Abstract
Background
Inherited retinal disorders are clinically and genetically heterogeneous with more than 150 gene defects accounting for the diversity of disease phenotypes. So far, mutation detection was mainly performed by APEX technology and direct Sanger sequencing of known genes. However, these methods are time consuming, expensive and unable to provide a result if the patient carries a new gene mutation. In addition, multiplicity of phenotypes associated with the same gene defect may be overlooked.
Methods
To overcome these challenges, we designed an exon sequencing array to target 254 known and candidate genes using Agilent capture. Subsequently, 20 DNA samples from 17 different families, including four patients with known mutations were sequenced using Illumina Genome Analyzer IIx next-generation-sequencing (NGS) platform. Different filtering approaches were applied to identify the genetic defect. The most likely disease causing variants were analyzed by Sanger sequencing. Co-segregation and sequencing analysis of control samples validated the pathogenicity of the observed variants.
Results
The phenotype of the patients included retinitis pigmentosa, congenital stationary night blindness, Best disease, early-onset cone dystrophy and Stargardt disease. In three of four control samples with known genotypes NGS detected the expected mutations. Three known and five novel mutations were identified in NR2E3, PRPF3, EYS, PRPF8, CRB1, TRPM1 and CACNA1F. One of the control samples with a known genotype belongs to a family with two clinical phenotypes (Best and CSNB), where a novel mutation was identified for CSNB. In six families the disease associated mutations were not found, indicating that novel gene defects remain to be identified.
Conclusions
In summary, this unbiased and time-efficient NGS approach allowed mutation detection in 75% of control cases and in 57% of test cases. Furthermore, it has the possibility of associating known gene defects with novel phenotypes and mode of inheritance.
Similar content being viewed by others
Background
Inherited retinal disorders affect approximately 1 in 2000 individuals worldwide [1]. Symptoms and associated phenotypes are variable. In some groups the disease can be mild and stationary such as in congenital stationary night blindness (CSNB) or achromatopsia (ACHM), whereas other disorders are progressive leading to severe visual impairment such as in rod-cone dystrophies, also known as retinitis pigmentosa (RP) or cone and cone-rod dystrophies. The heterogeneity of these diseases is reflected in the number of underlying gene defects. To date more than 150 genes have been implicated in different forms of retinal disorders http://www.sph.uth.tmc.edu/Retnet/home.htm and yet in a significant proportion of patients the disease causing mutation could not be identified, suggesting additional novel genes that remain to be discovered. Furthermore, recent studies have outlined that distinct phenotypes can be related to the dysfunction of the same gene [2–4]. Furthermore, there may be additional phenotype-genotype associations that are still not recognized. The state-of-the-art phenotypic characterization including precise family history and functional as well as structural assessment (i.e. routine ophthalmic examination, perimetry, color vision, full field and multifocal electroretinography (ERG), fundus autofluorescence (FAF) imaging and optical coherence tomography (OCT)) allows targeted mutation analysis for some disorders. However, in most cases of inherited retinal diseases, similar phenotypic features can be due to a large number of different gene defects.
Various methods can be used for the identification of the corresponding genetic defect. All these methods have advantages and disadvantages. Sanger sequencing is still the gold-standard in determining the gene defect, but due to the heterogeneity of the disorders it is time consuming and expensive to screen all known genes. Mutation detection by commercially available APEX genotyping microarrays (ASPER Ophthalmics, Estonia) [5, 6] allows the detection of only known mutations. In addition, a separate microarray has been designed for each inheritance pattern, which tends to escalate the costs especially in simplex cases, for which inheritance pattern cannot be predetermined. Indirect methods with single nucleotide polymorphism (SNP) microarrays for linkage and homozygosity mapping are also powerful tools, which has proven its reliability in identifying novel and known gene defects [7–12]. However, in case of homozygosity mapping the method can only be applied to consanguineous families or inbred populations. To overcome these challenges, we designed a custom sequencing array in collaboration with a company (IntegraGen, Evry, France) to target all exons and part of flanking sequences for 254 known and candidate retinal genes. This array was subsequently applied through NGS to a cohort of 20 patients from 17 families with different inheritance pattern and clinical diagnosis including RP, CSNB, Best disease, early-onset cone dystrophy and Stargardt disease.
Methods
Clinical investigation
The study protocol adhered to the tenets of the Declaration of Helsinki and was approved by the local Ethics Committee (CPP, Ile de France V). Informed written consent was obtained from each study participant. Index patients underwent full ophthalmic examination as described before [13]. Whenever available, blood samples from affected and unaffected family members were collected for co-segregation analysis.
Previous molecular genetic analysis
Total genomic DNA was extracted from peripheral blood leucocytes according to manufacturer's recommendations (Qiagen, Courtaboeuf, France). DNA samples from some patients with a diagnosis of RP were first analyzed and excluded for known mutations by applying commercially available microarray analysis (arRP and adRP ASPER Ophthalmics, Tartu, Estonia). In some cases, pathogenic variants in EYS, C2orf71, RHO, PRPF31, PRPH2 and RP1 were excluded by direct Sanger sequencing of the coding exonic and flanking intronic regions of the respective genes [13–17]. Conditions used to amplify PRPH2 can be provided on request.
Molecular genetic analysis using NGS
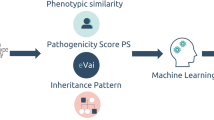
A custom-made SureSelect oligonucleotide probe library was designed to capture the exons of 254 genes for different retinal disorders and candidate genes according to Agilent's recommendations (Table 1). These genes include 177 known genes underlying retinal dysfunction (http://www.sph.uth.tmc.edu/retnet/sum-dis.htm, October 2010, Table 1) and 77 candidate genes associated with existing animal models and expression data (Table 2). The eArray web-based probe design tool was used for this purpose https://earray.chem.agilent.com/earray. The following parameters were chosen for probe design: 120 bp length, 3× probe-tiling frequency, 20 bp overlap in restricted regions, which were identified by the implementation of eArray's RepeatMasker program. A total of 27,430 probes, covering 1177 Mb, were designed and synthesized by Agilent Technologies (Santa Clara, CA, USA). Sequence capture, enrichment, and elution were performed according to the manufacturer's instructions (SureSelect, Agilent). Briefly, three μg of each genomic DNA were fragmented by sonication and purified to yield fragments of 150-200 bps. Paired-end adaptor oligonucleotides from Illumina were ligated on repaired DNA fragments, which were then purified and enriched by six PCR cycles. 500 ng of the purified libraries were hybridized to the SureSelect oligo probe capture library for 24 h. After hybridization, washing, and elution, the eluted fraction underwent 14 cycles of PCR-amplification. This was followed by purification and quantification by qPCR to obtain sufficient DNA template for downstream applications. Each eluted-enriched DNA sample was then sequenced on an Illumina GAIIx as paired-end 75 bp reads. Image analysis and base calling was performed using Illumina Real Time Analysis (RTA) Pipeline version 1.10 with default parameters. Sequence reads were aligned to the reference human genome (UCSC hg19) using commercially available software (CASAVA1.7, Illumina) and the ELANDv2 alignment algorithm. Sequence variation annotation was performed using the IntegraGen in-house pipeline, which consisted of gene annotation (RefSeq), detection of known polymorphisms (dbSNP 131, 1000 Genome) followed by mutation characterization (exonic, intronic, silent, nonsense etc.). For each position, the exomic frequencies (homozygous and heterozygous) were determined from all the exomes already sequenced by IntegraGen and the exome results provided by HapMap project.
