Abstract
Background
Previous reports suggest an as yet unidentifiable subset of patients with plasmacytoma will progress to myeloma. The current study sought to establish the risk of developing myeloma and determine the prognostic factors affecting the progression of disease.
Methods
Patients with plasmacytoma diagnosed between 1973 and 2005 were identified in the SEER database(1164 patients). Patient demographics and clinical characteristics, treatment(s), cause of death, and survival were extracted. Kaplan-Meier, log-rank, and Cox regression were used to analyze prognostic factors.
Results
The five year survival among patients initially diagnosed with plasmacytoma that later progressed to multiple myeloma and those initially diagnosed with multiple myeloma were almost identical (25% and 23%; respectively). Five year survival for patients with plasmacytoma that did not progress to multiple myeloma was significantly better (72%). Age > 60 years was the only factor that correlated with progression of disease (p = 0.027).
Discussion
Plasmacytoma consists of two cohorts of patients with different overall survival; those patients that do not progress to systemic disease and those that develop myeloma. Age > 60 years is associated with disease progression. Identifying patients with systemic disease early in the treatment will permit aggressive and novel treatment strategies to be implemented.
Similar content being viewed by others
Introduction
Plasmacytoma results from clonal proliferation of plasma cells that are identical to plasma cells of myeloma on both the cyotologic and immunophenotypic levels. Plasmacytoma can be subclassified as osseous disease or extraosseous tumor [1–7]. The clinical presentation of these diseases represent different groups of patients in terms of location, tumor progression, and overall survival rate [8]; however, they share many of the biologic features of other plasma cell disorders [1, 9]. Skeletal plasmacytoma is characterized clinically by a radiolytic lesion involving any part of the skeleton, a clonal plasma cell infiltrate and an absence of disseminated bone marrow involvement.
Local radiotherapy and alternatively surgery are treatment options yielding adequate local control [7, 10]. Despite local treatment efforts, 50-60% of patients with plasmacytoma progresses to myeloma [2, 11, 12]. It has been reported that skeletal plasmacytoma is known to progress more frequently to multiple myeloma than extraskeletal disease [2, 11, 13]. Most of the basis for the natural history of plasmacytoma is derived from reports emanating from single institutions. Knobel et al and Kilciksiz et al reported multi-center experiences but the small number of patients limited the statistical power of these studies[10, 14]. Recently Dores et al reported incidence and survival for patients with plasmacytoma, extraskeletal disease and myeloma from the SEER database [15]. In this study there was no analysis of prognostic factors associated with neither progression of cases initially diagnosed as plasmacytoma into myeloma nor an assessment of local disease control.
The current manuscript attempts to ascertain the impact of local treatment on disease progression in patients with skeletal plasmacytoma. Specifically, the study sought to establish the incidence of development of myeloma and the treatment outcomes of patients initially diagnosed with plasmacytoma. Furthermore, the study seeks to compare clinical parameters in cases of plasmacytoma not progressing to systemic disease with those developing into myeloma to identify prognostic factors. In order to answer these questions, the SEER Database was utilized as a source of patient data. Previously the population based SEER database has been used to describe the outcomes for breast, colorectal, prostate, lung, ovarian, sarcomas and neuroectodermal cancers and has been validated as to the accuracy [16–21]. The current study investigates the impact of local treatment on skeletal plasmacytoma and its progression to myeloma and demonstrates that a younger patient population has localized disease which does not progress to systemic disease.
Methods
The Surveillance, Epidemiology, and End-Results (SEER) Program of the National Cancer Institute (NCI) was established as a direct result of the National Cancer Act 1971. Currently SEER collects data from 17 population based registries covering approximately 26% of the US population. It is the only comprehensive source of population based data in the U.S. that includes the stage of cancer at the time of diagnosis and follow-up of all patients for survival data. In addition, each registry collects data on patient demographics, primary tumor site and morphology, and first course of treatment (occurring within 4 months of diagnosis) [22–34]. The SEER program is currently regarded as the standard of quality among cancer registries around the world with case completeness of 98% [35].
