Abstract
Cerebrospinal fluid and positron emission tomography biomarkers accurately predict an underlying Alzheimer's disease (AD) pathology; however, they represent either invasive or expensive diagnostic tools. Therefore, a blood-based biomarker like plasma amyloid beta (Aβ) that could correlate with the underlying AD pathology and serve as a prognostic biomarker or an AD screening strategy is urgently needed as a cost-effective and non-invasive diagnostic tool. In this paper we review the demographic, biologic, genetic and technical aspects that affect plasma Aβ levels. Findings of cross-sectional and longitudinal studies of plasma Aβ, including autosomal dominant AD cases, sporadic AD cases, Down syndrome cases and population studies, are also discussed. Finally, we review the association between cerebrovascular disease and Aβ plasma levels and the responses observed in clinical trials. Based on our review of the current literature on plasma Aβ, we conclude that further clinical research and assay development are needed before measures of plasma Aβ can be interpreted so they can be applied as trait, risk or state biomarkers for AD.
Similar content being viewed by others
Introduction
Alzheimer's disease (AD) is the most common underlying cause of dementia globally, and the leading cause of years lost to disability in high-income countries as well as the second greatest cause of this worldwide according to the World Health Organization. A definite diagnosis of AD can only be established by postmortem studies that demonstrate the presence of extracellular amyloid plaques and intracellular tau neurofibrillary tangles [1]. The measurement of the neuropathologic hallmarks of AD, namely tau and amyloid beta (Aβ), in cerebrospinal fluid (CSF) has been shown to be a reliable diagnostic biomarker for AD [2], but it would be attractive to have less invasive AD biomarkers, such as those that can be measured in plasma. Positron emission tomography (PET) using florbetapir-F18 (AV-45) or Pittsburgh Compound-B-C11 (PiB) as radiotracers reflects fibrillar brain amyloid deposits and is deemed a reliable method to measure brain amyloid plaque burden [3, 4], but cost and availability of PET biomarker measures are drawbacks associated with this diagnostic strategy. Therefore, the measurement of Aβ in plasma would be the least invasive and most cost-effective biomarker assay. In addition, blood samples could readily be obtained in nonspecialized facilities and sent to specialized laboratories to conduct the measurements. However, published results on the correlation of plasma Aβ with the presence of AD are contradictory and plasma Aβ measurements are subject to more sources of variability than CSF Aβ measurements [5]. Below we will summarize the demographic, biological and technical aspects related to Aβ plasma measures, the results of cross-sectional and longitudinal studies in populations with sporadic AD and AD due to autosomal dominant genetic inheritance, and application of these measurements in clinical trials.
Aβ distribution in blood, CSF and brain
Aβ production and correlation between plasma, CSF and parenchymal Aβ measurements
Aβ is a byproduct of Aβ precursor protein (APP) metabolism that is generated by nearly all cells, and amyloid plaques are the result of the deposition of mainly Aβ1-40 and Aβ1-42 in the brain, although other species of Aβ are also present [6]. The mechanism leading to Aβ deposition differs in subjects for whom this occurs on a genetic basis, leading to familial AD (FAD), versus those who develop sporadic AD. In autosomal dominantly inherited forms of AD, the main mechanism is an increased production of Aβ species [7], while the consensus is that there is a decreased Aβ clearance in sporadic forms of AD, which is modulated by the apolipoprotein E (APOE) genotype [8, 9].
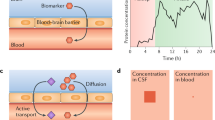
The blood-brain barrier and the blood-CSF barrier regulate the passage of solutes between blood and the central nervous system (CNS), including Aβ. Although there are a number of receptors that are implicated in the influx (for example, receptor of advanced glycation end products) and efflux (for example, low-density lipoprotein receptor, low-density lipoprotein receptor-related protein 1 and 2, P-glycoprotein, low-density and very low-density lipoprotein receptor) of Aβ through the blood-brain barrier, most of the studies that compared plasma Aβ levels with their CSF counterparts [10–13] or the binding of PET Aβ radiotracers [10, 14] have found no or low correlations between Aβ plasma measurements and CSF Aβ and PET amyloid plaque measurements. On the other hand, CSF and PET values show a high inverse correlation [10, 15, 16], although CSF ELISA/Luminex assays measure soluble Aβ and PIB/AV-45 PET measure insoluble fibrillar Aβ deposition. However, one study has described a stronger correlation between plasma Aβ and PET PiB measurements [17].
Origin, distribution and clearance of Aβ in plasma
There are several factors that can explain the low correlation between plasma and CSF Aβ/PET amyloid plaque measurements. First, Aβ species in the CSF and the CNS interstitial fluid originate in the CNS. CNS Aβ is then thought to diffuse from interstitial fluid into the CSF, while passage of Aβ through the blood-brain barrier is limited. In addition, Aβ in plasma and blood does not originate only in the brain since it also is the product of APP metabolism in skeletal muscle, pancreas, kidney, liver, vascular walls, lung, intestine, skin and several glands and APP can be found in almost all peripheral cells [18–20]. In addition, most of the Aβ1-40 and Aβ1-42 in plasma are bound to several proteins (that is, apolipoprotein A-I, A-IV, E and J, α2-macroglobulin, complement factors, immunoglobulins, transthyretin, apoferritin and serum amyloid P component) and erythrocytes[19, 21]. Finally, platelets are another important source of Aβ1-40 and Aβ1-42 in plasma [19] and activated platelets release APP and Aβ [22]. Therefore, it is not surprising that Aβ plasma values may only partially reflect altered APP metabolism or Aβ in the CNS since there is no evidence that AD is a systemic Aβ amyloidosis. While correlations between undiluted, diluted and cell bound plasma samples have been reported by some investigators to be high, the diagnostic utility of measuring Aβ at different dilutions or in different fractions remains uncertain [23]. Finally, regarding the elimination of plasma Aβ, animal models have implicated the liver as the major organ responsible for the clearance of Aβ from plasma [24], followed by renal clearance [25].