Investigation of annotated sequencing data
We received the annotated sequencing data in the form of excel tables. On average 946 SNPs and 83 insertions and deletions were identified for each sample (Figure 1). By using the filtering system, we first investigated variants (nonsense and missense mutations, intronic variants located +/- 5 apart from exon), which were absent in dbSNP and NCBI databases http://ncbi.nlm.nih.gov/. In the absence of known gene defects or putative pathogenic variants (see below) in the first step, we selected known genes, which were previously clinically associated including variants present in dbSNP and NCBI databases (Figure 1). Each predicted pathogenic variant was confirmed by Sanger sequencing.
Flow chart of variant analysis. IntegraGen provided the results in form of excel tables. For each sample on average 946 SNPs and 83 inDels were detected, of which 11 represent missense, nonsense or putative splice site mutations, which were absent in dbSNB, NCBI and 1000 genome databases. Of those 1-5 variants were predicted to be pathogenic. In case where none of the variants were predicted to be pathogenic, dbSNB, NCBI and 1000 genome databases were included to detect mutations referenced with an rs-number. Co-segregation analysis was performed in families with putative pathogenic variants.
Assessment of the pathogenicity of variants
Following criteria were applied to evaluate the pathogenic nature of novel variations identified by NGS: 1) stop/frameshift variants were considered as most likely to be disease causing; 2) co-segregation in the family; 3) absence in control samples; 4) for missense mutations amino acid conservation was studied in the UCSC Genome Browser http://genome.ucsc.edu/ across species from all different evolutionary branches. If the amino acid residue did not change it was considered as "highly conserved". If a different change was seen in fewer than five species and not in the primates then it was considered as "moderately conserved" and if a change was present in 5-7, it was considered as "weakly conserved", otherwise the amino acid residue was considered as "not conserved", 5) pathogenicity predictions with bioinformatic tools (Polyphen: Poly morphism Phen otyping, http://genetics.bwh.harvard.edu/pph/ and SIFT: Sorting Intolerant From Tolerant, http://blocks.fhcrc.org/sift/SIFT.html) if at least one of the program predicted the variant to be possibly damaging, it was considered to be pathogenic; 6) presence of the second mutant allele in the case of autosomal recessive inheritance. Mutations were described according to the HGVS website http://www.hgvs.org/mutnomen. In accordance with this nomenclature, nucleotide numbering reflects cDNA numbering with +1 corresponding to the A of the ATG translation initiation codon in the reference sequence. The initiation codon is codon 1. The correct nomenclature for mutation was checked applying Mutalyzer http://www.lovd.nl/mutalyzer/.
Results
The overall sequencing coverage of the captured regions was 98.4% and 90.4% for a 1× and a 10× coverage respectively. The overall sequencing depth was > 120×. The number of reference and variant sequences detected by NGS, reflected the correct zygosity state of the variant; on average if 50% of the sequences represented the variant, then a heterozygous state was called, while if 100% of the sequences represented the variant, then a homozygous or hemizygous state was annotated by IntegraGen.
Validation of the novel genetic testing tool for retinal disorders
To validate the novel genetic testing tool for retinal disorders, we used four DNA samples from families, in which we had previously identified different types of mutations by Sanger sequencing: one 1 bp duplication and one 1 bp deletion in PRPF31 and missense mutations in TRPM1 and BEST1 (Table 3). Three of the four mutations were detectable by NGS, whereas the deletion in PRPF31 was not identified. To validate if this was due to a technical problem of deletion detection in general or low coverage at this position, the sequencing depth was investigated in detail. Indeed the coverage at this position reflected by the mean depth was only ~1-6 for all samples. This indicates that although the coverage in general was very good, specific probes used here need to be redesigned to improve the capture for specific exons.
Detection of known and novel mutations
Some of the patients from the 14 families with no known gene defect were previously excluded for known mutations using microarray analysis and by Sanger sequencing in the known genes EYS, C2orf71, RHO, PRPF31, PRPH2 and RP1. Other samples were never genetically investigated. In four DNA samples known mutations were detected (Table 4) from three different families with autosomal dominant (ad) or recessive (ar) RP. All mutations co-segregated with the phenotype (Figure 2). In seven samples, novel mutations in known genes were identified. These mutations co-segregated with the phenotype from five different families with adCSNB, x-linked incomplete CSNB, adRP, arRP and x-linked RP (Table 5, Figures 3 and 4). One of the cases from these five families was also used as a control for Best disease carrying a known BEST1 mutation (Table 3). In addition to the Best phenotype, ERG-responses of this patient resembled those of complete CSNB, i.e. showing selective ON-bipolar pathway dysfunction. This phenotype was independent of the Best phenotype (Figure 3). The most likely disease causing mutation detected by NGS was a novel heterozygous TRPM1 mutation (Table 4, Figure 3).
Detection of known mutations by NGS in 254 retinal genes. The index patient 19 of family 16 with adRP revealed the p.T494M mutations in PRPF3, which co-segregates with the phenotype. Two family members never clinically investigated from the last generation (984 and 1167 carrying a question mark) were reported to be not affected but carried the mutation. They may develop the phenotype at a later stage. In addition variability of the phenotype of this mutation was documented [35]. Two patients, 128 and 943 of family 100 with arRP from Jewish origin revealed the known EYS mutation p.N137VfsX24, which was found in all screened affected family members. The index patient 893 of family 574 showed the previously described NR2E3 p.G56R mutation, which co-segregated with the phenotype.
