Abstract
Background
Foot pain has been shown to be prevalent across all age groups. The presence of foot pain may reduce mobility and impact on the ability to undertake activities of daily living. The aim of this study was to determine factors that are predictive of foot pain in a community based sample of the general population.
Methods
This study analysed data from the North West Adelaide Health Study, a cohort study located in the northwestern suburbs of Adelaide, South Australia. Data were obtained between 2004–2006 and 2008–2010, using a self-completed questionnaire, computer assisted telephone interviewing, and a clinical assessment. The sensitivity, specificity and positive predictive values of variables were determined and generalised linear models ascertained the variables associated with the highest relative risk of self-reporting foot pain in 2008–2010 based on the data obtained in 2004–2006.
Results
The prevalence of foot pain in 2004–2006 was 14.9 % (95 % CI 13.6–16.4) and in 2008–2010, 29.9 % (95 % CI 27.5–32.5). Variables with the highest sensitivity were: female sex, ever having back pain, self-reported arthritis, body mass index (BMI) classified as obese and having foot pain in 2004–2006, while most variables demonstrated high specificity. Those with the highest risk of reporting foot pain in 2008–2010 were those with depressive symptoms, self-reported arthritis, high BMI, self-reported upper limb pain and foot pain (in general or in specific regions of the foot) in 2004–2006.
Conclusion
Foot pain is common in the general population and those with the greatest risk of foot pain potentially represent a high level of chronicity and potential burden on the health system. Addressing the factors that predict foot pain, as well as the provision of targeted messages to highlight the importance of managing foot pain, may help reduce the impact on the population.
Similar content being viewed by others
Background
Foot pain has long been recognised as being widespread in older people, affecting approximately one in three people aged over 65 years [1, 2]. However, foot pain has also been shown to be highly prevalent among younger adults [3]. A recent systematic review demonstrated that 24 % of community dwelling participants aged 45 years and over reported frequent foot pain (pain on most days) [4].
Several potential risk factors for foot pain have been identified from cross-sectional studies, including obesity [5], osteoarthritis [6], diabetes [7], and depression [8]. Alcohol consumption and smoking may both have an impact on the feet, although few studies have directly explored this. Alcohol consumption has been shown to be associated with single or multi-site pain in men [9] and also with chronic widespread pain in both men and women [10]. Smoking has been shown to generally have a negative effect on the musculoskeletal system particularly with regard to bone mineral density [11], although variable associations have been shown with regard to smoking and the presence of osteoarthritis [12].
Physical inactivity has been identified as a risk factor for chronic musculoskeletal pain [13] and it is also recognised that activity has a beneficial effect on pain and disability [14]. However, it is also possible that those with musculoskeletal pain are less likely to undertake activity [15], particularly if pain is present in the foot. Arthritis is also a factor associated with foot pain, in particular rheumatoid arthritis and osteoarthritis of the midfoot and/or the first metatarsophalangeal joint [16]. In fact, over 35 % in a sample of patients with rheumatoid arthritis identified that foot pain was the presenting symptom [17]. It is of note, that pain in multiple sites has been shown by Keenan et al. [18] to be more common than joint pain at a single site. Gill et al. [19] have also shown previously that incident, recurrent and resolved shoulder pain were all associated with self-reported pain in various other joints.
Although these findings suggest a link between a range of possible risk factors and foot pain, their cross-sectional study designs cannot infer causation. Therefore, the aim of this study was to determine the predictive value of these variables, with regard to future foot pain by utilising prospective cohort data obtained from the North West Adelaide Health Study in 2004–2006 and 2008–2010.
Methods
The North West Adelaide Health Study (NWAHS) is a representative longitudinal study of over 4000 randomly selected adults aged 18 years and over at the time of recruitment from the north-west region of Adelaide, South Australia. The sample region represents approximately half of the metropolitan area (total population of approximately 1.2 million) and almost one-third of the population in South Australia (population of approximately 1.6 million), which has the second highest population of older people among all of the Australian states and territories [20]. The aim of the study is to provide self-reported data that has been longitudinally measured to inform strategies and policies to prevent, detect and manage a range of chronic conditions [21]. The study commenced with Stage 1, in 1999 to 2003, Stage 2 was conducted between 2004 and 2006 and Stage 3 was conducted between 2008 and 2010. Ethical approval for each stage of the study was obtained from the Human Research Ethics committee of The Queen Elizabeth Hospital, Adelaide, South Australia and all participants provided written informed consent.
