long term intake of 0.1% ethanol decreases serum adiponectin by suppressing PPARgamma expression via p38 MAPK pathway. Food Chem Toxicol 65:329–334. https://doi.org/10.1016/j.fct.2014.01.007
Liu Y, Shepherd EG, Nelin LD (2007) MAPK phosphatases-regulating the immune response. Nat Rev Immunol 7:202–212. https://doi.org/10.1038/nri2035
Bassi R, Heads R, Marber MS, Clark JE (2008) Targeting p38-MAPK in the ischaemic heart: kill or cure? Curr Opin Pharmacol 8:141–146. https://doi.org/10.1016/j.coph.2008.01.002
Huang W, Lv Q, Xiao Y, Zhong Z, Hu B, Yan S et al (2021) triggering receptor expressed on myeloid cells 2 protects dopaminergic neurons by promoting autophagy in the inflammatory pathogenesis of Parkinson’s disease. Front Neurosci 15:745815. https://doi.org/10.3389/fnins.2021.745815
Su VY, Yang KY, Chiou SH, Chen NJ, Mo MH, Lin CS et al (2019) Induced pluripotent stem cells regulate triggering receptor expressed on myeloid cell-1 expression and the p38 mitogen-activated protein kinase pathway in endotoxin-induced acute lung injury. Stem Cells 37:631–639. https://doi.org/10.1002/stem.2980
Ruganzu JB, Peng X, He Y, Wu X, Zheng Q, Ding B et al (2022) Downregulation of TREM2 expression exacerbates neuroinflammatory responses through TLR4-mediated MAPK signaling pathway in a transgenic mouse model of Alzheimer’s disease. Mol Immunol 142:22–36. https://doi.org/10.1016/j.molimm.2021.12.018
Gessi S, Fogli E, Sacchetto V, Merighi S, Varani K, Preti D et al (2010) Adenosine modulates HIF-1{alpha}, VEGF, IL-8, and foam cell formation in a human model of hypoxic foam cells. Arterioscler Thromb Vasc Biol 30:90–97. https://doi.org/10.1161/ATVBAHA.109.194902
Hopkins PN (2013) Molecular biology of atherosclerosis. Physiol Rev 93:1317–1542. https://doi.org/10.1152/physrev.00004.2012
Ren M, Guo Y, Wei X, Yan S, Qin Y, Zhang X et al (2018) TREM2 overexpression attenuates neuroinflammation and protects dopaminergic neurons in experimental models of Parkinson’s disease. Exp Neurol 302:205–213. https://doi.org/10.1016/j.expneurol.2018.01.016
Libby P, Buring JE, Badimon L, Hansson GK, Deanfield J, Bittencourt MS et al (2019) Atherosclerosis. Nat Rev Dis Primers 5:56. https://doi.org/10.1038/s41572-019-0106-z
Cholesterol Treatment Trialists C, Baigent C, Blackwell L, Emberson J, Holland LE, Reith C et al (2010) Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet 376:1670–1681. https://doi.org/10.1016/S0140-6736(10)61350-5
Collins R, Reith C, Emberson J, Armitage J, Baigent C, Blackwell L et al (2016) Interpretation of the evidence for the efficacy and safety of statin therapy. Lancet 388:2532–2561. https://doi.org/10.1016/S0140-6736(16)31357-5
Zheng SL, Roddick AJ (2019) Association of aspirin use for primary prevention with cardiovascular events and bleeding events: a systematic review and meta-analysis. JAMA 321:277–287. https://doi.org/10.1001/jama.2018.20578
Antithrombotic Trialists C (2002) Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ 324:71–86. https://doi.org/10.1136/bmj.324.7329.71
Acknowledgements
We thank the Central Laboratory of Union Hospital of Tongji Medical College for providing a confocal microscope and flow cytometer.
Funding
This work was supported by the National Natural Science Foundation of China (no. 81974182 and no. 82171325 to LM).
Author information
Authors and Affiliations
Contributions
Conceptualization: LM; methodology: XG and BL; formal analysis and investigation: XG, CW, FZ, XX, LN, and JC; writing–original draft preparation: XG and BL; writing–review and editing: LM and XG; funding acquisition: LM.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
This study was approved by the Tongji Medical School of Huazhong Technology University, China.
Consent to participate
Not applicable.
Consent for publication
All authors have been involved in writing the manuscript and consented to publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
18_2023_4786_MOESM1_ESM.pdf
Supplementary file1Fig. S1 TREM2 has no significant effect on body weight, lipid profile or collagen deposition. a. Antibody specificity validation of TREM2 molecules (red) in Trem2−/− mice. Scale bar: 50 µm. Nuclei were stained with DAPI (blue). b, Genotyping of TREM2 gene knockout in mice. Average body weights (c) and lipid profiles (d) of Trem2+/+/ApoE−/− and Trem2−/−/ApoE−/− mice (n = 6/group, student’s t-test). e, The percentage of collagen content and the thickness of fibrous caps were assessed in Masson staining images. Scale bar: 200 μm (n = 6/group, student’s t-test). *P < 0.05; ns, P > 0.05 (PDF 4323 KB)
18_2023_4786_MOESM2_ESM.pdf
Supplementary file2Fig. S2 TREM2 deficiency decreases CD36 expression. a, PCR-detected lentivirus overexpressing TREM2 in RAW264.7 cells and mSMCs (n = 6-7/group, student’s t-test). b, TREM2 stimulates primary BMDM foam cell formation. BMDMs isolated from Trem2+/+ and Trem2−/− mice were stimulated with oxLDL at 50 µg/mL for 24 h. Then the cells were incubated with BODIPY in DMEM for 1 h. A flow analyzer evaluated the mFI of the two groups of cells (n = 3/group, student’s t-test). c, Quantitative real-time PCR analysis of the mRNA levels of MSR1, OLR1, ABCA1 and ABCG1 in macrophages and mSMCs in the LV-GFP or LV-TREM2 group. Data are normalized to ACTB expression (n = 6/group, student’s t-test). d, Relative expression of CD36 (green) at the aortic sinus in Trem2+/+/ApoE−/− and Trem2−/−/ApoE−/− mice by immunofluorescence (n = 4/group, student’s t-test). Scale bar: 50 µm. e, Quantitative real-time PCR analysis of the mRNA levels of CD36 in primary BMDMs and mSMCs isolated from Trem2+/+ and Trem2−/− mice (n = 4/group, student’s t-test). *P < 0.05, **P < 0.01, ****P < 0.0001; ns, P > 0.05; mFI, mean fluorescence intensity (PDF 1510 KB)
18_2023_4786_MOESM3_ESM.pdf
Supplementary file3Fig. S3 Knockout of the TREM2 gene inhibits lipid uptake. a, Flow analysis showed the mFI of BMDMs isolated from Trem2+/+ and Trem2−/− mice stimulated with DiI-oxLDL at 10 µg/mL for 4 h (n = 3/group, student’s t-test). b, WB and PCR levels of CD36 expression in macrophages and mSMCs transfected with the control vector (NC) or the CD36 siRNA (siCD36, n = 4-6/group, student’s t-test). *P < 0.05, **P < 0.01, ****P < 0.0001; mFI, mean fluorescence intensity (PDF 123 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Guo, X., Li, B., Wen, C. et al. TREM2 promotes cholesterol uptake and foam cell formation in atherosclerosis. Cell. Mol. Life Sci. 80, 137 (2023). https://doi.org/10.1007/s00018-023-04786-9
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00018-023-04786-9