Abstract
Osteopetrosis ("marble bone disease") is a descriptive term that refers to a group of rare, heritable disorders of the skeleton characterized by increased bone density on radiographs. The overall incidence of these conditions is difficult to estimate but autosomal recessive osteopetrosis (ARO) has an incidence of 1 in 250,000 births, and autosomal dominant osteopetrosis (ADO) has an incidence of 1 in 20,000 births. Osteopetrotic conditions vary greatly in their presentation and severity, ranging from neonatal onset with life-threatening complications such as bone marrow failure (e.g. classic or "malignant" ARO), to the incidental finding of osteopetrosis on radiographs (e.g. osteopoikilosis). Classic ARO is characterised by fractures, short stature, compressive neuropathies, hypocalcaemia with attendant tetanic seizures, and life-threatening pancytopaenia. The presence of primary neurodegeneration, mental retardation, skin and immune system involvement, or renal tubular acidosis may point to rarer osteopetrosis variants, whereas onset of primarily skeletal manifestations such as fractures and osteomyelitis in late childhood or adolescence is typical of ADO. Osteopetrosis is caused by failure of osteoclast development or function and mutations in at least 10 genes have been identified as causative in humans, accounting for 70% of all cases. These conditions can be inherited as autosomal recessive, dominant or X-linked traits with the most severe forms being autosomal recessive. Diagnosis is largely based on clinical and radiographic evaluation, confirmed by gene testing where applicable, and paves the way to understanding natural history, specific treatment where available, counselling regarding recurrence risks, and prenatal diagnosis in severe forms. Treatment of osteopetrotic conditions is largely symptomatic, although haematopoietic stem cell transplantation is employed for the most severe forms associated with bone marrow failure and currently offers the best chance of longer-term survival in this group. The severe infantile forms of osteopetrosis are associated with diminished life expectancy, with most untreated children dying in the first decade as a complication of bone marrow suppression. Life expectancy in the adult onset forms is normal. It is anticipated that further understanding of the molecular pathogenesis of these conditions will reveal new targets for pharmacotherapy.
Similar content being viewed by others
Disease name and synonyms
The term osteopetrosis is derived from the Greek 'osteo' meaning bone and 'petros', stone. Osteopetrosis is variably referred to as 'marble bone disease' and 'Albers-Schönberg disease', after the German radiologist credited with the first description of the condition in 1904 [1].
Definition and classification
Osteopetrosis comprises a clinically and genetically heterogeneous group of conditions that share the hallmark of increased bone density on radiographs. The increase in bone density results from abnormalities in osteoclast differentiation or function. The Nosology Group of the International Skeletal Dysplasia Society classifies increased bone density conditions into several distinct entities based on clinical features, mode of inheritance and underlying molecular and pathogenetic mechanisms (Table 1) [2].
Epidemiology
These conditions are rare, and their overall incidence is difficult to estimate. Autosomal recessive osteopetrosis has an incidence of 1 in 250,000 births, with a particularly high incidence reported in Costa Rica (3.4:100,000) [3]. Autosomal dominant osteopetrosis has an incidence of 5:100,000 births [4].
Clinical descriptions
Osteopetrosis encompasses a group of highly heterogeneous conditions, ranging in severity from asymptomatic to fatal in infancy. The more severe forms tend to have autosomal recessive inheritance, while the mildest forms are observed in adults and are inherited in an autosomal dominant manner.
The increased bone mass can result in phenotypic features such as macrocephaly and altered craniofacial morphology, but more importantly impacts on other organs and tissues, notably the bone marrow and nervous systems. The key clinical manifestations, onset, severity, treatment, prognosis and recurrence risks for the main types of osteopetrosis are summarised in Table 2.
Autosomal recessive ("malignant") osteopetrosis (ARO) is a life-threatening condition, which classically manifests in the first few months of life. The increase in bone density can paradoxically weaken the bone, resulting in a predisposition to fractures and osteomyelitis. The longitudinal growth of bones is impaired, resulting in short stature of varying degrees. Macrocephaly and frontal bossing develop within the first year, resulting in a typical facial appearance. The skull changes can result in choanal stenosis and hydrocephalus [5]. The expanding bone can narrow nerve foramina, resulting in blindness, deafness, and facial palsy. Hearing loss is estimated to affect 78% of individuals with ARO [6]. Tooth eruption defects and severe dental caries are also common. Children with ARO are at risk of developing hypocalcaemia, with attendant tetanic seizures and secondary hyperparathyroidism. The most severe complication of ARO is bone marrow suppression. The abnormal expansion of bone interferes with medullary haematopoiesis, resulting in life-threatening pancytopaenia, and secondary expansion of extramedullary haematopoiesis sites such as the liver and spleen.
ARO variants. It is important to differentiate classic ARO from some of the rarer variants. Neuropathic ARO is characterised by seizures in the setting of normal calcium levels, developmental delay, hypotonia, retinal atrophy with absent evoked visual potentials and sensorineural deafness [7]. It is due to primary neurodegeneration not dissimilar to neuronal ceroid-lipofuschinosis, a lysosomal storage disorder [8]. Reported brain MRI findings include significantly delayed myelinisation, diffuse progressive cortical and subcortical atrophy, and bilateral atrial subependymal heterotopias [7]. Electron microscopy of skin biopsies reveals swollen unmyelinated axons that contain spheroids, reduced numbers of myelinated axons and the presence of secondary lipofuscin-containing lysosomes in Schwann cells [9].