Demographic, clinical, genetic and technical issues affecting Aβ levels and measurements
Demographic, genetic diagnostic and assay related factors affecting Aβ plasma levels
Most studies have described a strong association between older age and higher levels of plasma Aβ [10, 26–31]. This association has not been established in Down syndrome (DS) subjects, and there are conflicting results, with some studies finding an association [32, 33] and others not [34, 35]. Two studies have evaluated the heritability of Aβ plasma levels. The paper by Ertekin-Taner et al. found a higher heritability (54% for Aβ1-40 and 73% for Aβ1-42) [36] than the one by Ibrahim-Verbaas et al. (23% for Aβ1-40 and 30% for Aβ1-42) [37]. None of the studies found that APOE genotype explained a significant amount of the heritability, but the study by Ibrahim-Verbaas et al. found an association between SNPs located at the presenilin 2 gene (PSEN2) and Aβ1-40 levels. However, some studies have reported an association of lower Aβ1-42 in the presence of APOE ε4 alleles [10, 28, 38] and at least one study has described a lower Aβ1-42/Aβ1-40 ratio in non-APOE ε4 subjects in the highest tertile of physical activity [39]. A third study found increased Aβ in young, non-demented first-degree relatives of late onset AD compared to unrelated controls [31]. Other factors associated with Aβ plasma levels are creatinine levels [10, 28, 38, 40], high density lipoproteins [27], body mass index [27], race [38] and sex [38, 41]. One study included age, platelet count, total protein concentration and creatinine levels in a multivariate analysis and found that these variables accounted for 12.9% of plasma levels, underscoring the importance of using multivariable models that adjust for possible confounders [10]. Like CSF levels, plasma levels show a circadian fluctuation that decreases with aging [11]. Therefore, standardization of sampling time is important.
Technical aspects regarding sample storage and Aβ plasma measurements
Aβ1-40 and Aβ1-42 are stable at 2 to 8°C for 6 h but when Aβ is kept at room temperature for 24 h levels drop considerably, exceeding a 20% loss in most of the pools [42–45], although ratios of different Aβ species can be more stable [43]. Storage at -20°C is not suitable for long-term storage and Aβ levels are not stable through freeze-thaw cycles following storage at -20°C, whereas storage at-70°C shows no reductions in Aβ levels for up to three cycles and Aβ levels are stable for at least 12 months when stored at this temperature [42, 45]. One study has reported that some Aβ peptides increase their concentration once frozen [46]. Repeated samples taken during fasting and in the post-prandial state and repeated samples taken from cognitively normal (CN) subjects within three weeks show coefficients of variation (CV) that are within the range of the variability of the assay in both cases, indicating that these pre-analytical factors do not have an important effect on Aβ measurements [13]. Although not formally tested in plasma, storage in polypropylene tubes currently is the best way to minimize adherence of Aβ to the wall of storage vials compared to polystyrene for CSF samples [47], and is current practice for plasma samples. Different types of polypropylene are used in the manufacture of biofluid storage vials, but the effects of these differences on Aβ levels following short- and long-term storage are not well documented. Finally, collection parameters like collected blood volume and time to freeze have been associated with levels of plasma Aβ [48] and Aβ levels in serum are also less stable than plasma Aβ levels [43].
Association of Aβ with AD and cerebrovascular disease
Cross-sectional and longitudinal results in DS individuals and subjects harboring autosomal dominant FAD mutations
The initial study by Scheuner et al. described increased plasma levels of Aβ1-42 in subjects from FAD kindreds with pathogenic mutations in the APP, PSEN1 and PSEN2 genes when compared to non-mutation bearing controls [49] and Kosaka et al. found increased plasma levels of Aβ1-42 when comparing AD patients carrying the βAPP717 mutation to sporadic AD patients [50]. Recently, a cross-sectional cohort of asymptomatic carriers of the PSEN1 E280A mutation had higher Aβ1-42 and Aβ1-42/Aβ1-40 than matched CN controls without the mutation [51].
DS subjects show higher plasma Aβ1-42 and Aβ1-40 levels than CN subjects without trisomy 21 [34, 52]. Two studies found no differences comparing DS with and without dementia, although an association between Aβ levels and neuropsychological scores in multivariable adjusted models was found [34, 35]. In one of these studies demented DS (dDS) subjects with longer dementia duration showed higher Aβ1-42, lower Aβ1-40 and a higher Aβ1-42/Aβ1-40 ratio than those with shorter dementia duration [35]. Two other studies comparing dDS to cognitively normal DS (cnDS) found a higher Aβ1-42/Aβ1-40 ratio in dDS [53] and increased Aβ1-40 levels in dDS subjects compared to cnDS that remained stable during a follow-up of several years [54]. Consecutive studies by Schupf et al. [32, 52] have described increased Aβ1-42 in dDS when compared to cnDS. These and other studies of plasma Aβ levels in subjects with trisomy 21 and pathogenic FAD mutations are summarized in Table 1.
There are limited data from prospective studies of plasma Aβ levels in subjects with DS (Table 2), but one study described an increased risk of dementia in subjects who at baseline had increased levels of Aβ1-42 or Aβ1-40 [54]. However, in studies conducted by another group, only baseline levels of Aβ1-42 were associated with an increased risk of dementia and death [32]. Finally, in a third study, Schupf et al. [33] compared the measurements of the last and baseline visits, finding an increased risk of dementia with an increase in Aβ1-40, a decrease in Aβ1-42 or a decrease in Aβ1-42/Aβ1-40 ratio with repeated sampling during follow-up.
Cross-sectional results in sporadic AD cases
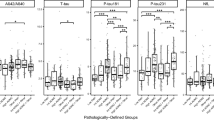
Results differ between studies including CN and sporadic AD subjects (Table 3). Different associations have been reported, with increased levels of Aβ1-42 in AD patients [27], decreased levels of Aβ1-42 in AD [14] and increased Aβ1-40 in AD [55]. Regarding the gender effect, one study found higher Aβ1-42 levels in women with mild cognitive impairment (MCI) compared to CN women and CN and MCI male subjects [41].
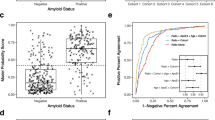
Some studies classified subjects not only based on clinical diagnosis but also on AD-like CSF profiles for tau and Aβ profiles [10, 13, 56]. In a study that included CN and MCI subjects, the group of CN and MCI subjects with AD-like CSF tau and Aβ profiles showed lower plasma Aβ1-42/Aβ1-40 than CN and MCI subjects with normal CSF tau and Aβ levels [13]. Another study found decreased Aβ1-42 and Aβ1-42/Aβ1-40 in MCI and AD subjects with an AD-like CSF tau and Aβ signature when compared to MCI and AD subjects with normal CSF tau and Aβ levels [56]. A more complex association was found for plasma Aβ1-40 and Aβ1-42 levels in the AD Neuroimaging Initiative (ADNI) cohort, showing an interaction between age and diagnostic groups defined by an AD-like CSF tau and Aβ profile [10]. Based on these results, only younger MCI and AD subjects with an AD-like CSF signature showed lower Aβ1-40 and Aβ1-42 values than older MCI and AD subjects with an AD-like CSF signature or subjects with a normal CSF signature. These findings indicate that the presence of AD-like CSF in younger cognitively impaired subjects was what defined the group with lower plasma Aβ. There were not enough CN subjects with AD-like CSF to test the association in this group of subjects who are in the pre-symptomatic stage of AD. Although most of these studies do not report sensitivity, specificity or area under the curve (AUC) measures for plasma Aβ levels, it is clear from these publications that determination of plasma Aβ levels is not useful as a diagnostic classifier.
