Abstract
The aim of the study was to evaluate the kinetic parameters of a specific serotonin transporter (SERT) and serotonin uptake in a mentally healthy subset of patients with fibromyalgia. Platelets were obtained from 40 patients and 38 healthy controls. SERT expression and functionality were evaluated through the measurement of [3H]paroxetine binding and the [3H]serotonin uptake itself. The values of maximal membrane binding capacity (Bmax) were statistically lower in the patients than in the healthy volunteers, whereas the dissociation constant (Kd) did not show any statistically significant variations. Moreover, a decrease in the maximal uptake rate of SERT (Vmax) was demonstrated in the platelets of patients, whereas the Michaelis constant (Km) did not show any statistically significant variations. Symptom severity score (tiredness, tender points index and Fibromyalgia Impact Questionnaire) were negatively correlated with Bmax and with Vmax, and positively correlated with Km. A change in SERT seems to occur in fibromyalgic patients, and it seems to be related to the severity of fibromyalgic symptoms.
Similar content being viewed by others
Introduction
Fibromyalgia syndrome (FMs) is a chronic pain syndrome characterized by widespread pain and stiffness, multiple tender points, and fatigue [1]. This pain syndrome has an incidence of 2% in the general population and occurs with higher frequency among women in middle age [2]. FM is often associated with increased prevalence of depressive symptoms, major depression and anxiety [3]. The cause and pathophysiology of FMs is unclear; pathophysiological hypotheses include impairment in the functioning of the hypothalamic-pituitary axis and alterations in specific neurotransmitters such as substance P, N-methyl-D-aspartate, noradrenaline (norepinephrine) and serotonin (5-HT). However, interest has been growing in a possible involvement of 5-HT in FM. Indeed, strong evidence has accumulated to support the hypothesis that a deficiency in serotonergic neuronal functioning might be related to the pathophysiology of FM [5–8]. Patients with FM have been found to have decreased concentrations of 5-HT and tryptophan (5-HT precursor) in serum and cerebrospinal fluid. 5-HT, in particular, is theorized to have a function in stage 4 sleep and in the pain threshold [9]. This neurotransmitter is implicated in psychiatric disorders such as depression, anxiety, and obsessive compulsive disorder. Stressful experiences lead to depression in some people who are already genetically predisposed, and increase the probability of FM exordium. The 5-HT gene could moderate the serotonergic response to stress [4].
As a mediator, 5-HT exerts its actions by means of interaction with distinct receptors, which are differentiated on the basis of structures, molecular mechanisms and pharmacological profiles [9]. On this basis, drugs acting on 5-HT receptors, in particular on 5-HT2 and 5-HT3, are being used or investigated for the clinical management of FM [10, 11]. Among drugs targeting 5-HT receptors, ketanserin is a selective 5-HT2 antagonist that can reduce the hyperalgesia, spontaneous pain, sleep disorders and other symptoms of FM [12], and granisetron and tropisetron are selective 5-HT3 receptor antagonists that show clinical efficacy in FM [11].
In an analogous manner to other transmitters, the endogenous activity of 5-HT is controlled by a specific 5-HT transporter (SERT), which mediates the intracellular reuptake of 5-HT and can be specifically blocked by selective 5-HT reuptake inhibitors (SSRIs) such as paroxetine and fluoxetine. SERT is widely expressed in intestinal epithelial cells, in central or peripheral serotonergic neurons and in platelets; it shares common molecular and physiological features in these locations [13–15]. Clinical studies have demonstrated the efficacy of SSRI in FM [16], but the data are not unequivocal. Nociception refers to the physiological process of transmitting a painful stimulus from the periphery through afferent neurons to the cerebral cortex. It has been postulated that serotonergic neurotransmission has a significant function in nociception [17, 18]; alterations in 5-HT metabolism and transmission might therefore be important in the pathogenesis of FM. These findings support the proposal that aberrant pain perception in FM also results from an instability of the 5-HT system in FM. There is also evidence that changes in the expression of SERT are due to a polymorphism in the transcription region in patients with FM [19].