ARO with renal tubular acidosis (RTA) has a milder course where RTA and cerebral calcifications are typical [10]. Other clinical manifestations comprise an increased frequency of fractures, short stature, dental abnormalities, cranial nerve compression and developmental delay [11].
The presence of severe immunodeficiency with ectodermal changes is observed in X-linked osteopetrosis, lymphedema, anhidrotic ectodermal dysplasia and immunodeficiency (OLEDAID). Common variable immune deficiency (CVID) has been described in association with a particular subtype of osteoclast-poor ARO [12], and some patients with leukocyte adhesion deficiency syndrome (LAD-III) also suffer from severe osteopetrosis [13, 14].
Autosomal dominant osteopetrosis (Albers-Schönberg disease) typically has onset in late childhood or adolescence, and classically displays the radiographic sign of "sandwich vertebrae" (dense bands of sclerosis parallel to the vertebral endplates – Figure 1). The main complications are confined to the skeleton, including fractures, scoliosis, hip osteoarthritis and osteomyelitis, particularly affecting the mandible in association with dental abscess or caries [15]. Cranial nerve compression is a rare but important complication, with hearing and visual loss affecting around 5% of individuals.
Pycnodysostosis was first described by Maroteaux and Lamy in 1962 [16], and there is evidence that the French painter Henri de Toulouse-Lautrec [17] and the ancient Greek author Aesop [18] were afflicted by this condition. Pycnodysostosis is characterised by short stature, increased bone fragility, persistent open anterior fontanelle and acro-osteolysis of the terminal phalanges (Figure 2). The typical 'open mouth outline' facial appearance is due to frontal bossing, micrognatia, loss of the mandibular angle (Figure 3), and dental anomalies including persistence of deciduous teeth resulting a double row of teeth [19, 20]. Other reported manifestations include joint hypermobility, obliteration of frontal and other sinuses [21], pituitary hypoplasia, cerebral demyelination [22], and hepatosplenomegaly [23].
Dysosteosclerosis was first described as a separate condition in 1968 [24] and is marked by the presence of skin changes (red-violet spots in a patchy distribution), developmental regression and an overall poor prognosis. It manifests in infancy and can be distinguished from other osteopetrotic conditions by platyspondyly, bowing of the long bones, and the lack of bone marrow involvement or acro-osteolysis [25]. Typically, the expanded areas of bone are relatively radiolucent, in contrast to the sclerosis of expanded areas seen in ARO [25].
Osteopoikilosis is a benign, usually asymptomatic condition diagnosed radiographically by the presence of multiple symmetrical circular/ovoid sclerotic opacities of the ischiae, pubic bones and the epimetaphysial regions of the short tubular bones. Osteopoikilosis can occur in isolation, or in association with elastic or collagen connective tissue naevi of the skin, a condition termed Buschke-Ollendorff syndrome (BOS). Both osteopoikilosis and BOS are inherited in an autosomal dominant pattern. In some families and individuals, osteopoikilosis can also occur in association with melorheostosis [26–29]. Melorheostosis is usually a sporadic sclerosing bone condition manifesting in a sclerotomal distribution, frequently affecting one limb. There is cortical hyperostosis with thickening, which resembles dripping candle wax on radiographs. Melorheostosis can be asymptomatic or if severe can result in pain, stiffness, leg-length discrepancy and deformity.
Osteopathia striata (OS) occurs in isolation or with cranial sclerosis (OS-CS). The key feature is longitudinal striation of the metaphyses of the long bones [30]. OS-CS in particular is a clinically heterogeneous condition, ranging from mild skeletal manifestations to multisystem organ involvement even within the same family [31]. The typical clinical features include macrocephaly, cleft palate and hearing loss; additional features including cardiac malformations, developmental delay, cranial nerve palsies, anal malformations, cataracts and nervous system malformations have been reported.
Aetiology
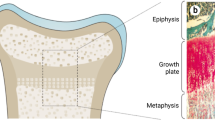
Osteopetrosis is caused by failure of osteoclast differentiation or function and mutations in at least 10 genes have been identified as causative in humans (Table 1). The pathogenesis of osteopetrosis is best understood with reference to normal osteoclast development and function (Figure 4).
Current model of the pathogenesis of osteopetrotic conditions in relation to normal osteoclast function, modified from Del Fattore et al [77] (ER: endoplasmic reticulum, ARO: autosomal recessive osteopetrosis, RTA: renal tubular acidosis).
Osteoclasts are highly specialised cells, which degrade bone mineral and organic bone matrix. These processes are crucial for bone remodelling and the maintenance of bone biomechanical stability and mineral homeostasis. It is estimated that the adult skeleton is completely regenerated every 10 years [32]. Osteoclasts are derived from the mononuclear precursors in the myeloid lineage of haematopoietic cells that also give rise to macrophages [33]. The osteoclast precursors fuse, resulting in osteoclasts, which typically have 5–8 nuclei. By contrast, osteoblasts are derived from multipotent mesenchymal stem cells, which also give rise to chondrocytes, adipocytes and muscle cells.
In light of the common origin of osteoclasts and cells of the haematopoietic system, it is not surprising that mutations in molecules such as IKBKG(NEMO) [34] and more recently CalDAG-GEF1 [13] and kindlin-3 [14] have been implicated in the pathogenesis of ARO variants associated with immune system dysfunction. Other important signals for osteoclast differentiation include the ligand of receptor activator of nuclear factor-kappa B (RANKL) and M-CSF. Op/op mice which do not express functional M-CSF lack osteoclasts and have osteopetrosis [35], however human patients with osteopetrosis secondary to M-CSF deficiency are yet to be identified. Recently a kindred with RANKL gene mutation [36], and seven families with RANK gene mutation [12] and osteopetrosis have been described. Failure of osteoclast differentiation as a result of mutations in these genes accounts for the rare osteoclast-poor forms of ARO, in which no mature osteoclasts are present.
