Abstract
Background
Portal vein gas is an ominous radiological sign, which indicates a serious gastrointestinal problem in the majority of patients. Many causes have been identified and the most important was bowel ischemia and mesenteric vascular accident. The presentation of patients is varied and the diagnosis of the underlying problem depends mainly on the radiological findings and clinical signs. The aim of this article is to show the clinical importance of portal vein gas and its management in emergency surgery.
Methods
A computerised search was made of the Medline for publications discussing portal vein gas through March 2008. Sixty articles were identified and selected for this review because of their relevance. These articles cover a period from 1975–2008.
Results
Two hundreds and seventy-five patients with gas in the portal venous system were reported. The commonest cause for portal vein gas was bowel ischemia and mesenteric vascular pathology (61.44%). This was followed by inflammation of the gastrointestinal tract (16.26%), obstruction and dilatation (9.03%), sepsis (6.6%), iatrogenic injury and trauma (3.01%) and cancer (1.8%). Idiopathic portal vein gas was also reported (1.8%).
Conclusion
Portal vein gas is a diagnostic sign, which indicates a serious intra-abdominal pathology requiring emergency surgery in the majority of patients. Portal vein gas due to simple and benign cause can be treated conservatively. Correlation between clinical and diagnostic findings is important to set the management plan.
Similar content being viewed by others
Background
Portal vein gas (PVG) represents a challenge for diagnosis and management of the underlying surgical cause in emergency surgery. PVG is not a disease; it is a diagnostic clue in patients who may be harbouring an intra-abdominal catastrophe [1]. Mortality could reach 75% [2], however, an increasing number of cases associated with benign conditions suitable for conservative treatment are being reported [3, 4]. The majority of patients present acutely to the Accident and Emergency department. Following assessment, surgeons will be alarmed immediately by the patients' critical and unstable condition. A significant number of patients with PVG are misdiagnosed and admitted to the medical ward because they are elderly and unwell and are subsequently not subjected to the specific diagnostic tools. The most common underlying pathology includes bowel ischemia, alteration of the gastrointestinal lining, inflammation and sepsis. However, PVG has recently been recognized as a rare complication of endoscopic and radiological procedures [5].
Methods
A computerised search was made of the Medline for publications discussing portal vein gas through March 2008. The search words were 'hepatic portal vein gas',' portal vein gas'. Other articles were identified by cross referencing. Sixty articles were identified and selected for this review because of their relevance. These articles cover a period from 1975–2008. The main topics were the aetiology of PVG, its presentation, investigations and the management. The conclusions of the major studies included in this review are presented and constitute the current concept of the significance of PVG in emergency surgery.
Results
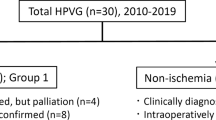
Two hundreds and seventy-five patients with gas in the portal venous system were reported. The commonest cause for portal vein gas was bowel ischemia and mesenteric vascular pathology (61.44%). This was followed by inflammation of the gastrointestinal tract (16.26%), obstruction and dilatation (9.03%), sepsis (6.6%), iatrogenic injury and trauma (3.01%) and cancer (1.8%). Idiopathic portal vein gas was also reported in1.8 %. Men and women affected equally. Majority of the patients are elderly and affected by most serious cause, the mesenteric vascular pathology. Diagnostic approach is based on the clinical suspicion and investigations such as CT scan which represents the standard test. The management depends on the underlying cause. Better outcome is reported because of advances in diagnostic facilities, the intensive care setting and less invasive operative technique such as laparoscopy.
Aetiology
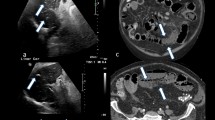
The most important cause for PVG is bowel ischemia, inflammation of the gastrointestinal tract GIT (see figure 1), obstruction and dilatation, gastro-intestinal leak, infection, diffuse peritonitis and sepsis [6–17] (see figure 2). It may follow GIT cancer, gastric ulcer, hypertrophic pyloric stenosis, cystic fibrosis and acute appendicitis [18–21]. PVG is also reported following perforated and non perforated diverticulitis, oesophageal and colonic carcinoma [22–26]. Inflammation of the GIT such as necrotizing enterocolitis, Crohn's disease and ulcerative colitis [27–30] are also reported in literatures. It is also reported following surgical procedures such as pancreaticoduodenectomy [31]. Vascular causes include septic thrombophlebitis of the superior mesenteric vein, superior mesenteric artery syndrome, and hemodialysis [32–35].