In the present study, both the expression and functionality of SERT were determined in platelets collected from patients with FM, with the following aims: first, to perform a comparison with the pharmacological profile of platelet SERT in healthy volunteers, and second, to examine putative correlations of SERT characteristics with the severity of symptoms such as tiredness, Fibromyalgia Impact Questionnaire (FIQ) score or tender point index (TPi).
Materials and methods
Materials
[3H]Serotonin (specific radioactivity 30 Ci/mmol) and [3H]paroxetine (specific radioactivity 19.1 Ci/mmol) were purchased from Perkin-Elmer Life Science (Milano, Italy). All other reagents were obtained from normal commercial sources.
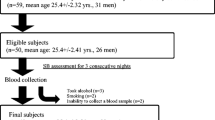
Subjects
Forty patients (all female) affected by primary FM, aged 53 ± 13 years (mean ± SD) took part in the study, and 38 healthy females age-matched to the patients (50 ± 12 years) were used as a control group. The American College of Rheumatology criteria for FM [1] were used to make the diagnosis of FM. The inclusion criteria for the study groups comprised a negative history for psychoactive drug treatment and other neurological disorders. None of the subjects had comorbid psychiatric disorders or had received treatment with antidepressant drugs. No patient was under pharmacological treatment. All patients underwent a wash-out period of 2 months before the study. They were enrolled at the University Division of Rheumatology, Santa Chiara Hospital, Pisa. Written consent was obtained from all patients and controls after a full explanation of the procedure. The study was approved by the local Ethics Committee.
Evaluation of clinical parameters
For each patient and control, tenderness at tender points was evaluated by means of the Fischer dolorimeter [20]. The total fibromyalgic tender point score (right plus left) was used for statistical analysis. Each positive tender point had a pain score between 0 (no pain) and 3 (severe pain). We also calculated the TPi as the sum of the scores of all tender points divided by the total number of tender points.
To estimate the impact of FM on the quality of life, all patients and controls received an FIQ [21]. The total score was the sum of the values of the 10 FIQ items, which reflected the impact of FM and ranged from 0 (no impact) to 100 (maximum impact).
Tiredness was evaluated as measured by the FIQ tiredness item, which consisted of a visual analogic scale numbered between 0 and 10.
To exclude major psychiatric disorders, all patients were evaluated by means of a diagnostic interview consisting of the administration of the Structured Clinical Interview for DSM-IV axis-I disorder (SCID-I/P) [22]. This assessment was conducted by psychiatrists who were trained and certified in the use of the study instruments at our department.
Separation of platelets
Venous blood (30 ml) was collected from each subject and gently mixed with 1 ml of anticoagulant (0.15 M EDTA). Platelet-rich plasma was obtained by low-speed centrifugation (200g for 20 minutes at 22°C). Platelets were counted automatically with a flux cytometer (Cell-dyn 3500 system; Abbott, Milano, Italy).
For measurement of [3H]serotonin reuptake, platelets were used immediately, whereas for [3H]paroxetine binding, platelets were precipitated by centrifugation at 10,000g for 10 minutes at 4°C and the pellets were then stored at -80°C until the assay.
[3H]Serotonin uptake
[3H]Serotonin uptake was performed as described by Arora and Meltzer [23], with some modifications. Aliquots of platelets (2 × 106 platelets) were incubated for 10 minutes at 37°C with [3H]serotonin at six concentrations from 15 to 700 nM in an assay buffer (118 mM NaCl, 4.7 mM KCl, 1.07 mM MgSO4.7H2O, 1.17 mM KH2PO4, 25 mM NaHCO3, 11.6 mM glucose, pH 7.4, in the presence of 0.1% ascorbate and 100 μM Pargyline) to a final volume of 0.5 ml. Non-specific uptake was measured in the presence of 10 μM Fluoxetine.
Preparation of platelet membranes
The platelet pellets were washed with 10 ml of buffer (150 mM NaCl, 20 mM EDTA, 50 mM Tris-HCl, pH 7.4). Pellets were lysed and homogenized in 10 ml of buffer (5 mM Tris-HCl, 5 mM EDTA, pH 7.4, containing the following protease inhibitors: 200 μg/ml bacitracin, 160 μg/ml benzamidine and 20 μg/ml soybean trypsin inhibitor) with an Ultra-Turrax homogenizer and centrifuged twice at 30,000g for 15 minutes at 4°C. The resulting pellets were resuspended in ice-cold 50 mM Tris-HCl buffer, pH 7.4, containing protease inhibitors, and centrifuged at 50,000g for 15 minutes at 4°C. The pellets were then suspended with assay buffer (50 mM Tris-HCl, 120 mM NaCl, 5 mM KCl, pH 7.4).
