Abstract
Background
In this study, a total of 426 human faecal samples were examined for the presence of Entamoeba histolytica, Entamoeba dispar, Entamoeba moshkovskii infection via a combination of microscopic examination and nested polymerase chain reaction (PCR) targeting 16S ribosomal RNA of Entamoeba species.
Methods
Faecal sample were collected from 426 participants in five rural villages in Peninsular Malaysia. The faecal samples were processed by direct wet smear and formalin ethyl acetate concentration technique followed by iodine staining and examined via microscopy for the presence of Entamoeba species and other intestinal parasites. Microscopically positive samples for Entamoeba species cysts were further characterized using a Nested Polymerase Chain Reaction (Nested-PCR) targeting 16S-like ribosomal RNA gene. The data entry and analysis was carried out using the SPSS software (Statistical Package for the Social Sciences) program for Windows version 17 (SPSS, Chicago, IL, USA).
Results
Based on single faecal examination, overall prevalence of Entamoeba infection was 17.6% (75/426). Females (19.1%) were more commonly infected compared to males (15.9%). Comparison by age groups showed that adults (23.9%) had higher infection rates than children (15.3%). The PCR results showed that 52 out of 75 microscopy positive samples successfully generated species-specific amplicons. The infection with E. histolytica (75.0%; 39/52) was the most common, followed by E. dispar (30.8%; 18/52) and E. moshkovskii (5.8%; 3/52). Of these, 33 (63.5%) were shown to contain only E. histolytica, 10 (19.2%) contained E. dispar and 3 (5.8%) contained only E. moshkovskii. Mixed infection with E. histolytica and E. dispar was found in 6 (11.5%) samples.
Conclusions
The present study essentially emphasized the benefit of molecular techniques in discriminating the pathogenic Entamoeba species from the non-pathogenic for accurate diagnosis and better management of amoebiasis. The presence of E. moshkovskii is of great public health concern as it was the first time it has been reported in Malaysia.
Similar content being viewed by others
Background
The genus Entamoeba comprises six species, namely Entamoeba histolytica, E. dispar, E. moshkovskii, E. coli, E. hartmanni and E. polecki that live in the human intestinal lumen. Infections with Entamoeba species can result in either a harmless colonization of the intestine or invasion of the colonic wall and damage of other host tissues such as liver, lung and brain. Most of the Entamoeba species are commensal parasites and do not cause human disease. Amoebiasis which is caused by Entamoeba histolytica is a global health problem as it is responsible for more than 100,000 deaths per year and is the second leading cause of global death due to protozoa after malaria [1–3]. Major symptoms of amoebiasis are abdominal pain, diarrhea, nausea, vomiting and flatulence. This infection is more preponderant in children compared to adults [4] and is commonly found in tropical and subtropical areas.
It has been reported that 10% of the world’s population are infected with Entamoeba species, in which pathogenic E. histolytica constitute 10% of these infections and the remaining 90% are infected by non-pathogenic E. dispar [5]. However, a recent study highlighted the existence of another species of Entamoeba known as E. moshkovskii which can also cause infection among humans [6]. E. histolytica, E. dispar and E. moshkovskii are morphologically identical but are different biochemically and genetically [6–8]. Although a previous study showed E. moshkovskii to be a non-pathogenic parasite, intestinal symptoms including diarrhea and other gastrointestinal disorders in individuals infected with this species have been reported [8–10]. This, however, has been rebutted by Al-Harthi and Jamjoon (2007) [11] who claimed that E. moshkovskii has never been associated with any disease. This may indicate that perhaps humans are a true host for this putatively free-living amoeba and are not just transiently infected. Therefore, the true prevalence of E. dispar and E. moshkovskii infections need to be investigated in order to determine their significant pathogenic potential in humans.
Traditionally, Entamoeba infections are diagnosed through microscopic examination of fresh or fixed faecal samples. However, very often E. histolytica cysts and trophozoites cannot be morphologically differentiated from E. dispar and E. moshkovskii through microscopic examination. Only when ingested red blood cells are present in trophozoites of E. histolytica, the ability to distinguish them from those of E. dispar and E. moshkovskii becomes easier. Recently, sensitive and specific serological and molecular techniques that are able to distinguish E. histolytica from E. dispar have been developed [10, 12–20]. These include the detection of E. histolytica antigen using an enzyme-linked immunosorbent assay (ELISA) [16, 17, 19], the detection of E. histolytica by monoclonal antibodies of E. histolytica that specifically recognize E. histolytica antigen [12, 15] and the use of the polymerase chain reaction (PCR) to amplify amoebic DNA [10, 13, 14]. More current approaches include the discrimination of E. histolytica E. dispar and E. moshkovskii by a simultaneous detection using multiplex nested PCR [18, 20].