Best disease and CSNB co-segregating in one family. a) Sanger and NGS detected in all patients with Best disease a BEST1 mutation. b) NGS detected in all patients with a cCSNB phenotype a novel TRPM1 mutation. c) Fundus colour photographs (above) and fundus autofluorescence (below) of patient 707 showing multiple yellow deposits within the posterior pole which are hyper autofluorescent d) Electro-oculogram of patient 707 showing no slight rise after illumination in keeping with the diagnosis of Best disease e) Full Field Electroretinogram of patient 707 showing ON-bipolar cell pathway dysfunction in keeping with the diagnosis of cCSNB.
Detection of novel mutations using NGS in 254 retinal genes. Novel mutations in PRPF8, CRB1, RPGR and CACNA1F co-segregated in affected and asymptomatic carriers with the adRP, arRP, x-linked dominant and X-liked icCSNB phenotypes respectively. Asymptomatic individuals are marked with a question mark.
Unsolved cases
In six of the 14 families with Stargardt disease, adRP, adCD with postreceptoral defects, arRP, early onset arCD with macrocephaly and mental retardation described in affected sister and x-linked cCSNB, the disease associated mutations remain to be elucidated or validated (Table 6, Figure 5).
Detection of novel mutation by using NGS in 254 retinal genes. Family 795 reveals autosomal dominant cone dystrophy with post-receptoral defects. Four putative disease causing mutations were investigated on the basis of co-segregation. However, none of them co-segregated in all affected family members with the phenotype and thus are not considered to be disease causing. Individuals marked with a star were clinically investigated, patients with a question mark are asymptomatic and patients with a plus sign show high myopia.
Discussion
By using NGS in 254 known and candidate genes we were able to detect known and novel mutations in 57% of families tested. In order to achieve this goal, we applied a rigorous protocol (Figure 1). To our knowledge, this is the first report using NGS to investigate all inherited retinal disorders at once. In a study restricted to adRP, Bowne and co-workers used a similar approach including 46 known and candidate genes for adRP [18]. All their cases had previously been screened and excluded for most of the known genes underlying adRP. The authors were able to identify known or novel mutations in five out of 21 cases in genes not included in a pre-screening [18]. This added five patients to their adRP cohort with known gene defects, indicating that 64% of their patients show known mutations with new genes still to be discovered in the remaining 36%. The current study provides a more exhaustive tool, since it incorporates screening of 254 genes implicated in various retinal disorders of different inheritance patterns and additional candidate genes for these phenotypes. With this approach a cohort of both pre-screened and unscreened samples, was investigated. The mutation detection rate of 57% is high and was never obtained before by high throughput screening methods. Furthermore, this approach is probably less time consuming and expensive than existing methods such as direct sequencing of all known genes or microarray analysis. Of note however is one of the variants detected with the NGS approach (i.e. p.V973L exchange in GUCY2D), which was not confirmed by direct Sanger sequencing, suggesting the possibility of false positive using the high throughput screening. Verification by direct Sanger sequencing of most likely pathogenic variants is therefore essential to validate NGS data, although the false positive rate is assumed to be low (in our study 1/28 verified sequence variants represented a false positive).
Overall, the study of 20 subjects from 17 families by NGS showed that most of the targeted regions are well covered (more than 98%). However, some of the regions showed a lower coverage (GC-rich regions) or were not captured (repetitive regions). This was for instance the case for two genes underlying cCSNB, (i.e. NYX and GRM6) and the repetitive region of ORF15 of RPGR. For GC-rich regions the capture design could be improved in the future by modifying NGS chemistry, as it was successfully achieved for Sanger sequencing using different additives, which improved the amplification and subsequent sequencing. If repetitive regions like ORF15 of RPGR remain problematic for sequencing by NGS, direct Sanger sequencing of these targets might be the first screening of choice; in particular for disorders caused only by a few gene defects such as CSNB, and xl-RP.
By applying NGS sequencing to our retinal panel, known and novel mutations were detected in different patients. We believe that our diagnostic tool is particularly important for heterogeneous disorders like RP, for which many gene defects with different prevalence have been associated to one phenotype. It also allows the rapid detection of novel mutations in minor genes which are often not screened as a priority by direct Sanger sequencing. This was the case in our study for three individuals from one family with adRP in which NGS detected a novel PRPF8 mutation in both affected and one unaffected family member (Table 4, Figure 4). In this family, the RP phenotype is mild and therefore it is possible that the unaffected member may develop symptoms later in life or alternatively it may be a case of incomplete penetrance as reported for another splicing factor gene, PRPF31 and recently for PRPF8 as well [19–22]. Interestingly, a novel TRPM1 mutation was identified in a patient with adCSNB, a gene previously only associated with arCSNB [23–26]. This is the first report of a TRPM1 mutation co-segregating with ad Schubert-Bornschein type complete CSNB. Since the location of this mutation is not different compared to other mutations leading to arCSNB, it is not quite clear how TRPM1 mutations might lead to either ad or arCSNB. Functional investigations are needed to validate the pathogenicity of this variant. Furthermore, this finding suggests that TRPM1 heterozygous mutation carriers from arCSNB families should be investigated by electroretinography to determine whether they display similar retinal dysfunction as in affected members of the presented adCSNB family. Detection of a novel RPGR splice site mutation in family 146 presented a challenge. The actual disease causing change was concealed under a wrongly annotated rs62638633, which had previously been clinically associated to RP by a German group http://www.ncbi.nlm.nih.gov/sites/varvu?gene=6103&rs=62638633, (personal communication, Markus Preising). These observations indicate that the stringent filtering we applied initially can mask those referenced disease causing variants. Bearing this in mind one can still first investigate unknown variants, but should then examine dbSNP for referenced variants either described to be disease causing, having a low minor allele frequency or present in interesting candidate genes. An accurate discrimination of non-pathogenic polymorphisms versus disease causing polymorphism in SNP databases is warranted to resolve this challenge.