Protein concentration was determined with the method of Lowry and colleagues [24] using bovine serum albumin as a standard.
[3H]Paroxetine binding assay to platelet membranes
[3H]Paroxetine binding was performed as described by Marazziti and colleagues [25]. The incubation mixture consisted of 100 μl of platelet membranes (50 to 100 μg of protein per tube), 50 μl of [3H]paroxetine at six concentrations (0.01, 0.025, 0.05, 0.25, 0.5 and 1 nM) and 1.85 ml of assay buffer. Specific binding was obtained by using 10 μM fluoxetine as a displacer.
Data analysis
Equilibrium-saturation binding data, the maximum binding capacity (Bmax, fmol/mg of protein) and the dissociation constant (Kd, nM) were analysed by means of the iterative curve-fitting computer programs EBDA and LIGAND (Kell for Windows, v. 6.0).
The maximal uptake rate of SERT (Vmax, pmol/109 cells per minute) and the Michaelis constant (Km, nM) were obtained by direct weighted nonlinear regression of uptake rate against [3H]serotonin concentration with GraphPad PRISM software (GraphPad, San Diego, CA, USA).
Statistical analysis was performed with Student's t test. The relationship between variables was checked with a two-tailed Spearman analysis.
Results
[3H]Paroxetine binding sites on the SERT of platelet membranes were used as a first marker of serotonergic function. Table 1 shows the mean Bmax values for the density, and Kd values for the affinity, of [3H]paroxetine binding on platelets in the patients and in the healthy controls. A statistically significant difference was found between the two groups for Bmax (1,048 ± 30 versus 1,260 ± 34 fmol/mg for control; mean ± SEM) but not for Kd (0.086 ± 0.021 nM versus 0.077 ± 0.012 nM for control; mean ± S.E.M.).
The evaluation of symptom severity in patients with FM (Table 2) yielded tiredness scores from 2 to 10 with a mean of 7.4 ± 2.2 (SD), TPi values from 1 to 3 with a mean of 2.2 ± 0.5 (SD), and FIQ scores from 8 to 94 with a mean of 57.1 ± 21.3 (SD). The severity of symptoms was shown to be related to the maximal binding capacity of platelet SERT, in that the statistical analysis showed a negative correlation between symptom scores and the respective Bmax values (p < 0.0001 for tiredness; p < 0.0001 for TPi and p < 0.0001 for FIQ). By contrast, no significant correlation was found when comparing symptom severity with Kd values.
Age did not seem to influence the binding parameters of platelet SERT in either patients with FM or healthy volunteers. [3H]Serotonin uptake on platelets was used as marker of the functionality of SERT. Vmax and Km values of [3H]serotonin uptake in patients with FM accounted for 90 ± 4 pmol/109 platelets per minute and 96 ± 15 nM, respectively (means ± SEM; Table 3). A comparison of these parameters with those in healthy volunteers indicated significant differences for Vmax values but not for Km values: whereas the mean Vmax in the patients with FM was significantly lower (90 ± 4 versus 114 ± 6 pmol/109 platelets per minute for controls; p < 0.001), the mean Km in the patients with FM was not significantly different (96 ± 15 versus 114 ± 15 nM for controls; Table 2).
The severity of the symptoms was related to Vmax and Km in that the statistical analysis showed a negative correlation between the symptom scores and the respective Vmax values (p < 0.0001 for tiredness; p < 0.05 for TPi and p < 0.001 for FIQ). We also found a positive correlation between Km values and tiredness (p < 0.001), TPi (p < 0.001) and FIQ (p < 0.001).
The covariate age was shown not to have an effect on the variability of the Vmax or Km values in either patients with FM or healthy volunteers.
