Abstract
Background
The genus Ajuga is used for the treatment of joint pain, gout, and jaundice in traditional Iranian medicine (TIM). Ajuga chamaecistus ssp. tomentella is an exclusive subspecies of Ajuga chamaecistus in the flora of Iran. The aim of this study was to evaluate antinociceptive properties of some extracts from aerial parts of A. chamaecistus ssp. tomentella.
Methods
Antinociceptive activities of total water and 80% methanol extracts, hexane, diethyl ether and n-butanolic partition fractions of the methanolic extract were analyzed using the formalin test in mice. Indomethacin (10 mg/kg) and normal saline were employed as positive and negative controls, respectively.
Results
Oral administration of all extracts (200, 400 and 600 mg/kg) 30 min before formalin injection had no effect against the acute phase (0–5 min after formalin injection) of the formalin-induced licking time, but hexane fraction (200 mg/kg) caused a significant effect (p < 0.001) on the chronic phase (15–60 min after formalin injection). Total water and diethyl ether extracts at a dose of 400 mg/kg showed a very significant analgesic activity on the chronic phase (p < 0.001 and p < 0.01, respectively).
Conclusions
The results of this study suggest that the extracts of A. chamaecistus ssp. tomentella have an analgesic property that supports traditional use of Ajuga genus for joint pain and other inflammatory diseases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Five species of genus Ajuga (Lamiaceae) are found in the flora of Iran in which Ajuga chamaecistus has been contained several endemic subspecies including A. chamaecistus ssp. tomentella[1]. Some species which belong to this annual and perennial genus are used as the medicinal plant in the traditional medicine of several countries mostly in Africa, Asia, and China as for wound healing; anthelmintic, antifungal, antifebrile, antitumor, antimicrobial, and diuretic agent, and for the treatment of hypertension, hyperglycemia, joint pain, etc. [2–4]. Ajuga chamaepitys (L.) Schreb. which grows in the Middle East and Asia has been used in the treatment of rheumatism, gout, dropsy, jaundice, and sclerosis. A. decombens Thunb. that originally grows in East Asia is used for analgesia, inflammation, fever, and joint pain [5]. Moreover in Iranian traditional medicine, the genus Ajuga (Kamaphytus) has been used for treatment of joint pain, gout, and jaundice [6].
Also, several biological studies have been performed on many species of this genus which have confirmed their ethno pharmacological properties such as hypoglycemic [7], anti-inflammatory [8], anabolic, analgesic, anti-arthritis, antipyretic, hepatoprotective, antibacterial, antifungal, antioxidant, cardiotonic [5], and antimalarial [9] properties and their application in the treatment of joint diseases [10].
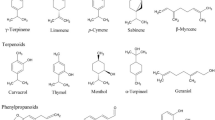
As well, many phytochemical studies on Ajuga species have been performed which have led to the isolation of phytoecdysteroids [11, 12], neo- clerodanediterpenoids [13], phenylethyl glycosides [3], withanolides [2], iridoids and flavonoids [14], and essential oils [15].
Prior to this study, we have isolated 10 compounds; 20-hydroxyecdysone, cyasterone, ajugalactone, makisterone A, and 24-dehydroprecyasterone (phytoecdysteroids), 8-acetylharpagide (iridoid), cis- and trans-melilotoside, lavandulifolioside, leonoside B, and martynoside (phenylethanoid glycosides), from diethyl ether and n-butanolic fractions of Ajuga chamaecistus ssp. tomentella. Cytotoxicity evaluation of some fractions of this plant showed the cytotoxicity of hexane fraction against normal and cancer cell lines. Most of the isolated compounds were inactive in the cytotoxicity assay [16, 17].
The aim of this study was to evaluate antinociceptive effects of oral administration of total water and 80% methanolic extracts and partition fractions of hexane, diethyl ether and n- butanol obtained from methanolic extract of aerial parts of Ajuga chamaecistus ssp. tomentella in an attempt to validate the traditional use of the plants belonging to genus Ajuga.