In six families from the investigated cohort the disease causing mutations still remain to be identified. In the Stargardt patient with no pathogenic ABCA4 mutations two variants in CFH were detected, one of which (rs1061170) had previously been reported to predispose to age related macular degeneration (AMD) [27–29]. The second CFH change is a novel variant, affecting a highly conserved residue, not found in NGS data from the other 19 samples and never associated with a disease. The variants co-segregated in the only available family members, which were the patient's parents. Apart from the association with AMD, CFH mutations have been previously associated with renal diseases, the most common being membranoproliferative glomerulonephritis and hemolytic uremic syndrome, which can be also associated with an eye phenotype [30, 31]. No renal dysfunction was present in our patient. To validate if the two variants identified in CFH are indeed disease causing, the DNA samples from other available family members for co-segregation analysis as well as characterization of functional consequences of the novel variant are needed. One patient with complete CSNB had an affected nephew and thus x-linked inheritance was assumed. However, neither Sanger nor NGS detected a mutation in the only known x-linked gene, NYX, causing cCSNB. To exclude recessive inheritance TRPM1 and GRM6 were investigated in detail. Indeed the patient carried a novel heterozygous TRPM1 variant, which affects a highly conserved amino acid and was not identified in the other 19 samples investigated here (Table 6). However, direct Sanger sequencing of lower covered regions did not identify a second mutation in this gene. Similarly no mutations in GRM6 were identified. These findings outline the need for additional family members to determine, through co-segregation, the pathogenicity of the numerous variants identified by NGS. This was also true for two other families with nonsense mutations in CUBN (Fam795) and RP1L1 (Fam761) (Table 6). The nonsense mutation in CUBN, co-segregated with the phenotype in most of the family members (Figure 5). Had we not had access to additional family members, we might have retained this gene defect as the underlying cause for adCD and considered CUBN as a new gene involved in adCD. None of the other putatively pathogenic mutations identified in CUBN, TRPM1 and GUCY2D co-segregated with the phenotype in this family (Table 6, Figure 5). RP1L1 was already a candidate for adRP [32] but was previously associated with occult macular dystrophy [33]. In our study, this variant did not co-segregate with the phenotype in other affected family members (data not shown).
This NGS study ended with six genetically unresolved families, which can be further investigated with whole exome sequencing. Although, no clear information about the actual percentage of missing gene defects underlying each group of inherited retinal disorders exists, previous studies have reported that in many cases the genetic cause still needs to be determined [18, 34]. Whole exome sequencing approaches allow the detection of both, novel and known gene defects, but also generate numerous variants and therefore require the inclusion of more than one DNA sample for each family to rapidly exclude non-pathogenic variants. Due to the higher costs of exome sequencing for one sample compared to targeted sequencing, we propose to initially perform targeted sequencing in the index patient and proceed only after exclusion of a known gene defect to whole exome sequencing.
Conclusions
In summary, our diagnostic tool is an unbiased time efficient method, which not only allows detecting known and novel mutations in known genes but also potentially associates known gene defects with novel phenotypes. This genetic testing tool can now be applied to large cohorts of inherited retinal disorders and should rapidly deliver the prevalence of known genes and the percentage of cases with missing genetic defect for underlying forms of retinal disorders.
Abbreviations
- ad:
-
autosomal dominant
- ar:
-
autosomal recessive
- as:
-
asymptomatic
- het:
-
heterozygous
- homo:
-
homozygous
- hemi:
-
hemizygous
- -:
-
not noted
- consang.:
-
consanguinity was reported
- n.a.:
-
not applicable
- CSNB:
-
congenital stationary night blindness
- RP:
-
retinitis pigmentosa:
References
Sohocki MM, Daiger SP, Bowne SJ, Rodriquez JA, Northrup H, Heckenlively JR, Birch DG, Mintz-Hittner H, Ruiz RS, Lewis RA, Saperstein DA, Sullivan LS: Prevalence of mutations causing retinitis pigmentosa and other inherited retinopathies. Hum Mutat. 2001, 17: 42-51. 10.1002/1098-1004(2001)17:1<42::AID-HUMU5>3.0.CO;2-K.
Boon CJ, den Hollander AI, Hoyng CB, Cremers FP, Klevering BJ, Keunen JE: The spectrum of retinal dystrophies caused by mutations in the peripherin/RDS gene. Prog Retin Eye Res. 2008, 27: 213-235. 10.1016/j.preteyeres.2008.01.002.
Boon CJ, Klevering BJ, Leroy BP, Hoyng CB, Keunen JE, den Hollander AI: The spectrum of ocular phenotypes caused by mutations in the BEST1 gene. Prog Retin Eye Res. 2009, 28: 187-205. 10.1016/j.preteyeres.2009.04.002.
Schorderet DF, Escher P: NR2E3 mutations in enhanced S-cone sensitivity syndrome (ESCS), Goldmann-Favre syndrome (GFS), clumped pigmentary retinal degeneration (CPRD), and retinitis pigmentosa (RP). Hum Mutat. 2009, 30: 1475-1485. 10.1002/humu.21096.
Jaakson K, Zernant J, Kulm M, Hutchinson A, Tonisson N, Glavac D, Ravnik-Glavac M, Hawlina M, Meltzer MR, Caruso RC, Testa F, Maugeri A, Hoyng CB, Gouras P, Simonelli F, Lewis RA, Lupski JR, Cremers FP, Allikmets R: Genotyping microarray (gene chip) for the ABCR (ABCA4) gene. Hum Mutat. 2003, 22: 395-403. 10.1002/humu.10263.
Zeitz C, Labs S, Lorenz B, Forster U, Uksti J, Kroes HY, De Baere E, Leroy BP, Cremers FP, Wittmer M, van Genderen MM, Sahel JA, Audo I, Poloschek CM, Mohand-Said S, Fleischhauer JC, Huffmeier U, Moskova-Doumanova V, Levin AV, Hamel CP, Leifert D, Munier FL, Schorderet DF, Zrenner E, Friedburg C, Wissinger B, Kohl S, Berger W: Genotyping microarray for CSNB-associated genes. Invest Ophthalmol Vis Sci. 2009, 50: 5919-5926. 10.1167/iovs.09-3548.
Wang H, den Hollander AI, Moayedi Y, Abulimiti A, Li Y, Collin RW, Hoyng CB, Lopez I, Bray M, Lewis RA, Lupski JR, Mardon G, Koenekoop RK, Chen R: Mutations in SPATA7 cause leber congenital amaurosis and juvenile retinitis pigmentosa. Am J Hum Genet. 2009, 84: 380-387. 10.1016/j.ajhg.2009.02.005.
den Hollander AI, McGee TL, Ziviello C, Banfi S, Dryja TP, Gonzalez-Fernandez F, Ghosh D, Berson EL: A homozygous missense mutation in the IRBP gene (RBP3) associated with autosomal recessive retinitis pigmentosa. Invest Ophthalmol Vis Sci. 2009, 50: 1864-1872.
