Abstract
Introduction
Alzheimer’s disease (AD) is characterized by the deposition of tau and amyloid in the brain. Although the core cerebrospinal fluid (CSF) AD biomarkers amyloid β peptide 1–42 (Aβ1–42), total tau (t-tau) and phosphorylated tau 181 (p-tau181) show good diagnostic sensitivity and specificity, additional biomarkers that can aid in preclinical diagnosis or better track disease progression are needed. Activation of the complement system, a pivotal part of inflammation, occurs at very early stages in the AD brain. Therefore, CSF levels of complement proteins that could be linked to cognitive and structural changes in AD may have diagnostic and prognostic value.
Methods
Using xMAP® technology based assays we measured complement 3 (C3) and factor H (FH) in the CSF of 110 controls (CN), 187 mild cognitive impairment (MCI) and 92 AD subjects of the AD Neuroimaging Initiative (ADNI) at baseline. All ADNI participants underwent clinical follow-up at 12 month intervals and MCI subjects had additional visits at 6 and 18 months. The association between CSF biomarkers and different outcome measures were analyzed using Cox proportional hazard models (conversion from MCI to AD), logistic regression models (classification of clinical groups) and mixed-effects models adjusted for age, gender, education, t-tau/Aβ1–42 and APOE ϵ4 presence (baseline and longitudinal association between biomarkers and cognitive scores).
Results
Although no association was found between the complement proteins and clinical diagnosis or cognitive measures, lower levels of C3 (β = −0.12, p = 0.041) and FH (β = −0.075, p = 0.041) were associated with faster cognitive decline in MCI subjects as measured by the AD Assessment Scale-cognitive subscale (ADAS-Cog) test. Furthermore, lower FH levels were associated with larger lateral ventricular volume (p = 0.024), which is indicative of brain atrophy.
Conclusions
Our study confirms a lack of suitability of CSF C3 and FH as diagnostic biomarkers of AD, but points to their modest potential as prognostic biomarkers and therapeutic targets in cognitively impaired patients.
Similar content being viewed by others
Introduction
Alzheimer’s disease (AD) affects an estimated 34 million people worldwide, a number that is predicted to triple by 2050 due to the aging population [1]. Despite intensive research and the identification of several promising drug candidates in preclinical studies, a neuroprotective treatment remains a major unmet need. Possible reasons for the failure of disease-modifying drug clinical trials include our inability to diagnose AD before substantial neuronal damage has occurred, as well as track disease progression and treatment response [2]. In this regard, sensitive and specific biomarkers are urgently needed.
The cerebrospinal fluid (CSF) biomarkers amyloid β peptide 1–42 (Aβ1–42), which correlates inversely with plaque pathology, total tau (t-tau), which is hypothesized to reflect neuroaxonal degeneration, and phosphorylated tau (p-tau181), which may correlate with tangle pathology, have recently been incorporated into the National Institute on Aging guidelines for AD diagnosis [3]. With regard to temporal dynamics, the decrease in CSF Aβ1–42 seems to be an early event, reaching a plateau before the onset of dementia and remaining relatively unchanged thereafter. The increase in CSF tau occurs after Aβ1–42 changes, but still in the preclinical stage of the disease and does not change appreciably over time in cognitively impaired subjects [4, 5]. Therefore, although these core biomarkers show good sensitivity and specificity for the diagnosis of AD, additional biomarkers that can aid in the early diagnosis of dementia or can better track disease progression will improve the design and interpretation of clinical trials.
Neuroinflammation is generally recognized to be a major component of AD [6]. However, whether it is a cause, a contributing factor, or merely a consequence of neurodegeneration is unclear. Clinical and experimental evidence supports the involvement of inflammatory changes in the early stages of AD before the appearance of amyloid plaques [7], as well as in the progression of neurodegeneration [8]. If this is indeed the case, biomarkers that reflect the inflammatory process in AD hold promise for both early diagnosis and tracking of disease progression.
The complement system is a pivotal part of the immune system and inflammatory processes. Depending on the trigger, complement can be activated via the classical, alternative, or lectin pathways. All three pathways culminate in the formation of complement convertases, which results in the proteolytic cleavage of complement 3 (C3) and, later in the cascade, complement 5. The resulting active fragments act as proinflammatory and chemotactic anaphylatoxins, opsonins allowing phagocytosis, or anchors for the assembly of the membrane attack complex. The complement system is kept under tight control by soluble and membrane-bound regulators, including factor H (FH), which inhibits C3 convertases in the alternative pathway, and complement 1 inhibitor, which inhibits several proteases of the classical and lectin pathways [9]. The final outcome therefore depends on the balance between complement activation and inhibition, and dysregulation of this balance may contribute to neuroinflammation and disease [10]. As expected, complement activation has been shown to occur in the AD brain [9], even at very early stages of the disease [11]. Furthermore, genome-wide association studies have identified AD-associated variants at the complement receptor 1 gene [12, 13], which correlate with a greater Aβ plaque burden and age-related cognitive decline [14]. Polymorphisms in the FH gene have also been linked to susceptibility to AD [15], although there are conflicting reports [16].
In a previous cross-sectional study, we found that CSF levels of C3 and FH were significantly increased in AD patients compared with controls (CN) and that the increase correlated significantly with lower Mini-Mental State Examination (MMSE) scores in AD patients. In the current study, we attempt to validate these observations in a large, independent cohort of well-characterized subjects. In addition, we extend the previous analysis by including patients diagnosed with mild cognitive impairment (MCI) and by analyzing additional clinical and neuroimaging data. Finally, we explore the prognostic potential of CSF C3 and FH levels by analyzing longitudinally collected clinical data.