Methods
Plant material
Aerial parts of Ajuga chamaecistus Ging. ssp. tomentella (Boiss.) Rech. f. were collected from “Sorkhe Hesar”, east of Tehran, Iran, in June 2008 and verified by Prof. G. Amin. A voucher specimen (THE-6697) was deposited in the herbarium of the Department of Pharmacognosy, Faculty of Pharmacy, Tehran University of Medical Sciences, Tehran, Iran.
Methanolic extraction
The air-dried and ground aerial parts of A. chamaecistus ssp. tomentella (250 g) were extracted with methanol 80% (3 × 0.5 L) at room temperature. The solvent was evaporated on a rotary evaporator and in a vacuum oven to give a dark brown extract (45 g). The extract (30 g) was suspended in 80% methanol and partitioned successively between 80% methanol, n-hexane, diethyl ether, and n-butanol. Removal of the solvents with a rotary evaporator resulted in the production of n-hexane, diethyl ether, and n-butanol fractions.
Water extraction
Two hundred and fifty grams of the powdered plant from the aerial parts of A. chamaecistus ssp. tomentella were extracted with distilled water (3 × 0.5 L) at room temperature. The solvent was removed with a rotary evaporator and freeze drying process to give an extract (30 g).
Administration
The extracts were dissolved in normal saline to achieve the working concentrations. Extracts, standard drug (Indomethacin 10 mg/kg), and normal saline were administered by oral gavage. Three doses of 200, 400 and 600 mg/kg of all extracts were examined.
Animals
Male albino mice weighing 25–30 g were obtained from Pasteur institute and housed in groups of 7 with a 12 h light–dark cycle and constant temperature (22°C). Mice were allowed to acclimatize to the laboratory for 30 min before the experiments began. This study was approved by the ethics committee of the Pharmaceutical Science Research Center of TUMS.
Formalin test in mice
Twenty microliters of formalin (0.5%) was injected subcutaneously according to the previous study [18]. The total time (second) spent on licking in response to the injected paw in the acute phase (0–5 min) and chronic phase (15–60 min) after formalin injection was measured as a pain indicator.
Statistical analysis
Results are expressed as mean ± standard error of mean (S.E.M). Statistical differences between the treatment and control groups were evaluated by one-way ANOVA, followed by Newman–Keuls post hoc test. p < 0.05 was considered significant.
Results
In the present study, antinociceptive activity of total water, 80% methanol extracts, and three fractions of methanolic extract from the aerial parts of Ajuga chamaecistus ssp. tomentella were evaluated in a nociception model in mice. All extracts were administered by a gastrointestinal tube at different doses (200, 400, and 600 mg/kg) 30 min before intraplantar injection of formalin (20 μl, 0.5%). The licking time was 40.29 ± 5.76 for indomethacin (10 mg/kg) in the acute phase. There was no significant difference between indomethacin and all treated extracts (Table 1).Figure 1 shows the antinociceptive effects of all extracts at different doses on the chronic phase of pain induction. Results demonstrated that hexane fraction (200 mg/kg), diethyl ether fraction and total water extract at a dose of 400 mg/kg significantly (p < 0.001) affected the duration of licking in the chronic phase, which was comparable to indomethacin (10 mg/kg). The total methanol extract (600 mg/kg) and n-butanolic (600 mg/kg) fraction also exhibited a reduction on the duration of licking in the chronic phase (p < 0.01).Comparison of the antinociceptive activity of all extracts showed that the maximum inhibitory response was obtained with 200 mg/kg of hexane fraction. According to results, there was no significant difference between the analgesic effect of total water extract and hexane fraction at a dose of 400 mg/kg, diethyl ether fraction (600 mg/kg), n-butanol fraction (600 mg/kg), and indomethacin (10 mg/kg) as an NSAID (Figure 2).
Effects of different extracts of Ajuga chamaecistus ssp . tomentella on chronic phase of formalin- induced pain. Different doses of all extracts (200, 400, 600 mg/kg), a) Total water extract, b) Total methanol extract, c) Hexane fraction, d) Diethyl ether fraction, and e) N-Butanol fraction, were administered to mice by oral tube. Control group received normal saline. All extracts of the plant were administered 30 min before formalin injection. Antinociception was recorded 15–60 min (Chronic phase), after formalin injection. Each point is the mean ± S.E.M of at least 7 animals. Control (normal saline), IND (Indomethacin). *p<0.05,** p < 0.01, ***p < 0.001 (as compared with normal saline), #p<0.05, ##p < 0.01, ###p < 0.001 (as compared with Indomethacin).