In Malaysia, intestinal parasitic infections (IPIs) including Entamoeba infections are more prevalent in rural areas especially among aboriginal communities compared to urban areas [21–23]. A recent study conducted by Ngui et al . (2011) among communities living in rural areas of Malaysia, showed that 10.2% of the participants were infected with Entamoeba . Another study showed that the infection rate of Entamoeba in rural communities in Malaysia was 21.0% [24]. Other local studies which include aboriginal groups reported prevalence ranging from 9.4% to 18.5% [25, 26]. However, these prevalence rates were based on microscopic examination which could not differentiate between E. histolytica E. dispar and E.moshkovskii infections.
In order to avoid unnecessary treatment of individuals with non-pathogenic Entamoeba species, it is important to discriminate these species from the pathogenic E. histolytica [1]. Additionally, there is also a need for simpler and better identification of these infections, not only for diagnostic purposes and care management, where E. dispar and E. moshkovskii infected individuals could be treated unnecessarily with antiamoebic chemotherapy, but also for a better understanding of the epidemiology of these parasites in the human population. Within this context, we conducted this study to determine the prevalence of Entamoeba species and the true E. histolytica, E. dispar and E. moshkovskii infections in human faecal samples using molecular techniques.
Methods
Study area and population
The present study was carried out from 2009 to 2011 in five rural villages, namely Pos Iskandar (102.65°E longitude, 3.06°N latitude), Sungai Koyan (101.63°E longitude, 4.25°N latitude), Sungai Bumbun (101.42°E longitude, 2.85°N latitude), Bukit Serok (102.82°E longitude, 2.91°N latitude) and Sungai Layau (104.10°E longitude, 1.53°N latitude) (Figure 1). In brief, the villages are inhabited by members of the indigenous ethnic groups. Each village has a small population and the number of residents in each village is estimated to be 80 to 100 inhabitants. They live in deprived circumstances where overcrowding, poor environmental sanitation, low levels of education and poor provision of safe water are widespread. Although provisions of basic facilities are provided by local authorities, most of them could not afford to pay their monthly utility bills leading to the termination of water supplies. Therefore, rivers located adjacent to the village remain their main source of water for domestic needs such as drinking, cooking, bathing and washing clothes. The condition of the surrounding environment of the village is also generally poor with limited provision of latrine facilities therefore encouraging defecation in and around bushes or nearby rivers. Children usually defecate indiscriminately around their houses without parental supervision. Cats, dogs and poultry are the most common domestic animals. Most of these domestic animals are left to roam freely within the village and were observed to defecate in the surrounding property of their owners. The villagers have very close contact with these animals, even sharing food from the same plate with them.
Consent, sample collection and laboratory procedures
The study protocol was approved by the Ethics Committee of the University of Malaya Medical Centre, Malaysia (UMMC; MEC Ref. No. 824.11). Before sample collection, an oral briefing to describe the objectives and methodology of the study was given to the participants by the investigator. Their consent was taken either in written form (signed) or verbally followed by thumb prints (for those who were illiterate) or their parents/guardians (on behalf of their children) after which pre-labeled plastic containers for faecal collection were handed out to all participants. Their ability to recognize their names was checked.
The filled containers were collected on the following day. The fresh faecal samples were stored at ambient temperature and transferred to the laboratory within 2–4 hours post-collection. Upon arrival at the laboratory, the samples were preserved in 2.5% potassium dichromate and kept at 4°C until further analysis. The faecal samples were processed by direct wet smear and formalin ethyl acetate sedimentation technique followed by iodine staining and examined via microscopy for the presence of Entamoeba species and other intestinal parasites. Microscopically positive samples for Entamoeba species cysts were further characterized using a molecular technique.
Extraction of entamoeba genomic DNA
DNA was extracted from microscopically positive faecal samples using PowerSoil® DNA Isolation Kit (Mo Bio, cat. no. 12888–100, CA, USA) according to the manufacturer’s instructions. Briefly, approximately 0.2 to 0.3 g of faecal sample was added into the PowerBead Tube® followed by incubation at 70°C for 10 minutes with the presence of cell lysis and disruption agent provided in the kit. Afterwards, homogenization and cell lysis procedure of the faecal sample were completed by mechanical shaking (vortexing) using MO BIO Vortex Adapter (MO BIO, cat. no. 13000-V1). The extracted DNA was stored at −20°C until required for PCR amplification.