Methods
Subjects
Data used in the current study were downloaded on 27 July 2013 from the Alzheimer’s Disease Neuroimaging Initiative (ADNI) database [17]. Ethics approval was obtained for each institution involved (see Acknowledgements and Additional file 1). The ADNI is conducted according to Good Clinical Practice guidelines, the Declaration of Helsinki, US 21CFR Part 50 – Protection of Human Subjects and Part 56 – Institutional Review Boards, and pursuant to state and federal Health Insurance Portability and Accountability Act regulations. Written informed consent is obtained from all subjects and/or authorized representatives and study partners before protocol-specific procedures are carried out. Institutional review boards were constituted according to applicable State and Federal requirements for each participating location. The protocols were submitted to the appropriate boards and their written unconditional approval obtained and submitted to Regulatory Affairs at the ADNI Coordinating Center prior to commencement of the study. The ADNI Coordinating Center supplied relevant data for investigators to submit to their hospital/university/independent institutional review boards for protocol review and approval. Verification of institutional review board unconditional approval of the protocol and the written informed consent statement with written information to be given to the participants and/or their authorized representatives and the study partners were transmitted and validated by the ADNI Coordinating Center in order to obtain approval for shipment of study supplies to study sites. The ADNI has previously been described extensively [18]. Criteria for the different diagnostic groups can be found in the ADNI procedures manual [19] (see also Additional file 2). In the current study, 389 ADNI 1 [20] subjects (110 CN, 187 MCI subjects and 92 AD subjects) had C3, FH, Aβ1–42, t-tau and p-tau181 measured in their CSF samples at baseline.
Clinical assessment and cognitive profile
The same neuropsychological testing battery was applied to all subjects in the ADNI, with visits scheduled every 12 months, except for the MCI subjects who had additional visits at 6 and 18 months. Tests included the MMSE, the Alzheimer’s Disease Assessment Scale – cognitive subscale (ADAS-Cog), the clock drawing test, the Rey Auditory Verbal Learning Test, Digit Span forward and backward, category fluency, the trail-making test, the digit symbol substitution test, the Boston naming test and the logical memory test. Finally, we further characterized the cognitive profile of each subject using the summary composite executive function and memory measures developed by Gibbons and colleagues [21] and Crane and colleagues [22]. These measures summarize into a score factors from different tests that belong to the same cognitive domain, giving each test a specific loading and accounting for the difficulty of the different variations of the tests; for example, the different word lists available for the Rey Auditory Verbal Learning Test.
Cerebrospinal fluid sample collection and analysis
CSF samples were obtained in the morning after an overnight fast at ADNI baseline visits. Lumbar puncture was performed with a 20-gauge or 24-gauge spinal needle as described previously [23] (for more details including sample handling and storage, see Additional file 2).
CSF C3 and FH levels were measured using an xMAP technology-based multiplex human neurodegenerative kit (HNDG1-36 K; Millipore, Billercia, MA, USA) according to the manufacturer’s overnight protocol with minor modifications. A detailed protocol can be found on the ADNI website [17]. Aβ1–42, t-tau and p-tau181 were measured using the multiplex xMAP Luminex platform (Luminex Corp, Austin, TX, USA) with an Innogenetics kit (INNO-BIA AlzBio3; Innogenetics, Ghent, Belgium) according to the manufacturer’s protocol [24]. CSF hemoglobin was measured using an ELISA kit from Bethyl Lab Inc. (Montgomery, TX, USA) according to the manufacturer’s instructions. Rules-based medicine (RBM; Austin, TX, USA) evaluated CSF samples using a multiplex Human DiscoveryMAP™ panel consisting of 159 analytes (including C3) on a Luminex 100 platform (Luminex Corp, Austin, TX, USA). More details on the methods used in the ADNI CSF Proteome study can be found on the ADNI website [25]. For details regarding each assay’s performance, see Additional file 2.
Magnetic resonance imaging acquisition and processing
Acquisition of 1.5-T magnetic resonance imaging (MRI) data for the ADNI 1 subjects followed a previously described standardized protocol that included sagittal volumetric three-dimensional magnetization prepared rapid acquisition gradient recalled echo (MPRAGE), with variable resolution around the target of 1.2 mm isotropically. The scans had gone through certain correction methods such as gradwarp, B1 calibration, N3 correction and (in-house) skull-stripping (for details see [17, 26]). The images were processed with a freely available pipeline [27] (for software see [28]). Briefly, images were segmented into three tissue types: grey matter, white matter and CSF. After high-dimensional image warping to an atlas, regional volumetric maps for grey matter, white matter and CSF were created – referred to herein as regional volumetric analysis of brain images, which are used for voxel-based analysis and group comparisons of regional tissue atrophy, as well as for constructing an index of AD brain morphology. We tested for differences in ventricular volume in our primary analysis and for associations with the different regions of interest in a secondary analysis.
Statistical analysis
For the analyses included in the descriptive table (Table 1), one-way analyses of variance were used for quantitatively normally distributed variables and the data are presented as the mean (standard deviation). Kruskall–Wallis tests were used for quantitative non-normally distributed variables and the data are presented as the median (first quartile to third quartile). Chi-square tests were applied for qualitative variables and the data are presented as the percentage of counts. For further analyses, distributions of the variables and residuals were tested and power transformations applied if necessary. C3, FH and the C3/FH ratio were standardized to compare effect sizes across analytes.
Previous studies suggest that blood contamination of CSF can significantly affect CSF concentrations of certain proteins [29]. We therefore first tested whether hemoglobin levels were associated with complement biomarker levels in CSF, using a model that included gender, age, apolipoprotein E epsilon 4 allele presence (APOE ϵ4) and clinical diagnosis as covariates. CSF levels of FH (Figure S1a in Additional file 3) but not of C3 were significantly associated with hemoglobin. This association disappeared after exclusion of samples with hemoglobin levels > 1,500 ng/ml (14 CN, 24 MCI subjects, nine AD subjects) (Figure S1b in Additional file 3). All further analyses were therefore performed on the remaining 342 subjects. Exclusion of the 47 subjects with high hemoglobin levels did not significantly change the difference between diagnostic groups for any of the variables reported in Table 1.
Associations between CSF complement biomarkers and age, gender and APOE ϵ4 presence were tested in linear regression models. FH and C3, but not C3/FH, were associated with both age and gender. None of the CSF complement biomarkers showed a significant association with APOE ϵ4 presence (Table S1 in Additional file 4).