A fully differentiated osteoclast dissolves bone mineral and degrades bone matrix using specialised enzymes. Crucial to this function is cell polarisation, and in particular the formation of the ruffled border and sealing zone. These form the resorption lacuna where hydrochloric acid is actively secreted resulting in the dissolution of bone mineral hydroxyapatite.
Most forms of osteoclast-rich osteopetrosis are caused by defects in gene products involved in the acidification machinery. Acid secretion is dependent on two key molecules, which facilitate proton transport: the proton pump vacuolar ATPase (V-ATPase) and the chloride-specific ion channel, chloride channel 7 (CLCN-7) [37]. Homozygous mutations in the genes encoding the a3 subunit of V-ATPase (TCIRG1) and the CLCN-7 produce severe malignant osteopetrosis phenotypes in both humans and mice [37–40]. TCIRG1 mutations are responsible for autosomal recessive osteopetrosis in more than 50% of affected individuals [38, 41] underscoring the crucial role of V-ATPase in osteoclast function. CLCN-7 on the other hand plays a key role in lysosomal acidification, which explains the severe neuronal storage and neurodegeneration in the CNS and retina in Clcn7-/- mice and in a subset of human ARO patients [8, 42]. Dominant-negative mutations of CLCN-7 have been shown to cause ADO [43]. CLCN-7 is closely associated with another membrane protein, OSTM1 [44]. Mutations in the OSTM1 gene are found in grey-lethal mice and a subset of ARO patients with neurological involvement [45, 46].
The protons and chloride ions that are expended in the acidification process need to be replenished intracellularly in order to avoid alkanization. This is achieved by carbonic anhydrase type II (CAII) and an anion exchanger. Given the key role of CAII in kidney function, it is not surprising that mutations in CAII result in ARO with tubular acidosis [47].
The collagen bone matrix is dissolved by two groups of enzymes, the matrix metalloproteinases (MMPs) and lysosomal cathepsins. Cathepsin K in particular has been identified as a key enzyme. It is secreted in the resorption lacuna [48, 49] where it degrades collagen I at acidic pH. Inhibition of cathepsin K prevents matrix degradation [50, 51], and deletion of the cathepsin K gene in mice leads to osteopetrosis [52, 53]. Homozygous mutations in the human cathepsin K gene lead to pycnodysostosis [54, 55].
The formation and maintenance of the osteoclast polarised membrane domains requires complex vesicular trafficking mechanisms and continuous remodelling of the osteoclast cytoskeleton. One protein, which plays a critical function in vesicle trafficking and acidification is PLEKHM1, and heterozygous mutations in this have been associated with intermediate forms of osteopetrosis [56, 57].
Other signalling pathways are likely to be important in osteoclast function, and mutations in the LEMD3 gene which codes for an integral protein of the inner nuclear membrane thought to be involved in BMP and TGFβ signalling, result in osteopoikilosis, Buschke-Ollendorff syndrome and melorheostosis [58, 59]. WNT-related signalling defects (of PORCN [60, 61] and WTX [62] genes) have recently been associated with hyperostotic phenotypes (osteopathia striata in Goltz syndrome and Osteopathia Striata with Cranial Stenosis, OSCS, respectively) implying a role for the WNT pathway in osteoclast function.
Mutations in genes described so far only account for approximately 70% of cases and the search continues for the genes responsible for the remainder. The field of osteopetrosis research has benefited from the many naturally occurring rodent models of the disease. Many genetic defects observed in rodents have not been observed in humans, and these form natural targets for future studies.
Diagnosis
The mainstay of diagnosis is clinical and largely depends on the radiographic appearance of the skeleton. The classic radiological features of osteopetrosis comprise:
• Diffuse sclerosis, affecting the skull, spine, pelvis and appendicular bones.
• Bone modelling defects at the metaphyses of long bones, such as funnel-like appearance ("Erlenmeyer flask" deformity) (Figure 5), and characteristic lucent bands (Figure 6).
• "Bone-in-bone" appearance particularly in the vertebrae and phalanges.
• Focal sclerosis of the skull base, pelvis and vertebral end plates – "sandwich" vertebrae (Figure 1) and "rugger-jersey" spine.
In the absence of typical radiographic findings, raised concentrations of the creatine kinase BB isoenzyme and tartrate resistant acid phosphatase (TRAP) can be helpful in making the diagnosis of ADO [63–65].
Age of onset, inheritance pattern and the presence of associated features, such as neurodegeneration, mental retardation, skin and immune system involvement, or renal tubular acidosis may point to particular subtypes of osteopetrosis. Bone biopsy can distinguish between osteoclast-poor and osteoclast-rich subtypes of ARO; however this is invasive and rarely performed.
Genetic testing is available either clinically or on a research basis for many of the genes implicated in osteopetrotic conditions. Genetic testing can be used to confirm the diagnosis and differentiate between different subtypes of osteopetrosis, providing additional information regarding prognosis, likely response to treatment and recurrence risks.
