Abstract
Background
Few population-based studies have examined the prevalence of foot pain in the general community. The aims of this study were therefore to determine the prevalence, correlates and impact of foot pain in a population-based sample of people aged 18 years and over living in the northwest region of Adelaide, South Australia.
Methods
The North West Adelaide Health Study is a representative longitudinal cohort study of n = 4,060 people randomly selected and recruited by telephone interview. The second stage of data collection on this cohort was undertaken between mid 2004 and early 2006. In this phase, information regarding the prevalence of musculoskeletal conditions was included. Overall, n = 3,206 participants returned to the clinic during the second visit, and as part of the assessment were asked to report whether they had pain, aching or stiffness on most days in either of their feet. Data were also collected on body mass index (BMI); major medical conditions; other joint symptoms and health-related quality of life (the Medical Outcomes Study Short Form 36 [SF-36]).
Results
Overall, 17.4% (95% confidence interval 16.2 – 18.8) of participants indicated that they had foot pain, aching or stiffness in either of their feet. Females, those aged 50 years and over, classified as obese and who reported knee, hip and back pain were all significantly more likely to report foot pain. Respondents with foot pain scored lower on all domains of the SF-36 after adjustment for age, sex and BMI.
Conclusion
Foot pain affects nearly one in five of people in the community, is associated with increased age, female sex, obesity and pain in other body regions, and has a significant detrimental impact on health-related quality of life.
Similar content being viewed by others
Background
Foot pain has long been recognised as highly prevalent in older people, affecting approximately one in three people aged over 65 years [1–3]. In older people, foot pain is associated with decreased ability to undertake activities of daily living, problems with balance and gait, and an increased risk of falls [4–6]. The prevalence of foot pain in other age-groups, however, has not been as widely studied. The 1990 US National Health Interview Survey of 119,631 people aged over 18 years included a podiatry supplement and found that 24% of the sample reported foot "trouble" [7]. More recently, a random community-based sample of 3,417 people drawn from a general practice register in the UK found that 10% of study participants aged 18 to 80 years had "disabling" foot pain [8], and a community-based postal survey of 16,222 people aged over 55 years found that 18% reported joint pain, swelling and/or stiffness in their feet [9].
Although several studies in relatively small samples of older people have been undertaken [3, 10, 11], the prevalence of foot pain in the general Australian population has never been thoroughly examined. Therefore, the aims of our study were to determine the prevalence of foot pain in a population-based sample, to explore associations between age, sex, major medical conditions, other chronic joint symptoms and foot pain, and to assess the impact of foot pain on health-related quality of life.
Methods
Setting and study population
The North West Adelaide Health Study (NWAHS) was established in 2000 in the North-West region of Adelaide, South Australia [12]. The north-west region of Adelaide comprises approximately half of the population of the city of Adelaide and a third of the population of the state of South Australia. The regions also reflect the demographic profile of the state, covering a broad range of ages and socioeconomic areas. The study was designed in response to a need to assess the prevalence of priority conditions and examine their progression over time in a population-based community-dwelling cohort, to inform policy decisions about health care provision in South Australia.
Participants for Stage 1 of the study (which was conducted between 2000 and July 2003) were recruited randomly from the Electronic White Pages telephone listings and an initial telephone interview was conducted. Those within each household who were last to have a birthday and aged 18 years and over were interviewed and invited to attend a clinic assessment. The overall response rate for an interview and attending the clinic assessment was 49.4%.
Between 2004 and 2006, Stage 2 of the study was conducted. Where possible, all participants were contacted and invited to participate in a Computer Assisted Telephone interview (CATI), a self complete questionnaire and/or a clinic assessment. Stage 2 specifically focused on the collection of information relating to musculoskeletal conditions. Overall, n = 3,206 participants took part in the clinical assessment.
Data collection
As part of the self completed questionnaire, information relating to demographics, self-reported prevalence of diabetes, levels of physical activity using the questions from the Australian National Health Survey [13] (the level of walking moderate or vigorous activity in the last two weeks) and health-related quality of life (the Medical Outcomes Study Short Form 36 (SF-36)[14] were collected. As part of the clinic assessment, height, weight, waist and hip circumference were measured, blood was taken, and as part of the CATI, the self reported prevalence of osteoporosis and cardiovascular disease were determined. Participants were also asked about the presence of knee, hip and back pain ("Have you had pain or aching in your knee/hip/back, either at rest or when moving, on most days for at least a month?").