Longitudinal results in the CN population and MCI and sporadic AD cases
Different measures of plasma Aβ have been associated with progression to dementia (Table 4): high baseline Aβ1-42 [30, 57], low baseline Aβ1-42/Aβ1-40 [58, 59], low baseline Aβ1-40 or Aβ1-42 [60], high baseline Aβ1-40 [29], high Aβ1-40 or low Aβ1-42/Aβ1-40 [61] and low Aβ1-40 in older subjects [62]. Finally, other studies found no associations of plasma Aβ levels with progression to dementia [10, 13, 63]. A study including information on vascular risk factors in midlife and a long follow-up period after baseline plasma sampling found an increased risk of dementia in subjects with low Aβ1-40 and Aβ1-42 at baseline and there was an interaction between plasma Aβ levels and diastolic blood pressure that indicated a higher incidence of dementia in subjects with higher diastolic blood pressure and low plasma Aβ levels [60]. One study that compared Aβ plasma levels in CN and MCI subjects who remained cognitively stable or progressed to AD found no differences in these two different cohorts [13], but, as noted above, there were significant differences based on the CSF-defined groups.
Other studies measuring plasma Aβ levels included correlations of these values with cognitive measures instead of using a diagnosis as outcome. One study included 481 subjects with a long follow-up and repeated measurements, and it used repeated brief telephone interviews for determining the study outcome, and the authors reported greater cognitive decline in subjects with a low Aβ1-42/Aβ1-40 at baseline [64]. However, interassay CV was over 30% (repeated subject measurements were included in the same assay with CV <10%). A larger study of 997 CN subjects followed for 9 years also found a faster cognitive decline in subjects with a lower Aβ1-42/Aβ1-40 at baseline [65]. Cosentino et al. [66] followed 880 subjects for 4.5 years who were CN at baseline or had cognitive impairment that was not severe enough for a dementia diagnosis. In this study, subjects with higher baseline Aβ1-40 and Aβ1-42 and stable or decreasing Aβ1-42 levels during follow-up had a faster rate of decline, whereas Aβ1-42/Aβ1-40 showed no such association. On the other hand, in another study by Locascio et al. [67], the rate of cognitive decline in 122 AD patients was determined in subjects followed for 4.2 years, and these authors described a faster decline in subjects with lower plasma Aβ1-40 and Aβ1-42 at baseline. Two studies found an interaction between cognitive reserve and Aβ plasma levels, indicating that subjects with lower cognitive reserve showed a greater decline associated with Aβ levels [10, 65].
Longitudinal sampling of Aβ plasma measures
A small number of studies have included repeated sampling of plasma Aβ levels [10, 27, 29, 57]. In the study by Mayeux et al. [27], a general increase was found for plasma Aβ1-40 over time, and plasma Aβ1-40 levels in CN stable subjects showed an increase over time, while incident and baseline AD subjects showed a decrease over time. A second study of the same group reported an increased incidence of dementia in CN subjects who showed a decrease in Aβ1-42 and Aβ1-42/Aβ1-40 during follow-up [57]. The study of Okereke et al. [64] found that a decrease in Aβ1-42/Aβ1-40 in the repeated plasma measurement was associated with greater cognitive decline. Lastly, studies reported by Hansson et al. [29] and Toledo et al. [10] found that during follow-up of 324 subjects for 5 years in the former and 613 subjects for 2 to 3 years in the latter study, there was an increase of Aβ1-40 and Aβ1-42, whereas Aβ1-42/Aβ1-40 decreased.
Aβ plasma measures and cerebrovascular disease
An association between plasma Aβ1-40 and Aβ1-42 levels in APOE ε4 carriers and in subjects known to have lacunar infarcts and white matter hyperintensities has been described in the Rotterdam study [28]. A second study that included subjects with cerebral amyloid angiopathy, MCI and AD also found an association between increased Aβ plasma and the presence of white matter hyperintensities and lacunar infarcts [68]. A third study specifically analyzed the association between microbleeds and plasma Aβ levels in subjects with AD and vascular dementia [69]. In this study, patients with nonlobar hemorrhages, located in the deep gray matter region and associated with hypertensive vasculopathy, showed higher Aβ1-40 plasma levels compared to subjects with lobar hemorrhages, which are associated with cerebral amyloid angiopathy. In the ADNI cohort, we found no association between Aβ plasma levels and white matter hyperintensities, but subjects with infarcts on MRI had higher plasma Aβ1-42 levels [10]. Finally, a longitudinal study by Lambert et al. [59] reported a higher incidence of vascular dementia in subjects with a low Aβ1-42/Aβ1-40.
Aβ plasma measures as biomarkers in clinical trials
Repeated sampling and measurement of plasma Aβ levels have been used to monitor the pharmacodynamic response of subjects in clinical trials of γ-secretase inhibitors (GSIs) and modulators (GSMs) as well as for passive immunotherapy. Studies in subjects treated with GSIs showed an initial dose-dependent decrease of total Aβ and Aβ1-40 levels that was followed by a dose-independent increase of both analytes [70, 71]. A model based on a hypothetical inhibition of α-secretase by increases in C99 associated with GSI treatment has been proposed in order to explain these changes, but this remains to be proven [72]. Both studies by Siemers et al. [70, 71] did not report changes in CSF Aβ1-40 and Aβ1-42 levels, although the second sample was taken 4 hours after treatment and a longer timeframe might be needed to assess changes in the CSF levels of these Aβ species. Due to the worse cognitive outcome and secondary effects (severe gastrointestinal toxicity, immunomodulation and skin cancer) in patients treated with GSIs [73], research in this area has shifted towards GSMs that spare Notch signaling. These GSM have also shown a decrease of plasma Aβ [74–76] but the results regarding any Aβ-rebound are contradictory for GSMs [75, 76]. On the other hand, passive immunotherapy results from clinical trials suggest that there is a dose-dependent transient increase of plasma Aβ in response to the monoclonal anti-Aβ antibody infusion and this was reported to last several weeks [77]. Thus, more research is clearly needed to elucidate the effects of these disease-modifying therapies on plasma Aβ levels.