The SEER database was used to identify all cases of skeletal plasmacytoma diagnosed from 1973-2005 using International Classification of Disease for Oncology, 3rd Edition (ICD-O-3) [36]. We used primary site of lesion to specifically select for cases involving bone. A total of 1164 patients were identified and information regarding patient demographics, clinical characteristics, treatment related characteristics were extracted (if provided within 4 months of diagnosis), and survival time (months) until death or loss to follow-up. Percentages were based on available data for each individual variable. Patients with missing data were excluded from each respective univariate and multivariate analysis.
Patients' age was converted to a categorical variable (0-29, 30-59, >60) for the purpose of analysis. The appendicular skeleton included long and short bones of limbs and associated joints, and the scapula. Axial skeleton included vertebra, ribs, sternum, clavicle and associated joints, bones of skull, face and associated joints, mandible, and pelvic bones. Staging categories of local, regional, and distant were described in SEER according to AJCC staging system [37]. Since, skeletal plasmacytoma by definition is a localized disease process we excluded the cases (5.6% of total) designated as 'distant'. Year of diagnosis was categorized in four categorical variables: 1973-1975, 1976-1985, 1986-1995, and 1996-2005. Results reported herein are in compliance with the Health Insurance Portability and Accountability Act of 1996.
Incidence rates were age adjusted and normalized using the 2000 US Standard population [38]. Statistical analysis was performed using SPSS version 17.0 (SPSPSS Inc., Chicago, IL). Chi-square test was used to make correlations between categorical variables. Overall and disease-specific survival from the time of initial diagnosis to the date of last contact (or the date of death) was calculated using the Kaplan-Meier method. The effects of demographic, clinical, pathological, and treatment variables were tested using the log-rank test for categorical values. A multivariate analysis was carried out for determination of independent prognostic factors using the Cox proportional hazards model. All prognostic factors found to be significant in the univariate analysis, namely gender, stage, primary site, size, and surgical therapy were included in a multivariate analysis.
Results
A total of 1164 cases of plasmacytoma are included in the SEER Data-base from 1973-2005. Nearly three quarter of the cases (74.7%) were diagnosed during the most recent decade, 1996-2005 reflecting the geographic expansion of the data collection effort during these years. The demographic and clinical characteristics of the entire patient cohort are summarized in Table 1. Most patients were older than 60 years at diagnosis (63.7% of the cases). Males comprised 61.9% of patients; race was predominantly Caucasian (84.1%) and ethnicity predominantly non-Hispanic (89.7%), respectively. Among all the cases identified, 5.2% of the tumors were designated as 'distant' at the time of diagnosis and thus were excluded from further analysis. Staging information was available for 51.4% of the cases that were subjected to analysis. Surgical resection alone was performed in 34.6% of patients, solely radiation therapy administered in 53.9%, and combined surgery and radiation in 0.9%. Approximately 10.5% of patients received no therapy for local disease control (dns).
The overall incidence for plasmacytoma was 0.3462/100,000 in 2005; similar to what has been reported by Dores et al [15]. Afro-American to Caucasian Incidence Rates Ratio to develop plasmacytoma was found to be approximately 1.30 (dns). Five and ten year overall survival for patients with skeletal plasmacytoma is summarized in Table 2. Kaplan-Meier prediction of survival of patients with plasmacytoma is affected by race with "races other than Caucasians" and Afro-Americans faring significantly better than Caucasians (p < 0.001). Since other races made up only 4.2% of the entire patient cohort, thus this result should be interpreted with caution. There was no significant difference in outcome between Caucasians and Afro-Americans.
Patients diagnosed at age < 60 years (Figure 1) had a significantly better 5 year survival (90% for patients aged 0-29 years & 80% for patients 30-59 years) when compared to patients diagnosed at age >60 years (5 year survival 45%) (p < 0.001). Patients with skeletal plasmacytoma had an overall survival of 57% at 5 years and 37% at 10 years. Females have a significantly lower 5 and 10 year survival than males (5 year survival 54% v/s 59% for males (p-value = 0.008). Patients with a solitary lesion carried significantly better prognosis with a 5 year survival of 59% as compared to 36% for patients with more than 2 lesions (p = 0.032). There was no significant difference in survival between patients with a single or two lesions (p-value = 0.28). There was no significant difference in 5 year survival outcome for axial lesions (58%) as compared to appendicular lesions (52%) (p = 0.24).