Differential diagnosis
Primary sclerosing conditions of bone caused by osteoclast dysfunction need to be distinguished from the large number of conditions in which bone sclerosis can occur as a secondary phenomenon. Some alternative diagnoses to consider include fluorosis; beryllium, lead and bismuth poisoning; myelofibrosis; Paget's disease (sclerosing form); and malignancies (lymphoma, osteoblastic cancer metastases). Neonatal radiographs can be particularly difficult to interpret in the absence of additional multiorgan involvement, as the normal neonatal skeleton can appear denser than normal. However, in contrast to osteopetrosis, this appearance will improve over time.
Once the diagnosis of a primary osteopetrotic condition is made, it is important to distinguish between different subtypes as they have different response to treatment, prognosis and recurrence risks.
Genetic counselling
Osteopetrosis is a trait that can be inherited in an autosomal dominant, autosomal recessive or X-linked manner, and genetic counselling will depend on the mode of inheritance in a particular family.
Autosomal recessive: the parents of the proband have a 1 in 4 (25%) risk of having further affected children in each pregnancy. 2/3 of unaffected siblings are expected to be carriers. Given the low incidence of osteopetrosis in the general population, the risk that the proband or their siblings would have affected children is low.
Autosomal dominant: the parents of the proband should be carefully evaluated for signs of osteopetrosis, including radiographic studies of the skeleton. Each child of an affected individual has a 1 in 2 (50%) risk of being affected. If the parents are unaffected, there may still be a low risk of further affected children due to gonadal mosaicism.
X-linked recessive: if the mother of the proband is a carrier, 50% of male pregnancies will be affected, and 50% of female pregnancies will be carriers. If the mother is not a carrier, there may still be a small risk of further affected offspring due to gonadal mosaicism.
Antenatal diagnosis
Pre-implantation and prenatal diagnosis is theoretically possible in families, in whom the genetic mutation has been identified, thus allowing for reproductive decisions to be made. In families with severe ARO and unknown mutations, pre-natal diagnosis may be possible using radiographs [66]. If a family decides to continue with an affected pregnancy, haematopoietic stem cell transplantation (HSCT) before the age of 3 months can be planned with the aim of improving neurological outcomes.
Management including treatment
At present, no effective medical treatment for osteopetrosis exists. Treatment is largely supportive and is aimed at providing multidisciplinary surveillance and symptomatic management of complications. Fractures and arthritis are common and require treatment by an experienced orthopaedic surgeon due to the brittleness of the bone, and the relatively frequent occurrence of secondary complications such as delayed union or non-union of fractures and osteomyelitis [67]. Hypocalcaemic seizures are treated with calcium and vitamin D supplementation, and bone marrow failure with red blood cell and platelet transfusions. Developmental delay and seizures in the setting of normal calcium levels may be indicative of neuropathic ARO and should prompt a formal neurological evaluation (including brain MRI, and EEG). Regular ophthalmologic surveillance including visual evoked potentials (VEPs) is important in detecting optic nerve atrophy. Surgical decompression of the optic nerve has been performed to prevent vision loss [68]. Dental problems such as delayed tooth eruption, ankylosis, abscesses, cysts and fistulas are common. Therefore, routine dental surveillance and maintenance of oral hygiene form an integral part of management and play an important role in preventing more severe complications such as osteomyelitis of the mandible.
Given the high associated morbidity and mortality, HSCT is reserved for the severe forms of ARO. HSCT using HLA-identical donors results in 73% 5-year disease-free survival [69]. Complications include rejection, delayed haematopoietic reconstitution, venous occlusive disease, pulmonary hypertension and hypercalcaemic crisis [70]. Furthermore HSCT does not necessarily reverse complications: retrospective report of HSCT in osteopetrosis [69] showed that only 7% of survivors experienced improvement in vision, whereas 69% had no further deterioration and 25% experienced further deterioration. HSCT had no effect on linear growth. Outcomes were better with earlier transplantation, particularly before the age of 3 months and of note, rescue of a malignant osteopetrosis mouse model by HSCT in utero has been demonstrated [71].
HSCT does not alter outcome in subtypes of osteopetrosis associated with primary rather than compressive neuropathy, such as autosomal recessive forms caused by CLCN7 and OSTM1 gene mutations. Other types of osteopetrosis that do not benefit from HSCT include those caused by absence rather than impaired function of osteoclasts (e.g. RANKL mutations) [36].
Interferon gamma 1b (IFNγ1b) treatment has been attempted in patients with osteopetrosis variants unlikely to respond to HSCT or as a bridge to transplantation. It has been reported to result in improvement in immune function, increase in bone resorption and increase in bone marrow space [72, 73]. Stimulation of host osteoclasts with calcium restriction, calcitrol, steroids, parathyroid hormone and interferon has also been attempted [74, 75].
Prognosis
The severe infantile forms of osteopetrosis are associated with diminished life expectancy, with most untreated children dying in the first decade as a complication of bone marrow suppression. Life expectancy in the adult onset forms is normal.
Unresolved questions
Despite recent advances in the understanding of the pathogenesis of osteopetrotic conditions, the genetic basis of approximately 30% of cases remains to be elucidated. The other major challenge in this group of conditions remains effective treatment of the severe recessive disorders and of complications such as optic and other cranial nerve compression. It is hoped that ongoing research into osteoclast physiology will result in novel therapeutic targets. For example, low levels of bone resorption are observed in even severely affected patients, pointing to the presence of multiple acidification mechanisms. The activation of alternative acidification mechanisms, including the Na+/H+ antiporter [65] have been proposed as potential therapeutic targets. The recent identification of RANKL-deficient patients has raised the possibility that this subgroup of patients would benefit from the administration of recombinant RANKL or from mesenchymal stem cell transplantation (MSCT)[76]. Feasibility studies of these approaches in animal studies are eagerly awaited.