Nested polymerase chain reaction (nested-PCR)
Nested PCR targeting 16S-like ribosomal RNA gene was used to genetically characterize E. histolytica, E. dispar and E. moshkovskii according to Que and Reed (1991) [27]. Primary PCR for the detection of Entamoeba genus used forward primer E-1 (5’-TAA GAT GCA GAG CGA AA-3’) and reverse primer E-2 (5’-GTA CAA AGG GCA GGG ACG TA-3’). Control samples without DNA (DNase free water, Sigma Cat. no. W4502) and with Entamoeba species genomic DNA (positive control) were included in each PCR run. The PCR was carried out in a 25 μl volume with the final mix containing 10× PCR buffer, 1.25 mM dNTPs, 25 mM MgCl2, 10 pmole of each primer, 2.5 U of Taq polymerase and 2.5 μl of DNA template. The sample was heated to 96°C for 2 min, followed by 30 cycles of 92°C for 1 min (denaturing), 56°C for 1 min (annealing), 72°C for 1 min 30 s (extension) and a final extension at 72°C for 7 min.
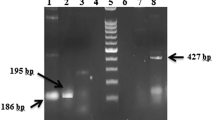
Subsequently, the primary PCR products were subjected to secondary PCR for Entamoeba species-specific characterization. Amplification was achieved using primer sets EH-1 (5’-AAG CAT TGT TTC TAG ATC TGA G-3’) and EH-2 (5’-AAG AGG TCT AAC CGA AAT TAG-3’) to detect E. histolytica (439 bp); ED-1 (5’-TCT AAT TTC GAT TAG AAC TCT-3’) and ED-2 (5’-TCC CTA CCTATT AGA CAT AGC-3’) to detect E. dispar (174 bp); Mos-1 (5’-GAA ACC AAG AGT TTC ACA AC-3’) and Mos-2 (5’-CAA TAT AAG GCT TGG ATG AT-3’) to detect E. moshkovskii (553 bp) [14] (Khairnar and Parija, 2007). The secondary amplification reagent concentrations were similar to the first PCR except that 2.5 μl of primary PCR product was added instead of genomic DNA template.
The secondary PCR had a similar cycling condition except that the annealing temperature (48°C instead of 56°C) and extension duration (1 min instead of 1 min 30 sec) were modified. In both amplifications, samples were incubated in the MyCycler thermal cycler (Bio-Rad, Hercules, USA). PCR generated amplicons of 174 bp for E. dispar, 439 bp for E. histolytica and 553 bp for E. moshkovskii were subjected to electrophoresis in 2% agarose gels at 100 V for 35 min and visualized in a UV transilluminator after staining with SYBR Safe DNA stain (Invitrogen, USA).
Data analysis
Detection of Entamoeba species was determined on the basis of morphological characteristics of the cysts under microscopy. The average cyst size is 12 μm but ranges from 10–20 μm in diameter. The data entry and analysis was carried out using the SPSS software (Statistical Package for the Social Sciences) program for Windows version 17 (SPSS, Chicago, IL, USA). Qualitative data were estimated and presented as frequencies and percentage. The prevalence and 95% confidence intervals (CIs) were calculated for each parasite. Associations between proportions were explored using Chi-Square X2 (test) and a P value of <0.05 was considered indicative of a statistically significant difference.
Results
Prevalence of Entamoeba infection via microscopy
A total of 426 samples were collected and 75 (17.6%; 95% CI = 14.0-21.2%) samples were microscopically positive for Entamoeba cysts, either singly or in combination with other intestinal parasites (Table 1). The overall prevalence of other intestinal parasites has been published (Ngui et al. 2011). Infection was more prevalent in females (19.1%; 95% CI = 14.0-24.2%) compared to males (15.9%; 95% CI = 10.8-21.0%), however, it was not statistically significant (data not shown). Similarly, more adults (23.9%; 95% CI = 16.0-31.8%) were found to be positive for Entamoeba infections compared to children (15.3%; 95% CI = 11.3-19.3%), but this difference was also not significant (P > 0.05). Higher prevalence rates were recorded in Pos Iskandar (29.2%), followed by Sungai Koyan (22.2%), Sungai Bumbun (16.8%), Bukit Serok (15.3%) while Sungai Layau (5.6%) had the least (Table 2).
