Abstract
Objectives
There has been a rise in the number of overweight women across the globe and sub-Saharan Africa has not been spared. Our objective was to describe the performance of household food security as a factor in determining overweight and underweight among Kenyan women of child-bearing age.
Design
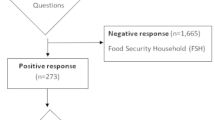
A cross sectional survey using a structured questionnaire was carried out among 656 households with women of child-bearing age from both rural and urban settings in the Rift Valley, Kenya.
Results
Of all households involved, 70.1% were categorized as severely food insecure, 21.9% were moderately food insecure, and 3.7% were mildly food insecure, whereas 4.3% were food secure. Urban women had higher mean BMI (M = 24.53, SD = 4.36), compared to rural women (M = 22.52, SD = 3.71; P <0.000). Households with more children had decreased dietary diversity (r = -0.154; P <0.01). Logistical regression indicated that more food-secure households (OR = 0.97; 95% CI 9.4, 1.0), urban residence (OR = 1.82; 95% CI 1.1, 3.0), older age (OR = 1.10; 95% CI 1.1, 1.5), and high standard of living (OR = 1.79; 95% CI 1.2, 1.5) were strong predictors of overweight while being underweight was predicted by younger age (OR = 0.91; 95% CI, 0.83, 1.0).
Conclusions
A food-secure household does not predict underweight but predicts overweight among women.
Similar content being viewed by others
Introduction
Overweight and obesity and their risk factors are in the increase in sub-Saharan Africa with higher increase among urban-poor dwellers[1–4]. The current estimates are that as much as 20% to 50% of urban populations in Africa are classified as either overweight or obese[5, 6], and that by 2025 three quarters of the obese population worldwide will be in non-industrialized countries[7]. Reasons for the increase in overweight and obesity are not fully understood, although physical inactivity and increased consumption of high fat and refined carbohydrates are thought to be contributing factors[8–10]. However, it has also been suggested that overweight and obesity may occur due to limited availability of food and this occurs if food insecurity leads to consumption of obesity-promoting foods[11], overeating when food becomes available, or metabolic changes that hinder the efficient use of energy[12].
Food security exists when all people at all times have access to sufficient, safe, nutritious food for a healthy and active life[13]. Food insecurity is defined as limited or uncertain availability of nutritionally, adequate and safe foods, or limited or uncertain ability to acquire acceptable foods in socially acceptable ways[14]. Food insecurity and malnutrition result in serious health problems and loss of human potential in developing countries[15]. Increasing food insecurity in the developing world paradoxically has resulted in increasing numbers of overweight. Past studies cite increased availability of high sugar and energy, low fibre foods as a major cause for overweight and obesity[16, 17]. However, some studies conducted in developed countries have consistently shown that mild but not severe food insecurity is associated with obesity among women[18–20]. This association between food insecurity and obesity has not been confirmed in studies performed in developing countries, where poverty rates are much higher[21]. In spite of the increasing numbers of overweight people, the underweight population still persists in these food insecure groups, and both may coexist within the same households or neighbourhoods[22, 23]. Although the prevalence of overweight exceeds that of underweight in most developing countries[24], the consequence of both are damaging to health. A study among adults and children from low- and middle-income families in Bogota, Columbia, indicated that food insecurity was related to maternal underweight but not to maternal overweight[25]. The association of food insecurity and overweight is not consistent as found by two studies[26, 27]. The adverse health effects resulting from overweight and underweight are far reaching and sometimes permanent, and may result in death[28, 29]. Women and children are vulnerable to malnutrition and food insecurity. Further, women globally have higher rates of obesity than men[9]. Therefore, this study targets women of childbearing age in Kenya to identify the relationship between food insecurity, overweight, and underweight among this group of women and to highlight the predictors of overweight and underweight.
Methods
Access Scale (HFIAS) Study, setting, design, and sampling
This was a cross-sectional study that took place in Narok County, Kenya. The Narok County is made up of an agricultural and agro-pastrolists community in the South Rift Valley. The study was carried out in the Narok District Hospital, where we purposively selected women of childbearing age (15–45 years old) to participate in this prevalence study. The women were randomly selected from the Mother and Child Health clinics where they were bringing their children for immunization and weighing. The women were approached and assigned a number between 1 and 2 and all the women assigned number 1 were asked if they were willing to participate. A total of 649 participants from rural and urban areas agreed to the study protocol and gave an informed consent. The inclusion criterion was that the women must have one child below five years of age at the time of the study.