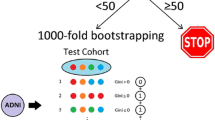
To test the classification accuracy of the analytes, we split the sample into a discovery set (67%) and a validation set (33%), stratifying by clinical diagnosis. To train a classifier and cross-validate the cutoff values in the discovery set, the subjects were further randomly split 10 times to form training (67%) versus test (33%) sets. The cutoff values of the model were selected in the discovery set using accuracy and the kappa index as performance metrics [30, 31]. The obtained logistic regression model was then applied to the validation set and the sensitivity, specificity and the area under the curve of the receiver operating characteristic curve were obtained [32].
A Cox hazards model, with age, gender, t-tau/Aβ1–42 ratio, APOE ϵ4 presence and education as covariates was used to study the conversion of MCI to AD for different CSF biomarkers. Standardized values (mean = 0, standard deviation = 1) were used for the biomarker values in order to compare the effect size of the association.
We analyzed the cross-sectional and longitudinal association between CSF biomarkers and different outcome measures using mixed-effects models [33, 34]. A mixed-effects model is an extension of a linear regression model that allows calculation of the mean trajectory of biomarker values for each group as well as the estimation of each patient’s trajectory. The mixed-effects model takes into account within-subject correlations from repeated measurements of biomarker values in the same subjects and for missing data points. Age, gender, education, APOE ϵ4 presence, t-tau/Aβ1–42 ratio and clinical diagnosis at baseline were included as fixed effects. We include an intercept, follow-up time and squared follow-up time in weeks as random effects. Our model specified the intercept and the regression coefficient for the follow-up time as random effects such that subjects have a unique intercept and slope characterizing their individual trajectories. An interaction between time and clinical diagnosis, between time and t-tau/Aβ1–42 ratio, and between time and the studied CSF biomarker was also included to assess whether these biomarkers were associated with the longitudinal change. A significant interaction between clinical diagnosis and time, for example, would indicate that the slope of change during follow-up is different in CN and MCI subjects. To plot the data we calculated the 25th, 50th and 75th percentile biomarker values for the MCI group and estimated the predicted changes based on the coefficients of the corresponding mixed-effects model (for the variables included in the model, median and mode values were used for quantitative and categorical predictors).
For the MRI analysis, a mixed-effects model was used, with a nested term inside subjects for the left and right sides for each region of interest. Age, gender and t-tau/Aβ1–42 ratio, clinical diagnosis and intracranial volume were included as fixed effects.
Statistical tests were two-sided and significance was set at P < 0.05. In the case of multiple comparisons, the Benjamini–Hochberg correction and the Holms method was applied when a large and lower number of comparisons, respectively, had been performed. Analyses were performed using R v. 3.0.1 [35].
Results
A total of 389 ADNI 1 participants with CSF C3, FH, Aβ1–42, t-tau and p-tau181 as well as MRI data were included in the current study. Clinical and demographic characteristics of the studied subjects are summarized in Table 1. As expected, the clinical groups differed in gender, MMSE, ADAS-Cog, APOE ϵ4 presence and CSF Aβ1–42, t-tau and p-tau181. The data for CSF Aβ1–42, t-tau and p-tau181 in the AD subjects are in line with published cutoff values from autopsy confirmed cases using the AlzBio3 kit [23]. However, no differences in CSF C3 or FH levels or the C3/FH ratio were noted between the diagnostic groups. As discussed earlier, all subsequent analysis were performed on the 342 subjects whose CSF samples had hemoglobin levels ≤ 1,500 ng/ml. Exclusion of subjects with hemoglobin levels > 1,500 ng/ml (14 CN, 24 MCI subjects, nine AD subjects) did not seem to result in any selection bias (Table 1).
Cross-sectional analysis
In linear regression analysis, a strong, positive correlation between C3 and FH (rpartial = 0.81, P < 0.0001) was present after adjusting for age and gender (Figure S2 in Additional file 3). In age, gender and APOE ϵ4 presence adjusted models, FH was significantly associated with t-tau but not with p-tau181 or Aβ1–42. C3 was not associated with Aβ1–42, t-tau or p-tau181 (Table S2 in Additional file 4).
Linear regression models adjusted for age, gender and APOE ϵ4 presence revealed no association of C3, FH or C3/FH with clinical diagnosis (Table S3 in Additional file 4). A lack of contribution from C3 and FH in classifying different clinical groups was further confirmed by the fact that the addition of C3, FH or C3/FH did not improve the performance of t-tau/Aβ1–42 in classifying AD subjects versus CN or MCI subjects versus CN (Table 2). The diagnostic utility of C3 and or FH was therefore not evaluated further.
Finally, with regard to disease severity C3, FH and C3/FH did not associate with baseline ADAS-cog, MMSE, memory summary or executive function summary scores of AD (Table 3) or MCI (Table 4) subjects in mixed-effects models adjusted for age, gender, education, APOE ϵ4 presence and t-tau/Aβ1–42 ratio.
Longitudinal analysis
Of the 160 MCI subjects included in the analysis, 79 converted to AD with a median follow-up time of 158 weeks. A Cox hazards model with age at baseline (hazard ratio = 1.01, P = 0.59), gender (hazard ratio = 1.05, P = 0.84), t-tau/Aβ1–42 ratio (hazard ratio = 1.49, P = 0.002), APOE ϵ4 presence (hazard ratio = 1.13, P = 0.63) and education (hazard ratio = 1.02, P = 0.70) as covariates was used to test the association of the CSF complement biomarkers with conversion of MCI to AD. A weak association between lower levels of C3 (hazard ratio = 0.62, Punadj = 0.046) and increased conversion was lost after adjustment for multiple comparisons (Padj = 0.14).
Longitudinal ADAS-Cog, MMSE, memory summary and executive function summary scores were next analyzed against baseline CSF C3 and FH levels. Follow-up of ADNI 1 patients with a baseline diagnosis of AD was discontinued at an earlier time point than baseline MCI patients (mean follow-up was 98.3 weeks for the AD group and 184 weeks for the MCI group). Owing to this imbalance in the number of visits, we analyzed the AD subjects and the MCI subjects separately. All of the following analyses were adjusted for age, gender, APOE ϵ4 presence, education and t-tau/Aβ1–42 ratio. In the analysis of the AD group, none of the complement biomarkers were associated with changes in ADAS-Cog, MMSE, memory summary, or executive function summary scores during follow-up (Table 3). In the MCI subjects, lower levels of both C3 and FH were associated with an increase (more severe cognitive impairment) in ADAS-Cog scores during follow-up (biomarker × time interaction, Table 4; Figure 1a,b). The C3/FH ratio showed no association with longitudinal ADAS-Cog score changes. Finally, none of the CSF complement biomarkers showed a significant association with MMSE, memory summary, or executive function summary scores, although there was a trend for an association of lower C3 levels with a decline in memory summary score during follow-up (biomarker × time interaction, Table 4; Figure 1c,d,e,f).