All participants attending the clinic in Stage 2 were asked: "On most days do you have pain, aching or stiffness in either of your feet?" If they answered yes to this question, they were regarded to have foot pain. Participants who answered "yes" then indicated on a chart (Figure 1) the location of the pain. This was the same figure used in the Framingham Study [15].
Statistical analysis
Data were weighted by age and sex, and probability of selection within the household, to the population of the north west suburbs of Adelaide. All analyses were undertaken using weighted data using SPSS Version 15. Frequencies were used to determine the prevalence of foot pain. Associations between foot pain, age and sex were undertaken using univariate logistic regression analyses to provide odds ratios. The association between foot pain and the remaining factors (BMI, selected chronic diseases and other areas of musculoskeletal pain) were determined using logistic regression analysis and including age and sex with in the model in order to adjust for these factors. As a result the impact of age and sex on the associations were determined. When examining the differences between males and females and age groups, in the proportion with foot pain at particular sites, Chi-square tests were undertaken. The mean health-related quality of life scores were determined using multiple analysis of variance (MANOVA). Age and sex were used as covariates in the analysis to adjust for their effects and the significant differences in scores between those with and without foot pain were determined. A significance level of p < 0.05 was used for all tests.
Results
Sample characteristics
Sample characteristics are shown in Table 1. The characteristics of the NWAHS cohort demonstrate that this is a relatively young, heavy cohort with 38% under 40 years and the mean BMI in the overweight range.
Prevalence and correlates of foot pain
Prevalence
Within the cohort, 558 (17.4%) of participants indicated that they had foot pain on most days over the past month. Of those with foot pain, 349 (62.5%) had bilateral foot pain and 209 (37.5%) had unilateral foot pain.
Foot pain, age, sex and weight
Associations between foot pain and age, sex and weight are shown in Table 2. Females were 40% more likely to report foot pain than males. Increasing age and a BMI classified as obese were factors associated with increased prevalence of foot pain. The presence of increased waist:hip ratio and absolute weight increase (per kg) was also associated with increased prevalence of foot pain.
Foot pain, chronic conditions, physical activity and pain in other regions
Associations between foot pain, chronic conditions, physical activity and pain in other body regions are shown in Table 3. There was an increased prevalence of foot pain amongst those with diabetes, cardiovascular disease and osteoporosis, however this did not reach significance following adjustment for age and sex. Of the participants with foot pain, 20.8% were sedentary compared to 16.4% of those without foot pain, however this difference was not statistically significant (odds ratio = 1.2; 95% confidence interval 0.9 – 1.4, p = 0.16). Foot pain was significantly associated with other joint pain, including knee, hip and back pain (all p < 0.001).
Foot pain location and sex
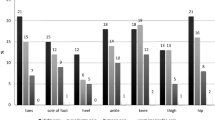
The location of foot pain according to sex is indicated in Table 4. Approximately equal numbers of males and females indicated pain in the forefoot, toes, ball, heel, hind foot and arch, with substantially less at the nails. Females were more likely to report pain in the toes and in the ball of the foot compared to males.
Foot pain location and age
The location of foot pain according to age is shown in Table 5. Pain in the hindfoot region demonstrated a U-shaped relationship with age, with the highest prevalence noted in the 20–34 year and >75 year groups. Pain in the forefoot increased linearly until age 55–64, then levelled out across the remaining age-groups. Pain in the toes increased linearly with age. Pain in the arch was most prevalent in the 20–34 year age-group and decreased with age, with the exception of the >75 year group. Pain in the ball of the foot was similar across all age-groups, and pain in the heel decreased with age. There were insufficient cases to apply inferential statistics to pain in the nails.
SF-36 scores in participants with and without foot pain
Respondents with foot pain had significantly lower scores for all dimensions of the SF-36 compared to those without foot pain (Table 6).