All study procedures were approved by the Institute for Research and Ethics Committee of Moi Teaching and Referral Hospital, Eldoret, Kenya. The subjects gave written and verbal consent to both the study procedure and participation. The data were collected by the principal author and three trained research assistants in July and August 2011.
Measurements
Data were collected through interviews and anthropometric measurements. The interview consisted of a structured questionnaire and included questions on household socioeconomic and demographic characteristics, 24-hour dietary recall, and a Household Food Insecurity measurement. After the interview, the respondents presented themselves for the anthropometric measurements. Data on standard of living (SOL), age, household size, marital status, and number of children were collected.
To measure SOL, we considered asset ownership as well as income and expenditure. Income and expenditure were categorized into 1 for high and 0 for low income as well as 1 for high expenditure and 0 for low expenditure. The assets included owning a radio, cell phone, refrigerator, mode of cooking (gas, firewood, or electricity), and type of house as well as having access to a toilet facility. We recorded the type of energy used for cooking into advanced and old methods of cooking: gas and electricity were included in the advanced list whereas charcoal and firewood, and other energy sources, were in the old methods of cooking. The type of house was the last factor, where type of house was defined by the roofing and the building materials. Iron sheets and tiled roofing as well as stone were categorized into 1 for higher levels whereas grass-thatched and mud/iron-sheet roofing were categorized into 0 for the lower level. Principle component analysis and calculation of Cronbach’s alpha resulted in an 8-item SOL scale.
Food insecurity was measured by the HFIAS, which is a 9-item scale consisting of two types of questions; an occurrence question followed by a frequency of occurrence question which asked the participant how often the condition reported in the previous occurrences question happened during the previous month[30]. The occurrence questions asked whether the respondent or other household members either felt a certain way or performed a particular behaviour over the previous month. Before inclusion in the questionnaire, the questions were reviewed with key informants as suggested in the protocol. A standard scoring procedure was used with 1 point for occurrence and 0 for non-occurrence. The frequency scores ranged from 0 to 3, where 0 was the score for non-occurrence, 1 for rarely (once or twice in the past four weeks), 2 for sometimes (three to ten times in the past four weeks), and 3 for often (more than ten times in the past month). For the purpose of this paper, we used the total score (9-items based on the frequency score). A total score of 27 represents the most food-insecure household whereas a lower score represents a more food-secure household.
Data on household dietary diversity was collected using a 24-hour recall method and information was entered into the Household Dietary Diversity Score (HDDS) sheet[13]. The HDDS captures dietary diversity in a normal 24-hour period by the household as a whole and not a single member. Food consumed outside the home that was not prepared in the home was not included. A set of 12 food groups was used to guide the scoring as per the food items consumed, with 1 being the minimum score and 12 as the maximum[13].
Anthropometric measurements of weight and height were taken from the woman who was interviewed. Weight was measured to the nearest 0.5 kg using a mechanical scale (SECA 762). Height was measured to the nearest millimetre also using a transportable stadiometer (SECA 214); the scales were calibrated after each session of measurements. Waist and hip measurements were measured using a tape. The waist was measured around the narrowest point between the navel and the ribcage and the hip was measured around the widest part of the hip to the nearest cm. All measurements were taken with light clothing on and without shoes. A total of two measurements were taken and an average calculated.
Data management and analysis
The data were entered using Microsoft® Excel 2003 and rechecked for accuracy to minimize errors. Analysis was done using Statistical Package for Social Sciences (SPPS) Version 17.1. Frequency distribution of all the data was done for descriptive purposes. Internal consistency of the measurements (Cronbach’s alpha) was calculated for the HFIAS and SOL. Pearson’s correlation analysis was performed to compare relationship between variables. Logistic regression analysis was used to examine factors related to underweight (body mass index (BMI) ≤18.5) and overweight (BMI ≥25), and linear regression analysis for predicting the total BMI score.
Results
Anthropometrics measurements and general characteristics
Table 1 presents data on the women’s age, marital status, education, and anthropometric measurements. Among the participants, 88.6% were married. At least 5.5% of the women had no formal or informal education and 49.2% had a post-primary level of education in the study group; primary education was reported by 45.3% of the women. Education beyond primary level was reported by 54.4% and 33.3% of the urban and rural participants, respectively. The main source of income, according to 38.6% of the respondents, was from formal employment. Running of a small holdings business, such as small shops or kiosks, as the main source of income was reported by 24.5%, whereas farming was the main source of income for 19.6% of participants. Crop production (28%) was the main agricultural activity followed by mixed farming at 11.6% (livestock and crop).