Comparision of different treatments of Ajuga chamaecistus ssp . tomentella on chronic phase of formalin- induced pain. All samples were administered to mice by oral tube. Control group received normal saline. All extracts of the plant were administered 30 min before formalin injection. Antinociception was recorded 15–60 min (Chronic phase), after formalin injection. Each point is the mean ± S.E.M of at least 7 animals. Control (normal saline), TW (total water), TM (total methanol), NB (n-butanol), HEX (hexane fraction), DEE (diethyl ether fraction). IND (Indomethacin). **p < 0.01, ***p < 0.001 (as compared with normal saline), #p<0.05, ##p < 0.01, ###p < 0.001 (as compared with Indomethacin).
Discussion
The formalin test provides a moderate and continuous pain because of tissue injury in the animal, which is a better approach to clinical conditions than more traditional tests of nociception [19]. Subcutaneous injection of formalin induces two distinctive periods of response. The early phase is explained as a direct stimulation of nociceptive neurons, and the late phase occurs secondary to the inflammatory reactions [20, 21]. Drugs which affect the central nervous system such as opioids inhibit both phases equally while peripherally acting drugs such as aspirin and indomethacin inhibit the late phase [22]. The early phase of response to the formalin test is insensitive to anti-inflammatory drugs [23]. Inflammation in the late phase is due to the release of chemical mediators, such as serotonin, histamine, bradykinin and prostaglandins and at least to some degree, the sensitization of central nociceptive neurons [24].
The results showed that hexane (200 mg/kg), diethyl ether (400 mg/kg), and n-butanol fractions (600 mg/kg) from the methanolic extract (80%) in addition to total water extract (400 mg/kg) significantly decreased the pain related to the late phase (inflammatory agents) of the formalin test. Since the analgesic properties of effective extracts were observed in late phase like NSAIDs, the antinociceptive activities of the extracts are apparently mediated by interactions with inflammatory mediators especially arachidonic acid metabolites. Recently, [9] reported that 70% ethanol extract of whole plants of Ajuga bracteosa showed a significant topical anti-inflammatory activity and a strong in vitro COX-1 and COX-2 inhibitory effect. Among the isolated compounds from this extract, lupulin A (a clerodane diterpenes) exhibited the highest inhibition of COX-1and 6-deoxyharpagide (an iridoid) showed the highest COX-2 inhibition [8]. Cyclooxygenase (COX) catalyzes the biosynthesis of prostaglandin G2 and H2 from arachidonic acid. The cyclooxygenase isoforms (COX-1 and COX-2) are the target of the non-steroidal anti-inflammatory drugs (NSAIDs), which provide therapeutic effects in the treatment of pain, fever, and inflammation [25].
Another herb that is used in treatment of pain and arthritis is Harpagophytum procumbens, commonly known as devil’s claw. The total water extract of this plant possesses anti-inflammatory and analgesic effects by suppressing cyclooxygenase-2 and inducible nitric oxide synthase expressions. Iridoid glycosides such as harpagoside and harpagide are principal constituent of devil’s claw [26, 27]. In our previous study, 8-acethyharpagide, an iridoid glycoside, was isolated in a large amount from the diethyl ether fraction [16]. Many studies have exhibited the biological effects of iridoids such as antioxidant, cytotoxic [9], chemoprotective [28], cardiovascular, hypoglycemic and hypolipidemic properties [29]. Li et al. [30] showed that the iridoid glycosides extract of Lamiophlomis rotate has a significant antinociceptive effect that was better at the second phase than the first phase of the formalin test [30].
Conclusion
In conclusion, hexane and diethyl ether fractions obtained from the methanolic extract 80%, and total water extract of aerial parts of Ajuga chamaecistus ssp. tomentella possess significant and promising antinociceptive properties. The mechanism is supposed to be mediated through the inhibition of endogenous mediators release like prostaglandins. According to the previous study, the isolated compound 8-acethylharpagide could be responsible for the antinociceptive effect of the total water extract and diethyl ether fraction. This study confirmed the traditional use of some Ajuga plants for the treatment of joint pain and other inflammatory diseases.