Discussion
The present study is the first examination of the relationships between SERT expression and kinetic parameters of 5-HT uptake. We have found statistically significant differences in Bmax and Vmax values between patients with FM and controls. Moreover, we found a negative correlation between symptom scores and the respective Bmax and Vmax values (Bmax and Vmax versus tiredness, TPi and FIQ score). The platelet is considered to be a peripheral model of neuronal activity with respect to 5-HT function. In fact, previous studies have demonstrated that the same SERT is expressed in the central nervous system and platelets [14]. Moreover, the identity between the two structures, as confirmed by sequence homologies through cloning studies [15], has provoked a surge of different studies in neuropsychiatric disorders, given the possibility of exploring peripherally a mechanism of the central nervous system [26]. Recently it has been proposed that altered serotonergic neuronal function might be related to the pathophysiology of FM [5, 8, 27]. These findings prompted us to investigate the characteristics of SERT in the platelets of patients with FM. Bmax and Kd values of [3H]Paroxetine binding were assumed to represent SERT density and ligand binding affinity, respectively, whereas Vmax and Km values of [3H]Serotonin uptake were taken as estimates of SERT rate and affinity, respectively. A very interesting observation was that both binding and uptake parameters differed significantly from those of healthy volunteers.
The patients with FM have fewer SERTs expressed on the cellular membrane than healthy subjects (a decreased Bmax, perhaps because the SERTs are less transcribed). Besides having fewer SERTs, patients with FM have a deficit in functionality (demonstrated by a decrease in transport rate).
Such combined changes in Bmax and Vmax values allow the inference that the efficiency of 5-HT uptake by platelet SERT is altered. Our previous studies demonstrated an alteration of SERT density and of the uptake rate of SERT in psychiatric patients [28, 29]. Consistent with this suggestion was the correlation analysis in the present study: the lower the density and rate of SERT on platelet membranes, the higher the severity of FM symptoms. Moreover, the Km values were also positively correlated with tiredness, TPi and FIQ.
A reduced density and rate of SERT are consistent with previous observations indicating that levels of 5-HT are altered in patients with FM [30, 31]. The biophysiological mechanism of FM has been proposed to be similar to that in depression, and it has been suggested that this is likely to result from a neuroendocrine/neurotransmitter dysregulation [32]. However, we suppose that the alterations in Bmax and Vmax values are not related to the pathophysiology of FM but are a consequence of FM. Our hypothesis is that a decrease in Bmax and Vmax of SERT is due to a pain stimulus [33, 34].
It has been shown that the decreased pain perception threshold during depression is likely to result from a dysfunction in several neurotransmitter systems, especially the serotoninergic one, which is also involved in the pathophysiology of depression [35]. In addition, an excessive stimulation of peripheral 5-HT receptors would account for pain and might explain why the clinical use of 5-HT3 receptor antagonists such as tropisetron or granisetron can promote the relief of disturbance associated with FM [11, 36].
SERT has been investigated previously in patients with FM, with discordant results. Russell and colleagues [37] found a higher Bmax in patients with FM than in healthy controls, whereas other authors found normal Bmax values [28, 35] using [3H]Paroxetine or [3H]Imipramine [38]. In our experiments we used [3H]Paroxetine, which binds with high affinity to a specific population of binding sites located on human platelets and neuronal membranes, associated with 5-HT uptake mechanisms [39]. The present results indicate a decrease in the density and rate of platelet SERT in patients with FM, and allow us to propose a specific role for SERT in the pathogenesis of FM. In fact, we avoided the inclusion of patients with FM who had psychiatric components because it is known that in psychiatric disorders such as depression, the expression of SERT is altered [40–42] and it is very difficult to identify the role of the two components in patients with FM who have comorbid psychiatric disorders. Thus, the changes in Bmax and Vmax demonstrated in our study may be due to FM only.
There is also a possible contribution from 5-HT to the aetiology of FM because of the efficacy of SSRIs in the management of chronic pain in idiopathic pain disorders [43]. Thus, in view of the decreased Bmax and Vmax values found in our subset of mentally healthy patients, who were SSRI free, we propose that there is a compensatory mechanism in the central nervous system to relieve the pain. This may clarify the improvement in the therapeutic effectiveness of SSRI in the patients with FM.