Association of cerebrospinal fluid complement 3 and factor H levels with longitudinal cognitive changes in mild cognitive impairment subjects. (a), (b) Alzheimer’s disease Assessment Scale – cognitive subscale (ADAS-Cog), (c), (d) summary memory scores and (e), (f) summary executive function scores are represented on the y axis, with follow-up time on the x axis. Although the variables examined here were treated as quantitative in the analysis, the graphs represent the different tertiles for ease of visual representation. C3, complement 3; FH, factor H.
Correlations of complement 3 and factor H with other ADNI variables
A subset (n = 256) of the ADNI 1 subjects included in the study also had RBM CSF data available. The RMB CSF panel included C3, but not FH. We explored the association between our CSF C3 measurements and the RBM C3 levels and found a strong correlation between the two (r = 0.79, P < 0.0001), indicating that the two immunoassays performed similarly. As expected, when we repeated the diagnostic and prognostic analyses described above using C3 levels obtained by the RBM assay, very similar, if not identical, results were found, especially with regard to the association between lower levels of C3 and faster cognitive decline of MCI subjects.
Since brain atrophy detected by MRI is associated with AD severity and correlates closely with changes in cognitive performance [36], we also studied the association between the CSF complement biomarkers and MRI volumes at baseline in a model adjusted for age, gender, clinical diagnosis, t-tau/Aβ1–42 ratio and intracranial volume. There were no associations between C3 levels or the C3/FH ratio and MRI volumes. However, although no association with CSF FH levels was noted when different region of interest were analyzed independently (Table S4 in Additional file 4), low FH values were clearly associated with increased lateral ventricular volume in the multiple comparison-adjusted analyses (Padj = 0.024), consistent with the argument that low CSF FH level is associated with greater brain atrophy.
Discussion
In this study, we explored the diagnostic and prognostic value of CSF C3 and FH levels in AD and MCI. In cross-sectional analysis, there were no significant differences in either biomarker or in their ratio between diagnostic groups, and nor were there any correlations with disease severity in AD or MCI subjects as measured by the MMSE, ADAS-Cog, memory summary score or executive function summary score. In the longitudinal analysis of MCI patients, however, low levels of both C3 and FH were modestly associated with an increase in ADAS-Cog scores (more severe cognitive impairment) and validation in an independent and longitudinal cohort is needed. Additionally, there was a significant association of low CSF FH levels with increased lateral ventricular volume, which is indicative of brain atrophy and has been shown to correlate strongly with changes in cognitive tests [37]. Strengths of the current study include the use of a large cohort of subjects that underwent detailed clinical and neuropsychological testing and longitudinal follow-up, the availability of APOE ϵ4 genotype data, hemoglobin measurements to control for blood contamination of CSF, as well as the use of RBM CSF C3 data to corroborate our own measurements and results.
Previous studies have generally reported elevated levels of complement components in AD CSF, although results are inconsistent. For example, in a recent study [38] using a commercially available ELISA kit, CSF C3 levels were increased in AD patients and CN subjects compared with stable MCI subjects, but there was no significant difference between AD patients and CN subjects, or between the MCI-to-AD group and any of the other groups. Consistent with the current finding, receiver operating characteristic analysis revealed no diagnostic utility for CSF C3. On the other hand, in a study using the RBM Human DiscoveryMAP™ panel on a Luminex 100 platform, CSF C3 levels were increased in autopsy-confirmed AD cases compared with normal controls. Furthermore, there was a significant correlation between CSF C3 levels and MMSE scores in AD subjects, but not in MCI subjects [39]. In contrast, a study using two-dimensional electrophoresis found no significant difference in the average percent volume for C3b or FH in CSF samples from AD compared with normal controls [40]. In line with the RBM study discussed above, our own earlier study found increased CSF C3 and FH levels in AD patients compared with CN subjects, as well as significant negative correlations between the two complement biomarkers and MMSE scores [41]. The failure to validate our own earlier findings in the current study may be related to differences between the two cohorts, including highly selected subjects in the ADNI versus the community-based cohort in our previous study, gender distribution and mean age, as well as the number of AD patients included in the analysis (38 in the previous study vs. 83 in the current study). One should also point out that although our original study found significant differences in CSF C3 and FH levels between diagnostic groups, receiver operating characteristic analysis showed that neither biomarker had acceptable sensitivity or specificity (>60%) for classifying CN versus AD subjects. In summary, we conclude that these studies are in agreement regarding a lack of suitability of CSF C3 and FH as diagnostic biomarkers of AD.