Patients undergoing surgery fared no better than patients without resection (5 year survival 59% and 56% respectively, p = 0.29). In contrast, administration of radiation therapy was associated with an improvement in survival (5 year survival of 60% among patients with radiation therapy as compared to 46% without any radiation therapy, p < 0.001). Further analysis revealed that use of any local disease control modality, either surgery or radiation therapy was associated with better outcomes as compared to the absence of any local disease control (p < 0.001; Figure 2). Surgery and radiation were found to be equally effective in local disease control. Use of both modalities was not associated with any significant survival advantage. No significant improvement in survival could be observed over time when stratified by decade for the past two decades (p = 0.19).
Table 3 illustrates a step-wise multivariate analysis employing the Cox proportional hazard model to ascertain the independent significant variables for the entire cohort. The parameters age > 60 years (p < 0.001), race other than Caucasians and Afro-Americans (p < 0.05), and absence of radiation therapy (p < 0.001) were all independent predictors of lower overall survival.
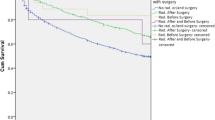
In order to compare the plasmacytoma as a localized disease with cases progressing to myeloma, the survival and cause of death information were extracted regarding all the cases of multiple myeloma from 1973-2005 (54,244 cases). We found that there was no significant difference in 5 year survival among patients initially diagnosed with multiple myeloma and those initially labeled as plasmacytoma who subsequently later progressed to multiple myeloma (5 year survival of 25% and 23% respectively). In contrast, 5 year survival for patients with plasmacytoma who did not progress to multiple myeloma was significantly better with (p < 0.001 5 year survival = 72%), Figure 3. Some of the more frequent causes of death in patients with plasmacytoma not progressing to myeloma included Diseases of Heart (4.5%) and Cerebrovascular Diseases (1.0%) as would be expected for patients in this age group.
Analysis of statistically significant factors on multivariate analysis did not reveal any prognostic factors significantly associated with progression of plasmacytoma into a systemic disease other than age (Table 4). Association between Age >60 years and development of myeloma approached significance (p = 0.027).
In order to assess the potential ascertainment bias: the potential bias of falsely diagnosing patients with myeloma as plasmacytoma patients, a cross-tabulation was performed between cause of death and different treatment groups. Our analysis reveals 27 of 60 patients with no attempt at local control, died of myeloma. This ratio of progression to myeloma was similar in other treatment groups (dns) with chi-square not revealing any statistical significance.
Discussion
The current study is the first to demonstrate the impact of local treatment on skeletal plasmacytoma using a population based registry. It further demonstrates the differences in treatment related outcomes among patients diagnosed with plasmacytoma not progressing to myeloma, those that progressed to myeloma. Epidemiological studies comparing SEER areas to non-SEER areas in the U.S. conclude that their age and sex distributions are comparable except that SEER areas tended to be more affluent and more urban than non-SEER areas [34]. When compared to NPCR and USCS, incidence rates for all sites combined were lower in SEER. But for category of interest: 'Bones and Joints', the differences were small: 0.6 in SEER versus 0.8 per 100,000 in NPCR among Black males was the largest reported difference [34]. Despite adequate local control with radiotherapy and/or surgery, cause of death in 59% of the patients initially diagnosed with plasmacytoma was progression to myeloma. Similarly, Soutar et al. reported >75% progression to multiple myeloma for skeletal plasmacytoma [12]. In the current study it cannot be determined that what is the absolute rate of progression to multiple myeloma among patients diagnosed with plasmacytoma, since some of the patients died of other causes and hence are censored. Despite these limitations, we can confidently say that rate of progression to Multiple Myeloma among cases of plasmacytoma is at least 59% and may be slightly greater than this number.