The percentage of women with more than one child under five years of age was 40%. The average household size was 5 and 4 in the rural and urban areas, respectively. At the interview date, 73.7% of the women had not moved residence within the past six months and 66.6% lived in rental houses. A total of 33.5% of women had access to their own tapped water, while 25.5% of the women used communal tapped-water points, 16% bought water from vendors, and 25% obtained the water from a borehole, a stream/river, or harvested rain water; 7.9% of women had no access to a toilet facility. Relief food, which is common in the arid and semi-arid areas, has not been accessed by 88.6% of the women in the community. Meals were shared at the same time by all family members in 66.3% of the households, whereas 16.9% served children first and 16.2% served husband or male figures in the households first.
Nutritional status and household food security
The BMI of women was higher in the urban (24.5) compared to the rural (22.5) areas. Combined overweight and obesity was higher in the urban (39.6%) compared to that of rural participants (21%). However, underweight was 11.2% and 3.7% among the rural and urban women, respectively. The percentage of the population that had a waist-to-hip ratio (WHR) ≥0.85 was 26.2%, whereas those who had a waist circumference ≥80 cm were 38.9% (Table 2). The HDDS had a mean score of 6.56 for the total population and did not significantly differ between urban and rural settings.
However, the HFIAS score differed slightly (P = 0.013) with rural settings being more insecure (12.61 ± 6.8) than the urban (11.20 ± 6.03). A total of 4.3% of the population were food secure, whereas 70.1% reported severe food insecure access. Affirmative responses to the 9 items in the scale ranged from 53.5% to 88.0%. The item least frequently receiving an affirmative response was question 8, ‘Did you or any household member go to sleep at night hungry?’ Whereas the item receiving the highest number of affirmative responses was question 1, ‘Did you worry that your household would not have enough food?’
Pearson product–moment correlations were computed to assess the relation between SOL, HDDS, education, residence, and number of children (Table 3). There was a positive association between HDDS and SOL (r = 0.27, P <0.01) and a negative association between HDDS and number of children (r = -0.15, P <0.01), whereas SOL was negatively associated with number of children (r = -0.31, P <0.01). When comparing education and BMI, there was a significant positive relationship between education and underweight (r = 0.15, P < 0.01). Looking at the numbers of those with no education and underweight, the numbers were higher in the rural (66.7%) areas compared to the urban (45.6%) areas. Overweight had a positive association with number of children (r = 0.082, P <0.05).
Logistic regression analyses were performed on overweight and underweight as separate outcomes and 8 predictor variables: marital status, education, SOL, number of children, HFIAS score, HDDS, age, and residence.
Tables 4 and5 show the regression coefficients, odds ratios (ORs) and 95% confidence intervals (CIs) for each of the 8 predictor variables. Predictors of overweight that were significant were SOL, age, number of children in the household, urban residence, and lower HFIAS scores as indicated in Table 4. Women who had higher SOL had higher odds of being overweight (OR = 1.79, 95% CI 1.19, 1.53), and older women had higher odds of being overweight (OR = 1.10, 95% CI, 1.05, 1.15). A negative association was reported between overweight and HFIAS (OR = 0.97, 95% CI 0.94, 1.0), indicating that the lower the HFIAS score the higher overweight and vice versa. Regarding the prediction of underweight, younger women had higher odds of being underweight (OR = 0.91, 95% CI 0.83, 1.0) (Table 5). Although not significant, being underweight reduced with increased SOL.
Linear regression analysis was computed to assess the association between BMI and all 8 predictor variables. There was a positive significant relation between BMI and the predictor variables (R2 = 0.17, P <0.001) as seen in Table 6. Only age (Beta = 0.28, P <0.001) and SOL (Beta = 0.29, P <0.001) were positively associated with BMI.
Discussion
In this study, urban women had higher numbers of overweight compared to their rural counterparts, and although underweight existed in both groups, the prevalence was lower compared to overweight in the study group. This is in agreement with many studies in developing countries that report that urban dwellers are frequently better nourished than their rural counterparts[31–33]. However, the fact that the urban areas in our study mainly consisted of peri-urban dwellers with a poor infrastructure and low economic status may explain the prevalence of underweight persisting among both the rural and urban dwellers, although the prevalence was high among rural dwellers. In addition, overweight is an emerging problem among the rural dwellers as observed in our study. The predictors of overweight among our participants were SOL, age, HFIAS score, residence, and number of children while age was a significant predictor of underweight.