Discussion
Our study provides the first population-based estimates of foot pain in Australia. The findings indicate that approximately one in five people report foot pain, aching or stiffness, with a higher prevalence observed in females, those aged 50 years and over and those classified as obese. However, even in patients aged under the age of 45 years old, at least 10% reported foot pain.
The overall prevalence rate reported in this study is higher than that reported in the Cheshire Foot Pain and Disability Survey in the UK (10%) [8], but lower than that reported in the US National Health Interview Survey (24%) [7] and the Framingham Foot Study (28%) [15]. These differences can be attributed to variations in the definitions of foot pain used in each study. The Cheshire survey used the case definition of the Manchester Foot Pain and Disability Index (MFPDI), which requires participants to have current foot pain, pain lasting at least one month, as well as recording at least one disability item on the questionnaire [16]. As such, the MFPDI probably identifies more severe levels of foot pain than the question we used. In contrast, the US National Health Interview Survey recorded a wide range of foot conditions under the heading of foot "trouble" (including corns and calluses), some of which may not have been symptomatic [7]. The Framingham Foot Study required participants to have pain on "most days" [15].
The associations reported between foot pain and age, female sex and obesity are largely consistent with previous reports. Prevalence studies involving participants across a wide age range have consistently found that older people have much higher rates of foot problems [7, 8, 17], which has been attributed to the cumulative effects of ageing on the integumentary, vascular and musculoskeletal structures of the foot. Similarly, several studies have found that women have a higher prevalence of foot pain than men [8, 11, 18, 19]. This has been attributed to the wearing of shoes with an elevated heel and narrow toe box, which has been shown to be associated with the development of corns, lesser toe deformities and hallux valgus (bunions) [20]. However, the higher prevalence of foot pain may also reflect sex differences in pain tolerance in general, as women are more likely to report musculoskeletal pain and pain interference at other body regions [21]. The association between foot pain and obesity can be partly explained by the significant increase in forces under the foot when walking in those who are obese [22] and the increased tendency for obese people to be flatfooted. Indeed, a recent case-control study indicated that those with chronic heel pain were three times more likely to be obese and four times more likely to have flat feet [23].
Although there was an increased prevalence of foot pain amongst those with self-reported diabetes, cardiovascular disease and osteoporosis, this did not reach significance following adjustment for age and sex. Previous studies have shown that foot problems are more common in older people with multiple chronic diseases [19, 24, 25], however in younger people foot pain is more likely to be related to overuse musculoskeletal conditions associated with physical activity (eg: plantar fasciitis) [7]. Indeed, although a strong linear relationship between foot pain and increased age was observed, this association was revealed to be considerably more complex when foot pain was stratified according to location. While pain in the toes and forefoot generally increased with age, pain in the arch and heel decreased with age, pain in the hindfoot region demonstrated a U-shaped relationship with age, and pain in the ball of the foot was similar across all age-groups. As no clinical assessments were undertaken to ascertain the underlying cause of the pain, the reasons for these variable patterns are uncertain. However, it could be speculated that foot pain in younger age-groups is more likely to be musculoskeletal in origin, whereas foot pain in older people is more likely to be caused by toe deformities, corns and calluses.
Irrespective of the underlying cause, our results indicate that foot pain has a significant impact on health-related quality of life. Participants who reported foot pain demonstrated lower scores on the SF-36, and this association persisted after adjusting for age, sex and BMI. Although significant associations between the presence of foot problems, self-reported disability [26] and inability to perform activities of daily living [4, 18, 19] have been reported in older people, the association reported between foot pain and reduced health-related quality of life across such a broad age range is a novel finding. Of particular interest, those with foot pain demonstrated lower scores for not only the physical and bodily pain components of the SF-36, but also the social functioning and mental health components. This finding suggests that the impact of foot pain extends beyond localised pain and encompasses much broader aspects of health-related quality of life.
The major strength of this study is the use of a population-based sample with excellent response rates over a broad age range. However, it is acknowledged that the study has several limitations. Firstly, we defined foot pain according to a single question rather than using foot-specific questionnaires, such as the Manchester Foot Pain and Disability Index [3, 16] or Foot Health Status Questionnaire [27]. Secondly, we were unable to examine the participants' feet in the study. We asked participants to indicate on a diagram (see Figure 1) the location of the foot pain, but did not ask which specific types of foot problem each participant had, or undertake any measurements of foot deformity. However, studies conducted in older people have indicated that only a small proportion of clinically-determined foot problems are reported as symptomatic [15, 28, 29]. Stronger associations have been reported for foot pain and pain in other regions of the body [9, 11, 24, 29, 30], suggesting that foot pain may develop as part of a generalised form of osteoarthritis or systemic pain condition.