Also, the 5 year survival for patients diagnosed with multiple myeloma and those diagnosed as plasmacytoma initially but who subsequently developed myeloma later on, were almost identical (Figure 3). This may suggest an underlying misdiagnosis for cases of myeloma as plasmacytoma. In order to overcome this problem, the use of MRI in initial staging of plasma cell neoplasm has been advocated by some authors [39] while others have reported conflicting evidence [14]. We tried to address this issue by determining any significant association of the independent predictors of overall survival among patients with plasmacytoma and subsequent development of multiple myeloma. None of the factors considered revealed any significant association with development of myeloma, other than age. Age > 60 years was significant with a p = 0.027 (Table 4). Conflicting evidence for age as a predictor of progression to myeloma has been reported in literature, with some studies supporting this observation [3, 40–42] while others have found no association [43–45]. Kilciksiz et al. identified age as an independent prognostic factor for progression to myeloma [10].
Another controversy highlighted in literature involves the fate of patients with plasmacytoma in regards to disease progression. While some have demonstrated a significant portion of patients free of disease after 5 and 10 years, others believe in the inevitability of progression for all patients [41, 43, 46, 47]. The current study clearly demonstrates that there is a cohort of plasmacytoma patients that do not progress to myeloma demonstrate as high as 72% 5-year survival rate (Figure 3).
Surgery alone has been proposed as the best treatment option for extramedullary plasmacytomas [48], but conflicting evidence has also been provided in the literature [14]. Uni- and multivariate analysis in the current study revealed no survival advantage associated with surgery alone for skeletal plasmacytoma (Table 2). This result reflects a selection bias: relatively smaller number of patients underwent surgical resection as a local treatment option. Radiotherapy was employed for a majority of cases. Further analysis, after stratification based on local treatment option clearly demonstrates that use of either option, i.e. surgical therapy or radiotherapy is associated with an improvement in survival in skeletal disease. Neither of the treatment options showed a survival benefit over the other nor similarly employment of both modalities of local control did not further improve survival.
Limitations of the current study include lack of any information on specific chemotherapy regimens or any other adjuvant therapy in the SEER Database. Thus we are unable to comment directly on survival benefit conferred upon by the use of chemotherapy or efficacy of a particular regimen in a particular subset of patients. Similarly, no information regarding any medical history, radiological studies or serological work up is provided in the database limiting our analysis on diagnostic accuracy of MRI, and prognostic significance of absence of myeloma protein, anemia, hypercalcemia, renal insufficiency and stability of M-protein. Accuracy of staging information can be a potential pitfall in all studies based on database. Another issue associated with the reported data in SEER is the potential bias of falsely labeling myeloma patients as plasmacytoma patients. The results of bone marrow aspirate are not reported in SEER, and in clinical practice treatment decisions are usually made based on this parameter. This raises the suspicion of marrow involvement >30% among those not receiving the local therapy. Our analysis reveals no correlation between any treatment groups and 'cause of death'. We also attempted to address the controversy regarding progression to myeloma. In clinical practice, the evaluation regarding progression to myeloma is carried out after a specified time interval. SEER does not report the time for evaluation regarding progression; we assessed the outcome using 'cause of death' information. The time to progression cannot be assessed.
Conclusion
Despite the above mentioned limitations such as retrospective nature of data, lack of information about chemotherapy or serological or radiological investigations; the current study addresses some of the controversies in disease progression and impact of local treatment for plasmacytoma using a large populations based well validated national database. The current study also reiterates the need of better understanding of the disease process of plasma cell neoplasm and the inclusion of molecular markers in the database.
References
Dimopoulos MA, Hamilos G: Solitary bone plasmacytoma and extramedullary plasmacytoma. Curr Treat Options Oncol. 2002, 3: 255-259. 10.1007/s11864-002-0015-2.
Dimopoulos MA, Moulopoulos LA, Maniatis A, Alexanian R: Solitary plasmacytoma of bone and asymptomatic multiple myeloma. Blood. 2000, 96: 2037-2044.
Ozsahin M, Tsang RW, Poortmans P, Belkacemi Y, Bolla M, Dincbas FO, Landmann C, Castelain B, Buijsen J, Curschmann J: Outcomes and patterns of failure in solitary plasmacytoma: a multicenter Rare Cancer Network study of 258 patients. Int J Radiat Oncol Biol Phys. 2006, 64: 210-217.