In our study, the urban dwellers reported a high number of overweight and underweight, respectively, and overweight was related to a high SOL. This was the case in a study by Ziraba et al. that indicated that urban dwellers had the highest cases of obesity[2]. High SOL using wealth index may be translated to mean wealthy households; thus, our study agrees with the findings from a study among Ghanian women which indicated that obesity was common among wealthy households as opposed to the poor[34], and a study by Shayo and Mugusi[35] which indicated that participants with a high socioeconomic status had a statistically significant increased risk for obesity compared to participants with low socioeconomic status. It is worth noting that the study by Ziraba et al.[2] reports an increase in obesity among higher socioeconomic groups as well as an increase in the number of obese among the lower socioeconomic group. In our study, SOL was a measure of income, expenditure, access to toilet facility, advanced cooking methods, owning a cell phone, and type of housing material, thus, it cannot be used interchangeably with socioeconomic status in the reported studies.
Education levels within the study area were still low compared to other counties in Kenya[36]. Education is important in terms of making choices when it comes to resource allocation. Studies indicated that women who receive even a minimal education are generally more aware than those who have no education of how to utilize available resources for the improvement of their own nutritional status and that of their families[37–39]. A cultural practice that is common among the study population is that of marrying-off girls at a young age; thus, within this community one is likely to find young married women. The youngest participant among the study population was 15 years of age. According to a government document released in 2008, secondary education enrolment rate for girls in the study area was 15% and that of boys was 20%, while primary education enrolment rate was 73% and 83% for girls and boys, respectively[36]. Using education as a proxy for socioeconomic status the study by Ziraba et al.[2], which included data from Kenya, indicated that the prevalence of obesity was higher among the non-educated than educated group; however, in our study, it is worth noting that the percentage of women who had attained post-primary education was higher among rural dwellers compared to urban dwellers. Thus, the non-educated and the primary level-educated women were mainly found in the urban areas, where overweight was higher. In addition, overweight women were low among households where the respondent had no education but the numbers increased among the primary and secondary level of education respondents. This may relate to income or job opportunities, whereby the non-educated women had lower opportunities of obtaining higher paying employment while those with primary or secondary level of education had higher incomes and thus an increase in access to food; however, this may not always be the case.
Age was an important predictor of BMI among women; the older the women the higher the chances of them being overweight and the younger the women the higher the probability of underweight and thinness[40]. Women tend to gain weight with increasing age and parity[41–44]. However, some studies indicate greatest weight gain among young adults (20–29 y), and in particular women[45]. During pregnancy women gain weight which is difficult to lose after pregnancy and in the event that they become pregnant again additional weight is gained. This concurs with other studies that indicated that if excessive pregnancy weight is not lost soon after breastfeeding, overweight and obesity may occur[46]. However, younger age was an important predictor of underweight as also reported by Griffiths et al.[40]. In our study, underweight prevalence was also higher among rural women compared to urban women, which may be explained by the longer distances women travelled to access social amenities such as shops, health centres, searching for water, etc. Thus, activity levels may be high among this group leading to underweight and thinness. However, this is beyond the scope of this paper and will be discussed elsewhere.
Most households were predominantly male-headed households as indicated by the larger percentage of married women among the participants. According to a study in Ethiopia, marital status of women is associated with household headship and other social and economic status which affect women’s nutritional status[37]. When women control resources, children and household members are more well-nourished[47]. However, when it comes to nutritional status of children, conflicting results have also been reported in studies that show children of working mothers to have a lower nutritional status compared to children of mothers who work at home[48]. This brings into focus the issue of care, whereby women who leave their children in the care of others may compromise the nutritional status of their children as opposed to the mothers who work at home and care for their children themselves. In our study, the married participants had higher prevalence of overweight compared to the single, divorced, or separated; however, underweight was more prevalent among the younger group (15–24 years old).