Conclusion
This is to our knowledge the first observation that, apart from a decrease in expression, there is also an alteration in the rate of SERT which seems to depend not only on the SERT number. In fact, Bmax is not correlated with Vmax (data not shown).
In the patients with FM, the decrease in 5-HT levels, which had already been observed, together with the impaired SERT functionality, might contribute to the pathogenesis of the disease, both in quantity and rate. In fact, these two factors are important because they are correlated with the level of disease severity.
Thus, the results of the present study are in agreement with the hypothesis that a deficit in the 5-HT transporter site could be of pathogenetic significance in FM syndrome.
Abbreviations
- 5-HT:
-
= serotonin
- B max :
-
= maximal membrane binding capacity
- FIQ:
-
= Fibromyalgia Impact Questionnaire
- FM:
-
= fibromyalgia
- K d :
-
= dissociation constant
- K m :
-
= Michaelis constant
- SERT:
-
= specific serotonin transporter
- SSRI:
-
= selective 5-HT reuptake inhibitor
- TPi:
-
= tender point index
- V max :
-
= maximal uptake rate of SERT.
References
Wolfe F, Smythe HA, Yunus MD, Bennett RM, Bombardier C, Goldenberg DL, Tugwell P, Campbell SM, Abeles M, Clark P, et al: The American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia: report of the Multicenter Criteria Committee. Arthritis Rheum. 1990, 33: 160-172.
Wolfe F, Ross K, Anderson J, Russell IJ, Herbert L: The prevalence and characteristics of fibromyalgia in the general population. Arthritis Rheum. 1995, 38: 19-28.
Hudson JI, Goldenberg DL, Pope HG, Keck PE, Schlesinger L: Comorbidity of fibromyalgia with medical and psychiatric disorders. Am J Med. 1992, 92: 363-367. 10.1016/0002-9343(92)90265-D.
Caspi A, Sugden K, Moffitt TE, Taylor A, Craig IW, Harrington H, McClay J, Mill J, Martin J, Braithwaite A, Poulton R: Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science. 2003, 301: 386-389. 10.1126/science.1083968.
Neeck G: Pathogenic mechanisms of fibromyalgia. Ageing Res Rev. 2002, 1: 243-255. 10.1016/S1568-1637(01)00004-6.
Neeck G, Rieder W: Neuromediator and hormonal perturbations in fibromyalgia syndrome: results of chronic stress?. Baillieres Clin Rheumatol. 1994, 8: 763-775. 10.1016/S0950-3579(05)80047-0.
Yunus MB, Dailey JW, Aldag JC, Masi AT, Jobe PC: Plasma tryptophan and other amino acids in primary fibromyalgia: a controlled study. J Rheumatol. 1992, 19: 90-94.
Moldofsky H, Warsh JJ: Plasma tryptophan and musculoskeletal pain in non-articular rheumatism ('fibrositis syndrome'). Pain. 1978, 5: 65-71. 10.1016/0304-3959(78)90025-8.
Raymond JR, Mukhin YV, Gelasco A, Turner J, Collinsworth G, Gettys TW, Grewal JS, Garnovskaya MN: Multiplicity of mechanisms of serotonin receptor signal transduction. Pharmacol Ther. 2001, 92: 179-212. 10.1016/S0163-7258(01)00169-3.
Miller LJ, Kubes KL: Serotonergic agents in the treatment of fibromyalgia syndrome. Ann Pharmacother. 2002, 36: 707-712. 10.1345/aph.1A184.
Gursoy S, Erdal E, Herken H, Madenci E, Alasehirli B: Association of T102C polymorphism of the 5-HT2A receptor gene with psychiatric status in fibromyalgia syndrome. Rheumatol Int. 2001, 21: 58-61. 10.1007/s002960100130.
Stratz T, Fiebich B, Haus U, Muller W: Influence of tropisetron on the serum substance P levels in fibromyalgia patients. Scand J Rheumatol Suppl. 2004, 119: 41-43.
Stratz T, Mennet P, Benn HP, Muller W: Blocking of S2 receptors: a new treatment principle in generalized tendomyopathy (fibromyalgia)?. Z Rheumatol. 1991, 50: 21-22.