Tong D, Griffin TW, Laramore GE, Kurtz JM, Russell AH, Groudine MT, Herron T, Blasko JC, Tesh DW: Solitary plasmacytoma of bone and soft tissues. Radiology. 1980, 135: 195-198.
Galieni P, Cavo M, Avvisati G, Pulsoni A, Falbo R, Bonelli MA, Russo D, Petrucci MT, Bucalossi A, Tura S: Solitary plasmacytoma of bone and extramedullary plasmacytoma: two different entities?. Ann Oncol. 1995, 6: 687-691.
Jaffe ES, Harris NL, Stein H, Vardiman JW: World Health Organization Classification of Tumours: Pathology and Genetics of Tumours of Hematopoietic and Lymphoid Tissues. 2001, IARC Press, Lyon
Knowling MA, Harwood AR, Bergsagel DE: Comparison of extramedullary plasmacytomas with solitary and multiple plasma cell tumors of bone. J Clin Oncol. 1983, 1: 255-262.
Hussong JW, Perkins SL, Schnitzer B, Hargreaves H, Frizzera G: Extramedullary plasmacytoma. A form of marginal zone cell lymphoma?. Am J Clin Pathol. 1999, 111: 111-116.
Aalto Y, Nordling S, Kivioja AH, Karaharju E, Elomaa I, Knuutila S: Among numerous DNA copy number changes, losses of chromosome 13 are highly recurrent in plasmacytoma. Genes Chromosomes Cancer. 1999, 25: 104-107. 10.1002/(SICI)1098-2264(199906)25:2<104::AID-GCC5>3.0.CO;2-C.
Kilciksiz S, Celik OK, Pak Y, Demiral AN, Pehlivan M, Orhan O, Tokatli F, Agaoglu F, Zincircioglu B, Atasoy BM: Clinical and prognostic features of plasmacytomas: a multicenter study of Turkish Oncology Group-Sarcoma Working Party. Am J Hematol. 2008, 83: 702-707. 10.1002/ajh.21211.
Liebross RH, Ha CS, Cox JD, Weber D, Delasalle K, Alexanian R: Clinical course of solitary extramedullary plasmacytoma. Radiother Oncol. 1999, 52: 245-249. 10.1016/S0167-8140(99)00114-0.
Soutar R, Lucraft H, Jackson G, Reece A, Bird J, Low E, Samson D: Guidelines on the diagnosis and management of solitary plasmacytoma of bone and solitary extramedullary plasmacytoma. Clin Oncol (R Coll Radiol). 2004, 16: 405-413.
Mayr NA, Wen BC, Hussey DH, Burns CP, Staples JJ, Doornbos JF, Vigliotti AP: The role of radiation therapy in the treatment of solitary plasmacytomas. Radiother Oncol. 1990, 17: 293-303. 10.1016/0167-8140(90)90003-F.
Knobel D, Zouhair A, Tsang RW, Poortmans P, Belkacemi Y, Bolla M, Oner FD, Landmann C, Castelain B, Ozsahin M: Prognostic factors in solitary plasmacytoma of the bone: a multicenter Rare Cancer Network study. BMC Cancer. 2006, 6: 118-10.1186/1471-2407-6-118.
Dores GM, Landgren O, McGlynn KA, Curtis RE, Linet MS, Devesa SS: Plasmacytoma of bone, extramedullary plasmacytoma, and multiple myeloma: incidence and survival in the United States, 1992-2004. Br J Haematol. 2009, 144: 86-94. 10.1111/j.1365-2141.2008.07421.x.
Gutierrez JC, Franceschi D, Koniaris LG: How many lymph nodes properly stage a periampullary malignancy?. J Gastrointest Surg. 2008, 12: 77-85. 10.1007/s11605-007-0251-7.
Hodgson N, Koniaris LG, Livingstone AS, Franceschi D: Gastric carcinoids: a temporal increase with proton pump introduction. Surg Endosc. 2005, 19: 1610-1612. 10.1007/s00464-005-0232-4.