Data collection
Participant information was obtained from a Computer Assisted Telephone Interview (CATI), a self-complete questionnaire and a clinical assessment at each stage [21, 22]. The original cohort of participants was 4056, with 3205 (81.5 % of the eligible sample) participating in all three data collections (the CATI survey, self-complete questionnaire and clinical assessment) in Stage 2 and 2487 (67.0 % of the eligible sample) completing these assessments in Stage 3. Foot pain related data were collected in Stage 2 and Stage 3, and these stages are the focus of this study.
Stage 2 variables
In 2004–2006, smoking, physical activity and alcohol consumption were determined from the responses to the self-completed questionnaire. The level of physical activity was determined from descriptions of physical activity type and time over a 2 week time frame [23]. Smoking was determined using standard questions relating current smoking and the frequency and alcohol consumption was determined from questions based on the National Heart Foundation Risk Factor Prevalence Study undertaken in 1989 [24].
Depression was determined from the CATI response to the Centre for Epidemiological Studies in Epidemiology Depression questionnaire (CES-D) [25]. Participants were asked if they been told by a doctor that they had arthritis. If the response was in the affirmative, participants were then asked what type of arthritis they had. Participants were also asked if they had used podiatry services in the last 12 months. The presence of pain and/or stiffness in the shoulder, hip, knee and back was determined by asking participants if they had ever had pain/stiffness in those areas on most days for at least a month. The presence of hand pain was determined by asking if participants had had pain, aching or stiffness on most days for at least a month.
The presence of diabetes was determined from a self-reported doctor diagnosis of diabetes and/or a fasting plasma glucose level of greater than or equal to 7.0 mmol/L. Age was calculated from the participants’ date of birth and the date participants attended their clinical assessment. During the clinical assessment height and weight were measured with standardised protocols. A wall mounted stadiometer measured height to the nearest 0.5 cm and weight was measured using calibrated scales to the nearest 0.1 kg. BMI was then calculated using the following formula [26]: weight (kg)/height (m2).
Foot pain
In 2004–2006, participants were asked as part of the telephone questionnaire, “On most days, do you have pain, aching or stiffness in either of your feet?" In addition, as part of the clinical assessment, which included measurements such as blood pressure, lung function and taking of blood samples, participants were shown a diagram of the foot and asked to identify areas that they had pain, that is, hindfoot, forefoot, toes, nails, arch, ball and heel. The diagram was based on the Framingham Foot Study, 2002–2008 [27]. In 2008–2010, participants were asked as part of the self-complete questionnaire “Over the past month, have you had pain, aching or stiffness in either of your feet on most days?” This question was used to more specifically determine the presence of current pain.
Data weighting
In Stage 1, data were weighted by region (western and northern health regions), age group, sex and probability of selection in the household to the Australian Bureau of Statistics 1999 Estimated Resident Population and the 2001 Census data. Weighting was undertaken to reflect the population of interest and to correct for potential non-response bias in which some groups of respondents may be over- or under-represented. Weighting variables were also created for Stage 2 and 3 using the 2004 and 2009 Estimated Resident Population for South Australia respectively, and also incorporating participation in the three components (CATI, self-complete questionnaire, clinic), whilst retaining the original weight from Stage 1 in the calculation. All analyses in this paper, where applicable, are weighted to the population of the northern and western suburbs of Adelaide.