References
Mozaffarian V: A Dictionary of Iranian Plant Names. 2007, Tehran: Farhangmoaser, 21-22.
Nawaz HR, Malik A, Khan PM, Ahmed S: Ajugin E and F: two withanolides from Ajuga parviflora. Phytochemistry. 1999, 52: 1357-1360. 10.1016/S0031-9422(99)00345-3.
Akbay P, Calis I, Heimann J, Sticher O: Ionon, iridoid and phenylethanoid glycosides from Ajuga salicifolia. Z Naturforsch. 2003, 58c: 177-180.
Hilaly JE, Israili ZH, Lyoussi B: Acute and chronic toxicological studies of Ajuga iva in experimental animals. J Ethnophar. 2004, 91: 43-50. 10.1016/j.jep.2003.11.009.
Israili HZ, Lyoussi B: Ethnopharmacology of the plants of genus Ajuga. Pak J Pharm Sci. 2009, 22: 425-462.
Naghibi F, Mosaddegh M, Mohammadi Motamed S, Ghorbani A: Labiatae family in folk medicine in Iran: from ethnobotany to pharmacology. Iran J Pharm Res. 2005, 2: 63-79.
Hilaly JE, Lyoussi B: Hypoglycemic effect of lyophilized total water extract of Ajuga iva in normal and streptozotocin diabetic rats. J Ethnophar. 2002, 80: 109-113. 10.1016/S0378-8741(01)00407-X.
Gautam R, Jachak SM, Saklani A: Anti-inflammatory effect of Ajuga bracteosa Wall ex Benth. mediated through cyclooxygenase (COX) inhibition. J Ethnophar. 2011, 133: 928-930. 10.1016/j.jep.2010.11.003.
Kuria KAM, Coster S, Muriuki G, Masengo W, Kibwage I, Hoogmartens J, Laekeman GM: Antimalarial activity of Ajuga remota Benth (labiatae) and Caesalpinia volkensii Harms (Caesalpiniaceae): in vitro confirmation of ethnopharmacological use. J Ethnophar. 2001, 74: 141-148. 10.1016/S0378-8741(00)00367-6.
Ono Y, Fukaya Y, Imai S, Yamakuni T: Beneficial effects of Ajuga decumbens on osteoprosis and arthritis. Biol Pharm Bull. 2008, 31: 1199-1204. 10.1248/bpb.31.1199.
Castro A, Coll J, Tandron YA, Pant AK, Mathela C: Phytoecdysteroids from Ajuga macrosperma var. breviflora roots. J Nat Prod. 2008, 71: 1294-1296. 10.1021/np800131f.
Vanyolos A, Simon A, Toth G, Polgar L, Kele Z, Ilku A, Matyus P, Bathori M: C-29 Ecdysteroids from Ajuga reptans. J Nat Prod. 2009, 72: 929-932. 10.1021/np800708g.
Coll J: NMR shift data of neo-clerodane diterpens from the genus Ajuga. Phytochem Anal. 2002, 13: 372-380. 10.1002/pca.671.
Manguro LOA, Ogur JA, Okora DM, Wagal SO, Lemen P: Further flavonol and iridoid glycosides from Ajuga remota. J Asian Nat Prod Res. 2007, 9: 617-629. 10.1080/10286020600979480.
Shams Ardekani MR, Khanavi M, Taheri P, Samadi N, Safaripour E, Salimpour F: The essential oil composition of Ajuga chamaecistus Ging. subsp. tomentella Rech. f. JEOBP. 2010, 13: 45-51.
Sadati N, Ostad SN, Karimian Z, Shams Ardekani MR, Akbarzadeh T, Hadjiakhoondi A, Khanavi M: Phytochemical study and in vitro cytotoxic effect of Ajuga chamaecistus ssp. tomentella. Asian J Chem. 2012, 24: 2871-2874.
Sadati N, Jenett-Siems K, Siems K, Shams Ardekani MR, Hadjiakhoondi A, Akbarzadeh T, Ostad SN, Khanavi M: Major constituents and cytotoxic effects of Ajuga chamaecistus subsp. tomentella. Z Naturforsch. 2012, 67: 275-281.