Chen JX, Pan H, Rothman TP, Wade PR, Gershon MD: Guinea pig 5-HT transporter: cloning, expression, distribution and function in intestinal sensory reception. Am J Physiol. 1998, 275: G433-G438.
Lesch KP, Wolozin BL, Murphy DL, Reiderer P: Primary structure of the human platelet serotonin uptake site: identity with the brain serotonin transporter. J Neurochem. 1993, 60: 2319-2322.
Lesch KP, Wolozin BL, Estler HC, Murphy DL, Riederer P: Isolation of cDNA encoding the human brain serotonin transporter. J Neural Transm Gen Sect. 1993, 91: 67-72. 10.1007/BF01244919.
Goldenberg D, Mayskiy M, Mossey C, Ruthazer R, Schmid C: A randomized, double blind crossover trial of fluoxetine and amitriptyline in the treatment of fibromylagia. Arthritis Rheum. 1996, 39: 1852-1859.
Russell IJ: Advances in fibromyalgia possible role for central neurochemicals. Am J Med Sci. 1998, 315: 377-384. 10.1097/00000441-199806000-00006.
Offenbaecher M, Bondy B, De Jonge S, Glatzeder K, Kruger M, Schoeps P, Ackenheil M: Possible association of fibromyalgia with a polymorphism in the serotonin transporter gene regulatory region. Arthritis Rheum. 1999, 42: 2482-2488. 10.1002/1529-0131(199911)42:11<2482::AID-ANR27>3.0.CO;2-B.
Fischer AA: Pressure tolerance over muscles and bones in normal subjects. Arch Phys Med Rehabil. 1986, 67: 406-409.
Burckhardt CS, Clark SR, Bennett RM: The Fibromyalgia Impact Questionnaire: development and validation. J Rheumatol. 1991, 18: 728-734.
First MB, Spitzer RL, Williams JBW, Gibbon M: Structured Clinical Interview for DSM-IV-Patient Edition (SCID-P). 1995, Washington, DC: American Psychiatric Press
Arora RC, Meltzer HY: A modified assay method for determining serotonin uptake in human platelets. Clin Chim Acta. 1981, 112: 225-233. 10.1016/0009-8981(81)90381-8.
Lowry OH, Rosebrough NJ, Farr AL, Randall RJ: Protein measurement with the Folin phenol reagent. J Biol Chem. 1951, 193: 265-275.
Marazziti D, Rossi A, Gemignani A, Giannaccini G, Pfanner C, Milanfranchi A, Presta S, Lucacchini A, Cassano GB: Deceased platelet [3H]paroxetine binding in obsessive-compulsive patients. Neuropsychobiology. 1996, 34: 184-187.
Stahl SM: The human platelets. A diagnostic and research tool for the study of biogenic amines in psychiatric and neurological disorders. Arch Gen Psychiatry. 1977, 34: 509-516.
Legangneux E, Mora JJ, Spreux-Varoquaux O, Thorin I, Herrou M, Gomeni C: Cerebrospinal fluid biogenic amine metabolites, plasma-rich platelet serotonin and [3H]imipramine reuptake in the primary fibromyalgia syndrome. Rheumatology (Oxford). 2001, 40: 290-296. 10.1093/rheumatology/40.3.290.
Marazziti D, Dell'Osso L, Rossi A, Masala I, Baroni S, Armani A, Giannaccini G, Di Nasso E, Lucacchini A, Cassano GB: Decreased platelet [3H]paroxetine binding sites in suicide attempters. Psychiatry Res. 2001, 103: 125-131. 10.1016/S0165-1781(01)00281-5.
Marazziti D, Dell'Osso L, Presta S, Pfanner C, Rossi A, Masala I, Baroni S, Giannaccini G, Lucacchini A, Cassano GB: Platelet [3H]paroxetine binding in patients with OCD-related disorders. Psychiatry Res. 1999, 89: 223-228. 10.1016/S0165-1781(99)00102-X.
Wolfe F, Russel IJ, Vipraio G, Ross K, Anderson J: Serotonin level, pain threshold, and fibromyalgia symptoms in the general population. J Rheumatol. 1997, 24: 555-559.