References
Albers-Schonberg: Rontgenbilder einer seltenen Knockenerkrankung. Munch Med Wochenschr. 1904, 5: 365-368.
Superti-Furga A US, and the Nosology Group of the International Skeletal Dysplasia Society: Nosology and Classification of Genetic Skeletal Disorders: 2006 Revision. American Journal of Medical Genetics Part A. 2007, 143A: 1-18. 10.1002/ajmg.a.31483.
Loria-Cortes R, Quesada-Calvo E, Cordero-Chaverri C: Osteopetrosis in children: a report of 26 cases. J Pediatr. 1977, 91: 43-47. 10.1016/S0022-3476(77)80441-1.
Bollerslev J, Andersen PE: Radiological, biochemical and hereditary evidence of two types of autosomal dominant osteopetrosis. Bone. 1988, 9: 7-13. 10.1016/8756-3282(88)90021-X.
Al-Tamimi YZ, Tyagi AK, Chumas PD, Crimmins DW: Patients with autosomal-recessive osteopetrosis presenting with hydrocephalus and hindbrain posterior fossa crowding. J Neurosurg Pediatrics. 2008, 1: 103-106. 10.3171/PED-08/01/103.
Dozier TS, Duncan IM, Klein AJ, Lambert PR, Key LL: Otologic manifestations of malignant osteopetrosis. Otol Neurotol. 2005, 26: 762-766. 10.1097/01.mao.0000178139.27472.8d.
Maranda B, Chabot G, Decarie JC, Pata M, Azeddine B, Moreau A, Vacher J: Clinical and cellular manifestations of OSTM1-related infantile osteopetrosis. J Bone Miner Res. 2008, 23: 296-300. 10.1359/jbmr.071015.
Steward CG: Neurological aspects of osteopetrosis. Neuropathol Appl Neurobiol. 2003, 29: 87-97. 10.1046/j.1365-2990.2003.00474.x.
Alroy J, Pfannl R, Ucci A, Lefranc G, Frattini A, Megarbane A: Electron microscopic findings in skin biopsies from patients with infantile osteopetrosis and neuronal storage disease. Ultrastruct Pathol. 2007, 31: 333-338. 10.1080/01913120701578098.
Jacquemin C, Mullaney P, Svedberg E: Marble brain syndrome: osteopetrosis, renal acidosis and calcification of the brain. Neuroradiology. 1998, 40: 662-663. 10.1007/s002340050660.
Whyte MP: Carbonic anhydrase II deficiency. Clin Orthop Relat Res. 1993, 52-63.
Guerrini MM, Sobacchi C, Cassani B, Abinun M, Kilic SS, Pangrazio A, Moratto D, Mazzolari E, Clayton-Smith J, Orchard P: Human osteoclast-poor osteopetrosis with hypogammaglobulinemia due to TNFRSF11A (RANK) mutations. Am J Hum Genet. 2008, 83: 64-76. 10.1016/j.ajhg.2008.06.015.
Kilic SS, Etzioni A: The Clinical Spectrum of Leukocyte Adhesion Deficiency (LAD) III due to Defective CalDAG-GEF1. J Clin Immunol. 2008
Mory A, Feigelson SW, Yarali N, Kilic SS, Bayhan GI, Gershoni-Baruch R, Etzioni A, Alon R: Kindlin-3: a new gene involved in the pathogenesis of LAD-III. Blood. 2008, 112: 2591-10.1182/blood-2008-06-163162.
Benichou OD, Laredo JD, de Vernejoul MC: Type II autosomal dominant osteopetrosis (Albers-Schonberg disease): clinical and radiological manifestations in 42 patients. Bone. 2000, 26: 87-93. 10.1016/S8756-3282(99)00244-6.
Maroteaux P, Lamy M: [Pyknodysostosis.]. Presse Med. 1962, 70: 999-1002.
Maroteaux P, Lamy M: The Malady of Toulouse-Lautrec. Jama. 1965, 191: 715-717.
Bartsocas CS: Pycnodysostosis: Toulouse-Lautrec's and Aesop's disease?. Hormones (Athens). 2002, 1: 260-262. 10.1159/000068796.
Edelson JG, Obad S, Geiger R, On A, Artul HJ: Pycnodysostosis. Orthopedic aspects with a description of 14 new cases. Clin Orthop Relat Res. 1992, 263-276.
Muto T, Michiya H, Taira H, Murase H, Kanazawa M: Pycnodysostosis. Report of a case and review of the Japanese literature, with emphasis on oral and maxillofacial findings. Oral Surg Oral Med Oral Pathol. 1991, 72: 449-455. 10.1016/0030-4220(91)90559-U.
Jones CM, Rennie JS, Blinkhorn AS: Pycnodysostosis. A review of reported dental abnormalities and a report of the dental findings in two cases. Br Dent J. 1988, 164: 218-220. 10.1038/sj.bdj.4806405.
Soliman AT, Ramadan MA, Sherif A, Aziz Bedair ES, Rizk MM: Pycnodysostosis: clinical, radiologic, and endocrine evaluation and linear growth after growth hormone therapy. Metabolism. 2001, 50: 905-911. 10.1053/meta.2001.24924.
Baker RK, Wallach S, Tashjian AH: Plasma calcitonin in pycnodysostosis: intermittently high basal levels and exaggerated responses to calcium and glucagon infusions. J Clin Endocrinol Metab. 1973, 37: 46-55.
