Abstract
Background
Mycobacterium spp. is one of the most important species of zoonotic pathogens that can be transmitted from cattle to humans. The presence of these opportunistic, pathogenic bacteria in bovine milk has emerged as a public-health concern, especially among individuals who consume raw milk and related dairy products. To address this concern, the Brazilian control and eradication program focusing on bovine tuberculosis, was established in 2001. However, bovine tuberculosis continues to afflict approximately 1,3 percent of the cattle in Brazil. In the present study, 300 samples of milk from bovine herds, obtained from both individual and collective bulk tanks and informal points of sale, were cultured on Löwenstein-Jensen and Stonebrink media. Polymerase chain reaction (PCR)-based tests and restriction-enzyme pattern analysis were then performed on the colonies exhibiting phenotypes suggestive of Mycobacterium spp., which were characterized as acid-fast bacilli.
Results
Of the 300 bovine milk samples that were processed, 24 were positively identified as Mycobacterium spp.
Molecular identification detected 15 unique mycobacterial species: Mycobacterium bovis, M. gordonae, M. fortuitum, M. intracellulare, M. flavescens, M. duvalii, M. haemophilum, M. immunogenum, M. lentiflavum, M. mucogenicum, M. novocastrense, M. parafortuitum, M. smegmatis, M. terrae and M. vaccae. The isolation of bacteria from the various locations occurred in the following proportions: 9 percent of the individual bulk-tank samples, 7 percent of the collective bulk-tank samples and 8 percent of the informal-trade samples. No statistically significant difference was observed between the presence of Mycobacterium spp. in the three types of samples collected, the milk production profiles, the presence of veterinary assistance and the reported concerns about bovine tuberculosis prevention in the herds.
Conclusion
The microbiological cultures associated with PCR-based identification tests are possible tools for the investigation of the presence of Mycobacterium spp. in milk samples. Using these methods, we found that the Brazilian population may be regularly exposed to mycobacteria by consuming raw bovine milk and related dairy products. These evidences reinforces the need to optimize quality programs of dairy products, to intensify the sanitary inspection of these products and the necessity of further studies on the presence of Mycobacterium spp. in milk and milk-based products.
Similar content being viewed by others
Background
Milk is an important source of proteins, sugars, lipids and other nutrients for humans. However, these nutrients can also serve as substrates for pathogenic microorganisms. The traditional consumption of homemade dairy products, and especially cheeses, that are composed of non-heat-treated milk poses a serious risk to public health [1]. It is estimated that more than 90 percent of all of the cases of illness related to the consumption of dairy products are of bacterial etiology, and at least 21 different diseases of this type have been identified [2].
Over the last three decades, approximately 75 percent of emerging infectious diseases in humans have been zoonoses. The increasing interdependence of humans on animals and animal products has been determined to be the most critical risk factor for such infectious diseases [3]. Mycobacterial infections are among the most debilitating conditions affecting humans and animals because these infections are both chronic and progressive [4]. Among such infections, tuberculosis is one of the main zoonotic diseases transmitted by bovine milk [5]. Microorganisms of the Mycobacterium genus, such as Mycobacterium bovis, are highly able to survive in bovine milk and other dairy products. These microbes can be found in the form of viable bacilli in cream cheese and yogurt produced from raw milk for over 14 days and in butter for over 100 days [6]. Recently, the presence of these opportunistic, pathogenic bacteria in milk has emerged as a public-health concern, especially among individuals who consume raw milk and related dairy products [2].