Nested PCR
Of the 75 microscopy-positive samples, 52 (69.3%) samples were successfully amplified and characterized the Entamoeba species on the basis of its amplicons size using nested PCR. Additionally, 351 microscopy-negative samples were also examined using PCR and the results confirmed that these samples were negative for the Entamoeba infection. Every sample that was negative by PCR (23 samples) but positive by microscopy, was retested by PCR, and each was again found to be PCR negative. Of the 52 PCR positive results, E. histolytica infection (75.0%; 39/52) appeared to be the most predominant, followed by E. dispar (30.8%; 18/52) and E. moshkovskii (5.8%; 3/52). Of these, 33 (63.5%) were shown to contain only E. histolytica, 10 (19.2%) contained only E. dispar and 3 (5.8%) contained only E. moshkovskii. Mixed infection with E. histolytica and E. dispar was found in 6 (11.5%) samples (Table 3).
Pos Iskandar recorded the highest prevalence of E. histolytica (53.8%; 28/52), followed by Sungai Layau (5.8%; 3/52) and 2 (3.8%) samples each from Sungai Koyan, Sungai Bumbun and Bukit Serok. As for E. dispar, the highest prevalence was detected in Sungai Bumbun (13.5%; 7/52), followed by Sungai Koyan (7.8%; 4/52), Bukit Serok (5.8%; 3/52) and 2% each (1/52) for Pos Iskandar and Sungai Layau. Meanwhile, E. moshkovskii was only found in two villages with Bukit Serok (3.8%; 2/52) recorded as having the highest prevalence rate followed by one infection in Sungai Bumbun.
Discussion
The present study reported an overall prevalence of Entamoeba species as determined by microscopy as 17.6% (75/426). In Malaysia, previous studies have also reported high prevalence of Entamoeba infection with prevalence rates ranging from 9.4% to 21.0% among rural communities [23–26, 28]. In contrast, the most recent study among rural communities in Malaysia demonstrated 10.2% of the participants were infected with Entamoeba species [23]. The high prevalence of Entamoeba infection may be due to the transmission and pathogenesis as well as other risk factors which favor the persistence of this infection. Given its faecal-oral route, habits related to eating, defecation, personal hygiene, cleanliness and level of education may have an impact on the prevalence rates. The findings of this study confirmed a trend of high risk of infection with Entamoeba species among the rural population as shown by other local studies [21–23, 25], where prevailing poverty, poor socioeconomic condition, low standards of sanitation and hygiene and lack of education attainment may contribute to high prevalence of Entamoeba infection.
Additionally, the use of untreated river water as a source for household needs could also lead to the increase in the transmission of Entamoeba infection. A study in Thailand conducted to determine the occurrence of Entamoeba species in water samples using molecular techniques has indicated that water is a possible source for transmission of Entamoeba to humans [29]. From our personal observation, the majority of the households have no toilet facilities. They often defecate indiscriminately in the bushes and nearby river at the back of their houses. These water sources may be highly polluted especially in rainy seasons, by rain runoff contaminated with cysts of parasites from human faeces. Another possible source of infection could also be from the consumption of water contaminated with Entamoeba cysts from faeces of infected wild or domestic animals as they may come to the river bank to drink and at the same time defecate in or near the river. This situation is further aggravated as the drinking of unboiled water is a common practice among this community. Therefore, these communities should be given health education and made aware of the danger of drinking unboiled or improperly boiled untreated water.
Our molecular technique showed that E. histolytica (75.0%) was found to be the most common species detected in this study, followed by E. dispar (30.8%) and E. moshkovskii (5.8%). Similarly, the only available species-specific study of Entamoeba species conducted in Malaysia found that E. histolytica (13.2%) was more prevalent compared to E. dispar (5.6%) [28]. Interestingly, the high prevalence of E. histolytica in the present study was in contrast to the worldwide distribution of Entamoeba species, which indicated that E. dispar is perhaps 10 times more common than E. histolytica[1, 2, 30], however, the local prevalence may vary significantly, thus necessitating the assessment of prevalence in different geographical regions. Similar observation also reported that 70.8% of patients were infected with E. dispar, compared to 4.5% of E. histolytica and 61.8% of E. moshkovskii in Australia [10]. A study in Brazil also showed that the prevalence of E. dispar (90%) was more frequent compared to E. histolytica (10%) among infected individuals [5]. A study in India also showed parallel findings, where 49.5% patients were infected with E. dispar and only 7.4% with E. histolytica[18]. Likewise, a study in the Netherlands also found 91.2% microscopic positive samples were identified as E. dispar while 6.7% were E. histolytica by PCR [31]. In Canada, 97.1% of the examined samples contained E. dispar compared to 2.9% of E. histolytica by both PCR and ELISA assay [16].