Spranger J, Albrecht C, Rohwedder HJ, Wiedemann HR: [Dysosteosclerosis – a special form of generalized osteosclerosis]. Fortschr Geb Rontgenstr Nuklearmed. 1968, 109: 504-512.
Elcioglu NH, Vellodi A, Hall CM: Dysosteosclerosis: a report of three new cases and evolution of the radiological findings. J Med Genet. 2002, 39: 603-607. 10.1136/jmg.39.8.603.
Ghai S, Sharma R, Ghai S: Mixed sclerosing bone dysplasia – a case report with literature review. Clin Imaging. 2003, 27: 203-205. 10.1016/S0899-7071(02)00516-8.
Butkus CE, Michels VV, Lindor NM, Cooney WP: Melorheostosis in a patient with familial osteopoikilosis. Am J Med Genet. 1997, 72: 43-46. 10.1002/(SICI)1096-8628(19971003)72:1<43::AID-AJMG9>3.0.CO;2-W.
Debeer P, Pykels E, Lammens J, Devriendt K, Fryns JP: Melorheostosis in a family with autosomal dominant osteopoikilosis: report of a third family. Am J Med Genet A. 2003, 119A: 188-193. 10.1002/ajmg.a.20072.
Nevin NC, Thomas PS, Davis RI, Cowie GH: Melorheostosis in a family with autosomal dominant osteopoikilosis. Am J Med Genet. 1999, 82: 409-414. 10.1002/(SICI)1096-8628(19990219)82:5<409::AID-AJMG10>3.0.CO;2-2.
Voorhoeve N: L'image radiologique non encore decrit d'une anomalie du squelette; ses rapports avec la dyschondroplasie et l'osteopathia condensans disseminata. Acta Radiol. 1924, 3: 407-427. 10.3109/00016922409133734.
Savarirayan R, Nance J, Morris L, Haan E, Couper R: Osteopathia striata with cranial sclerosis: highly variable phenotypic expression within a family. Clin Genet. 1997, 52: 199-205.
Manolagas SC: Birth and death of bone cells: basic regulatory mechanisms and implications for the pathogenesis and treatment of osteoporosis. Endocr Rev. 2000, 21: 115-137. 10.1210/er.21.2.115.
Walker DG: The classic: Osteopetrosis cured by temporary parabiosis. Clin Orthop Relat Res. 1982, 2-3.
Doffinger R, Smahi A, Bessia C, Geissmann F, Feinberg J, Durandy A, Bodemer C, Kenwrick S, Dupuis-Girod S, Blanche S: X-linked anhidrotic ectodermal dysplasia with immunodeficiency is caused by impaired NF-kappaB signaling. Nat Genet. 2001, 27: 277-285. 10.1038/85837.
Yoshida H, Hayashi S, Kunisada T, Ogawa M, Nishikawa S, Okamura H, Sudo T, Shultz LD, Nishikawa S: The murine mutation osteopetrosis is in the coding region of the macrophage colony stimulating factor gene. Nature. 1990, 345: 442-444. 10.1038/345442a0.
Sobacchi C, Frattini A, Guerrini MM, Abinun M, Pangrazio A, Susani L, Bredius R, Mancini G, Cant A, Bishop N: Osteoclast-poor human osteopetrosis due to mutations in the gene encoding RANKL. Nat Genet. 2007, 39: 960-962. 10.1038/ng2076.
Kornak U, Kasper D, Bosl MR, Kaiser E, Schweizer M, Schulz A, Friedrich W, Delling G, Jentsch TJ: Loss of the ClC-7 chloride channel leads to osteopetrosis in mice and man. Cell. 2001, 104: 205-215. 10.1016/S0092-8674(01)00206-9.
Frattini A, Orchard PJ, Sobacchi C, Giliani S, Abinun M, Mattsson JP, Keeling DJ, Andersson AK, Wallbrandt P, Zecca L: Defects in TCIRG1 subunit of the vacuolar proton pump are responsible for a subset of human autosomal recessive osteopetrosis. Nat Genet. 2000, 25: 343-346. 10.1038/77131.
Kornak U, Schulz A, Friedrich W, Uhlhaas S, Kremens B, Voit T, Hasan C, Bode U, Jentsch TJ, Kubisch C: Mutations in the a3 subunit of the vacuolar H(+)-ATPase cause infantile malignant osteopetrosis. Hum Mol Genet. 2000, 9: 2059-2063. 10.1093/hmg/9.13.2059.
Li YP, Chen W, Liang Y, Li E, Stashenko P: Atp6i-deficient mice exhibit severe osteopetrosis due to loss of osteoclast-mediated extracellular acidification. Nat Genet. 1999, 23: 447-451. 10.1038/70563.
Sobacchi C, Frattini A, Orchard P, Porras O, Tezcan I, Andolina M, Babul-Hirji R, Baric I, Canham N, Chitayat D: The mutational spectrum of human malignant autosomal recessive osteopetrosis. Hum Mol Genet. 2001, 10: 1767-1773. 10.1093/hmg/10.17.1767.
Kasper D, Planells-Cases R, Fuhrmann JC, Scheel O, Zeitz O, Ruether K, Schmitt A, Poet M, Steinfeld R, Schweizer M: Loss of the chloride channel ClC-7 leads to lysosomal storage disease and neurodegeneration. Embo J. 2005, 24: 1079-1091. 10.1038/sj.emboj.7600576.