Respiratory tract infection, abdominal trauma, diagnostic and therapeutic gastrointestinal procedures, resuscitation procedures, drugs and caustics ingestion are rare causes for PVG, while it is idiopathic in certain cases [36–44] (see additional file 1).
Presentation
Portal vein gas is a radiological sign of underlying pathology mostly related to the gastrointestinal tract [5]. The presentation is that of primary disease and in the majority of patients is characterised by acute onset of abdominal pain and carries relatively high morbidity and mortality despite modern surgical and medical management. Other patients are asymptomatic and PVG is discovered during investigation for another problem. No special predilection for male or female and PVG usually affect elderly patients, although cases affecting the younger population including infants have been reported as well [18].
Diagnosis
Clinical findings
An accurate history and thorough examination are crucial for the management plan. Correlation between the clinical signs and the radiological findings will be the most important factor in the decision to proceed to laparotomy or not. Acute abdominal signs and positive radiology will mandate emergency operation in the majority of cases. On the other hand positive radiology with no acute abdominal signs may indicate a conservative treatment especially in elderly frail patients.
Computed axial tomography CT
Is superior to other radiological modalities and it is the gold standard for diagnosis of PVG and its aetiology [45, 46] (see figure 2). At CT, portal vein gas appears as tubular areas of decreased attenuation in the liver, predominantly in the left lobe [47]. The extent of PVG depends on the cause and severity of the underlying pathology and therefore the demonstration of a small amount of gas in the portal vein may indicate a less severe condition and suggest a less invasive approach. [48]. In these cases CT scan can provide crucial information for diagnosis and whether emergency surgery is needed or not. The most important information provided by CT scan is to rule out bowel ischemia, thus a negative CT scan could help to decide the next step of management which could be a conservative one. Although modern imaging contributes to the safe and effective management plan, CT scan however, may be of limited value in certain cases where the prediction of the extent of the gastrointestinal ischemia can not be accurately assessed. Therefore partial thickness infarction and necrosis which can produce PVG and pneumatosis intestinalis may be undetectable by CT study [49].
Ultrasound examination US
Can be used to assess the PVG and predict the outcome[50]. The ultrasound features include dot-like, streak-like and fruit-pulp-like patterns [51]. The real time phase of US is advantageous to detect the PVG and may be of comparable accuracy to the CT scan, however CT scan is more valuable in detecting the aetiology of PVG or excluding abdominal catastrophes [52]. When US is positive, urgent clinical evaluation followed by contrast-enhanced CT is indicated to assess for associated intestinal ischemia[53].
Colour Doppler flow imaging (CDFI)
The efficacy of this modality is less than CT scan in detection of PVG [54].
Magnetic resonance imaging MRI
This modality will delineate the portal system and is helpful in the assessment of patency of the portal vein and associated tributaries and whether there is occlusive or non occlusive ischemia.
Plain abdominal radiology
The plain film is of no specific diagnostic criteria; nevertheless, it can show indirect signs such as oedematous bowel wall, ileus, gasless abdomen, or gas in the bowel wall and portal vein in more severe cases of bowel ischemia. Plain abdominal x-ray can detect PVG in about 12.5% of cases [55].
Blood test
An increase in the white cell count in more than 50% of cases and lactic acidosis in more than 90% of patients with established bowel ischemia is usually confirmed. Polycythemia and thrombocythemia may indicate a clue to the likely cause. These non specific parameters will help in the overall assessment of patients.
Management
Is largely applied to the underlying cause (see Additional file 1). However, there are cases where a surgeon will proceed to abdominal exploration in the presence of borderline abdominal signs. Gas in portal vein is a good predictive factor for diagnosis, management, and prognosis [56]. In the past the traditional teaching is to operate once you have radiological evidence of PVG. However with the advances in diagnostic radiology, endoscopy, baseline support and intensive care setting, a less invasive approach is suggested especially for benign cases which indicate no intrabdominal catastrophe and thus reducing the rate of negative laparotomy [57]. Endoscopy can be very helpful in assessment or exclusion of upper and lower gastrointestinal pathology in the presence of PVG when CT scan gave no clue to the diagnosis, therefore a more sensible decision can be made. Patients diagnosed by CT scan with obstruction, infarction or vascular problems need no further endoscopic confirmation and are candidates for emergency exploration.