Statistical analyses
Statistical analyses were conducted using STATA version 13 (StataCorp, College Station, TX, USA). The weighted prevalence (using the “svy” estimators and “pweight” as the weighting variable) of foot pain obtained from Stage 2 and Stage 3 was determined and the frequency of each of the variables measured as part of the Stage 2 assessment, for those with and without foot pain on most days in the last month, was determined. These variables were then used as predictors for the presence of foot pain as determined at Stage 3 and thus, tests aimed at examining how well variables predicted the presence of foot pain were used. The sensitivity (probability that the associated factor is present when foot pain is present), specificity (probability that the associated factor is not present when foot pain is not present), positive predictive value of each of the predictor variables (the probability that foot pain is present given that the associated factor is present) and the area under the Receiver Operating Characteristic (ROC) curve (the summary of the performance of each variable in terms of the ability to predict foot pain) were all determined. An area under the ROC curve equal to one indicates that a variable perfectly predicts those at risk of the outcome whereas a value of 0.5 represents a predictor that is no better than chance at predicting the outcome of interest. The area under the ROC curve was calculated using predictors as binary variables as this is the most common occurrence in clinical practice, however is must be noted that generally continuous variables are more appropriate to use for ease of interpretability.
Generalised linear models using the binary outcome variable of presence of foot pain/no foot pain on most days in the past month were used with the “svy” estimators and weighted data to determine the relative risks (RR) of each of the predictors in association with the outcome variable. Multivariable models were created with all relevant predictor variables included. The participants reporting toe and nail pain were combined (due to the small number of participants reporting the presence of toe pain). In addition, the areas of joint pain were combined. Hand and shoulder pain were defined as upper limb pain and hip and knee pain were defined as lower limb pain. Back pain remained a separate variable. In total, four separate multivariable models were created with adjustment for all possible predictors.
Results
The prevalence of foot pain in 2004–2006 was 14.9 % (95 % CI 13.6–16.4) and 29.9 % (95 % CI 27.5–32.5) in 2008–2010. Table 1 shows the proportion of those with foot pain in the last month by each of the 2004–2006 characteristics. In particular, foot pain was higher among females, older people, those with symptoms of depression and those categorised as obese.
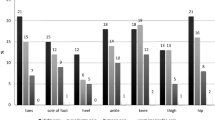
Table 2 shows the sensitivity, specificity, positive predictive value and area under the ROC (95 % CI) curve for the presence of foot pain in 2008–2010 using each of the predictor variables from 2004 to 2006. Those with the highest sensitivity, that is, the ability to correctly identify those with foot pain were: sex (female), self-reported arthritis, BMI classified as obese, ever having had back pain/stiffness and having reported foot pain in 2004–2006. The variable with the lowest specificity was sex (female) while all other variables were able to strongly identify those without foot pain. In general, foot pain and the specific areas of foot pain all had the highest positive predictive values. Values of the area under the ROC curve were all similar, indicating that most of the variables were no better than chance at predicting foot pain. Those with the highest value were general foot pain and self-reported arthritis. However, it is also of note that these were the variables with the highest positive predictive value, that is, those factors most likely to be present when foot pain it present.
Multivariable analysis was undertaken, with generalised linear models used to determine the RR of each of the factors in association with foot pain on most days in the last month compared to not having foot pain on most days. Four models were undertaken, the first using the reported prevalence of foot pain only and the second using the location of foot pain (Table 3). Models 3 and 4 repeated Models 1 and 2, respectively, but included the areas of joint pain variables (upper limb, lower limb, back pain) (Table 4). The factors associated with the presence of foot pain in 2008–2010 were: symptoms of depression, self-reported arthritis, BMI classified as obese, foot pain (general and specific areas) and reporting having experienced shoulder and/or hand pain.
Discussion
The results of this study demonstrate that foot pain is a common condition within the general population. While there has been some recent work attempting to identify phenotypes using radiographic information for those with foot osteoarthritis [28] there has been little work, particularly across all age groups, attempting to identify the predictors of generalised foot pain. This study used a questionnaire and a set of clinical measures to collect specific data as part of a cohort study to determine whether these variables predicted the presence of foot pain at a later stage.