Cleiren E, Benichou O, Van Hul E, Gram J, Bollerslev J, Singer FR, Beaverson K, Aledo A, Whyte MP, Yoneyama T: Albers-Schonberg disease (autosomal dominant osteopetrosis, type II) results from mutations in the ClCN7 chloride channel gene. Hum Mol Genet. 2001, 10: 2861-2867. 10.1093/hmg/10.25.2861.
Lange PF, Wartosch L, Jentsch TJ, Fuhrmann JC: ClC-7 requires Ostm1 as a beta-subunit to support bone resorption and lysosomal function. Nature. 2006, 440: 220-223. 10.1038/nature04535.
Chalhoub N, Benachenhou N, Vacher J: Physical and transcriptional map of the mouse Chromosome 10 proximal region syntenic to human 6q16-q21. Mamm Genome. 2001, 12: 887-892. 10.1007/s00335-001-1014-5.
Ramirez A, Faupel J, Goebel I, Stiller A, Beyer S, Stockle C, Hasan C, Bode U, Kornak U, Kubisch C: Identification of a novel mutation in the coding region of the grey-lethal gene OSTM1 in human malignant infantile osteopetrosis. Hum Mutat. 2004, 23: 471-476. 10.1002/humu.20028.
Sly WS, Hewett-Emmett D, Whyte MP, Yu YS, Tashian RE: Carbonic anhydrase II deficiency identified as the primary defect in the autosomal recessive syndrome of osteopetrosis with renal tubular acidosis and cerebral calcification. Proc Natl Acad Sci USA. 1983, 80: 2752-2756. 10.1073/pnas.80.9.2752.
Everts V, Korper W, Hoeben KA, Jansen ID, Bromme D, Cleutjens KB, Heeneman S, Peters C, Reinheckel T, Saftig P, Beertsen W: Osteoclastic bone degradation and the role of different cysteine proteinases and matrix metalloproteinases: differences between calvaria and long bone. J Bone Miner Res. 2006, 21: 1399-1408. 10.1359/jbmr.060614.
Troen BR: The regulation of cathepsin K gene expression. Ann N Y Acad Sci. 2006, 1068: 165-172. 10.1196/annals.1346.018.
Bossard MJ, Tomaszek TA, Thompson SK, Amegadzie BY, Hanning CR, Jones C, Kurdyla JT, McNulty DE, Drake FH, Gowen M, Levy MA: Proteolytic activity of human osteoclast cathepsin K. Expression, purification, activation, and substrate identification. J Biol Chem. 1996, 271: 12517-12524. 10.1074/jbc.271.21.12517.
Votta BJ, Levy MA, Badger A, Bradbeer J, Dodds RA, James IE, Thompson S, Bossard MJ, Carr T, Connor JR: Peptide aldehyde inhibitors of cathepsin K inhibit bone resorption both in vitro and in vivo. J Bone Miner Res. 1997, 12: 1396-1406. 10.1359/jbmr.1997.12.9.1396.
Saftig P, Hunziker E, Wehmeyer O, Jones S, Boyde A, Rommerskirch W, Moritz JD, Schu P, von Figura K: Impaired osteoclastic bone resorption leads to osteopetrosis in cathepsin-K-deficient mice. Proc Natl Acad Sci USA. 1998, 95: 13453-13458. 10.1073/pnas.95.23.13453.
Gowen M, Lazner F, Dodds R, Kapadia R, Feild J, Tavaria M, Bertoncello I, Drake F, Zavarselk S, Tellis I: Cathepsin K knockout mice develop osteopetrosis due to a deficit in matrix degradation but not demineralization. J Bone Miner Res. 1999, 14: 1654-1663. 10.1359/jbmr.1999.14.10.1654.
Gelb BD, Shi GP, Chapman HA, Desnick RJ: Pycnodysostosis, a lysosomal disease caused by cathepsin K deficiency. Science. 1996, 273: 1236-1238. 10.1126/science.273.5279.1236.
Johnson MR, Polymeropoulos MH, Vos HL, Ortiz de Luna RI, Francomano CA: A nonsense mutation in the cathepsin K gene observed in a family with pycnodysostosis. Genome Res. 1996, 6: 1050-1055. 10.1101/gr.6.11.1050.
Van Wesenbeeck L, Odgren PR, Coxon FP, Frattini A, Moens P, Perdu B, MacKay CA, Van Hul E, Timmermans JP, Vanhoenacker F: Involvement of PLEKHM1 in osteoclastic vesicular transport and osteopetrosis in incisors absent rats and humans. J Clin Invest. 2007, 117: 919-930. 10.1172/JCI30328.
van Wesenbeeck L, Odgren PR, Mackay CA, Van Hul W: Localization of the gene causing the osteopetrotic phenotype in the incisors absent (ia) rat on chromosome 10q32.1. J Bone Miner Res. 2004, 19: 183-189. 10.1359/jbmr.2004.19.2.183.
Hellemans J, Preobrazhenska O, Willaert A, Debeer P, Verdonk PC, Costa T, Janssens K, Menten B, Van Roy N, Vermeulen SJ: Loss-of-function mutations in LEMD3 result in osteopoikilosis, Buschke-Ollendorff syndrome and melorheostosis. Nat Genet. 2004, 36: 1213-1218. 10.1038/ng1453.
Hellemans J, Debeer P, Wright M, Janecke A, Kjaer KW, Verdonk PC, Savarirayan R, Basel L, Moss C, Roth J: Germline LEMD3 mutations are rare in sporadic patients with isolated melorheostosis. Hum Mutat. 2006, 27: 290-10.1002/humu.9403.