Ernberg M, Voog U, Alstergren P, Lundemberg T, Kopp S: Plasma and serum serotonin levels and their relationship to orofacial pain and anxiety in fibromyalgia. J Orofac Pain. 2000, 14: 37-46.
Yunus MB, Khan MA, Rawlings KK, Green JR, Olson JM, Shah S: Genetic linkage analysis of multicase families with fibromyalgia syndrome. J Rheumatol. 1999, 26: 408-412.
Yamamoto S, Ouchi Y, Onoe H, Yoshikawa E, Tsukada H, Takahashi H, Iwase M, Yamaguti K, Kuratsune H, Watanabe Y: Reduction of serotonin transporters of patients with chronic fatigue syndrome. Neuroreport. 2004, 15: 2571-2574. 10.1097/00001756-200412030-00002.
Kim HJ, Camilleri M, Carlson PJ, Cremonini F, Ferber I, Stephens D, McKinzie S, Zinsmeister AR, Urrutia R: Association of distinct α2 adrenoceptor and serotonin transporter polymorphisms with constipation and somatic symptoms in functional gastrointestinal disorders. Gut. 2004, 53: 829-837. 10.1136/gut.2003.030882.
Lenzinger E, Neumeister A, Praschak-Rieder N, Fuchs K, Gerhard E, Willeit M, Sieghart W, Kasper SF, Hornik K, Aschauer HN: Behavioral effects of tryptofan depletation in seasonal affective disorder associated with the serotonin transporter gene. Psychiatry Res. 1999, 22: 241-246. 10.1016/S0165-1781(99)00009-8.
Ernberg M, Lundeberg T, Kopp S: Effects on muscle pain by intramuscular injection of granisetron in patients with fibromyalgia. Pain. 2003, 101: 275-282. 10.1016/S0304-3959(02)00334-2.
Russell IJ, Michalek JE, Vipraio GA, Fletcher EM, Javors MA, Bowden CA: Platelet [3H]imipramine uptake receptor density and serum serotonin levels in patients with fibromyalgia/fibrositis syndrome. J Rheumatol. 1992, 19: 104-109.
Kravitz HM, Katz R, Kot E, Helmke N, Fawcett J: Biochemical clues to a fibromyalgia-depression link: imipramine binding in patients with fibromyalgia or depression and healthy controls. J Rheumatol. 1992, 19: 1428-1432.
Magni G, Andreoli F, Arduino C, Arise D, Ceccherelli F, Ambrosio F, Eandi M: [3H]Imipramine binding sites are decreased in platelets of chronic pain patients. Clin Neuropharmacol. 1987, 10: 175-177.
Mellerup ET, Plenge P, Engelstoft M: High affinity binding of [3H]paroxetine and [3H]imipramine to human platelet membranes. Eur J Pharmacol. 1983, 96: 303-309. 10.1016/0014-2999(83)90321-7.
Owens MJ, Nemeroff CB: Role of the serotonin in the pathophysiology of depression: focus on the serotonin transporter. Clin Chem. 1994, 40: 288-295.
Gursoy S: Absence of association of the serotonin transporter gene polymorphism with the mentally healthy subset of fibromyalgia patients. Clin Rheumatol. 2002, 21: 194-197. 10.1007/s10067-002-8284-5.
Almay BG, Maggendal J, Von KL, Oreland L: 5-HIAA and HVA in CSF in patients with idiopatic pain disorders. Biol Psychiatry. 1987, 22: 403-412. 10.1016/0006-3223(87)90162-4.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
L Bazzichi was responsible for the design of the study and patient recruitment. GG was responsible for the design of the study and was the supervisor of the laboratory analysis. LB drafted the manuscript and was the coordinator of the laboratory activity. GM performed the statistical analysis. LF and PI conducted the binding assays. FDF and TG were responsible for the uptake assays. CG drafted the manuscript and performed the statistical analysis. AR was responsible for the preparation of the samples and for their storage. AL and SB were general supervisors of the research group. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Bazzichi, L., Giannaccini, G., Betti, L. et al. Alteration of serotonin transporter density and activity in fibromyalgia. Arthritis Res Ther 8, R99 (2006). https://doi.org/10.1186/ar1982
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1186/ar1982