The variables with the highest positive predictive values: BMI, depression, areas of foot pain, self-reported arthritis and podiatry use were those most strongly associated with the occurrence of foot pain on most days in the past month in the multivariable model and indicate that there are likely to be specific characteristics concomitant with foot pain, even though these variables have a relatively low ability to predict the occurrence of foot pain (the highest area under the ROC curve being 70.37 for ball of the foot pain). Addressing these associated factors are consequently still likely to impact on the overall prevalence of foot pain.
Those with symptoms of depression and classified as obese according to their BMI in 2004–2006 were at higher risk of reporting foot pain in 2008–2010. There have been strong cross-sectional associations demonstrated between foot pain and BMI [5, 29], which is likely to be biomechanical in nature due to increased pressure under the feet. Gay et al. [30] have also demonstrated, using longitudinal data, that foot joint pain was highly prevalent among middle aged women and that a high BMI was predictive of foot pain, independent of age. In this study, the probability of being obese was 41.8 % if participants reported foot pain on most days in the last month and when examined in the multivariable model, the risk of reporting a high BMI remained. However, recent work has also identified that fat mass and the association with biochemical markers may play a greater role in the development of foot pain than BMI [29, 31, 32] and further examination of these issues may be important over the longer term.
An association between foot pain and depression has previously been shown [32] and the development of major depressive disorders may occur as a consequence of inflammation [33]. Inflammatory markers are associated with fat mass and thus may impact on the development of depression. There is also a relationship between obesity itself and depression [34]. These factors combined are likely to have an effect on the association between depression and foot pain.
It is not surprising that those reporting arthritis or foot pain in 2004–2006, whether this is general foot pain or by location, were at a higher risk of reporting foot pain in 2008–2010. Multiple joint problems such as those that occur with arthritis have been shown to be more common than single joint problems [18]. Hill et al. [3] have also demonstrated that foot pain in the North West Adelaide cohort is also associated with reports of pain in other joints. Gill et al. [19] demonstrated that shoulder pain was associated with pain in other joint areas, which may be as a result of arthritis. The apparent existence of foot pain over a period of time provides an indication of chronicity and burden. Chronic musculoskeletal pain is associated with longer-term declines in overall health and physical mobility [35]. Efforts should be made to determine if earlier intervention can limit these declines, which are not only characterised by painful feet, but by the negative sequelae associated with physical inactivity [36].
There are three main limitations of this study. Firstly, the foot pain questions were non-specific, lacked a clinical diagnosis, and did not involve objective measures such as x-rays. Secondly, the sample has been obtained from the metropolitan area of a city in Australia, and thus the factors predictive of foot pain may be different in other populations. Thirdly, the focus of the study is on predictive factors, and as such causation cannot be inferred. Strengths of this study are the use of a longitudinal cohort with questions relating to foot pain asked at two time points, the level of detail collected on the location of foot pain and the data available over a 6–7 year time period. More than 2000 participants provided responses to the foot pain questions in 2004–2006 and 2008–2010 and a broad range of covariates were available for analysis. To our knowledge there are no previous longitudinal studies of foot pain from a population-based sample with the same breadth of covariates conducted in Australia.
Conclusion
Foot pain affects a significant proportion of the population over a period of time. Those reporting depression, arthritis, previous foot pain, upper limb pain and a high BMI were at greater risk of reporting foot pain on most days in the last month. However, the sensitivity, specificity and positive predictive values of variables to predict the presence of foot pain varied greatly. Those with the greatest risk of having foot pain were those with arthritis and previous foot pain, which indicates a high level of chronicity and subsequent burden on the health system. Addressing BMI, depression and general joint health with the use of targeted messages to highlight the impact of foot pain on daily functioning may be of benefit in order to reduce the burden of foot pain on the population.
Abbreviations
BMI, body mass index; CATI, computer assisted telephone interviewing; CES-D, Centre for Epidemiological Studies in Depression questionnaire; CI, confidence interval; NWAHS, North West Adelaide Health Study; ROC, receiver operating characteristic; RR, relative risk
References
Dunn J, Link C, Felson D, Crincoli MG, Keysor JJ, McKinlay JB. Prevalence of foot and ankle conditions in a multiethnic community sample of older adults. Am J Epidemiol. 2004;159:491–8.