Household food insecurity arises when families do not have enough to eat due to food being neither available nor accessible. In our study area, food insecurity was predominant in many households as reported in government documents[49]. Seasonal hunger, per se, is most common during planting seasons and just before harvest. According to a study by Vaitla et al., most of the world’s hunger and under-nutrition occurs during the pre-harvest season[50]. However, as much as this is the case in this population, overweight is still reported among some of the participants in our study, indicating that overweight is not only a disease of the rich but also of the poor. The results from this study indicated that household food insecurity access is a predictor of overweight, as has also been reported in other studies[2, 19, 21, 35]. In this study, household food insecurity access is not a statistically significant predictor of underweight. This is in contradiction with a study which showed that food insecurity predicted underweight but not overweight among adults and children[25]. The increasing overweight and underweight among respondents within food insecure household brings into question the quality of the food consumed, and perhaps also the quantity, particularly of fried foods which are cheap and easily available, predominantly in urban areas.
Parity was also a predictor of overweight in this study, given that when a woman gives birth to many children without losing the pregnancy weight between births, her weight progressively increases. Parity, according to a study done in Ghana, was significant in predicting obesity[34]. However, in our study, women who had one or two children were more likely to be underweight. The increased number of children per household means scarcer resources and increased physical activity for the mother in providing and caring for the children, and thus a lower BMI. Sanitation is equally important in determining nutrition. In the present study, most of the households used communal water points and in the rural area women travelled long distances to get water, whereas within the urban area water was sold at the communal water-points by water vendors. Several studies have looked at the relationship between sources of water and availability of toilet facility in that inadequate water and sanitation increase the probability of infectious disease and indirectly cause some types of malnutrition[38, 39]. The relationship between sanitation and nutritional status of women was reported in another unpublished article[51].
Our study had some limitations. Firstly, we did not study cultural diversity; different cultures have different food consumption patterns and dietary habits and thus nutritional status of the different communities (tribes) would differ as a result of varied dietary habits. Second, nutrient security is also important in explaining the overall nutritional status of an individual; our study did not look at the different nutrients in the diet, which would predispose one to either overweight or underweight. Finally, we did not take into consideration physical activity to explain overweight and underweight among women but included this in another ongoing study.
Conclusions
Overweight is a major nutritional problem among women in the study area although food insecurity is also a problem confirming the paradox of over-nutrition occurring where food insecurity exists. In our study, food secure households have higher odds of being overweight and not underweight. Other predictors of overweight included being in an urban settlement, high SOL, increasing number of children, and age, whereas, dietary diversity reduced with increasing household food insecurity.
Abbreviations
- BMI:
-
Body mass index
- HFIAS:
-
Household food insecurity access scale
- HDDS:
-
Household dietary diversity score
- SOL:
-
Standard of living
- WHR:
-
Waist-to-hip ratio.
References
Villamor E, Msamanga G, Urassa W, Petraro P, Spiegelman D, Hunter DJ, Fawzi WW: Trends in obesity, underweight and wasting among women attending prenatal clinics in urban Tanzania 1995–2004. Am J Clin Nutr. 2006, 83 (6): 1387-1394.
Ziraba AK, Fotso JC, Ochako R: Overweight and obesity in urban Africa: a problem of the rich or the poor?. BMC Public Health. 2009, 9: 465.
Abubakari AR, Lauder W, Agyemang C, Jones M, Kirk A, Bhopal RS: Prevalence and time trends in obesity among adult West African populations: a meta-analysis. Obes Rev. 2008, 9 (4): 297-311.
Martorell R, Khan LK, Hughes ML, Grummer-Strawn LM: Obesity in women in developing countries. Eur J Clin Nutr. 2000, 54 (3): 247-252.
Kamadjeu RM, Edwards R, Atanga JS, Kiawi EC, Unwin N, Mbanya JC: Anthropometry measures and prevalence of obesity in the urban adult population of Cameroon: an update from Cameroon burden of diabetes baseline survey. BMC Public Health. 2006, 6: 228.
Sodjinou R, Agueh V, Fayomi B, Delisle H: Obesity and cardio-metabolic risk factors in urban adult of Benin: relationship with socio-economic status, urbanization, and lifestyle patterns. BMC Public Health. 2008, 8: 84.
WHO: Preventing Chronic Diseases, A Vital Investment. 2005, Geneva: World Health Organization
Gulliford MC, Mahabir D, Rocke B: Food insecurity, food choices, and body mass index in adults: nutrition transition in Trinidad and Tobago. Int J Epidemiol. 2003, 32: 508-516.