Conclusions
Plasma Aβ is well known to originate in different organs and it also is known that Aβ binds to different proteins and cells in the blood, thereby possibly accounting for why plasma Aβ levels do not correlate with Aβ measured in CSF or CNS plaque burden measured by PET amyloid plaque imaging. Levels of plasma Aβ increase with aging and some clinical associations may change depending on the age of the selected sample. The selection of capture antibodies and analytical platforms can have an important impact on the measured Aβ levels; a wide range of mean Aβ1-40 (214 [15] to 985 pg/ml [40]) and Aβ1-42 (36 [15] to 140 pg/ml [19]) levels in AD patients has been reported in different studies and this also is the case for studies of CN subjects. Moreover, even in studies that use the same analytical platform and capture antibodies, there are important differences in the measured Aβ levels, which could be attributed to pre-analytical and analytical factors [10, 42–44, 48]. A recent study showed that automating multiple pipetting steps in a commercially available immunoassay that measures Aβ1-42 and Aβ1-40 provided better precision, thus leading to standardization of reagent dispensing in this test system [48]. Therefore, standardization efforts such as this and similar to the ones undertaken in the field of CSF Aβ measurements are needed [47]. Thus, this variability precludes the possibility of establishing diagnostic or prognostic cut-offs across different studies and populations until these assays are better standardized.
Using the profile of CSF tau and Aβ levels to define groups that have an underlying AD pathology reveals associations between subjects with and without AD-like CSF irrespective of a clinical diagnosis of CN, MCI or AD. Clinical diagnosis in the absence of a neuropathological validation or a CSF Aβ levels/PET plaque load validation may underestimate and confound the diagnostic/prognostic value of plasma Aβ measurements [2]. Cerebrovascular disease, which is a frequent finding in aged populations, is another important factor that can affect plasma Aβ levels and the prevalence of vascular risk factor and vascular disease varies considerably in the different samples according to the design of the study. While not useful as a diagnostic biomarker as shown by the cross-sectional studies, repeated Aβ plasma measurements in the same individual over time could become useful as a prognostic biomarker. Longitudinal studies favor the 'peripheral sink' hypothesis with a decrease of plasma levels starting in the dementia stage in contrast to an increase of plasma Aβ during the pre-symptomatic stage so that disease stage-specific changes later in the course of AD may explain previously described conflicting results. Although the reported differences or changes in Aβ plasma levels might not be large enough to predict the longitudinal outcome, it is potentially possible that this biomarker can serve as a prognostic factor or as an endpoint during follow-up of AD patients. However, prospective studies of cohorts with subsequent neuropathology confirmation of their diagnosis or in concert with data on CSF tau and Aβ levels as well as other biomarker data are needed to establish how to best interpret data on plasma Aβ levels in CN, MCI and AD subjects with and without other comorbid conditions such as cerebrovascular disease.
Note
This article is part of a series on Peripheral Biomarkers, edited by Douglas Galasko. Other articles in this series can be found at http://alzres.com/series/biomarkers
Abbreviations
- Aβ:
-
amyloid beta
- AD:
-
Alzheimer's disease
- ADNI:
-
Alzheimer's Disease Neuroimaging Initiative
- APOE:
-
apolipoprotein E
- APP:
-
Aβ precursor protein
- AV-45:
-
florbetapir-F18
- CN:
-
cognitively normal
- cnDS:
-
cognitively normal Down syndrome
- CNS:
-
central nervous system
- CSF:
-
cerebrospinal fluid
- CV:
-
coefficient of variation
- dDS:
-
demented Down syndrome
- DS:
-
Down syndrome
- ELISA:
-
enzyme-linked immunosorbent assay
- FAD:
-
familial Alzheimer's disease
- GSI:
-
γ-secretase inhibitor
- GSM:
-
γ-secretase modulator
- MCI:
-
mild cognitive impairment
- PET:
-
positron emission tomography
- PiB:
-
Pittsburgh Compound-B-C11
References
Montine TJ, Phelps CH, Beach TG, Bigio EH, Cairns NJ, Dickson DW, Duyckaerts C, Frosch MP, Masliah E, Mirra SS, Nelson PT, Schneider JA, Thal DR, Trojanowski JQ, Vinters HV, Hyman BT, National Institute on Aging; Alzheimer's Association: National Institute on Aging-Alzheimer's Association guidelines for the neuropathologic assessment of Alzheimer's disease: a practical approach. Acta Neuropathol. 2012, 123: 1-11. 10.1007/s00401-011-0910-3.
Toledo JB, Brettschneider J, Grossman M, Arnold SE, Hu WT, Xie SX, Lee VM, Shaw LM, Trojanowski JQ: CSF biomarkers cutoffs: the importance of coincident neuropathological diseases. Acta Neuropathol. 2012, 124: 23-35. 10.1007/s00401-012-0983-7.
Clark CM, Schneider JA, Bedell BJ, Beach TG, Bilker WB, Mintun MA, Pontecorvo MJ, Hefti F, Carpenter AP, Flitter ML, Krautkramer MJ, Kung HF, Coleman RE, Doraiswamy PM, Fleisher AS, Sabbagh MN, Sadowsky CH, Reiman EP, Zehntner SP, Skovronsky DM, AV45-A07 Study Group: Use of florbetapir-PET for imaging beta-amyloid pathology. JAMA. 2011, 305: 275-283. 10.1001/jama.2010.2008.
Wolk DA, Zhang Z, Boudhar S, Clark CM, Pontecorvo MJ, Arnold SE: Amyloid imaging in Alzheimer's disease: comparison of florbetapir and Pittsburgh compound-B positron emission tomography. J Neurol Neurosurg Psychiatry. 2012, 83: 923-926. 10.1136/jnnp-2012-302548.
Rissman RA, Trojanowski JQ, Shaw LM, Aisen PS: Longitudinal plasma amyloid beta as a biomarker of Alzheimer's disease. J Neural Transm. 2012, 119: 843-850. 10.1007/s00702-012-0772-4.
Arai H, Lee VM, Otvos L, Greenberg BD, Lowery DE, Sharma SK, Schmidt ML, Trojanowski JQ: Defined neurofilament, tau, and beta-amyloid precursor protein epitopes distinguish Alzheimer from non-Alzheimer senile plaques. Proc Natl Acad Sci USA. 1990, 87: 2249-2253. 10.1073/pnas.87.6.2249.
Sinha S, Anderson JP, Barbour R, Basi GS, Caccavello R, Davis D, Doan M, Dovey HF, Frigon N, Hong J, Jacobson-Croak K, Jewett N, Keim P, Knops J, Lieberburg I, Power M, Tan H, Tatsuno G, Tung J, Schenk D, Seubert P, Suomensaari SM, Wang S, Walker D, Zhao J, McConlogue L, John V: Purification and cloning of amyloid precursor protein beta-secretase from human brain. Nature. 1999, 402: 537-540. 10.1038/990114.
Mawuenyega KG, Sigurdson W, Ovod V, Munsell L, Kasten T, Morris JC, Yarasheski KE, Bateman RJ: Decreased clearance of CNS beta-amyloid in Alzheimer's disease. Science. 2010, 330: 1774-10.1126/science.1197623.