To the best of our knowledge, the detection E. moshkovskii (5.8%) in this study was the first to be reported in Malaysia. Cases of humans infected with E. moshkovskii have been reported sporadically from different parts of the world including Thailand [6], India [9, 18, 20], Bangladesh [8, 32] and Australia [10]. A study in Bangladesh highlighted that infection with E. moshkovskii was common in children aged 2 to 5 years [8] while a study in India found that E. moshkovskii infection was associated with dysentery [9]. In our study, it was noted that all individuals infected with E. moshkovskii were children and were asymptomatic. Although amoebic liver abscess (65%) has been documented in patients admitted to an urban hospital in Malaysia [33], information from rural communities is not available as this infection can only be confirmed in a hospital setup. Therefore, future investigation which includes the clinical impact of E. moshkovskii and other Entamoeba species is imperative for a better understanding of a true pathogenic potential of E. moshkovskii.
Although every negative PCR sample was retested by PCR, each was again found to be negative. This result can potentially be explained by the presence of faecal inhibitor substances which were not completely eliminated prior to PCR reaction. Further study to optimize the reduction of these inhibitors is necessary during the extraction process in order to increase PCR sensitivity. It is also possible that the samples which were detected by microscopy but not PCR may belong to other Entamoeba species such as E. coli, E. hartmanni and E. polecki, or the contained a low number of parasites, which fell below the PCR detection limit. Therefore, a more sensitive method such as Real-Time PCR and employing primers for all Entamoeba species should be considered in future study. The failure to amplify samples could also be due to the fact that samples may contain only trophozoites that could have degenerated with time. Several studies have confirmed that the presence of Entamoeba cysts in the faecal samples, in contrast to trophozoites, somewhat increase the chances of the PCR assay [10, 34].
Conclusion
Molecular techniques are indeed promising tools for epidemiological studies, particularly in discriminating the pathogenic from the non-pathogenic species of the Entamoeba species. This study reports for the first time the identification of E. moshkovskii in human faecal samples from Malaysia. Since all of the infected participants with E. moshkovskii including those infected with the other two species were asymptomatic, further investigations are needed to determine the true pathogenic potential of these three species.
Financial support
This research work was funded by the High Impact Research Grant (E00050-20001), University of Malaya Research Grant (RG221-10HTM) and Postgraduate Research Fund (PV024/2011B) from University of Malaya. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
References
WHO: World Health Organization/Pan American Health Organization/UNESCO report of a consultation of experts on amoebiasis. Wkly Epidemiol Rec WHO. 1997, 72: 97-99.
Markell EK, John DJ, Krotoski WA: Lumen dwelling protozoa. 1999, Philadelphia, USA: WB Saunders, 8
Delialioglu N, Aslan G, Ozturk C, Ozturhan H, Sen S, Emekdas G: Detection of Entamoeba histolytica antigen in stool samples in Mersin, Turkey. J Parasitol. 2008, 94: 530-532. 10.1645/GE-1355.1.
Salvioli L, Bundy DAP, Tomkin A: Intestinal parasitic infections. Trans R Soc Trop Med Hyg. 1992, 86: 353-354. 10.1016/0035-9203(92)90215-X.
Braga L, Gomes ML, Silva MW, Paiva C, Sales A, Mann BJ: Entamoeba histolytica and Entamoeba dispar infections as detected by monoclonal antibody in an urban slum in Fortaleza, Northeastern Brazil. Rev Soc Bras Med Trop. 2001, 34: 467-471. 10.1590/S0037-86822001000500010.
Hamzah Z, Petmitr S, Mungthin M, Leelayoova S, Chavalitshewinkoon-Petmitr P: Differential detection of Entamoeba histolytica, Entamoeba dispar and Entamoeba moshkovskii by a single-round PCR Assay. J Clin Microbiol. 2006, 44: 3196-3200. 10.1128/JCM.00778-06.