WHO: Obesity: Preventing and Managing Global Epidemic in Report of a WHO Consultation WHO Technical Report. 2000, Geneva: World Health Organization
Hannack LJ, Jeffrey RW, Boutelle KN: Temporal trends in energy intake in the US: an ecological perspective. Am J Clin Nutr. 2002, 71: 1478-1484.
Dietz WH: Does hunger cause obesity?. Pediatrics. 1995, 95: 766-767.
Alaimo K, Olson CM, Frongilo EA: Low family income & food insufficiency in relationship to overweight in US children: is there a paradox. Arch Pediatrics Adolescents Med. 2001, 155: 1161-1167. 10.1001/archpedi.155.10.1161.
Swindale A, Bilinsky P: Household Dietary Diversity Score (HDDS) for Measurement of Household Food Access: Indicator Guide V. 2. 2006, Washington DC: Food and Nutrition Technical Assistance Project
Carlson SJ, Andrews MS, Biekel GW: Measuring food insecurity and hunger in the United Stats: development of a national benchmark measure and prevalence estimate. J Nutr. 1999, 129: 510S-06S.
Pinstrup-Andersen P, Cohen MJ: Modern biotechnology for food agriculture: risks and opportunity for the poor. Int J Biotechnology. 2000, 2 (1/2/3): 145-163. 10.1504/IJBT.2000.000123.
Popkin BM: An overview on the nutrition transition and its health implications: the Bellagio meeting. Public Health Nutr. 2002, 5 (1A): 93-103.
Clugston GA, Smith TE: Global nutrition problems and novel foods. Asia Pac J Clin Nutri. 2002, 11 (S6): S100-S111. 10.1046/j.1440-6047.11.s6.1.x.
Sarlio-Lahteenkorva S, Lahelma E: Food insecurity is associated with past and present economic disadvantage and body mass index. J Nutr. 2001, 131: 2880-2884.
Adams EJ, Grummer-Strawn L, Chavez G: Food insecurity is associated with increased risk of obesity in California women. J Nutr. 2003, 133: 1070-1074.
Townsend MS, Peerson J, Love B, Achterberg C, Murphy SP: Food insecurity is positively related to overweight in women. J Nutr. 2001, 131: 1738-1745.
Velasquez-Melendez G, Schlüssel MM, Brito AS, Silva AA, Lopes-Filho JD, Kac G: Mild but not light or severe food insecurity is associated with obesity among Brazilian women. J Nutri. 2011, 141 (5): 898-902. 10.3945/jn.110.135046.
Doak CM, Adair LS, Monteiro C, Popkin BM: Overweight and underweight coexist within households in Brazil, China and Russia. J Nutr. 2000, 130: 2965-2971.
Caballero B: A nutrition paradox – underweight and obesity in developing countries. N Engl J Med. 2005, 352 (15): 1514-1516.
Mendez MA, Monteiro CA, Popkin MB: Overweight exceeds underweight among women in most developing countries. Am J Clin Nutr. 2005, 81: 714-721.
Isanaka S, Mora-Plazas M, Lopez-Arana S, Baylin A, Villamor E: Food insecurity is highly prevalent and predicts underweight but not overweight in adults and school children from Bogota. Columbia. J Nutr. 2007, 137 (12): 2747-2755.
Whitaker RC, Sarin A: Change in food security status and change in weight are not associated in urban women with preschool children. J Nutr. 2007, 137: 2134-2139.
Jones SJ, Frongillo EA: Food insecurity and subsequent weight gain in women. Public Health Nutr. 2007, 10: 145-151.
Krause RM, Winston M, Fletcher BJ, Grundy SM: Obesity: impact on cardiovascular disease. Circulation. 1998, 98: 1472-1476. 10.1161/01.CIR.98.14.1472.
WHO: Obesity: Preventing and Managing the Global Epidemic in Report of WHO Consultation on Obesity 3–5 June 1997. 1997, Geneva: World Health Organization
Coates J, Swindale A, Bilinsky P: Household Food Insecurity Access Scale (HFIAS) for Measurement of Food Access: Indicator Guide v. 3. 2007, Washington DC: Food and Nutrition Technical Assistance Project
Smith LC, Ruel MT, Ndiaye A: Why is child malnutrition lower in urban than in rural areas? Evidence from 36 developing countries. World Dev. 2005, 33 (8): 1285-1305. 10.1016/j.worlddev.2005.03.002.