Conclusion
This study indicates that although it has received relatively little attention in the epidemiological literature, foot pain is highly prevalent, even in young people, and has a significant detrimental impact on health-related quality of life. As the population ages and the prevalence of obesity increases, there is likely to be an increasing prevalence of foot pain. Further research is required to determine best practice models for managing foot pain and to determine whether the provision of foot care services, such as podiatry, are sufficient to meet this increasing demand.
References
Black JR, Hale WE: Prevalence of foot complaints in the elderly. Journal of the American Podiatric Medical Association. 1987, 77 (6): 308-311.
Dunn JE, Link CL, Felson DT, Crincoli MG, Keysor JJ, McKinlay JB: Prevalence of foot and ankle conditions in a multiethnic community sample of older adults. American Journal of Epidemiology. 2004, 159: 491-498. 10.1093/aje/kwh071.
Menz HB, Tiedemann A, Kwan MMS, Plumb K, Lord SR: Foot pain in community-dwelling older people: an evaluation of the Manchester foot pain and disability index. Rheumatology. 2006, 45: 863-867. 10.1093/rheumatology/kel002.
Bowling A, Grundy E: Activities of daily living: changes in functional ability in three samples of elderly and very elderly people. Age and Ageing. 1997, 26: 107-114. 10.1093/ageing/26.2.107.
Menz HB, Morris ME, Lord SR: Foot and ankle characteristics associated with impaired balance and functional ability in older people. Journal of Gerontology. 2005, 60A (12): 1546-1552.
Menz HB, Morris ME, Lord SR: Foot and ankle risk factors for falls in older people: a prospective study. Journal of Gerontology. 2006, 61A (8): M866-870.
Greenberg L, Davis H: Foot problems in the US. The 1990 National Health Interview survey. Journal of the American Podiatric Medical Association. 1993, 83: 475-483.
Garrow AP, Silman AJ, Macfarlane GJ: The Cheshire foot pain and disability survey: a population survey assessing prevalence and associations. Pain. 2004, 110: 378-384. 10.1016/j.pain.2004.04.019.
Keenan AM, Tennant A, Fear J, Emery P, Conaghan PG: Impact of multiple joint problems on daily living tasks in people in the community over age fifty-five. Arthritis and Rheumatism. 2006, 55: 757-764. 10.1002/art.22239.
Munro BJ, Steele JR: Foot-care awareness. A survey of persons aged 65 years and older. Journal of the American Podiatric Medical Association. 1998, 88 (5): 242-248.
Menz HB, Morris ME: Determinants of disabling foot pain in retirement village residents. Journal of the American Podiatric Medical Association. 2005, 95: 573-579.
Grant JF, Chittleborough CR, Taylor AW, DalGrande E, Wilson DH, Phillips PJ, Adams RJ, Price K, Gill T, Ruffin RE: The North West Adelaide Health Study: detailed methods and baseline segmentation of a cohort for selected chronic diseases. Epidemiological Perspectives and Innovations. 2006, 3: 4-10.1186/1742-5573-3-4.
AustralianBureauofStatistics: National Health Survey: Users Guide (4363.0.55.001). 2001, Canberra , Australian Bureau of Statistics
Ware JE, Snow KK, Kosinski M, Gandek B: SF-36 Health Survey Manual and Interpretation Guide. 1993, Boston , New England Medical Centre, The Health Institute
Hannan MT, McLennan CE, Rivinus MC, Hillstrom HJ, Lu M, Broe KE, Kiel DP: Population-based study of foot disorders in men and women from the Framingham Study. Arthritis Rheum. 2006, 54 ((Suppl)): S497-
Garrow AP, Papageorgiou AC, Silman AJ, Thomas E, Jayson MIV, Macfarlane GJ: Development and validation of a questionnaire to assess disabling foot pain. Pain. 2000, 85: 107-113. 10.1016/S0304-3959(99)00263-8.