Collin RW, Littink KW, Klevering BJ, van den Born LI, Koenekoop RK, Zonneveld MN, Blokland EA, Strom TM, Hoyng CB, den Hollander AI, Cremers FP: Identification of a 2 Mb human ortholog of Drosophila eyes shut/spacemaker that is mutated in patients with retinitis pigmentosa. Am J Hum Genet. 2008, 83: 594-603. 10.1016/j.ajhg.2008.10.014.
Collin RW, Safieh C, Littink KW, Shalev SA, Garzozi HJ, Rizel L, Abbasi AH, Cremers FP, den Hollander AI, Klevering BJ, Ben-Yosef T: Mutations in C2ORF71 cause autosomal-recessive retinitis pigmentosa. Am J Hum Genet. 2010, 86: 783-788. 10.1016/j.ajhg.2010.03.016.
Bandah-Rozenfeld D, Collin RW, Banin E, van den Born LI, Coene KL, Siemiatkowska AM, Zelinger L, Khan MI, Lefeber DJ, Erdinest I, Testa F, Simonelli F, Voesenek K, Blokland EA, Strom TM, Klaver CC, Qamar R, Banfi S, Cremers FP, Sharon D, den Hollander AI: Mutations in IMPG2, encoding interphotoreceptor matrix proteoglycan 2, cause autosomal-recessive retinitis pigmentosa. Am J Hum Genet. 2010, 87: 199-208. 10.1016/j.ajhg.2010.07.004.
Audo I, Bujakowska K, Mohand-Said S, Tronche S, Lancelot ME, Antonio A, Germain A, Lonjou C, Carpentier W, Sahel JA, Bhattacharya S, Zeitz C: A novel DFNB31 mutation associated with Usher type 2 syndrome showing variable degrees of auditory loss in a consanguineous Portuguese family. Mol Vis. 2011, 17: 1598-1606.
Audo I, Sahel JA, Mohand-Said S, Lancelot ME, Antonio A, Moskova-Doumanova V, Nandrot EF, Doumanov J, Barragan I, Antinolo G, Bhattacharya SS, Zeitz C: EYS is a major gene for rod-cone dystrophies in France. Hum Mutat. 2010, 31: E1406-1435. 10.1002/humu.21249.
Audo I, Lancelot ME, Mohand-Said S, Antonio A, Germain A, Sahel JA, Bhattacharya SS, Zeitz C: Novel C2orf71 mutations account for approximately 1% of cases in a large French arRP cohort. Hum Mutat. 2011, 32: E2091-2103. 10.1002/humu.21460.
Audo I, Manes G, Mohand-Said S, Friedrich A, Lancelot ME, Antonio A, Moskova-Doumanova V, Poch O, Zanlonghi X, Hamel CP, Sahel JA, Bhattacharya SS, Zeitz C: Spectrum of rhodopsin mutations in French autosomal dominant rod-cone dystrophy patients. Invest Ophthalmol Vis Sci. 2010, 51: 3687-3700. 10.1167/iovs.09-4766.
Audo I, Bujakowska K, Mohand-Said S, Lancelot ME, Moskova-Doumanova V, Waseem NH, Antonio A, Sahel JA, Bhattacharya SS, Zeitz C: Prevalence and novelty of PRPF31 mutations in French autosomal dominant rod-cone dystrophy patients and a review of published reports. BMC Med Genet. 2010, 11: 145-10.1186/1471-2350-11-145.
Audo I, Mohand-Said S, Dhaenens CM, Germain A, Orhan E, Antonio A, Hamel C, Sahel JA, Bhattacharya SS, Zeitz C: RP1 and autosomal dominant rod-cone dystrophy: Novel mutations, a review of published variants, and genotype-phenotype correlation. Hum Mutat. 2012, 33: 73-80. 10.1002/humu.21640.
Bowne SJ, Sullivan LS, Koboldt DC, Ding L, Fulton R, Abbott RM, Sodergren EJ, Birch DG, Wheaton DH, Heckenlively JR, Liu Q, Pierce EA, Weinstock GM, Daiger SP: Identification of disease-causing mutations in autosomal dominant retinitis pigmentosa (adRP) using next-generation DNA sequencing. Invest Ophthalmol Vis Sci. 2011, 52: 494-503. 10.1167/iovs.10-6180.
Vithana EN, Abu-Safieh L, Pelosini L, Winchester E, Hornan D, Bird AC, Hunt DM, Bustin SA, Bhattacharya SS: Expression of PRPF31 mRNA in patients with autosomal dominant retinitis pigmentosa: a molecular clue for incomplete penetrance?. Invest Ophthalmol Vis Sci. 2003, 44: 4204-4209. 10.1167/iovs.03-0253.
McGee TL, Devoto M, Ott J, Berson EL, Dryja TP: Evidence that the penetrance of mutations at the RP11 locus causing dominant retinitis pigmentosa is influenced by a gene linked to the homologous RP11 allele. Am J Hum Genet. 1997, 61: 1059-1066. 10.1086/301614.
Vithana EN, Abu-Safieh L, Allen MJ, Carey A, Papaioannou M, Chakarova C, Al-Maghtheh M, Ebenezer ND, Willis C, Moore AT, Bird AC, Hunt DM, Bhattacharya SS: A human homolog of yeast pre-mRNA splicing gene, PRP31, underlies autosomal dominant retinitis pigmentosa on chromosome 19q13.4 (RP11). Mol Cell. 2001, 8: 375-381. 10.1016/S1097-2765(01)00305-7.
Maubaret CG, Vaclavik V, Mukhopadhyay R, Waseem NH, Churchill A, Holder GE, Moore AT, Bhattacharya SS, Webster AR: Autosomal Dominant Retinitis Pigmentosa with Intrafamilial Variability and Incomplete Penetrance in Two Families carrying Mutations in PRPF8. Invest Ophthalmol Vis Sci. 2011
Li Z, Sergouniotis PI, Michaelides M, Mackay DS, Wright GA, Devery S, Moore AT, Holder GE, Robson AG, Webster AR: Recessive mutations of the gene TRPM1 abrogate ON bipolar cell function and cause complete congenital stationary night blindness in humans. Am J Hum Genet. 2009, 85: 711-719. 10.1016/j.ajhg.2009.10.003.
van Genderen MM, Bijveld MM, Claassen YB, Florijn RJ, Pearring JN, Meire FM, McCall MA, Riemslag FC, Gregg RG, Bergen AA, Kamermans M: Mutations in TRPM1 are a common cause of complete congenital stationary night blindness. Am J Hum Genet. 2009, 85: 730-736. 10.1016/j.ajhg.2009.10.012.