Clark CG, Diamond LS: The Laredo strain and other ‘Entamoeba histolytica like’ amoebae are Entamoeba moshkovskii. Mol Biochem Parasitol. 1991, 46: 11-18. 10.1016/0166-6851(91)90194-B.
Ali IKM, Hossain MB, Roy S, Ayeh-Kumi P, Petri JWA, Haque R, Clark CG: Entamoeba moshkovskii infections in children, Bangladesh. Emerg Infect Dis Emerging. 2003, 9: 580-584. 10.3201/eid0905.020548.
Parija SC, Khairnar K: Entamoeba moshkovskii and Entamoeba dispar-associated infections in Pondicherry, India. J Health Popul Nutr. 2005, 23: 292-295.
Fotedar R, Stark D, Beebe N, Marriot D, Ellis J, Harkness J: PCR detection of Entamoeba histolytica, Entamoeba dispar and Entamoeba moshkovskii in stool samples from Sydney, Australia. J Clin Microbiol. 2007, 45: 1035-1037. 10.1128/JCM.02144-06.
Al-Harthi SA, Jamjoon MB: Diagnosis and differentiation of Entamoeba infection in Makkah Al Mukarramah using microscopy and stool antigen detection kits. World J Med Sci. 2007, 2: 15-20.
Wonsit R, Thammapalerd N, Tharavanji S, Radomyos P, Bunnarg D: Enzyme-linked immunorsorbent assay based on monoclonal and polyclonal antibodies for the detection of Entamoeba histolytica antigens in faecal specimens. Trans Roy Soc Trop Med Hyg. 1992, 86: 166-169. 10.1016/0035-9203(92)90553-O.
Katzwinkel-Wladarsch S, Loscher T, Reider H: Direct amplification and differentiation of pathogenic and non-pathogenic Entamoeba histolytica DNA from stool specimen. Am Soc Trop Med Hyg. 1994, 51: 115-118.
Troll H, Marti H, Weiss N: Simple differential detection of Entamoeba histolytica and Entamoeba dispar in fresh stool specimens by sodium acetate-acetic acid-formalin concentration and PCR. J Clin Microbiol. 1997, 35: 1701-1705.
Yvonne CW, Crandal I, Kain CK: Development of monoclonal antibodies which specifically recognize Entamoeba histolytica in preserved stool samples. J Clin Microbiol. 2001, 39: 716-719. 10.1128/JCM.39.2.716-719.2001.
Gonin P, Louise T: Detection and differentiation of Entamoeba histolytica and Entamoeba dispar isolates in clinical samples by PCR and enzyme-linked immunosorbent assay. J Clin Microbiol. 2003, 41: 237-241. 10.1128/JCM.41.1.237-241.2003.
Redondo RB, Mendez LGM, Baer G: Entamoeba histolytica and Entamoeba dispar: differentiation by enzyme-linked immunosorbent assay (ELISA) and its clinical correlation in pediatric patients. Parasitol Latinoam. 2006, 6: 37-42.
Khairnar K, Parija SC: A novel nested multiplex polymerase chain reaction (PCR) assay for differential detection of Entameoba histolytica, E. moshkovskii and E. dispar DNA in stool samples. BMC Microbiol. 2007, 7: 47-10.1186/1471-2180-7-47.
Zeehaida M, Wan Nor Amilah WAW, Amry AR, Hassan S, Sarimah A, Rahmah N: A study on the usefulness of Techlab Entamoeba histolytica II antigen detection ELISA in the diagnosis of amoebic liver abscess (ALA) at Hospital Universiti Sains Malaysia(HUSM), Kelantan, Malaysia. Trop Biomed. 2008, 25: 209-216.
Parija SC, Garg A, Puspha K, Khairnar K, Priya T: Polymerase chain reaction of diagnosis of intestinal amebiasis in Puducherry. Indian J Gastroenterol. 2010, 29: 140-142. 10.1007/s12664-010-0033-0.
Norhayati M, Fatmah MS, Yusof S: Intestinal parasitic infections in man: A review. Med J Malaysia. 2003, 58: 2-10.
Lim YAL, Romano N, Colin N, Chow SC, Smith HV: Intestinal parasitic infections amongst Orang Asli (indigenous) in Malaysia: Has socioeconomic development alleviated the problem?. Trop Biomed. 2009, 26: 110-122.