Ruel MT, Garrett JL, Morris SS, Maxwell DG, Oshaug A, Engle PL, Menon P, Slack AT, Haddad LJ: Urban challenges to food and nutrition security: a review of food security, health and Caregiving in the cities. FCND Discussion Paper. 1998, Washington DC: International Food Policy Research Institute
Marie T, Garrett JL: Features of Urban Food and Nutrition Security and Considerations for Successful Urban Programming in Paper Prepared for FAO Technical Workshop. 2003, Rome: Food Agricultural Organization
Dake FA, Tawiah EO, Badasu DM: Sociodemographic correlates of obesity among Ghanaian women. Public Health Nutr. 2010, 14 (7): 1285-1291.
Shayo GA, Mugusi FM: Prevalence of obesity and associated risk factors among adults in Kinondoni municipal district, Dar es Salam, Tanzania. BMC Public Health. 2011, 11: 365-
GOK: Narok District Development Plan. 2008, Nairobi: Kenya Bureau of Statistics & National Development Office (KNBS)
Girma W, Genebo T: Determinants of Nutritional Status of Women and Children in Ethiopia. 2002, Calverton, Maryland, USA: Measure DHS
UNICEF: Strategies of improving nutritional status of children and women in developing countries. Indian J Pediatr. 1990, 58 (1): 13-24.
Engle PL: Care and Child Nutrition: Theme Paper for the International Conference on Nutrition (ICN). 1992, New York: UNICEF
Griffiths PL, Bentley ME: The nutrition transition is underway in India. J Nutr. 2001, 131 (10): 2692-2700.
Cohen SS, Larson CO, Matthews CE, Buchowski MS, Signorello LB, Hargreaves MK, Blot WJ: Parity and breastfeeding in relation to obesity among black and white women in the southern community cohort study. J Womens Health. 2009, 18 (9): 1323-1332. 10.1089/jwh.2008.1181.
Harris HE, Elisson GT, Holliday M: Is there an independent association between parity and maternal weight gain?. Ann Hum Biol. 1997, 24 (6): 507-519.
Cohen A, Pieper CF, Brown AJ, Bastian LA: Number of children and risk of metabolic syndrome in women. J Womens Health. 2006, 15: 763-773. 10.1089/jwh.2006.15.763.
Buschur E, Kim C: Guidelines & interventions for obesity during pregnancy. Int J Gynaecol Obstet. 2012, 119 (1): 6-10.
Kimokoti RW, Newby PK, Gona P, Zhu L, McKeon-O'Malley C, Pablo Guzman J, D'Agostino RB, Millen BE: Patterns of weight change and progression to overweight and obesity differ in men and women: implications for research and interventions. Public Health Nutr. 2013, 16 (8): 1463-1475.
Rooney BL, Schauberger CW: Excessive pregnancy weight gain and long-term obesity: one decade later. Obstet Gynecol. 2002, 100 (2): 245-252.
Kelkar G: Rural Women’s Work and Capabilities: Information for Gender-Responsibilities Development Policies, in High-Level Consultation on Rural Women & Information. 1999, Rome: FAO
Bennett L: The role of women in income, production and intra-household allocation of resources as a determinant of child nutrition and health. Food Nutrition Bull. 1988, 10 (3):http://archive.unu.edu/unupress/food/8F103e/8F103E03.htm
GOK: Arid Lands Resource Management Project in Drought Monthly Bulletin. 2011, Nairobi: Ministry of State for Development of Northern Kenya and other Arid Lands
Vaitla B, Devereux S, Swan HS: Seasonal hunger: a neglected problem with proven solutions. PLoS Med. 2009, 6 (6): e1000101
Keino S, Plasqui G, van den Borne B: Is overweight found among the food insecure? - A study on prevalence and risk factors of malnutrition among children in Narok, Kenya. 2013, Unpublished Manuscript.
Acknowledgements
The authors are grateful to the Netherlands Fellowship Programme of NUFFIC for financing the study. They also would like to thank the staff of Narok District Hospital Mother and Child Health department for their cooperation during the data collection period. We also appreciate the effort of the research assistants.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors agree that they have no conflicting interests to declare.
Authors’ contributions
SK participated in the data collection, analysis, literature review and writing up the manuscript, GP and BVB also participated in analysis and interpreting results. All authors read and approved the manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an open access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Keino, S., Plasqui, G. & van den Borne, B. Household food insecurity access: a predictor of overweight and underweight among Kenyan women. Agric & Food Secur 3, 2 (2014). https://doi.org/10.1186/2048-7010-3-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/2048-7010-3-2