A limitation of our investigation is the potential confounding effect of pharmacotherapy, because subjects were not drug naïve at the time of CSF collection, although the use of many central nervous system-active drugs such as antidepressants or neuroleptics with anti-cholinergic properties, narcotic analgesics and anti-Parkinsonian medications were excluded. The other limitation relates to the fact that the data are correlational without clear mechanistic interpretation. That said, we wish to put forward two hypotheses for discussion. First, our finding of low levels of CSF C3 and FH in MCI patients with accelerated cognitive decline may reflect increased deposition of these complement biomarkers in senile plaques. Decreased Aβ1–42 in AD CSF is hypothesized to be the result of trapping the peptide in plaques, and C3 and FH have both been shown to be present in Aβ plaques [11, 42, 43]. Trapping of C3 and FH in plaques may therefore lead to a decrease in the CSF levels of these proteins. However, we did not find a correlation between CSF Aβ1–42 and C3 or FH, suggesting that the observed decrease in complement biomarkers cannot be readily explained by such a simplistic model. An alternative hypothesis could therefore be that the low CSF levels of C3 and FH in faster progressors may reflect accelerated dysregulation of the complement system in the brain. To this end, many studies have indicated potential involvement of complement system in AD pathogenesis, including observations that: Aβ fibrils activate both the classical and alternative complement pathways in vitro[44–46]; inhibition of C3 in a mouse model of AD resulted in accelerated and increased Aβ plaque deposition, as well as neurodegeneration [47–49]; and AD mice lacking C1q (part of the complex triggering activation of the classical pathway) had decreased levels of activated glia in proximity to plaques, as well as reduced neuronal injury [50] consistent with a detrimental role for complement activation in this model. Indeed, based on these and other studies, a hypothesis has been suggested that classical complement activation is detrimental in neurodegeneration, whereas alternative complement activation is beneficial up to a certain threshold or depending on the complement receptor CR1 genotype [51]. Thus, if CSF levels of C3 and FH mirror their levels in the brain, our finding of a decreased total C3 level may indicate increased cleavage of C3 to generate more of its active fragments at the expense of the holoprotein. This increased activation of C3 might be due to increased activation of the classical, lectin and/or alternative pathways, as C3 is a joining point for all three. Decreased levels of FH will also lead to increased cleavage of C3 via the alternative pathway, because FH regulates this pathway at the C3 convertase level [9]. The strong correlation observed between CSF C3 and FH in the current study supports this hypothesis. The negative finding with regard to the longitudinal analysis in AD patients could be secondary to the much shorter followup in these patients and a smaller sample size, which results in less statistical power.
Conclusions
In summary, our data suggest that CSF C3 and FH levels are prognostic biomarkers of accelerated cognitive decline in MCI, although validation in an independent cohort is needed. Additionally, studies with repeated CSF measurements will shed more light on the utility of CSF C3 and FH levels as AD progression biomarkers. Finally, results obtained in this study should encourage further investigations exploring the mechanisms underlying complement activation, both the classical and alternative cascades, in AD development and progression.
Abbreviations
- Aβ1–42:
-
amyloid β peptide 1–42
- AD:
-
Alzheimer’s disease
- ADAS-Cog:
-
Alzheimer’s Disease Assessment Scale – cognitive subscale
- ADNI:
-
Alzheimer’s Disease Neuroimaging Initiative
- APOE ϵ4:
-
apolipoprotein E epsilon 4 allele
- C3:
-
complement 3
- CN:
-
controls
- CSF:
-
cerebrospinal fluid
- FH:
-
factor H
- MCI:
-
mild cognitive impairment
- MMSE:
-
Mini-Mental State Examination
- MRI:
-
magnetic resonance imaging
- p-tau181:
-
tau phosphorylated at threonine 181
- RBM:
-
rules-based medicine
- t-tau:
-
total tau.
References
Barnes DE, Yaffe K: The projected effect of risk factor reduction on Alzheimer’s disease prevalence. Lancet Neurol. 2011, 10: 819-828. 10.1016/S1474-4422(11)70072-2.
Dunkel P, Chai CL, Sperlagh B, Huleatt PB, Matyus P: Clinical utility of neuroprotective agents in neurodegenerative diseases: current status of drug development for Alzheimer’s, Parkinson’s and Huntington’s diseases, and amyotrophic lateral sclerosis. Expert Opin Investig Drugs. 2012, 21: 1267-1308. 10.1517/13543784.2012.703178.
Jack CR, Albert MS, Knopman DS, McKhann GM, Sperling RA, Carrillo MC, Thies B, Phelps CH: Introduction to the recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011, 7: 257-262. 10.1016/j.jalz.2011.03.004.
Jack CR, Knopman DS, Jagust WJ, Petersen RC, Weiner MW, Aisen PS, Shaw LM, Vemuri P, Wiste HJ, Weigand SD, Lesnick TG, Pankratz VS, Donohue MC, Trojanowski JQ: Tracking pathophysiological processes in Alzheimer’s disease: an updated hypothetical model of dynamic biomarkers. Lancet Neurol. 2013, 12: 207-216. 10.1016/S1474-4422(12)70291-0.
Toledo JB, Xie SX, Trojanowski JQ, Shaw LM: Longitudinal change in CSF Tau and Aβ biomarkers for up to 48 months in ADNI. Acta Neuropathol. 2013, 126: 659-670. 10.1007/s00401-013-1151-4.
McGeer EG, McGeer PL: Neuroinflammation in Alzheimer’s disease and mild cognitive impairment: a field in its infancy. J Alzheimers Dis. 2010, 19: 355-361.
Ferretti MT, Cuello AC: Does a pro-inflammatory process precede Alzheimer’s disease and mild cognitive impairment?. Curr Alzheimer Res. 2011, 8: 164-174. 10.2174/156720511795255982.
Gao HM, Hong JS: Why neurodegenerative diseases are progressive: uncontrolled inflammation drives disease progression. Trends Immunol. 2008, 29: 357-365. 10.1016/j.it.2008.05.002.
Veerhuis R, Nielsen HM, Tenner AJ: Complement in the brain. Mol Immunol. 2011, 48: 1592-1603. 10.1016/j.molimm.2011.04.003.
Sjoberg AP, Trouw LA, Blom AM: Complement activation and inhibition: a delicate balance. Trends Immunol. 2009, 30: 83-90. 10.1016/j.it.2008.11.003.
Zanjani H, Finch CE, Kemper C, Atkinson J, McKeel D, Morris JC, Price JL: Complement activation in very early Alzheimer disease. Alzheimer Dis Assoc Disord. 2005, 19: 55-66. 10.1097/01.wad.0000165506.60370.94.
Lambert JC, Heath S, Even G, Campion D, Sleegers K, Hiltunen M, Combarros O, Zelenika D, Bullido MJ, Tavernier B, Letenneur L, Bettens K, Berr C, Pasquier F, Fiévet N, Barberger-Gateau P, Engelborghs S, De Deyn P, Mateo I, Franck A, Helisalmi S, Porcellini E, Hanon O, de Pancorbo MM, Lendon C, Dufouil C, Jaillard C, Leveillard T, Alvarez V, European Alzheimer's Disease Initiative: Genome-wide association study identifies variants at CLU and CR1 associated with Alzheimer’s disease. Nat Genet. 2009, 41: 1094-1099. 10.1038/ng.439.