Therefore, patients who present with PVG can be divided into three categories: Firstly: those who have acute abdominal features and positive diagnostic criteria will need immediate exploration by laparoscopy or laparotomy.
Secondly: Patients who have positive diagnosis of PVG but without abdominal signs, are relatively stable and have no mesenteric ischemia will be good candidates for a conservative approach [58].
Thirdly: Patients who have borderline features of acute abdomen and less dense diagnostic signs of PVG may need endoscopic examination of the upper and lower GIT as a safe approach rather than to wait for underlying bowel ischemia [59]. This can be achieved using diagnostic laparoscopy which can help identify GIT pathology. In non GIT cause such as vascular disease or when the problem cannot be managed laparoscopically, laparotomy is indicated.
The history, severity of clinical signs and the density of PVG depicted by diagnostic tests will direct the management to either emergency intervention or conservative plan. With prompt surgical response a high mortality figure of 86% in bowel ischemia can be reduced to an acceptable figure [60]. Although the amount of gas is correlated with the severity of the pathology, the prognosis however, was related to the pathology itself and was not influenced by the presence of the gas in the portal system [6].
Conclusion
Portal vein gas is a diagnostic sign which indicates a serious intra-abdominal pathology requiring emergency surgery in the majority of patients. Benign hepatic portal vein gas due to less dangerous disease can be treated conservatively after exclusion of intra-abdominal catastrophe. Correlation between clinical and diagnostic findings is important to set the management plan.
Abbreviations
- PVG:
-
Portal vein gas
- GIT:
-
Gastrointestinal tract
- CT:
-
Computarised axial tomography
- US:
-
Ultrasound.
References
Mohammed AH, Khot UP, Thomas D: Portal venous gas – case report and review of the literature. Anaesthesia. 2007, 62: 400-4. 10.1111/j.1365-2044.2007.05022.x.
Little AF, Ellis SJ: 'Benign' hepatic portal venous gas. Australas Radiol. 2003, 47: 309-12. 10.1046/j.1440-1673.2003.01184.x.
Magrach LA, Martín E, Sancha A, García M, Cendoya I, Olabarria I, Gómez-Portilla A, Tejada I, Carrero C, López de Torre J, García-Urra JA, Echavarri J: [Hepatic portal venous gas. Clinical significance and review of the literature]. Cir Esp. 2006, 2: 78-82.
Alqahtani S, Coffin CS, Burak K, Chen F, MacGregor J, Beck P: Hepatic portal venous gas: a report of two cases and a review of the epidemiology, pathogenesis, diagnosis and approach to management. Can J Gastroenterol. 2007, 5: 309-13.
Monneuse O, Pilleul F, Barth X, Gruner L, Allaouchiche B, Valette PJ, Tissot E: Portal venous gas detected on computed tomography in emergency situations: surgery is still necessary. World J Surg. 2007, 31 (5): 1065-71. 10.1007/s00268-006-0589-0.
Keskek M, Hamaloglu E, Ozdemir A, Ozenç A: Portomesenteric gas due to intestinal obstruction: a case report. Acta Chir Belg. 2002, 3: 201-2.
Gilbeau JP, De Merlier Y, Lacrosse M: [Mesenteric and portal venous gas in infarction of the small intestine in adults. Apropos of 3 clinical cases. Value of x-ray computed tomography]. J Radiol. 1997, 6: 439-42.
Sarti J, Kennedy A: Portal venous gas in hypertrophic pyloric stenosis. J Pediatr Surg. 2006, 11: 1935-6. 10.1016/j.jpedsurg.2006.07.011.
Tuite DJ, Byrne A, Colhoun E, Torreggiani WC: Pneumatosis intestinalis and portal-venous gas: an unusual presentation of acute appendicitis. Australas Radiol. 2007, 51: 137-9.
Duggal A, Rankin RN, Wall WJ: Hepatic portal venous gas from perforated sigmoid diverticulitis. Can J Surg. 2007, 6: 19-20.