Menz H, Tiedemann A, Kwan M, Plumb K, Lord SR. Foot pain in community-dwelling older people: an evaluation of the Manchester Foot Pain and Disability Index. Rheumatology. 2006;45:863–7.
Hill C, Gill T, Menz H, Taylor AW. Prevalence and correlates of foot pain in a population-based study: the North West Adelaide Health Study. J Foot Ankle Res. 2008;1:2.
Thomas MJ, Roddy E, Zhang W, Menz HB, Hannan MT, Peat GM. The population prevalence of foot and ankle pain in middle and old age: a systematic review. Pain. 2011;152:2870–80.
Butterworth PA, Landorf KB, Smith SE, Menz HB. The association between body mass index and musculoskeletal foot disorders: a systematic review. Obes Rev. 2012;13:630–42.
Menz HB, Morris ME. Determinants of disabling foot pain in retirement village residents. J Am Podiatr Med Assoc. 2005;95:573–9.
Gorter KJ, Kuyvenhoven MM, de Melker RA. Nontraumatic foot complaints in older people. A population-base survey of risk factors, mobility and well-being. J Am Podiatr Med Assoc. 2000;90:397–402.
Awale A, Dufour AB, Katz P, Menz HB, Hannan MT. Severity of foot pain is linked to the prevalence of depressive symptoms. Arthritis Care Res. 2016;68:871-6.
Leveille SG, Zhang Y, McMullen W, Kelly-Hayes M, Felson DT. Sex differences in musculoskeletal pain in older adults. Pain. 2005;116:332–8.
Macfarlane GJ, Beasley M. Alcohol consumption in relation to risk and severity of chronic widespread pain: Results from a UK population-based study. Arthritis Care Res. 2015;67:1297–303.
Abate M, Vanni D, Pantalone A, Salini V. Cigarette smoking and musculoskeletal disorders. Muscles Ligaments Tendons J. 2013;3:63–9.
Felson DT, Zhang Y. Smoking and osteoarthritis: a review of the evidence and its implications. Osteoarthritis Cartilage. 2015;23:331–3.
Sluka KA, O’Donnell JM, Danielson J, Rasmussen LA. Regular physical activity prevents development of chronic pain and activation of central neurons. J Appl Physiol (1985). 2013;114:725–33.
Uthman OA, van der Windt DA, Jordan JL, Dziedzic KS, Healey EL, Peat GM, et al. Exercise for lower limb osteoarthritis: Systematic review incorporating trial sequential analysis and network meta-analysis. BMJ. 2013;347:f5555.
Stubbs BB, Patchay S, Soundy A, Schofield P. The avoidance of activities due to fear of falling contributes to sedentary behaviour among community-dwelling older adults with chronic musculoskeletal pain: a multisite observational study. Pain Med. 2014;15:1861–71.
Rao S, Riskowski J, Hannan MT. Musculoskeletal conditions of the foot and ankle: Assessments and treatment options. Best Pract Res Clin Rheumatol. 2012;26:345–68.
Otter SJ, Lucas K, Springett K, Moore A, Davies K, Cheek L, et al. Foot pain in rheumatoid arthritis prevalence, risk factors and management: an epidemiological study. Clin Rheumatol. 2010;29:255–71.
Keenan AM, Tennant A, Fear J, Emery P, Conaghan P. Impact of multiple joint problems on daily living tasks in people in the community over age fifty-five. Arthritis Rheum. 2006;55:757–64.
Gill TK, Shanahan EM, Taylor AW, Buchbinder R, Hill CL. Shoulder pain in the community: an examination of associative factors using a longitudinal cohort study. Arthritis Care Res. 2013;65:2000–7.
Australian Bureau of Statistics. 3235.0 - Population by Age and Sex, Regions of Australia, 2011. Available at: http://www.abs.gov.au/ausstats/abs@.nsf/Products/3235.0~2011~Main+Features~South+Australia?OpenDocument. Accessed 1 Dec 2016.
Grant JF, Taylor AW, Ruffin RE, Wilson DH, Phillips PJ, Adams RJ, et al. Cohort profile: The North West Adelaide Health Study (NWAHS). Int J Epidemiol. 2009;38:1479–86.