Perez EA, Livingstone AS, Franceschi D, Rocha-Lima C, Lee DJ, Hodgson N, Jorda M, Koniaris LG: Current incidence and outcomes of gastrointestinal mesenchymal tumors including gastrointestinal stromal tumors. J Am Coll Surg. 2006, 202: 623-629. 10.1016/j.jamcollsurg.2006.01.002.
Jawad MU, Extein J, Min ES, Scully SP: Prognostic Factors for Survival in Patients with Epithelioid Sarcoma: 441 Cases from the SEER Database. Clin Orthop Relat Res. 2009,
Jawad MU, Cheung MC, Min ES, Schneiderbauer MM, Koniaris LG, Scully SP: Ewing sarcoma demonstrates racial disparities in incidence-related and sex-related differences in outcome: an analysis of 1631 cases from the SEER database, 1973-2005. Cancer. 2009, 115: 3526-3536. 10.1002/cncr.24388.
Giuffrida AY, Burgueno JE, Koniaris LG, Gutierrez JC, Duncan R, Scully SP: Chondrosarcoma in the United States (1973 to 2003): an analysis of 2890 cases from the SEER database. J Bone Joint Surg Am. 2009, 91: 1063-1072. 10.2106/JBJS.H.00416.
Bach PB, Guadagnoli E, Schrag D, Schussler N, Warren JL: Patient demographic and socioeconomic characteristics in the SEER-Medicare database applications and limitations. Med Care. 2002, 40 (IV): 19-25.
Cooper GS, Virnig B, Klabunde CN, Schussler N, Freeman J, Warren JL: Use of SEER-Medicare data for measuring cancer surgery. Med Care. 2002, 40 (IV): 43-48.
Earle CC, Nattinger AB, Potosky AL, Lang K, Mallick R, Berger M, Warren JL: Identifying cancer relapse using SEER-Medicare data. Med Care. 2002, 40 (IV): 75-81.
Gloeckler Ries LA, Reichman ME, Lewis DR, Hankey BF, Edwards BK: Cancer survival and incidence from the Surveillance, Epidemiology, and End Results (SEER) program. Oncologist. 2003, 8: 541-552. 10.1634/theoncologist.8-6-541.
Hayat MJ, Howlader N, Reichman ME, Edwards BK: Cancer statistics, trends, and multiple primary cancer analyses from the Surveillance, Epidemiology, and End Results (SEER) Program. Oncologist. 2007, 12: 20-37. 10.1634/theoncologist.12-1-20.
Merrill RM, Dearden KA: How representative are the surveillance, epidemiology, and end results (SEER) program cancer data of the United States?. Cancer Causes Control. 2004, 15: 1027-1034. 10.1007/s10552-004-1324-5.
Petrelli NJ: SEER data: it can be thought provoking, but where do we go from here?. Ann Surg Oncol. 2007, 14: 2173-2174. 10.1245/s10434-007-9453-1.
Potosky AL, Warren JL, Riedel ER, Klabunde CN, Earle CC, Begg CB: Measuring complications of cancer treatment using the SEER-Medicare data. Med Care. 2002, 40 (IV): 62-68.
Schrag D, Bach PB, Dahlman C, Warren JL: Identifying and measuring hospital characteristics using the SEER-Medicare data and other claims-based sources. Med Care. 2002, 40 (IV): 96-103.
Virnig BA, Warren JL, Cooper GS, Klabunde CN, Schussler N, Freeman J: Studying radiation therapy using SEER-Medicare-linked data. Med Care. 2002, 40 (IV): 49-54.
Warren JL, Harlan LC, Fahey A, Virnig BA, Freeman JL, Klabunde CN, Cooper GS, Knopf KB: Utility of the SEER-Medicare data to identify chemotherapy use. Med Care. 2002, 40 (IV): 55-61.
Warren JL, Klabunde CN, Schrag D, Bach PB, Riley GF: Overview of the SEER-Medicare data: content, research applications, and generalizability to the United States elderly population. Med Care. 2002, 40 (IV): 3-18.