Sellner F, Sobhian B, Baur M, Sellner S, Horvath B, Mostegel M, Karner J, Staettner S: Intermittent hepatic portal vein gas complicating diverticulitis – a case report and literature review. Int J Colorectal Dis. 2007, 11: 1395-9. 10.1007/s00384-007-0346-3.
Alonso-Burgos A, Nogueral JJ, Cosín O, Viudez A, Pueyo J, Elorz M, Aquerreta JD: [Intestinal pneumatosis and portomesenteric gas: a case review]. Rev Med Univ Navarra. 2007, 2: 3-6.
Ishida A, Masuda M: [A case of hepatic portal venous gas caused by splenic flexure carcinoma diagnosed by CT]. Rinsho Hoshasen. 1987, 10: 1165-7.
Silva CT, Daneman A, Navarro OM, Moore AM, Moineddin R, Gerstle JT, Mittal A, Brindle M, Epelman M: Correlation of sonographic findings and outcome in necrotizing enterocolitis. Pediatr Radiol. 2007, 3: 274-82. 10.1007/s00247-006-0393-x.
Ng SS, Yiu RY, Lee JF, Li JC, Leung KL: Portal venous gas and thrombosis in a Chinese patient with fulminant Crohn's colitis: a case report with literature review. World J Gastroenterol. 2006, 34: 5582-6.
Liebman PR, Patten MT, Manny J, Benfield JR, Hechtman HB: Hepatic – portal venous gas in adults: etiology, pathophysiology and clinical significance. Ann Surg. 1978, 3: 281-7. 10.1097/00000658-197803000-00012.
Chau TN, Loke TK, Leung VK, Law ST, Lai MH, Ho YW: Hepatic portal venous gas complicating septic thrombophlebitis of the superior mesenteric vein. Hong Kong Med J. 2007, 1: 69-72.
Tsai CL, Chen MJ, Tan CK, Chan KS, Cheng KC: Superior mesenteric artery syndrome with hepatic portal venous gas. Med J Aust. 2007, 1:: 48.
Sato M, Kikuchi H, Takada K, Iida H, Gohongi T, Orii K: Transient portomesenteric venous gas in long-term hemodialysis patients. Radiat Med. 2005, 8: 570-3.
Ergaz Z, Arad I, Simanovsky N: Portal venous gas following trauma in a preterm infant. Fetal Pediatr Pathol. 2006, 3: 147-50. 10.1080/15513810600908271.
Barthet M, Membrini P, Bernard JP, Sahel J: Hepatic portal venous gas after endoscopic biliary sphincterotomy. Gastrointest Endosc. 1994: 261-3. 2 Pt 1
Quirke TE: Hepatic-portal venous gas associated with ileus. Am Surg. 1995, 12: 1084-6.
Sebastià C, Quiroga S, Espin E, Boyé R, Alvarez-Castells A, Armengol M: Portomesenteric vein gas: pathologic mechanisms, CT findings, and prognosis. Radiographics. 2000, 5: 1213-24.
Chan SC, Wan YL, Cheung YC, Ng SH, Wong AM, Ng KK: Computed tomography findings in fatal cases of enormous hepatic portal venous gas. World J Gastroenterol. 2005, 19: 2953-5.
Sebastià C, Quiroga S, Espin E, Boyé R, Alvarez-Castells A, Armengol M: Portomesenteric vein gas: pathologic mechanisms, CT findings, and prognosis. Radiographics. 2000, 20: 1213-24.
Torzilli G, Cattaneo S, Lumachi V, Leoni P, Stefanini P, Gnocchi P, Olivari N: Ultrasonographic detection of portal branches and hepatic vein gas associated with mesenteric artery occlusion: a new finding correlated with patient prognosis?. Chir Ital. 2000, 3: 295-8.
Wiesner W, Mortelé KJ, Glickman JN, Ji H, Ros PR: Pneumatosis intestinalis and portomesenteric venous gas in intestinal ischemia: correlation of CT findings with severity of ischemia and clinical outcome. AJR Am J Roentgenol. 2001, 177: 1319-23.