Castellano JM, Kim J, Stewart FR, Jiang H, DeMattos RB, Patterson BW, Fagan AM, Morris JC, Mawuenyega KG, Cruchaga C, Goate AM, Bales KR, Paul SM, Bateman RJ, Holtzman DM: Human apoE isoforms differentially regulate brain amyloid-beta peptide clearance. Sci Transl Med. 2011, 3: 89ra57-10.1126/scitranslmed.3002156.
Toledo JB, Vanderstichele H, Figurski M, Aisen PS, Petersen RC, Weiner MW, Jack CR, Jagust W, Decarli C, Toga AW, Toledo E, Xie SX, Lee VM, Trojanowski JQ, Shaw LM, Alzheimer's Disease Neuroimaging Initiative: Factors affecting Abeta plasma levels and their utility as biomarkers in ADNI. Acta Neuropathol. 2011, 122: 401-413. 10.1007/s00401-011-0861-8.
Huang Y, Potter R, Sigurdson W, Kasten T, Connors R, Morris JC, Benzinger T, Mintun M, Ashwood T, Ferm M, Budd SL, Bateman RJ: beta-Amyloid dynamics in human plasma. Arch Neurol. 2012, 69: 1591-1597. 10.1001/archneurol.2012.18107.
Le Bastard N, Aerts L, Leurs J, Blomme W, De Deyn PP, Engelborghs S: No correlation between time-linked plasma and CSF Abeta levels. Neurochem Int. 2009, 55: 820-825. 10.1016/j.neuint.2009.08.006.
Hansson O, Zetterberg H, Vanmechelen E, Vanderstichele H, Andreasson U, Londos E, Wallin A, Minthon L, Blennow K: Evaluation of plasma Abeta(40) and Abeta(42) as predictors of conversion to Alzheimer's disease in patients with mild cognitive impairment. Neurobiol Aging. 2010, 31: 357-367. 10.1016/j.neurobiolaging.2008.03.027.
Lui JK, Laws SM, Li QX, Villemagne VL, Ames D, Brown B, Bush AI, De Ruyck K, Dromey J, Ellis KA, Faux NG, Foster J, Fowler C, Gupta V, Hudson P, Laughton K, Masters CL, Pertile K, Rembach A, Rimajova M, Rodrigues M, Rowe CC, Rumble R, Szoeke C, Taddei K, Taddei T, Trounson B, Ward V, Martins RN, AIBL Research Group: Plasma amyloid-beta as a biomarker in Alzheimer's disease: the AIBL study of aging. J Alzheimers Dis. 2010, 20: 1233-1242.
Fagan AM, Mintun MA, Shah AR, Aldea P, Roe CM, Mach RH, Marcus D, Morris JC, Holtzman DM: Cerebrospinal fluid tau and ptau(181) increase with cortical amyloid deposition in cognitively normal individuals: implications for future clinical trials of Alzheimer's disease. EMBO Mol Med. 2009, 1: 371-380. 10.1002/emmm.200900048.
Weigand SD, Vemuri P, Wiste HJ, Senjem ML, Pankratz VS, Aisen PS, Weiner MW, Petersen RC, Shaw LM, Trojanowski JQ, Knopman DS, Jack CR, Alzheimer's Disease Neuroimaging Initiative: Transforming cerebrospinal fluid Abeta42 measures into calculated Pittsburgh Compound B units of brain Abeta amyloid. Alzheimers Dement. 2011, 7: 133-141. 10.1016/j.jalz.2010.08.230.
Devanand DP, Schupf N, Stern Y, Parsey R, Pelton GH, Mehta P, Mayeux R: Plasma Abeta and PET PiB binding are inversely related in mild cognitive impairment. Neurology. 2011, 77: 125-131. 10.1212/WNL.0b013e318224afb7.
Selkoe DJ, Podlisny MB, Joachim CL, Vickers EA, Lee G, Fritz LC, Oltersdorf T: Beta-amyloid precursor protein of Alzheimer disease occurs as 110- to 135-kilodalton membrane-associated proteins in neural and nonneural tissues. Proc Natl Acad Sci USA. 1988, 85: 7341-7345. 10.1073/pnas.85.19.7341.
Roher AE, Esh CL, Kokjohn TA, Castaño EM, Van Vickle GD, Kalback WM, Patton RL, Luehrs DC, Daugs ID, Kuo YM, Emmerling MR, Soares H, Quinn JF, Kaye J, Connor DJ, Silverberg NB, Adler CH, Seward JD, Beach TG, Sabbagh MN: Amyloid beta peptides in human plasma and tissues and their significance for Alzheimer's disease. Alzheimers Dement. 2009, 5: 18-29. 10.1016/j.jalz.2008.10.004.
Arai H, Lee VM, Messinger ML, Greenberg BD, Lowery DE, Trojanowski JQ: Expression patterns of beta-amyloid precursor protein (beta-APP) in neural and nonneural human tissues from Alzheimer's disease and control subjects. Ann Neurol. 1991, 30: 686-693. 10.1002/ana.410300509.
Kuo YM, Kokjohn TA, Kalback W, Luehrs D, Galasko DR, Chevallier N, Koo EH, Emmerling MR, Roher AE: Amyloid-beta peptides interact with plasma proteins and erythrocytes: implications for their quantitation in plasma. Biochem Biophys Res Commun. 2000, 268: 750-756. 10.1006/bbrc.2000.2222.
Skovronsky DM, Lee VM, Pratico D: Amyloid precursor protein and amyloid beta peptide in human platelets. Role of cyclooxygenase and protein kinase C. J Biol Chem. 2001, 276: 17036-17043. 10.1074/jbc.M006285200.
Pesini P, Perez-Grijalba V, Monleon I, Boada M, Tarraga L, Martinez-Lage P, San-Jose I, Sarasa M: Reliable measurements of the beta-amyloid pool in blood could help in the early diagnosis of AD. Int J Alzheimers Dis. 2012, 2012: 604141-
Ghiso J, Shayo M, Calero M, Ng D, Tomidokoro Y, Gandy S, Rostagno A, Frangione B: Systemic catabolism of Alzheimer's Abeta40 and Abeta42. J Biol Chem. 2004, 279: 45897-45908. 10.1074/jbc.M407668200.
Ghiso J, Calero M, Matsubara E, Governale S, Chuba J, Beavis R, Wisniewski T, Frangione B: Alzheimer's soluble amyloid beta is a normal component of human urine. FEBS Lett. 1997, 408: 105-108. 10.1016/S0014-5793(97)00400-6.