Grzeschik KH, Bornholdt D, Oeffner F, Konig A, del Carmen Boente M, Enders H, Fritz B, Hertl M, Grasshoff U, Hofling K: Deficiency of PORCN, a regulator of Wnt signaling, is associated with focal dermal hypoplasia. Nat Genet. 2007, 39: 833-835. 10.1038/ng2052.
Wang X, Reid Sutton V, Omar Peraza-Llanes J, Yu Z, Rosetta R, Kou YC, Eble TN, Patel A, Thaller C, Fang P, Veyver Van den IB: Mutations in X-linked PORCN, a putative regulator of Wnt signaling, cause focal dermal hypoplasia. Nat Genet. 2007, 39: 836-838. 10.1038/ng2057.
Jenkins ZA, van Kogelenberg M, Morgan T, Jeffs A, Fukuzawa R, Pearl E, Thaller C, Hing AV, Porteous ME, Garcia-Minaur S: Germline mutations in WTX cause a sclerosing skeletal dysplasia but do not predispose to tumorigenesis. Nat Genet. 2009, 41: 95-100. 10.1038/ng.270.
Waguespack SG, Hui SL, White KE, Buckwalter KA, Econs MJ: Measurement of tartrate-resistant acid phosphatase and the brain isoenzyme of creatine kinase accurately diagnoses type II autosomal dominant osteopetrosis but does not identify gene carriers. J Clin Endocrinol Metab. 2002, 87: 2212-2217. 10.1210/jc.87.5.2212.
Alatalo SL, Ivaska KK, Waguespack SG, Econs MJ, Vaananen HK, Halleen JM: Osteoclast-derived serum tartrate-resistant acid phosphatase 5b in Albers-Schonberg disease (type II autosomal dominant osteopetrosis). Clin Chem. 2004, 50: 883-890. 10.1373/clinchem.2003.029355.
Del Fattore A, Peruzzi B, Rucci N, Recchia I, Cappariello A, Longo M, Fortunati D, Ballanti P, Iacobini M, Luciani M: Clinical, genetic, and cellular analysis of 49 osteopetrotic patients: implications for diagnosis and treatment. J Med Genet. 2006, 43: 315-325. 10.1136/jmg.2005.036673.
Ogur G, Ogur E, Celasun B, Baser I, Imirzalioglu N, Ozturk T, Alemdaroglu A: Prenatal diagnosis of autosomal recessive osteopetrosis, infantile type, by X-ray evaluation. Prenat Diagn. 1995, 15: 477-481. 10.1002/pd.1970150512.
Landa J, Margolis N, Di Cesare P: Orthopaedic management of the patient with osteopetrosis. J Am Acad Orthop Surg. 2007, 15: 654-662.
Hwang JM, Kim IO, Wang KC: Complete visual recovery in osteopetrosis by early optic nerve decompression. Pediatr Neurosurg. 2000, 33: 328-332. 10.1159/000055980.
Driessen GJ, Gerritsen EJ, Fischer A, Fasth A, Hop WC, Veys P, Porta F, Cant A, Steward CG, Vossen JM: Long-term outcome of haematopoietic stem cell transplantation in autosomal recessive osteopetrosis: an EBMT report. Bone Marrow Transplant. 2003, 32: 657-663. 10.1038/sj.bmt.1704194.
Steward CG, Pellier I, Mahajan A, Ashworth MT, Stuart AG, Fasth A, Lang D, Fischer A, Friedrich W, Schulz AS: Severe pulmonary hypertension: a frequent complication of stem cell transplantation for malignant infantile osteopetrosis. Br J Haematol. 2004, 124: 63-71. 10.1046/j.1365-2141.2003.04739.x.
Frattini A, Blair HC, Sacco MG, Cerisoli F, Faggioli F, Cato EM, Pangrazio A, Musio A, Rucci F, Sobacchi C: Rescue of ATPa3-deficient murine malignant osteopetrosis by hematopoietic stem cell transplantation in utero. Proc Natl Acad Sci USA. 2005, 102: 14629-14634. 10.1073/pnas.0507637102.
Key LL, Ries WL, Rodriguiz RM, Hatcher HC: Recombinant human interferon gamma therapy for osteopetrosis. J Pediatr. 1992, 121: 119-124. 10.1016/S0022-3476(05)82557-0.
Key LL, Rodriguiz RM, Willi SM, Wright NM, Hatcher HC, Eyre DR, Cure JK, Griffin PP, Ries WL: Long-term treatment of osteopetrosis with recombinant human interferon gamma. N Engl J Med. 1995, 332: 1594-1599. 10.1056/NEJM199506153322402.
Kocher MS, Kasser JR: Osteopetrosis. Am J Orthop. 2003, 32: 222-228.
Key L, Carnes D, Cole S, Holtrop M, Bar-Shavit Z, Shapiro F, Arceci R, Steinberg J, Gundberg C, Kahn A: Treatment of congenital osteopetrosis with high-dose calcitriol. N Engl J Med. 1984, 310: 409-415.
Villa A, Guerrini MM, Cassani B, Pangrazio A, Sobacchi C: Infantile Malignant, Autosomal Recessive Osteopetrosis: The Rich and The Poor. Calcif Tissue Int. 2008
Del Fattore ACA, Teti A: Genetics, pathogenesis and complications of osteopetrosis. Bone. 2008, 42: 19-29. 10.1016/j.bone.2007.08.029.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
Both authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Stark, Z., Savarirayan, R. Osteopetrosis. Orphanet J Rare Dis 4, 5 (2009). https://doi.org/10.1186/1750-1172-4-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1750-1172-4-5