Chevallier P, Peten E, Souci J, Chau Y, Padovani B, Bruneton JN: Detection of portal venous gas on sonography, but not on CT. Eur Radiol. 2002, 5: 1175-8. 10.1007/s00330-001-1144-x.
Pan HB, Huang JS, Yang TL, Liang HL: Hepatic portal venous gas in ultrasonogram – benign or noxious. Ultrasound Med Biol. 2007, 8: 1179-83. 10.1016/j.ultrasmedbio.2007.01.014.
Oktar SO, Karaosmanoğlu D, Yücel C, Erbaş G, Ilkme A, Canpolat I, Ozdemir H: Portomesenteric venous gas: imaging findings with an emphasis on sonography. J Ultrasound Med. 2006, 8: 1051-8.
Maher MM, Tonra BM, Malone DE, Gibney RG: Portal venous gas: detection by gray-scale and Doppler sonography in the absence of correlative findings on computed tomography. Abdom Imaging. 2001, 4: 390-4. 10.1007/s002610000192.
ulze CG, Blum U, Haag K: Hepatic portal venous gas. Imaging modalities and clinical significance. Acta Radiol. 1995, 4: 377-80.
Schindera ST, Triller J, Vock P, Hoppe H: Detection of hepatic portal venous gas: its clinical impact and outcome. Emerg Radiol. 2006, 4: 164-70. 10.1007/s10140-006-0467-y.
Yüksel O, Sare M, Salman B, Irkörücü O, Tezcaner T, Taşçilar O, Akyürek N, Tatlicioğlu E: [Hepatic portal venous gas: a case report]. Ulus Travma Acil Cerrahi Derg. 2006, 2: 167-9.
Hong JJ, Gadaleta D, Rossi P, Esquivel J, Davis JM: Portal vein gas, a changing clinical entity. Report of 7 patients and review of the literature. Arch Surg. 1997, 10: 1071-5.
Wiesner W, Mortelé KJ, Glickman JN, Ji H, Ros PR: Portal-venous gas unrelated to mesenteric ischemia. Eur Radiol. 2002, 6: 1432-7. 10.1007/s00330-001-1159-3.
Niki M, Shimizu I, Horie T, Okazaki M, Shiraishi T, Takeuchi H, Fujiwara S, Murata M, Yamamoto K, Iuchi A, Atagi Y, Ito S: Hepatic portal venous gas disappearing within 24 hours. Intern Med. 2002, 11: 950-2. 10.2169/internalmedicine.41.950.
Paran H, Epstein T, Gutman M, Shapiro Feinberg M, Zissin R: Mesenteric and portal vein gas: computerized tomography findings and clinical significance. Dig Surg. 2003, 2: 127-32. 10.1159/000069388.
Kung D, Ruan DT, Chan RK, Ericsson ML, Saund MS: Pneumatosis intestinalis and portal venous gas without bowel ischemia in a patient treated with irinotecan and cisplatin. Dig Dis Sci. 2008, 1: 217-9. 10.1007/s10620-007-9846-9.
Negro U, Verdecchia M, Paci E, Antico E, Valeri G, Risaliti A, Vecchi A, Svegliati-Baroni G, Giovagnoni A: Hepatic portal venous gas in a patient with enterovascular fistula. Abdom Imaging. 2006, 6: 706-9. 10.1007/s00261-005-8011-1.
Lai CF, Chang WT, Liang PC, Lien WC, Wang HP, Chen WJ: Pneumatosis intestinalis and hepatic portal venous gas after CPR. Am J Emerg Med. 2005, 2: 177-81. 10.1016/j.ajem.2004.05.010.
Bobba RK, Arsura EL: Hepatic portal and mesenteric vein gas as a late complication of percutaneous endoscopic gastrostomy tube placement in an elderly patient. Dig Dis Sci. 2005, 2: 411-4. 10.1007/s10620-005-1620-2.
Mognol P, Chosidow D, Marmuse JP: Hepatic portal gas due to gastro-jejunal anastomotic leak after laparoscopic gastric bypass. Obes Surg. 2005, 2: 278-81. 10.1381/0960892053268480.
Parada González P, Fernández Rodríguez E, Nuño Váquez-Garza JM, González Fernández S, Casal Núñez JE: [Portal venous gas secondary to acute gastric dilatation]. Rev Esp Enferm Dig. 2004, 3: 227-8.