Wingo PA, Jamison PM, Hiatt RA, Weir HK, Gargiullo PM, Hutton M, Lee NC, Hall HI: Building the infrastructure for nationwide cancer surveillance and control--a comparison between the National Program of Cancer Registries (NPCR) and the Surveillance, Epidemiology, and End Results (SEER) Program (United States). Cancer Causes Control. 2003, 14: 175-193. 10.1023/A:1023002322935.
NCI: Surveillance, Epidemiology and End Results (SEER) Program. 2008, National Cancer Institute
IACR: International Classification of Diseases for Oncology. 2000
AJCC Cancer Staging Manual. 2002
Li Y, Yang D, Chen J: [Primary small cell carcinoma of thyroid with solitary plasmacytoma of the hyoid bone: report of a case]. Zhonghua Bing Li Xue Za Zhi. 2008, 37: 351-353.
Moulopoulos LA, Dimopoulos MA, Weber D, Fuller L, Libshitz HI, Alexanian R: Magnetic resonance imaging in the staging of solitary plasmacytoma of bone. J Clin Oncol. 1993, 11: 1311-1315.
Bataille R, Sany J, Serre H: [Apparently isolated plasmacytoma of bone. Clinical and prognostic data. 114 cases and review of literature (author's transl)]. Nouv Presse Med. 1981, 10: 407-411.
Frassica DA, Frassica FJ, Schray MF, Sim FH, Kyle RA: Solitary plasmacytoma of bone: Mayo Clinic experience. Int J Radiat Oncol Biol Phys. 1989, 16: 43-48.
Tsang RW, Gospodarowicz MK, Pintilie M, Bezjak A, Wells W, Hodgson DC, Stewart AK: Solitary plasmacytoma treated with radiotherapy: impact of tumor size on outcome. Int J Radiat Oncol Biol Phys. 2001, 50: 113-120.
Bolek TW, Marcus RB, Mendenhall NP: Solitary plasmacytoma of bone and soft tissue. Int J Radiat Oncol Biol Phys. 1996, 36: 329-333. 10.1016/S0360-3016(97)85732-X.
Holland J, Trenkner DA, Wasserman TH, Fineberg B: Plasmacytoma. Treatment results and conversion to myeloma. Cancer. 1992, 69: 1513-1517. 10.1002/1097-0142(19920315)69:6<1513::AID-CNCR2820690633>3.0.CO;2-X.
Shih LY, Dunn P, Leung WM, Chen WJ, Wang PN: Localised plasmacytomas in Taiwan: comparison between extramedullary plasmacytoma and solitary plasmacytoma of bone. Br J Cancer. 1995, 71: 128-133.
Delauche-Cavallier MC, Laredo JD, Wybier M, Bard M, Mazabraud A, Le Bail Darne JL, Kuntz D, Ryckewaert A: Solitary plasmacytoma of the spine. Long-term clinical course. Cancer. 1988, 61: 1707-1714. 10.1002/1097-0142(19880415)61:8<1707::AID-CNCR2820610832>3.0.CO;2-N.
Wiltshaw E: The natural history of extramedullary plasmacytoma and its relation to solitary myeloma of bone and myelomatosis. Medicine (Baltimore). 1976, 55: 217-238. 10.1097/00005792-197605000-00002.
Alexiou C, Kau RJ, Dietzfelbinger H, Kremer M, Spiess JC, Schratzenstaller B, Arnold W: Extramedullary plasmacytoma: tumor occurrence and therapeutic concepts. Cancer. 1999, 85: 2305-2314. 10.1002/(SICI)1097-0142(19990601)85:11<2305::AID-CNCR2>3.0.CO;2-3.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
MUJ carried out analysis and wrote the manuscript.
SPS conceived the idea and was the senior author in preparation of manuscript.
Both authors have read and approve the manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Jawad, M.U., Scully, S.P. Skeletal Plasmacytoma: Progression of disease and impact of local treatment; an analysis of SEER database. J Hematol Oncol 2, 41 (2009). https://doi.org/10.1186/1756-8722-2-41
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1756-8722-2-41