Harold D, Abraham R, Hollingworth P, Sims R, Gerrish A, Hamshere ML, Pahwa JS, Moskvina V, Dowzell K, Williams A, Jones N, Thomas C, Stretton A, Morgan AR, Lovestone S, Powell J, Proitsi P, Lupton MK, Brayne C, Rubinsztein DC, Gill M, Lawlor B, Lynch A, Morgan K, Brown KS, Passmore PA, Craig D, McGuinness B, Todd S, Holmes C: Genome-wide association study identifies variants at CLU and PICALM associated with Alzheimer’s disease. Nat Genet. 2009, 41: 1088-1093. 10.1038/ng.440.
Chibnik LB, Shulman JM, Leurgans SE, Schneider JA, Wilson RS, Tran D, Aubin C, Buchman AS, Heward CB, Myers AJ, Hardy JA, Huentelman MJ, Corneveaux JJ, Reiman EM, Evans DA, Bennett DA, De Jager PL: CR1 is associated with amyloid plaque burden and age-related cognitive decline. Ann Neurol. 2011, 69: 560-569. 10.1002/ana.22277.
Zetterberg M, Landgren S, Andersson ME, Palmer MS, Gustafson DR, Skoog I, Minthon L, Thelle DS, Wallin A, Bogdanovic N, Andreasen N, Blennow K, Zetterberg H: Association of complement factor H Y402H gene polymorphism with Alzheimer’s disease. Am J Med Genet B Neuropsychiatr Genet. 2008, 147B: 720-726. 10.1002/ajmg.b.30668.
Le Fur I, Laumet G, Richard F, Fievet N, Berr C, Rouaud O, Delcourt C, Amouyel P, Lambert JC: Association study of the CFH Y402H polymorphism with Alzheimer’s disease. Neurobiol Aging. 2010, 31: 165-166. 10.1016/j.neurobiolaging.2008.03.003.
Alzheimer’s Disease Neuroimaging Initiative.http://adni.loni.usc.edu/,
Weiner MW, Veitch DP, Aisen PS, Beckett LA, Cairns NJ, Green RC, Harvey D, Jack CR, Jagust W, Liu E, Morris JC, Petersen RC, Saykin AJ, Schmidt ME, Shaw L, Siuciak JA, Soares H, Toga AW, Trojanowski JQ, Alzheimer’s Disease Neuroimaging Initiative: The Alzheimer’s Disease Neuroimaging Initiative: a review of papers published since its inception. Alzheimers Dement. 2012, 8: S1-S68. 10.1016/j.jalz.2011.09.172.
ADNI procedures manual.http://www.adni-info.org/Scientists/Pdfs/adniproceduresmanual12.pdf,
Petersen RC, Aisen PS, Beckett LA, Donohue MC, Gamst AC, Harvey DJ, Jack CR, Jagust WJ, Shaw LM, Toga AW, Trojanowski JQ, Weiner MW: Alzheimer’s Disease Neuroimaging Initiative (ADNI): clinical characterization. Neurology. 2010, 74: 201-209. 10.1212/WNL.0b013e3181cb3e25.
Gibbons LE, Carle AC, Mackin RS, Harvey D, Mukherjee S, Insel P, Curtis SM, Mungas D, Crane PK: A composite score for executive functioning, validated in Alzheimer’s Disease Neuroimaging Initiative (ADNI) participants with baseline mild cognitive impairment. Brain Imaging Behav. 2012, 6: 517-527. 10.1007/s11682-012-9176-1.
Crane PK, Carle A, Gibbons LE, Insel P, Mackin RS, Gross A, Jones RN, Mukherjee S, Curtis SM, Harvey D, Weiner M, Mungas D, Alzheimer’s Disease Neuroimaging Initiative: Development and assessment of a composite score for memory in the Alzheimer’s Disease Neuroimaging Initiative (ADNI). Brain Imaging Behav. 2012, 6: 502-516. 10.1007/s11682-012-9186-z.
Shaw LM, Vanderstichele H, Knapik-Czajka M, Clark CM, Aisen PS, Petersen RC, Blennow K, Soares H, Simon A, Lewczuk P, Dean R, Siemers E, Potter W, Lee VM, Trojanowski JQ, Alzheimer's Disease Neuroimaging Initiative: Cerebrospinal fluid biomarker signature in Alzheimer’s disease neuroimaging initiative subjects. Ann Neurol. 2009, 65: 403-413. 10.1002/ana.21610.
Shaw LM, Vanderstichele H, Knapik-Czajka M, Figurski M, Coart E, Blennow K, Soares H, Simon AJ, Lewczuk P, Dean RA, Siemers E, Potter W, Lee VM, Trojanowski JQ, Alzheimer's Disease Neuroimaging Initiative: Qualification of the analytical and clinical performance of CSF biomarker analyses in ADNI. Acta Neuropathol. 2011, 121: 597-609. 10.1007/s00401-011-0808-0.
Biomarkers Consortium Project Use of Targeted Multiplex Proteomic Strategies to Identify Novel Cerebrospinal Fluid (CSF) Biomarkers in Alzheimer’s Disease (AD). [http://adni.loni.usc.edu/wp-content/uploads/2012/01/2011Dec28-Biomarkers-Consortium-Data-Primer-FINAL1.pdf]
Jack CR, Bernstein MA, Fox NC, Thompson P, Alexander G, Harvey D, Borowski B, Britson PJ, L Whitwell J, Ward C, Dale AM, Felmlee JP, Gunter JL, Hill DL, Killiany R, Schuff N, Fox-Bosetti S, Lin C, Studholme C, DeCarli CS, Krueger G, Ward HA, Metzger GJ, Scott KT, Mallozzi R, Blezek D, Levy J, Debbins JP, Fleisher AS, Albert M: The Alzheimer’s Disease Neuroimaging Initiative (ADNI): MRI methods. J Magn Reson Imaging. 2008, 27: 685-691. 10.1002/jmri.21049.
Davatzikos C, Genc A, Xu D, Resnick SM: Voxel-based morphometry using the RAVENS maps: methods and validation using simulated longitudinal atrophy. NeuroImage. 2001, 14: 1361-1369. 10.1006/nimg.2001.0937.