Audo I, Kohl S, Leroy BP, Munier FL, Guillonneau X, Mohand-Said S, Bujakowska K, Nandrot EF, Lorenz B, Preising M, Kellner U, Renner AB, Bernd A, Antonio A, Moskova-Doumanova V, Lancelot ME, Poloschek CM, Drumare I, Defoort-Dhellemmes S, Wissinger B, Leveillard T, Hamel CP, Schorderet DF, De Baere E, Berger W, Jacobson SG, Zrenner E, Sahel JA, Bhattacharya SS, Zeitz C: TRPM1 is mutated in patients with autosomal-recessive complete congenital stationary night blindness. Am J Hum Genet. 2009, 85: 720-729. 10.1016/j.ajhg.2009.10.013.
Nakamura M, Sanuki R, Yasuma TR, Onishi A, Nishiguchi KM, Koike C, Kadowaki M, Kondo M, Miyake Y, Furukawa T: TRPM1 mutations are associated with the complete form of congenital stationary night blindness. Mol Vis. 2010, 16: 425-437.
Klein RJ, Zeiss C, Chew EY, Tsai JY, Sackler RS, Haynes C, Henning AK, SanGiovanni JP, Mane SM, Mayne ST, Bracken MB, Ferris FL, Ott J, Barnstable C, Hoh J: Complement factor H polymorphism in age-related macular degeneration. Science. 2005, 308: 385-389. 10.1126/science.1109557.
Edwards AO, Ritter R, Abel KJ, Manning A, Panhuysen C, Farrer LA: Complement factor H polymorphism and age-related macular degeneration. Science. 2005, 308: 421-424. 10.1126/science.1110189.
Haines JL, Hauser MA, Schmidt S, Scott WK, Olson LM, Gallins P, Spencer KL, Kwan SY, Noureddine M, Gilbert JR, Schnetz-Boutaud N, Agarwal A, Postel EA, Pericak-Vance MA: Complement factor H variant increases the risk of age-related macular degeneration. Science. 2005, 308: 419-421. 10.1126/science.1110359.
Ault BH: Factor H and the pathogenesis of renal diseases. Pediatr Nephrol. 2000, 14: 1045-1053. 10.1007/s004670050069.
Boon CJ, van de Kar NC, Klevering BJ, Keunen JE, Cremers FP, Klaver CC, Hoyng CB, Daha MR, den Hollander AI: The spectrum of phenotypes caused by variants in the CFH gene. Mol Immunol. 2009, 46: 1573-1594. 10.1016/j.molimm.2009.02.013.
Bowne SJ, Daiger SP, Malone KA, Heckenlively JR, Kennan A, Humphries P, Hughbanks-Wheaton D, Birch DG, Liu Q, Pierce EA, Zuo J, Huang Q, Donovan DD, Sullivan LS: Characterization of RP1L1, a highly polymorphic paralog of the retinitis pigmentosa 1 (RP1) gene. Mol Vis. 2003, 9: 129-137.
Akahori M, Tsunoda K, Miyake Y, Fukuda Y, Ishiura H, Tsuji S, Usui T, Hatase T, Nakamura M, Ohde H, Itabashi T, Okamoto H, Takada Y, Iwata T: Dominant mutations in RP1L1 are responsible for occult macular dystrophy. Am J Hum Genet. 2010, 87: 424-429. 10.1016/j.ajhg.2010.08.009.
Berger W, Kloeckener-Gruissem B, Neidhardt J: The molecular basis of human retinal and vitreoretinal diseases. Prog Retin Eye Res. 2010, 29: 335-375. 10.1016/j.preteyeres.2010.03.004.
Vaclavik V, Gaillard MC, Tiab L, Schorderet DF, Munier FL: Variable phenotypic expressivity in a Swiss family with autosomal dominant retinitis pigmentosa due to a T494M mutation in the PRPF3 gene. Mol Vis. 2010, 16: 467-475.
Zhao SH, Pan DY, Zhang Y, Wu JH, Liu X, Xu Y: Annexin A2 promotes choroidal neovascularization by increasing vascular endothelial growth factor expression in a rat model of argon laser coagulation-induced choroidal neovascularization. Chin Med J (Engl). 2010, 123: 713-721.
Cantagrel V, Silhavy JL, Bielas SL, Swistun D, Marsh SE, Bertrand JY, Audollent S, Attie-Bitach T, Holden KR, Dobyns WB, Traver D, Al-Gazali L, Ali BR, Lindner TH, Caspary T, Otto EA, Hildebrandt F, Glass IA, Logan CV, Johnson CA, Bennett C, Brancati F, Valente EM, Woods CG, Gleeson JG: Mutations in the cilia gene ARL13B lead to the classical form of Joubert syndrome. Am J Hum Genet. 2008, 83: 170-179. 10.1016/j.ajhg.2008.06.023.
Sehgal R, Sheibani N, Rhodes SJ, Belecky Adams TL: BMP7 and SHH regulate Pax2 in mouse retinal astrocytes by relieving TLX repression. Dev Biol. 2009, 332: 429-443. 10.1016/j.ydbio.2009.05.579.
Beales PL, Badano JL, Ross AJ, Ansley SJ, Hoskins BE, Kirsten B, Mein CA, Froguel P, Scambler PJ, Lewis RA, Lupski JR, Katsanis N: Genetic interaction of BBS1 mutations with alleles at other BBS loci can result in non-Mendelian Bardet-Biedl syndrome. Am J Hum Genet. 2003, 72: 1187-1199. 10.1086/375178.
Badano JL, Leitch CC, Ansley SJ, May-Simera H, Lawson S, Lewis RA, Beales PL, Dietz HC, Fisher S, Katsanis N: Dissection of epistasis in oligogenic Bardet-Biedl syndrome. Nature. 2006, 439: 326-330. 10.1038/nature04370.
Kornak U, Kasper D, Bosl MR, Kaiser E, Schweizer M, Schulz A, Friedrich W, Delling G, Jentsch TJ: Loss of the ClC-7 chloride channel leads to osteopetrosis in mice and man. Cell. 2001, 104: 205-215. 10.1016/S0092-8674(01)00206-9.
Colville DJ, Savige J: Alport syndrome. A review of the ocular manifestations. Ophthalmic Genet. 1997, 18: 161-173. 10.3109/13816819709041431.