Ngui R, Saidon I, Chow SK, Rohela M, Lim YAL: Prevalence and risks factors of intestinal parasitism in rural and remote West Malaysia. PLoS Negl Trop Dis. 2011, 5: e974-10.1371/journal.pntd.0000974.
Nor A, Ashley S, Albert J: Parasitic infection in human communities living on the fringes of the Crocker Range Park Sabah, Malaysia. ASEAN Review of Biodiversity and Environmental Conservation (ARBEC). 2003,http://www.arbec.com.my/pdf/art11janmar03.pdf,
Rajeswari B, Sinniah B, Hussein H: Socioeconomic factor associate with intestinal parasites among children living in Gombak, Malaysia. Asia Pac J Publ Health. 1994, 7: 21-25. 10.1177/101053959400700104.
Hakim SL, Gan CC, Malkit K, Azian MN, Chong CK, Shaari N, Zainuddin W, Chin CN, Sara Y, Lye MS: Parasitic infections among Orang Asli (aborigine) in the Cameron Highlands, Malaysia. Southeast Asian J Trop Med Publ. 2007, 38: 415-419.
Que X, Reed SL: Nucleotide sequence of a small subunit ribosomal RNA (16S like rRNA) gene from Entamoeba histolytica: differentiation of pathogenic from non pathogenic isolates. Nucleic Acids Res. 1991, 19: 5438-10.1093/nar/19.19.5438.
Noor Azian MY, San YM, Gan CC, Yusri MY, Nurulsyamzawaty Y, Zuhaizam AH, Maslawaty MN, Norparina I, Vythilingam I: Prevalence of intestinal protozoa in an aborigine community in Pahang, Malaysia. Trop Biomed. 2006, 24: 55-62.
Sukprasert S, Rattaprasert P, Hamzah Z, Shipin OV, Chavalitshewinkoon-Petmitr P: PCR detection of Entamoeba spp from surface and waste water samples using genus-specific primers. Southeast Asian J Trop Med Publ. 2008, 39: 6-9.
Petri JWA, Haque R, Lyerly D, Vines R: Estimating the impact of amoebiasis on health. Parasitol Today. 2000, 16: 320-321. 10.1016/S0169-4758(00)01730-0.
Visser LG, Verweij JJ, Van Esbroeck M, Edeling WM, Clerinx J, Polderman AM: Diagnostic methods for differentiation of Entamoeba histolytica and Entamoeba dispar in carriers: performance and clinical implications in a non-endemic setting. Int J Med Microbiol. 2006, 296: 397-403. 10.1016/j.ijmm.2006.03.001.
Haque R, Ali IKM, Clark CG, Petri JWA: A case report of Entamoeba moshkovskii infection in a Bangladeshi child. Parasitol Int. 1998, 47: 201-202.
Farhana F, Jamaiah I, Rohela M, Abdul-Aziz NM, Nissapatorn V: A ten year (1999–2008) retrospective study of amoebiasis in University Malaya Medical Centre (UMMC), Kuala Lumpur, Malaysia. Trop Biomed. 2009, 26: 262-266.
Kebede A, Verweij JJ, Endeshaw T, Messele T, Tasew G, Petros B, Polderman AM: The use of real-time PCR to identify Entamoeba histolytica and E. dispar infections in prisoners and primary-school children in Ethiopia. Ann Trop Med Parasitol. 2004, 98: 43-48. 10.1179/000349804225003082.
Acknowledgments
The authors are very grateful to Mr. Saidon Ishak and Mr. Abdul Hamid for their assistance during sample collection. Most importantly, the authors would like to thank all the villages who have voluntarily participated in this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors have declared that no competing interests exist.
Authors’ contributions
RM, YALL, LYL and JI planned and designed the protocols. RN, LA and SAF conducted the field study the study programme, including the collections of stool samples and data from the questionnaire interviews, as well as the management of collected data. RM, YALL, LYL and JI supervised all the laboratory work. RN, LA and SAF carried out the data analysis and interpretation. RN, LA, YALL and RM prepared the first draft of the manuscript and all authors revised the manuscript critically. All authors read and approved the final version of the manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Ngui, R., Angal, L., Fakhrurrazi, S.A. et al. Differentiating Entamoeba histolytica, Entamoeba dispar and Entamoeba moshkovskii using nested polymerase chain reaction (PCR) in rural communities in Malaysia. Parasites Vectors 5, 187 (2012). https://doi.org/10.1186/1756-3305-5-187
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1756-3305-5-187