Fukumoto H, Tennis M, Locascio JJ, Hyman BT, Growdon JH, Irizarry MC: Age but not diagnosis is the main predictor of plasma amyloid beta-protein levels. Arch Neurol. 2003, 60: 958-964. 10.1001/archneur.60.7.958.
Mayeux R, Honig LS, Tang MX, Manly J, Stern Y, Schupf N, Mehta PD: Plasma A[beta]40 and A[beta]42 and Alzheimer's disease: relation to age, mortality, and risk. Neurology. 2003, 61: 1185-1190. 10.1212/01.WNL.0000091890.32140.8F.
van Dijk EJ, Prins ND, Vermeer SE, Hofman A, van Duijn CM, Koudstaal PJ, Breteler MM: Plasma amyloid beta, apolipoprotein E, lacunar infarcts, and white matter lesions. Ann Neurol. 2004, 55: 570-575. 10.1002/ana.20050.
Hansson O, Stomrud E, Vanmechelen E, Ostling S, Gustafson DR, Zetterberg H, Blennow K, Skoog I: Evaluation of plasma Abeta as predictor of Alzheimer's disease in older individuals without dementia: a population-based study. J Alzheimers Dis. 2012, 28: 231-238.
Mayeux R, Tang MX, Jacobs DM, Manly J, Bell K, Merchant C, Small SA, Stern Y, Wisniewski HM, Mehta PD: Plasma amyloid beta-peptide 1-42 and incipient Alzheimer's disease. Ann Neurol. 1999, 46: 412-416. 10.1002/1531-8249(199909)46:3<412::AID-ANA19>3.0.CO;2-A.
Ertekin-Taner N, Younkin LH, Yager DM, Parfitt F, Baker MC, Asthana S, Hutton ML, Younkin SG, Graff-Radford NR: Plasma amyloid beta protein is elevated in late-onset Alzheimer disease families. Neurology. 2008, 70: 596-606. 10.1212/01.wnl.0000278386.00035.21.
Schupf N, Patel B, Pang D, Zigman WB, Silverman W, Mehta PD, Mayeux R: Elevated plasma beta-amyloid peptide Abeta(42) levels, incident dementia, and mortality in Down syndrome. Arch Neurol. 2007, 64: 1007-1013. 10.1001/archneur.64.7.1007.
Schupf N, Zigman WB, Tang MX, Pang D, Mayeux R, Mehta P, Silverman W: Change in plasma Ass peptides and onset of dementia in adults with Down syndrome. Neurology. 2010, 75: 1639-1644. 10.1212/WNL.0b013e3181fb448b.
Head E, Doran E, Nistor M, Hill M, Schmitt FA, Haier RJ, Lott IT: Plasma amyloid-beta as a function of age, level of intellectual disability, and presence of dementia in Down syndrome. J Alzheimers Dis. 2011, 23: 399-409.
Prasher VP, Sajith SG, Mehta P, Zigman WB, Schupf N: Plasma beta-amyloid and duration of Alzheimer's disease in adults with Down syndrome. Int J Geriatric Psychiatry. 2010, 25: 202-207. 10.1002/gps.2321.
Ertekin-Taner N, Graff-Radford N, Younkin LH, Eckman C, Adamson J, Schaid DJ, Blangero J, Hutton M, Younkin SG: Heritability of plasma amyloid beta in typical late-onset Alzheimer's disease pedigrees. Genet Epidemiol. 2001, 21: 19-30. 10.1002/gepi.1015.
Ibrahim-Verbaas CA, Zorkoltseva IV, Amin N, Schuur M, Coppus AM, Isaacs A, Aulchenko YS, Breteler MM, Ikram MA, Axenovich TI, Verbeek MM, van Swieten JC, Oostra BA, van Duijn CM: Linkage analysis for plasma amyloid beta levels in persons with hypertension implicates Abeta-40 levels to presenilin 2. Hum Genet. 2012, 131: 1869-1876. 10.1007/s00439-012-1210-2.
Metti AL, Cauley JA, Ayonayon HN, Harris TB, Rosano C, Williamson JD, Yaffe K: The demographic and medical correlates of plasma Abeta40 and Abeta42. Alzheimer Dis Assoc Disord. 2012,
Brown BM, Peiffer JJ, Taddei K, Lui JK, Laws SM, Gupta VB, Taddei T, Ward VK, Rodrigues MA, Burnham S, Rainey-Smith SR, Villemagne VL, Bush A, Ellis KA, Masters CL, Ames D, Macaulay SL, Szoeke C, Rowe CC, Martins RN: Physical activity and amyloid-beta plasma and brain levels: results from the Australian Imaging, Biomarkers and Lifestyle Study of Ageing. Mol Psychiatry. 2012,
Arvanitakis Z, Lucas JA, Younkin LH, Younkin SG, Graff-Radford NR: Serum creatinine levels correlate with plasma amyloid Beta protein. Alzheimer Dis Assoc Disord. 2002, 16: 187-190. 10.1097/00002093-200207000-00009.
Assini A, Cammarata S, Vitali A, Colucci M, Giliberto L, Borghi R, Inglese ML, Volpe S, Ratto S, Dagna-Bricarelli F, Baldo C, Argusti A, Odetti P, Piccini A, Tabaton M: Plasma levels of amyloid beta-protein 42 are increased in women with mild cognitive impairment. Neurology. 2004, 63: 828-831. 10.1212/01.WNL.0000137040.64252.ED.
Lachno DR, Emerson JK, Vanderstichele H, Gonzales C, Martenyi F, Konrad RJ, Talbot JA, Lowe SL, Oefinger PE, Dean RA: Validation of a multiplex assay for simultaneous quantification of amyloid-beta peptide species in human plasma with utility for measurements in studies of Alzheimer's disease therapeutics. J Alzheimers Dis. 2012, 32: 905-918.
Bibl M, Welge V, Esselmann H, Wiltfang J: Stability of amyloid-beta peptides in plasma and serum. Electrophoresis. 2012, 33: 445-450. 10.1002/elps.201100455.
Lachno DR, Evert BA, Vanderstichele H, Robertson M, Demattos RB, Konrad RJ, Talbot JA, Racke MM, Dean RA: Validation of assays for measurement of amyloid-beta peptides in cerebrospinal flui and plasma specimens from patients with Alzheimer's disease treated with solanezumab. J Alzheimers Dis. 2013,
Le Bastard N, Leurs J, Blomme W, De Deyn PP, Engelborghs S: Plasma amyloid-beta forms in Alzheimer's disease and non-Alzheimer's disease patients. J Alzheimers Dis. 2010, 21: 291-301.
Lewczuk P, Esselmann H, Bibl M, Paul S, Svitek J, Miertschischk J, Meyrer R, Smirnov A, Maler JM, Klein C, Otto M, Bleich S, Sperling W, Kornhuber J, Rüther E, Wiltfang J: Electrophoretic separation of amyloid beta peptides in plasma. Electrophoresis. 2004, 25: 3336-3343. 10.1002/elps.200406068.