Lemmink HH, Mochizuki T, van den Heuvel LP, Schroder CH, Barrientos A, Monnens LA, van Oost BA, Brunner HG, Reeders ST, Smeets HJ: Mutations in the type IV collagen alpha 3 (COL4A3) gene in autosomal recessive Alport syndrome. Hum Mol Genet. 1994, 3: 1269-1273. 10.1093/hmg/3.8.1269.
Jefferson JA, Lemmink HH, Hughes AE, Hill CM, Smeets HJ, Doherty CC, Maxwell AP: Autosomal dominant Alport syndrome linked to the type IV collage alpha 3 and alpha 4 genes (COL4A3 and COL4A4). Nephrol Dial Transplant. 1997, 12: 1595-1599. 10.1093/ndt/12.8.1595.
Lemmink HH, Kluijtmans LA, Brunner HG, Schroder CH, Knebelmann B, Jelinkova E, van Oost BA, Monnens LA, Smeets HJ: Aberrant splicing of the COL4A5 gene in patients with Alport syndrome. Hum Mol Genet. 1994, 3: 317-322. 10.1093/hmg/3.2.317.
Stoilov I, Akarsu AN, Sarfarazi M: Identification of three different truncating mutations in cytochrome P4501B1 (CYP1B1) as the principal cause of primary congenital glaucoma (Buphthalmos) in families linked to the GLC3A locus on chromosome 2p21. Hum Mol Genet. 1997, 6: 641-647. 10.1093/hmg/6.4.641.
Mitton KP, Swain PK, Khanna H, Dowd M, Apel IJ, Swaroop A: Interaction of retinal bZIP transcription factor NRL with Flt3-interacting zinc-finger protein Fiz1: possible role of Fiz1 as a transcriptional repressor. Hum Mol Genet. 2003, 12: 365-373. 10.1093/hmg/ddg035.
Xu X, Quiambao AB, Roveri L, Pardue MT, Marx JL, Rohlich P, Peachey NS, Al-Ubaidi MR: Degeneration of cone photoreceptors induced by expression of the Mas1 protooncogene. Exp Neurol. 2000, 163: 207-219. 10.1006/exnr.2000.7370.
Kubota R, Kudoh J, Mashima Y, Asakawa S, Minoshima S, Hejtmancik JF, Oguchi Y, Shimizu N: Genomic organization of the human myocilin gene (MYOC) responsible for primary open angle glaucoma (GLC1A). Biochem Biophys Res Commun. 1998, 242: 396-400. 10.1006/bbrc.1997.7972.
Pennesi ME, Cho JH, Yang Z, Wu SH, Zhang J, Wu SM, Tsai MJ: BETA2/NeuroD1 null mice: a new model for transcription factor-dependent photoreceptor degeneration. J Neurosci. 2003, 23: 453-461.
Liu B, Neufeld AH: Expression of nitric oxide synthase-2 (NOS-2) in reactive astrocytes of the human glaucomatous optic nerve head. Glia. 2000, 30: 178-186. 10.1002/(SICI)1098-1136(200004)30:2<178::AID-GLIA7>3.0.CO;2-C.
Leveillard T, Mohand-Said S, Lorentz O, Hicks D, Fintz AC, Clerin E, Simonutti M, Forster V, Cavusoglu N, Chalmel F, Dolle P, Poch O, Lambrou G, Sahel JA: Identification and characterization of rod-derived cone viability factor. Nat Genet. 2004, 36: 755-759. 10.1038/ng1386.
Chalmel F, Leveillard T, Jaillard C, Lardenois A, Berdugo N, Morel E, Koehl P, Lambrou G, Holmgren A, Sahel JA, Poch O: Rod-derived Cone Viability Factor-2 is a novel bifunctional-thioredoxin-like protein with therapeutic potential. BMC Mol Biol. 2007, 8: 74-10.1186/1471-2199-8-74.
Tsutsumi M, Ikeyama K, Denda S, Nakanishi J, Fuziwara S, Aoki H, Denda M: Expressions of rod and cone photoreceptor-like proteins in human epidermis. Exp Dermatol. 2009, 18: 567-570. 10.1111/j.1600-0625.2009.00851.x.
Rezaie T, Child A, Hitchings R, Brice G, Miller L, Coca-Prados M, Heon E, Krupin T, Ritch R, Kreutzer D, Crick RP, Sarfarazi M: Adult-onset primary open-angle glaucoma caused by mutations in optineurin. Science. 2002, 295: 1077-1079. 10.1126/science.1066901.
Onishi A, Peng GH, Hsu C, Alexis U, Chen S, Blackshaw S: Pias3-dependent SUMOylation directs rod photoreceptor development. Neuron. 2009, 61: 234-246. 10.1016/j.neuron.2008.12.006.
Montezuma SR, Sobrin L, Seddon JM: Review of genetics in age related macular degeneration. Semin Ophthalmol. 2007, 22: 229-240. 10.1080/08820530701745140.
Murga-Zamalloa CA, Atkins SJ, Peranen J, Swaroop A, Khanna H: Interaction of retinitis pigmentosa GTPase regulator (RPGR) with RAB8A GTPase: implications for cilia dysfunction and photoreceptor degeneration. Hum Mol Genet. 2010, 19: 3591-3598. 10.1093/hmg/ddq275.
Jia L, Oh EC, Ng L, Srinivas M, Brooks M, Swaroop A, Forrest D: Retinoid-related orphan nuclear receptor RORbeta is an early-acting factor in rod photoreceptor development. Proc Natl Acad Sci USA. 2009, 106: 17534-17539. 10.1073/pnas.0902425106.
Daniele LL, Sauer B, Gallagher SM, Pugh EN Jr, Philp NJ: Altered visual function in monocarboxylate transporter 3 (Slc16a8) knockout mice. Am J Physiol Cell Physiol. 2008, 295: C451-457. 10.1152/ajpcell.00124.2008.
Ng L, Hurley JB, Dierks B, Srinivas M, Salto C, Vennstrom B, Reh TA, Forrest D: A thyroid hormone receptor that is required for the development of green cone photoreceptors. Nat Genet. 2001, 27: 94-98.