Brodie BS, Rees CL, Robins DJ, Wilson AFJ: Wessex Feet: a regional foot health survey, Volume I: The survey. The Chiropodist. 1988, 43: 152-165.
Benvenuti F, Ferrucci L, Guralnik JM, Gangemi S, Baroni A: Foot pain and disability in older persons: an epidemiologic survey. Journal of the American Geriatrics Society. 1995, 43: 479-484.
Gorter KJ, Kuyvenhoven MM, deMelker RA: Nontraumatic foot complaints in older people. A population-based survey of risk factors, mobility, and well-being. Journal of the American Podiatric Medical Association. 2000, 90: 397-402.
Menz HB, Morris ME: Footwear characteristics and foot problems in older people. Gerontology. 2005, 51: 346-351. 10.1159/000086373.
Thomas E, Peat G, Harris L, Wilkie R, Croft PR: The prevalence of pain and pain interference in a general population of older adults: cross-sectional findings from the North Staffordshire Osteoarthritis Project (NorStOP). Pain. 2004, 110: 361-368. 10.1016/j.pain.2004.04.017.
Birtane M, Tuna H: The evaluation of plantar pressure distribution in obese and non-obese adults. Clinical Biomechanics. 2004, 19: 1055-1059. 10.1016/j.clinbiomech.2004.07.008.
Irving DB, Cook JL, Young MA, Menz HB: Obesity and pronated foot type may increase the risk of chronic plantar heel pain: a matched case-control study. BMC Musculoskelet Disord. 2007, 8: 41-10.1186/1471-2474-8-41.
Leveille SG, Guralnik JM, Ferrucci L, Hirsch R, Simonsick E, Hochberg MC: Foot pain and disability in older women. American Journal of Epidemiology. 1998, 148: 657-665.
Barr ELM, Browning C, Lord SR, Menz HB, Kendig H: Foot and leg problems are important determinants of functional status in community dwelling older people. Disability and Rehabilitation. 2005, 27: 917-923. 10.1080/09638280500030506.
Keysor JJ, Dunn JE, Link CL, Badlissi F, Felson DT: Are foot disorders associated with functional limitation and disability among community-dwelling older adults?. Journal of Aging and Health. 2005, 17: 734-752. 10.1177/0898264305280998.
Bennett PJ, Patterson C, Wearing S, Baglioni T: Development and validation of a questionnaire designed to measure foot-health status. J Am Podiatr Med Assoc. 1998, 88: 419-428.
Cartwright A, Henderson G: More trouble with feet - a survey of the foot problems and chiropody needs of the elderly. 1986, London , Department of Health and Social Security, HMSO
Badlissi F, Dunn JE, Link CL, Keysor JJ, McKinlay JB, Felson DT: Foot musculoskeletal disorders, pain, and foot-related functional limitation in older persons. Journal of the American Geriatrics Society. 2005, 53: 1029-1033. 10.1111/j.1532-5415.2005.53315.x.
Chen J, Devine A, Dick IM, Dhaliwal SS, Prince RL: Prevalence of lower extremity pain and its association with functionality and quality of life in elderly women in Australia. Journal of Rheumatology. 2003, 30: 2689-2693.
Acknowledgements
This study received financial support from a grant from Human Services Research and Innovation Program (large projects) 2000–01, Department of Health, South Australia. HBM is currently a National Health and Medical Research Council fellow (Clinical Career Development Award, ID: 433049). We would also like to acknowledge the contribution of the NWAHS staff and participants.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
HBM is Editor-in-Chief of the Journal of Foot and Ankle Research. It is journal policy that editors are removed from the peer review and editorial decision making processes for papers they have co-authored.
Authors' contributions
CLH, TKG and AWT conceived the study design, TKG conducted the statistical analysis, CLH and HBM interpreted the results and drafted the manuscript, and all authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Hill, C.L., Gill, T.K., Menz, H.B. et al. Prevalence and correlates of foot pain in a population-based study: the North West Adelaide health study. J Foot Ankle Res 1, 2 (2008). https://doi.org/10.1186/1757-1146-1-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1757-1146-1-2