Saksena M, Harisinghani MG, Wittenberg J, Mueller PR: Case report. Hepatic portal venous gas: transient radiographic finding associated with colchicine toxicity. Br J Radiol. 2003, 911: 835-7. 10.1259/bjr/13712140.
Lewin M, Pocard M, Caplin S, Blain A, Tubiana JM, Parc R: Benign hepatic portal venous gas following caustic ingestion. Eur Radiol. 2002, 3: S59-61.
Ho MC, Hu RH: Hepatic portal vein gas following blunt colon injury: report of a case. J Formos Med Assoc. 1995, 9: 578-80.
Tsubono T, Sato K, Fukuda M: Hepatic portal venous gas associated with cholangitis following pancreaticoduodenectomy: report of a case. Surg Today. 1994, 4: 375-7. 10.1007/BF02348572.
Bach MC, Anderson LG, Martin TA, McAfee RE: Gas in the hepatic portal venous system. A diagnostic clue to an occult intra-abdominal abscess. Arch Intern Med. 1982, 9: 1725-6. 10.1001/archinte.142.9.1725.
Rovito V: Hepatic-portal vein gas associated with bronchopneumonia. Am J Gastroenterol. 1982, 4: 243-4.
Kees CJ, Hester CL: Portal vein gas following barium enema examination. Radiology. 1972, 3: 525-6.
Lien WC, Chang WT, Huang SP, Chiu HM, Lai TI, Weng TI, Fang CC, Wang HP, Chen WJ: Hepatic portal venous gas associated with poor outcome in out-of-hospital cardiac arrest patients. Resuscitation. 2004, 3: 303-7. 10.1016/j.resuscitation.2003.12.002.
Nguyen HN, Purucker E, Riehl J, Matern S: Hepatic portal venous gas following emergency endoscopic sclerotherapy of gastric varices. Hepatogastroenterology. 1998, 23: 1767-9.
Ghai S, O'Malley ME: Portal vein gas resulting from ingestion of hydrogen peroxide. AJR Am J Roentgenol. 2003, 6: 1719-20.
Morrison SC, Czinn SJ: Portal vein gas associated with rotavirus infection. J Pediatr Gastroenterol Nutr. 2001, 5: 626-8. 10.1097/00005176-200111000-00024.
Schilling EM, Stückle CA, Kirchner J, Donnerstag F, Liermann D: [Computerized tomography detection of portal vein air accumulation in severe gastroenteritis during chemotherapy]. Wien Klin Wochenschr. 2000, 2: 80-3.
Ozgur HT, Unger EC, Wright WH: Portal venous gas in a cardiac transplant patient. AJR Am J Roentgenol. 1996, 4: 992-3.
Mallens WM, Schepers-Bok R, Nicolai JJ, Jacobs FA, Heyerman HG: Portal and systemic venous gas in a patient with cystic fibrosis: CT findings. AJR Am J Roentgenol. 1995, 165: 338-9.
Kurata S, Kawano H, Yamasaki T, Mizumachi S, Furoi A, Tokunaga M, Ebe K, Nagaoka S, Tanimura A, Akiyama T, et al: [A case of acute emphysematous cholecystitis with portal venous gas]. Nippon Shokakibyo Gakkai Zasshi. 1993, 90: 1526-9.
Takahashi H, Okamura Y, Hashimoto S, Kawamura A, Yamamoto Y, Yamamoto Y: [A case of portal venous gas complicated with gastric ulcer with acute gastric dilatation]. Nippon Shokakibyo Gakkai Zasshi. 1991, 88: 82-6.
Acknowledgements
We thank Jackie Nicholls for checking the language of this article.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
AH carried out the Medline search and participated in the sequence alignment and drafted the manuscript. HM carried out the statistical data and formatted the figures and tables. SEL conceived the study, and participated in its design and coordination and helped to draft the manuscript. All authors read and approved the final manuscript.
Electronic supplementary material
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Hussain, A., Mahmood, H. & El-Hasani, S. Portal vein gas in emergency surgery. World J Emerg Surg 3, 21 (2008). https://doi.org/10.1186/1749-7922-3-21
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1749-7922-3-21