Valente EM, Logan CV, Mougou-Zerelli S, Lee JH, Silhavy JL, Brancati F, Iannicelli M, Travaglini L, Romani S, Illi B, Adams M, Szymanska K, Mazzotta A, Lee JE, Tolentino JC, Swistun D, Salpietro CD, Fede C, Gabriel S, Russ C, Cibulskis K, Sougnez C, Hildebrandt F, Otto EA, Held S, Diplas BH, Davis EE, Mikula M, Strom CM, Ben-Zeev B, et al: Mutations in TMEM216 perturb ciliogenesis and cause Joubert, Meckel and related syndromes. Nat Genet. 2010, 42: 619-625. 10.1038/ng.594.
Baala L, Romano S, Khaddour R, Saunier S, Smith UM, Audollent S, Ozilou C, Faivre L, Laurent N, Foliguet B, Munnich A, Lyonnet S, Salomon R, Encha-Razavi F, Gubler MC, Boddaert N, de Lonlay P, Johnson CA, Vekemans M, Antignac C, Attie-Bitach T: The Meckel-Gruber syndrome gene, MKS3, is mutated in Joubert syndrome. Am J Hum Genet. 2007, 80: 186-194. 10.1086/510499.
Reichman S, Kalathur RK, Lambard S, Ait-Ali N, Yang Y, Lardenois A, Ripp R, Poch O, Zack DJ, Sahel JA, Leveillard T: The homeobox gene CHX10/VSX2 regulates RdCVF promoter activity in the inner retina. Hum Mol Genet. 2010, 19: 250-261. 10.1093/hmg/ddp484.
Cronin T, Raffelsberger W, Lee-Rivera I, Jaillard C, Niepon ML, Kinzel B, Clerin E, Petrosian A, Picaud S, Poch O, Sahel JA, Leveillard T: The disruption of the rod-derived cone viability gene leads to photoreceptor dysfunction and susceptibility to oxidative stress. Cell Death Differ. 2010, 17: 1199-1210. 10.1038/cdd.2010.2.
Leonard KC, Petrin D, Coupland SG, Baker AN, Leonard BC, LaCasse EC, Hauswirth WW, Korneluk RG, Tsilfidis C: XIAP protection of photoreceptors in animal models of retinitis pigmentosa. PLoS ONE. 2007, 2: e314-10.1371/journal.pone.0000314.
Chakarova CF, Hims MM, Bolz H, Abu-Safieh L, Patel RJ, Papaioannou MG, Inglehearn CF, Keen TJ, Willis C, Moore AT, Rosenberg T, Webster AR, Bird AC, Gal A, Hunt D, Vithana EN, Bhattacharya SS: Mutations in HPRP3, a third member of pre-mRNA splicing factor genes, implicated in autosomal dominant retinitis pigmentosa. Hum Mol Genet. 2002, 11: 87-92. 10.1093/hmg/11.1.87.
Coppieters F, Leroy BP, Beysen D, Hellemans J, De Bosscher K, Haegeman G, Robberecht K, Wuyts W, Coucke PJ, De Baere E: Recurrent mutation in the first zinc finger of the orphan nuclear receptor NR2E3 causes autosomal dominant retinitis pigmentosa. Am J Hum Genet. 2007, 81: 147-157. 10.1086/518426.
Bandah-Rozenfeld D, Littink KW, Ben-Yosef T, Strom TM, Chowers I, Collin RW, den Hollander AI, van den Born LI, Zonneveld MN, Merin S, Banin E, Cremers FP, Sharon D: Novel null mutations in the EYS gene are a frequent cause of autosomal recessive retinitis pigmentosa in the Israeli population. Invest Ophthalmol Vis Sci. 2010, 51: 4387-4394. 10.1167/iovs.09-4732.
Bujakowska K, Audo I, Mohand-Said S, Lancelot ME, Antonio A, Germain A, Leveillard T, Letexier M, Saraiva JP, Lonjou C, Carpentier W, Sahel JA, Bhattacharya SS, Zeitz C: CRB1 mutations in inherited retinal dystrophies. Hum Mutat. 2011, 306-315. 33
Rivera A, White K, Stohr H, Steiner K, Hemmrich N, Grimm T, Jurklies B, Lorenz B, Scholl HP, Apfelstedt-Sylla E, Weber BH: A comprehensive survey of sequence variation in the ABCA4 (ABCR) gene in Stargardt disease and age-related macular degeneration. Am J Hum Genet. 2000, 67: 800-813. 10.1086/303090.
Shroyer NF, Lewis RA, Lupski JR: Analysis of the ABCR (ABCA4) gene in 4-aminoquinoline retinopathy: is retinal toxicity by chloroquine and hydroxychloroquine related to Stargardt disease?. Am J Ophthalmol. 2001, 131: 761-766. 10.1016/S0002-9394(01)00838-8.
Acknowledgements
The authors are grateful to the families described in this study, Dominique Santiard-Baron and Christine Chaumeil for their help in DNA collection and to clinical staff. The project was financially supported by GIS-maladies rares (CZ), Agence Nationale de la Recherche (ANR, SSB), Foundation Voir et Entendre and BQR, Foundation Fighting Blindness (IA, FFB Grant # CD-CL-0808-0466-CHNO and the CIC503 recognized as an FFB center, FFB Grant # C-CMM-0907-0428-INSERM04), Ville de Paris and region Ile de France.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
IA was involved in the study design, participated in the choice of genes, interpreted the NGS data, clinically investigated patients, collected DNA samples, and has been involved in drafting the manuscript. KB participated in the choice of genes, interpreted the NGS data and has been involved in drafting the manuscript. TL was involved in the study design, participated in the choice of genes and has been involved in drafting the manuscript. SM-S clinically investigated patients and collected DNA samples. M-EL confirmed the NGS data by Sanger sequencing, performed control and co-segregation analysis. AG extracted DNA, confirmed the NGS data by Sanger sequencing, and performed control and co-segregation analysis. AA extracted DNA, confirmed the NGS data by Sanger sequencing, and performed control and co-segregation analysis. CM confirmed the NGS data by Sanger sequencing, and performed control and co-segregation analysis. J-PS performed NGS. ML performed the bioinformatic interpretation of NGS. J-AS clinically investigated patients and participated in the study design. SSB participated in the study design and has been involved in drafting the manuscript. CZ has made the study design, participated in the choice of genes, interpreted the NGS data and wrote the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Audo, I., Bujakowska, K.M., Léveillard, T. et al. Development and application of a next-generation-sequencing (NGS) approach to detect known and novel gene defects underlying retinal diseases. Orphanet J Rare Dis 7, 8 (2012). https://doi.org/10.1186/1750-1172-7-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1750-1172-7-8