Penn Medicine Department of Radiology. [http://www.rad.upenn.edu/sbia]
Hong Z, Shi M, Chung KA, Quinn JF, Peskind ER, Galasko D, Jankovic J, Zabetian CP, Leverenz JB, Baird G, Montine TJ, Hancock AM, Hwang H, Pan C, Bradner J, Kang UJ, Jensen PH, Zhang J: DJ-1 and alpha-synuclein in human cerebrospinal fluid as biomarkers of Parkinson’s disease. Brain. 2010, 133: 713-726. 10.1093/brain/awq008.
Venables W, Ripley B: Modern Applied Statistics with S. 2002, New York: Springer Verlag
Kuhn M: Building predictive models in R using the caret package. J Stat Softw. 2008, 28:
Robin X, Turck N, Hainard A, Tiberti N, Lisacek F, Sanchez JC, Muller M: pROC: an open-source package for R and S + to analyze and compare ROC curves. BMC Bioinforma. 2011, 12: 77-10.1186/1471-2105-12-77.
Laird NM, Ware JH: Random-effects models for longitudinal data. Biometrics. 1982, 38: 963-974. 10.2307/2529876.
Pinheiro J, Bates D, DebRoy S, Sarkar D: nlme: Linear and Nonlinear Mixed Effects Models. R package version 3.1-117. 2014
R Core Team: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing. Vienna, Austria; 2014. http://www.R-project.org/
Frisoni GB, Fox NC, Jack CR, Scheltens P, Thompson PM: The clinical use of structural MRI in Alzheimer disease. Nat Rev Neurol. 2010, 6: 67-77. 10.1038/nrneurol.2009.215.
Nestor SM, Rupsingh R, Borrie M, Smith M, Accomazzi V, Wells JL, Fogarty J, Bartha R, Alzheimer’s Disease Neuroimaging Initiative: Ventricular enlargement as a possible measure of Alzheimer’s disease progression validated using the Alzheimer’s disease neuroimaging initiative database. Brain. 2008, 131: 2443-2454. 10.1093/brain/awn146.
Daborg J, Andreasson U, Pekna M, Lautner R, Hanse E, Minthon L, Blennow K, Hansson O, Zetterberg H: Cerebrospinal fluid levels of complement proteins C3, C4 and CR1 in Alzheimer’s disease. J Neural Transm. 2012, 119: 789-797. 10.1007/s00702-012-0797-8.
Hu WT, Chen-Plotkin A, Arnold SE, Grossman M, Clark CM, Shaw LM, Pickering E, Kuhn M, Chen Y, McCluskey L, Elman L, Karlawish J, Hurtig HI, Siderowf A, Lee VM, Soares H, Trojanowski JQ: Novel CSF biomarkers for Alzheimer’s disease and mild cognitive impairment. Acta Neuropathol. 2010, 119: 669-678. 10.1007/s00401-010-0667-0.
Finehout EJ, Franck Z, Lee KH: Complement protein isoforms in CSF as possible biomarkers for neurodegenerative disease. Dis Markers. 2005, 21: 93-101. 10.1155/2005/806573.
Wang Y, Hancock AM, Bradner J, Chung KA, Quinn JF, Peskind ER, Galasko D, Jankovic J, Zabetian CP, Kim HM, Leverenz JB, Montine TJ, Ginghina C, Edwards KL, Snapinn KW, Goldstein DS, Shi M, Zhang J: Complement 3 and factor h in human cerebrospinal fluid in Parkinson’s disease, Alzheimer’s disease, and multiple-system atrophy. Am J Pathol. 2011, 178: 1509-1516. 10.1016/j.ajpath.2011.01.006.
Strohmeyer R, Ramirez M, Cole GJ, Mueller K, Rogers J: Association of factor H of the alternative pathway of complement with agrin and complement receptor 3 in the Alzheimer’s disease brain. J Neuroimmunol. 2002, 131: 135-146. 10.1016/S0165-5728(02)00272-2.
Eikelenboom P, Hack CE, Rozemuller JM, Stam FC: Complement activation in amyloid plaques in Alzheimer’s dementia. Virchows Arch B Cell Pathol Incl Mol Pathol. 1989, 56: 259-262.
Rogers J, Cooper NR, Webster S, Schultz J, McGeer PL, Styren SD, Civin WH, Brachova L, Bradt B, Ward P, Lieberburg I: Complement activation by beta-amyloid in Alzheimer disease. Proc Natl Acad Sci U S A. 1992, 89: 10016-10020. 10.1073/pnas.89.21.10016.
Jiang H, Burdick D, Glabe CG, Cotman CW, Tenner AJ: beta-Amyloid activates complement by binding to a specific region of the collagen-like domain of the C1q A chain. J Immunol. 1994, 152: 5050-5059.
Bradt BM, Kolb WP, Cooper NR: Complement-dependent proinflammatory properties of the Alzheimer’s disease beta-peptide. J Exp Med. 1998, 188: 431-438. 10.1084/jem.188.3.431.
Stephan AH, Barres BA, Stevens B: The complement system: an unexpected role in synaptic pruning during development and disease. Annu Rev Neurosci. 2012, 35: 369-389. 10.1146/annurev-neuro-061010-113810.
Wyss-Coray T, Yan F, Lin AH, Lambris JD, Alexander JJ, Quigg RJ, Masliah E: Prominent neurodegeneration and increased plaque formation in complement-inhibited Alzheimer’s mice. Proc Natl Acad Sci U S A. 2002, 99: 10837-10842. 10.1073/pnas.162350199.
Maier M, Peng Y, Jiang L, Seabrook TJ, Carroll MC, Lemere CA: Complement C3 deficiency leads to accelerated amyloid beta plaque deposition and neurodegeneration and modulation of the microglia/macrophage phenotype in amyloid precursor protein transgenic mice. J Neurosci. 2008, 28: 6333-6341. 10.1523/JNEUROSCI.0829-08.2008.
Fonseca MI, Zhou J, Botto M, Tenner AJ: Absence of C1q leads to less neuropathology in transgenic mouse models of Alzheimer’s disease. J Neurosci. 2004, 24: 6457-6465. 10.1523/JNEUROSCI.0901-04.2004.