Vanderstichele H, Bibl M, Engelborghs S, Le Bastard N, Lewczuk P, Molinuevo JL, Parnetti L, Perret-Liaudet A, Shaw LM, Teunissen C, Wouters D, Blennow K: Standardization of preanalytical aspects of cerebrospinal fluid biomarker testing for Alzheimer's disease diagnosis: a consensus paper from the Alzheimer's Biomarkers Standardization Initiative. Alzheimers Dement. 2012, 8: 65-73. 10.1016/j.jalz.2011.07.004.
Figurski MJ, Waligorska T, Toledo J, Vanderstichele H, Korecka M, Lee VM, Trojanowski JQ, Shaw LM: Improved protocol for measurement of plasma beta-amyloid in longitudinal evaluation of Alzheimer's Disease Neuroimaging Initiative study patients. Alzheimers Dement. 2012, 8: 250-260. 10.1016/j.jalz.2012.01.001.
Scheuner D, Eckman C, Jensen M, Song X, Citron M, Suzuki N, Bird TD, Hardy J, Hutton M, Kukull W, Larson E, Levy-Lahad E, Viitanen M, Peskind E, Poorkaj P, Schellenberg G, Tanzi R, Wasco W, Lannfelt L, Selkoe D, Younkin S: Secreted amyloid beta-protein similar to that in the senile plaques of Alzheimer's disease is increased in vivo by the presenilin 1 and 2 and APP mutations linked to familial Alzheimer's disease. Nat Med. 1996, 2: 864-870. 10.1038/nm0896-864.
Kosaka T, Imagawa M, Seki K, Arai H, Sasaki H, Tsuji S, Asami-Odaka A, Fukushima T, Imai K, Iwatsubo T: The beta APP717 Alzheimer mutation increases the percentage of plasma amyloid-beta protein ending at A beta42(43). Neurology. 1997, 48: 741-745. 10.1212/WNL.48.3.741.
Reiman EM, Quiroz YT, Fleisher AS, Chen K, Velez-Pardo C, Jimenez-Del-Rio M, Fagan AM, Shah AR, Alvarez S, Arbelaez A, Giraldo M, Acosta-Baena N, Sperling RA, Dickerson B, Stern CE, Tirado V, Munoz C, Reiman RA, Huentelman MJ, Alexander GE, Langbaum JB, Kosik KS, Tariot PN, Lopera F: Brain imaging and fluid biomarker analysis in young adults at genetic risk for autosomal dominant Alzheimer's disease in the presenilin 1 E280A kindred: a case-control study. Lancet Neurol. 2012, 11: 1048-1056. 10.1016/S1474-4422(12)70228-4.
Schupf N, Patel B, Silverman W, Zigman WB, Zhong N, Tycko B, Mehta PD, Mayeux R: Elevated plasma amyloid beta-peptide 1-42 and onset of dementia in adults with Down syndrome. Neurosci Lett. 2001, 301: 199-203. 10.1016/S0304-3940(01)01657-3.
Matsuoka Y, Andrews HF, Becker AG, Gray AJ, Mehta PD, Sano MC, Dalton AJ, Aisen PS: The relationship of plasma Abeta levels to dementia in aging individuals with Down syndrome. Alzheimer Dis Assoc Disord. 2009, 23: 315-318. 10.1097/WAD.0b013e3181aba61e.
Coppus AM, Schuur M, Vergeer J, Janssens AC, Oostra BA, Verbeek MM, van Duijn CM: Plasma beta amyloid and the risk of Alzheimer's disease in Down syndrome. Neurobiol Aging. 2012, 33: 1988-1994. 10.1016/j.neurobiolaging.2011.08.007.
Mehta PD, Pirttila T, Mehta SP, Sersen EA, Aisen PS, Wisniewski HM: Plasma and cerebrospinal fluid levels of amyloid beta proteins 1-40 and 1-42 in Alzheimer disease. Arch Neurol. 2000, 57: 100-105. 10.1001/archneur.57.1.100.
Lewczuk P, Kornhuber J, Vanmechelen E, Peters O, Heuser I, Maier W, Jessen F, Bürger K, Hampel H, Frölich L, Henn F, Falkai P, Rüther E, Jahn H, Luckhaus Ch, Perneczky R, Schmidtke K, Schröder J, Kessler H, Pantel J, Gertz HJ, Vanderstichele H, de Meyer G, Shapiro F, Wolf S, Bibl M, Wiltfang J: Amyloid beta peptides in plasma in early diagnosis of Alzheimer's disease: A multicenter study with multiplexing. Exp Neurol. 2010, 223: 366-370. 10.1016/j.expneurol.2009.07.024.
Schupf N, Tang MX, Fukuyama H, Manly J, Andrews H, Mehta P, Ravetch J, Mayeux R: Peripheral Abeta subspecies as risk biomarkers of Alzheimer's disease. Proc Natl Acad Sci USA. 2008, 105: 14052-14057. 10.1073/pnas.0805902105.
Graff-Radford NR, Crook JE, Lucas J, Boeve BF, Knopman DS, Ivnik RJ, Smith GE, Younkin LH, Petersen RC, Younkin SG: Association of low plasma Abeta42/Abeta40 ratios with increased imminent risk for mild cognitive impairment and Alzheimer disease. Arch Neurol. 2007, 64: 354-362. 10.1001/archneur.64.3.354.
Lambert JC, Schraen-Maschke S, Richard F, Fievet N, Rouaud O, Berr C, Dartigues JF, Tzourio C, Alperovitch A, Buee L, Amouyel P: Association of plasma amyloid beta with risk of dementia: the prospective Three-City Study. Neurology. 2009, 73: 847-853. 10.1212/WNL.0b013e3181b78448.
Shah NS, Vidal JS, Masaki K, Petrovitch H, Ross GW, Tilley C, DeMattos RB, Tracy RP, White LR, Launer LJ: Midlife blood pressure, plasma beta-amyloid, and the risk for Alzheimer disease: the Honolulu Asia Aging Study. Hypertension. 2012, 59: 780-786. 10.1161/HYPERTENSIONAHA.111.178962.
van Oijen M, Hofman A, Soares HD, Koudstaal PJ, Breteler MM: Plasma Abeta(1-40) and Abeta(1-42) and the risk of dementia: a prospective case-cohort study. Lancet Neurol. 2006, 5: 655-660. 10.1016/S1474-4422(06)70501-4.