Khanavi M, Sharifzadeh M, Hadjiakhoondi A, Shafiee A: Phytochemical investigation and anti-inflammatory activity of aerial parts of Stachys byzanthina C Koch. J Ethnophar. 2005, 97: 463-468. 10.1016/j.jep.2004.11.037.
Tjølsen A, Berge O-G, Hunscaar S, Rusland JH, Hole K: The formalin test: an evaluation of method. Pain. 1992, 51 (1): 5-17. 10.1016/0304-3959(92)90003-T.
Dubuisson D, Dennis SG: The formalin test: a quantitative study of the analgesic effect of morphine, meperidine and brain stem stimulation in rats and cats. Pain. 1977, 4: 161-164.
Hunskaar S, Berge OG, Hole K: Dissociation between antinociceptive and anti-inflammatory effects of acetylsalicylic acid and indomethacin in the formalin test. Pain. 1986, 25: 125-132. 10.1016/0304-3959(86)90014-X.
Chen YF, Tsai HY, Wu TS: Anti-inflammatory and analgesic activity from roots of Angelica pubescens. Planta Med. 1995, 61: 2-8. 10.1055/s-2006-957987.
Rosland JH, Tjolsen A, Maehle B, Hole K: The formalin test in mice: effect of formalin concentration. Pain. 1990, 42: 235-242. 10.1016/0304-3959(90)91167-H.
Verma PR, Joharapurkar AA, Chatpalliwar VA, Asnani AJ: Antinociceptive activity of alcoholic extract of Hemidesmus indicus R Br. In mice. J Ethnophar. 2005, 102: 298-301. 10.1016/j.jep.2005.05.039.
Carol A, Rouzer CA, Marnett LJ: Cyclooxygenases: structural and functional insights. JLR. 2009, 50: 529-534.
Jang M-H, Lim S, Han S-M, Park H-J, Shin I, Kim J-W, Kim N-J, Lee J-S, Kim K-A, Kim CJ: Harpagophytum procumbens suppress lipopolysaccharide-stimulated expressions of cyclooxygenase-2 and inducible nitric oxide synthase in fibroblast cell line L929. J Pharmacol Sci. 2003, 93: 367-371. 10.1254/jphs.93.367.
Choubey J, Patel A, Verma MK: Phytotherapy in the treatment of arthritis: a review. IJ PSR. 2013, 4: 2853-2865.
Konoshima T, Takasaki M, Tokuda H, Nishino H: Cancer chemoprotective activity of iridoid glycoside, 8-acetylharpagide, from Ajuga decumbens. Cancer Lett. 2000, 157: 87-92. 10.1016/S0304-3835(00)00479-1.
Bouderbala S, Prost J, Lacaille-Dubois MA, Bouchenak M: Iridoid extracts from Ajuga iva increase the antioxidant enzyme activities in red blood cells of rats fed a cholesterol-rich diet. Nut Res. 2010, 30: 358-365. 10.1016/j.nutres.2010.05.004.
Li M, Shang X, Zhang R, Jia Z, Fan P, Ying Q, Wei L: Antinociceptive and anti-inflammatory activities of iridoid glycosides extract of Lamiophlomis rotate (Benth.) Kudo. Fitoter. 2010, 81: 167-172. 10.1016/j.fitote.2009.08.018.
Acknowledgements
This study was part of a Pharm. D. thesis funded and supported by Tehran University of Medical Sciences (TUMS) (Grant No: 10784-33-02-89). The authors wish to acknowledge the grammatical revision of the manuscript in English carried out by the Consultation Unit, Office of Publications and Scientometrics, Tehran University of Medical Sciences.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
MK: Participated in introducing the plant and designing the study, AD: carried out the antinociception effect, NS: Participated in extraction of the plant and drafting the manuscript, MRS: Helped to revise the manuscript, MS: Participated in design and interpreting of the data. All authors read and approve the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Khanavi, M., Davoodipoor, A.M., Sadati, S.N. et al. Antinociceptive effect of some extracts from Ajuga chamaecistus Ging. ssp. tomentella (Boiss.) Rech. f. aerial parts. DARU J Pharm Sci 22, 56 (2014). https://doi.org/10.1186/2008-2231-22-56
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/2008-2231-22-56