Zabel MK, Kirsch WM: From development to dysfunction: microglia and the complement cascade in CNS homeostasis. Ageing Res Rev. 2013, 12: 749-756. 10.1016/j.arr.2013.02.001.
Acknowledgements
Data collection and sharing for this project was funded by the ADNI (National Institutes of Health Grant U01 AG024904). The ADNI is funded by the National Institute on Aging, the National Institute of Biomedical Imaging and Bioengineering, and through generous contributions from the following: Alzheimer’s Association; Alzheimer’s Drug Discovery Foundation; BioClinica, Inc.; Biogen Idec Inc.; Bristol-Myers Squibb Company; Eisai Inc.; Elan Pharmaceuticals, Inc.; Eli Lilly and Company; F. Hoffmann-La Roche Ltd and its affiliated company Genentech, Inc.; GE Healthcare; Innogenetics, N.V.; IXICO Ltd; Janssen Alzheimer Immunotherapy Research & Development, LLC.; Johnson & Johnson Pharmaceutical Research & Development LLC.; Medpace, Inc.; Merck & Co., Inc.; Meso Scale Diagnostics, LLC.; NeuroRx Research; Novartis Pharmaceuticals Corporation; Pfizer Inc.; Piramal Imaging; Servier; Synarc Inc.; and Takeda Pharmaceutical Company. The Canadian Institutes of Health Research is providing funds to support ADNI clinical sites in Canada. Private-sector contributions are facilitated by the Foundation for the National Institutes of Health (http://www.fnih.org). The grantee organization is the Northern California Institute for Research and Education, and the study is coordinated by the Alzheimer’s Disease Cooperative Study at the University of California, San Diego. ADNI data are disseminated by the Laboratory for Neuro Imaging at the University of California, Los Angeles. This research was also supported by National Institutes of Health grants P30 AG010129 and K01 AG030514. The authors’ efforts were also supported by the National Institutes of Health (P42 ES004696-5897 and P30 ES007033-6364), the National Institute on Aging (R01 AG033398), the National Institute of Environmental Health Sciences (R01 ES016873 and R01 ES019277) and the National Institute of Neurological Disorders and Stroke (R01 NS057567, P50 NS062684-6221 and U01 NS082137). JQT is the William Maul Measey-Truman G. Schnabel, Jr, Professor of Geriatric Medicine and Gerontology. Ethics approval was obtained from the institutional review boards of each institution involved: Oregon Health and Science University; University of Southern California; University of California--San Diego; University of Michigan; Mayo Clinic, Rochester; Baylor College of Medicine; Columbia University Medical Center; Washington University, St. Louis; University of Alabama – Birmingham; Mount Sinai School of Medicine; Rush University Medical Center; Wien Center; Johns Hopkins University; New York University; Duke University Medical Center; University of Pennsylvania; University of Kentucky; University of Pittsburgh; University of Rochester Medical Center; University of California, Irvine; University of Texas Southwestern Medical School; Emory University; University of Kansas, Medical Center; University of California, Los Angeles; Mayo Clinic, Jacksonville; Indiana University; Yale University School of Medicine; McGill Univ., Montreal-Jewish General Hospital; Sunnybrook Health Sciences, Ontario; U.B.C. Clinic for AD & Related Disorders; Cognitive Neurology – St. Joseph’s, Ontario; Cleveland Clinic Lou Ruvo Center for Brain Health; Northwestern University; Premiere Research Inst (Palm Beach Neurology); Georgetown University Medical Center; Brigham and Women’s Hospital; Stanford University; Banner Sun Health Research Institute; Boston University; Howard University; Case Western Reserve University; University of California, Davis – Sacramento; Neurological Care of CNY; Parkwood Hospital; University of Wisconsin; University of California, Irvine – BIC; Banner Alzheimer’s Institute; Dent Neurologic Institute; Ohio State University; Albany Medical College; Hartford Hospital, Olin Neuropsychiatry Research Center; Dartmouth-Hitchcock Medical Center; Wake Forest University Health Sciences; Rhode Island Hospital; Butler Hospital; UC San Francisco; Medical University South Carolina; St. Joseph’s Health Care Nathan Kline Institute; University of Iowa College of Medicine; Cornell University and University of South Florida: USF Health Byrd Alzheimer’s Institute.
Data used in preparation of this article were obtained from the ADNI database (adni.loni.ucla.edu). As such, the investigators within the ADNI contributed to the design and implementation of the ADNI and/or provided data but did not participate in analysis or writing of this report. A complete listing of ADNI investigators can be found online (http://adni.loni.usc.edu/wp-content/uploads/how_to_apply/ADNI_Acknowledgement_List.pdf).
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
JBT, AK, LMS, JQT and JZ made substantial contributions to the conception and design of the study and were involved in drafting the manuscript and revising it critically for important intellectual content. AK performed the xMAP assays. JBT, AK and JZ had full access to the entire dataset. LMS and JQT contributed to acquisition and storage of the samples. JBT and AK undertook the statistical analyses. All authors read and approved the final manuscript.
Jon B Toledo, Ané Korff contributed equally to this work.
Electronic supplementary material
13195_2014_262_MOESM1_ESM.pdf
Additional file 1: is an acknowledgement list for ADNI publications: ADNI infrastructure and site investigators.(PDF 662 KB)
13195_2014_262_MOESM2_ESM.pdf
Additional file 2: is the supplemental methods, including subjects, recruitment criteria, CSF sample collection and handling, CSF immunoassay performance and references.(PDF 130 KB)
13195_2014_262_MOESM3_ESM.pdf
Additional file 3: is Supplemental Figures S1 and S2 showing associations between CSF FH and hemoglobin, and CSF C3 and FH.(PDF 134 KB)
13195_2014_262_MOESM4_ESM.pdf
Additional file 4: is Supplemental Tables S1 to S4 presenting data showing CSF C3 and FH biomarker associations.(PDF 47 KB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Toledo, J.B., Korff, A., Shaw, L.M. et al. Low levels of cerebrospinal fluid complement 3 and factor H predict faster cognitive decline in mild cognitive impairment. Alz Res Therapy 6, 36 (2014). https://doi.org/10.1186/alzrt266
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/alzrt266