Sundelöf J, Giedraitis V, Irizarry MC, Sundström J, Ingelsson E, Rönnemaa E, Arnlöv J, Gunnarsson MD, Hyman BT, Basun H, Ingelsson M, Lannfelt L, Kilander L: Plasma beta amyloid and the risk of Alzheimer disease and dementia in elderly men: a prospective, population-based cohort study. Arch Neurol. 2008, 65: 256-263. 10.1001/archneurol.2007.57.
Lopez OL, Kuller LH, Mehta PD, Becker JT, Gach HM, Sweet RA, Chang YF, Tracy R, DeKosky ST: Plasma amyloid levels and the risk of AD in normal subjects in the Cardiovascular Health Study. Neurology. 2008, 70: 1664-1671. 10.1212/01.wnl.0000306696.82017.66.
Okereke OI, Xia W, Selkoe DJ, Grodstein F: Ten-year change i n plasma amyloid beta levels and late-life cognitive decline. Arch Neurol. 2009, 66: 1247-1253. 10.1001/archneurol.2009.207.
Yaffe K, Weston A, Graff-Radford NR, Satterfield S, Simonsick EM, Younkin SG, Younkin LH, Kuller L, Ayonayon HN, Ding J, Harris TB: Association of plasma beta-amyloid level and cognitive reserve with subsequent cognitive decline. JAMA. 2011, 305: 261-266. 10.1001/jama.2010.1995.
Cosentino SA, Stern Y, Sokolov E, Scarmeas N, Manly JJ, Tang MX, Schupf N, Mayeux RP: Plasma β-amyloid and cognitive decline. Arch Neurol. 2010, 67: 1485-1490. 10.1001/archneurol.2010.189.
Locascio JJ, Fukumoto H, Yap L, Bottiglieri T, Growdon JH, Hyman BT, Irizarry MC: Plasma amyloid beta-protein and C-reactive protein in relation to the rate of progression of Alzheimer disease. Arch Neurol. 2008, 65: 776-785. 10.1001/archneur.65.6.776.
Gurol ME, Irizarry MC, Smith EE, Raju S, Diaz-Arrastia R, Bottiglieri T, Rosand J, Growdon JH, Greenberg SM: Plasma beta-amyloid and white matter lesions in AD, MCI, and cerebral amyloid angiopathy. Neurology. 2006, 66: 23-29. 10.1212/01.wnl.0000191403.95453.6a.
Goos JD, Teunissen CE, Veerhuis R, Verwey NA, Barkhof F, Blankenstein MA, Scheltens P, van der Flier WM: Microbleeds relate to altered amyloid-beta metabolism in Alzheimer's disease. Neurobiol Aging. 2012, 33: e1011-1019. 1011
Siemers ER, Dean RA, Friedrich S, Ferguson-Sells L, Gonzales C, Farlow MR, May PC: Safety, tolerability, and effects on plasma and cerebrospinal fluid amyloid-beta after inhibition of gamma-secretase. Clin Neuropharmacol. 2007, 30: 317-325. 10.1097/WNF.0b013e31805b7660.
Siemers E, Skinner M, Dean RA, Gonzales C, Satterwhite J, Farlow M, Ness D, May PC: Safety, tolerability, and changes in amyloid beta concentrations after administration of a gamma-secretase inhibitor in volunteers. Clin Neuropharmacol. 2005, 28: 126-132. 10.1097/01.wnf.0000167360.27670.29.
Ortega F, Stott J, Visser SA, Bendtsen C: Interplay between a lpha-, beta-, and gamma-secretases determines biphasic amyloid-beta protein level in the presence of a gamma-secretase inhibitor. J Biol Chem. 2013, 288: 785-792. 10.1074/jbc.M112.419135.
Imbimbo BP, Panza F, Frisardi V, Solfrizzi V, D'Onofrio G, Logroscino G, Seripa D, Pilotto A: Therapeutic intervention for Alzheimer's disease with gamma-secretase inhibitors: still a viable option?. Expert Opin Investig Drugs. 2011, 20: 325-341. 10.1517/13543784.2011.550572.
Galasko DR, Graff-Radford N, May S, Hendrix S, Cottrell BA, Sagi SA, Mather G, Laughlin M, Zavitz KH, Swabb E, Golde TE, Murphy MP, Koo EH: Safety, tolerability, pharmacokinetics, and Abeta levels after short-term administration of R-flurbiprofen in healthy elderly individuals. Alzheimer Dis Assoc Disord. 2007, 21: 292-299. 10.1097/WAD.0b013e31815d1048.
Li T, Huang Y, Jin S, Ye L, Rong N, Yang X, Ding Y, Cheng Z, Zhang J, Wan Z, Harrison DC, Hussain I, Hall A, Lee DH, Lau LF, Matsuoka Y: Gamma-secretase modulators do not induce Abeta-rebound and accumulation of beta-C-terminal fragment. J Neurochem. 2012, 121: 277-286. 10.1111/j.1471-4159.2011.07560.x.
Tong G, Wang JS, Sverdlov O, Huang SP, Slemmon R, Croop R, Castaneda L, Gu H, Wong O, Li H, Berman RM, Smith C, Albright CF, Dockens RC: Multicenter, randomized, double-blind, placebo-controlled, single-ascending dose study of the oral gamma-secretase inhibitor BMS-708163 (Avagacestat): tolerability profile, pharmacokinetic parameters, and pharmacodynamic markers. Clin Ther. 2012, 34: 654-667. 10.1016/j.clinthera.2012.01.022.
Uenaka K, Nakano M, Willis BA, Friedrich S, Ferguson-Sells L, Dean RA, Ieiri I, Siemers ER: Comparison of pharmacokinetics, pharmacodynamics, safety, and tolerability of the amyloid beta monoclonal antibody solanezumab in Japanese and white patients with mild to moderate alzheimer disease. Clin Neuropharmacol. 2012, 35: 25-29. 10.1097/WNF.0b013e31823a13d3.
Blasko I, Kemmler G, Jungwirth S, Wichart I, Krampla W, Weissgram S, Jellinger K, Tragl KH, Fischer P: Plasma amyloid beta-42 independently predicts both late-onset depression and Alzheimer disease. Am J Geriatric Psychiatry. 2010, 18: 973-982. 10.1097/JGP.0b013e3181df48be.
Acknowledgements
The studies reviewed here from Penn were supported in part by AD10124. JQT is the William Maul Measey-Truman G Schnabel Jr Professor of Geriatric Medicine and Gerontology and JBT is supported in part by a grant of the Alfonso Martín Escudero Foundation.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Toledo, J.B., Shaw, L.M. & Trojanowski, J.Q. Plasma amyloid beta measurements - a desired but elusive Alzheimer's disease biomarker. Alz Res Therapy 5, 8 (2013). https://doi.org/10.1186/alzrt162
Published:
DOI: https://doi.org/10.1186/alzrt162