Grant JF, Chittleborough CR, Taylor AW, Dal Grande E, Wilson DH, Phillips PJ, et al. The North West Adelaide Health Study: detailed methods and baseline segmentation of a cohort for selected chronic diseases. Epidemiol Perspect Innov. 2006;3:4.
Australian Bureau of Statistics. National Health Survey: Users Guide, 2001. Cat no 4363.0.55.001. Canberra: ABS; 2003.
Australian Institute of Health and Welfare and National Heart Foundation. Risk factor prevalence study: Survey no 3. Canberra: AIHW; 1989.
Radloff LS. The CES-D Scale: a self report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401.
World Health Organization. Obesity: Preventing and Managing the Global Epidemic. Geneva: WHO; 2000.
Dufour AB, Broe KE, Nguyen US, Gagnon DR, Hillstrom HJ, Walker AH, et al. Foot pain: is current or past shoewear a factor? Arthritis Rheum. 2009;61:1352–8.
Rathod T, Marshall M, Thomas MJ, Menz HB, Myers HL, Thomas E, et al. Investigation of potential phenotypes of foot osteoarthritis: Cross-sectional analysis from the Clinical Assessment Study of the Foot. Arthritis Care Res. 2016;68:217–27.
Tanamas SK, Wluka AE, Berry P, Menz HB, Strauss BJ, Davies-Tuck M, et al. Relationship between obesity and foot pain and its association with fat mass, fat distribution, and muscle mass. Arthritis Care Res. 2012;64:262–8.
Gay A, Culliford D, Leyland K, Arden NK, Bowen CJ. Associations between body mass index and foot joint pain in middle-aged and older women: A longitudinal population-based study. Arthritis Care Res. 2014;66:1873–9.
Walsh TP, Gill TK, Evans AM, Yaxley A, Shanahan EM, Hill CL. The association of fat mass and adipokines with foot pain in a community cohort. Arthritis Care Res. 2016;68:526–33.
Butterworth PA, Menz HB, Urquhart DM, Cicuttini FM, Landorf KB, Pasco JA, et al. Fat mass is associated with foot pain in men. J Rheumatol. 2016;43:138–43.
Krishnadas R, Cavanagh J. Depression: an inflammatory illness? J Neurol Neurosurg Psychiatry. 2012;83:495–502.
Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BWJH, et al. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010;67:220–9.
Eggermont LH, Leveille SG, Shi L, Kiely DK, Shmerling RH, Jones RN, et al. Pain characteristics associated with the onset of disability in older adults: The maintenance of balance, independent living, intellect, and zest in the Elderly Boston Study. J Am Geriatr Soc. 2014;62:1007–16.
Lee IM, Shiroma EJ, Lobelo F, Puska P, Blair SN, Katzmarzyk PT, et al. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. 2012;380:219–29.
Acknowledgements
Hylton Menz is currently a National Health and Medical Research Council Senior Research Fellow (2012–2017, ID 1020925).
Funding
Not applicable.
Availability of data and materials
Data from this study form part of the NWAHS. As this is an ongoing cohort study, these data are available on application to the chief investigators. Details are available at: http://health.adelaide.edu.au/pros/data/nwahs/.
Authors’ contributions
All authors contributed to the planning of the paper. TKG undertook the analysis and prepared the first draft. HBM, KBL, JBA, AWT and CLH provided critical review of the paper and the analysis. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Ethics approval for the study was obtained from the Human Research Ethics committee of The Queen Elizabeth Hospital, Adelaide, South Australia and all participants provided written informed consent.
Declarations
HBM is Editor in Chief of the Journal of Foot and Ankle Research. It is journal policy that editors are removed from the peer review and editorial decision making process for the papers that they have co-authored.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Gill, T.K., Menz, H.B., Landorf, K.B. et al. Predictors of foot pain in the community: the North West Adelaide health study. J Foot Ankle Res 9, 23 (2016). https://doi.org/10.1186/s13047-016-0150-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13047-016-0150-9