Considering these health concerns and international trade requirements, many countries have implemented national programs for the control and eradication of bovine tuberculosis [7]. In Brazil, the National Program for Control and Eradication of Brucellosis and Tuberculosis (‘Programa Nacional de Controle e Erradicação da Brucelose e Tuberculose’ - PNCEBT) was established in 2001, with the aim of reducing the incidence of tuberculosis in bovine and bubaline herds [8]. Brazilian legislative measures now require the regulation of the storage, collection and transport of refrigerated raw milk [9]. The country has also established a National Program of Milk Quality to increase the quality of milk production. Despite this program, however, small farmers are still selling unpasteurized milk that has not undergone sanitary inspection to individuals who prefer this type of dairy product. National surveys have confirmed the habit of consumption of milk without any heat treatment [10], and there are no validated laboratory methods that allow the certification of such untreated milk or dairy products as “free of viable mycobacteria” [6].
The aim of the current study was to investigate the occurrence of mycobacteria in bovine raw-milk samples, obtained from both individual and collective bulk tanks and informal trade in the southeast region of Sao Paulo, Brazil, using microbiological cultures and polymerase chain reaction (PCR)-based testing. The specific objectives of this study included the comparison of the presence of mycobacteria in various sample types, the use of bovine milk samples from herds to evaluate the risk of human contact with these bacteria and the use of PCR and restriction-enzyme pattern analysis (PRA) to identify the Mycobacterium spp.
Methods
Ethical statement
The study was approved by the Ethics Committee on the Use of Animals of the School of Veterinary Medicine and Animal Science of Sao Paulo State University (FMVZ-UNESP/Botucatu), under the protocol number 156/2010-CEUA.
Enrolled farms
This study included small- and medium-sized farms in the southeast region of Sao Paulo state, a major milk-producing area of Brazil, inserted into the largest national consumer market. The farms, which were randomly chosen, used either automatic or manual milking systems and possessed between two and 200 lactating animals. The herds were composed of the Holstein, Jersey or Girolando breeds or of crossbreeds with the ability to produce milk and exhibited a median milk production of 12 liters per day.
Epidemiological data on the herds were obtained using a questionnaire administered to farmers and milk-sellers that requested information on the following: the city where the farm was located, the type of milking system, the daily total volume milked (in liters), the mean volume milked (in liters), the number of lactating animals, the breeds of the lactating animals, the presence or absence of veterinary assistance and whether there were concerns about tuberculosis prevention in the herd. In the case of collective bulk tanks, which are used by more than one farmer to deliver milk, the number of delivering producers per bulk tank was also ascertained.
Sample collection
One hundred samples were collected directly from the individual bulk tanks, and 100 were collected from the collective bulk tanks. One hundred samples were also collected at informal points of sale in the same region. In this case, milk was bought directly from informal sellers. This sample collection included 25 different cities in the southeast region of Sao Paulo, Brazil.
A total volume of 100 milliliters was collected per sample, and each of the 300 samples was placed in a sterilized collection flask at the time of collection. The samples were immediately stored on ice in isothermal boxes (4 to 8 degrees Celsius) until their arrival at the laboratory.
Mycobacterial cultures
To avoid contamination or biological risk, the samples were processed in a class II biological safety cabinet that had been cleaned with 10 percent sodium hypochlorite and 70 percent alcohol, followed by exposure to ultraviolet light for 30 minutes, with the air circulation system turned on. An 8-milliliter aliquot of each sample was then transferred into a screw-top centrifuge tube for high-speed centrifugation (10.000 rotations per minute for 20 minutes). During this process, the cells and fat from the samples were concentrated, and the remaining serum was removed. The Petroff decontamination method, using 4% sodium hydroxide and 4% sulfuric acid [11], was performed on the mixture of fat and protein sediment derived from each sample to be used for mycobacterial culture.
The cultures were maintained on Löwenstein-Jensen and Stonebrink media, incubated aerobically at 37 degrees Celsius for 90 days and examined weekly. Any colonies exhibiting phenotypes suggestive of mycobacteria were stained using the Ziehl-Neelsen method and maintained on the same media at room temperature and hidden from light until PRA was performed.
PCR-based species identification
For the PCR-based species identification using PRA, DNA extraction was performed by thermolysis. A loopful (10 microliters) of mycobacteria was suspended in 300 microliters of Tris-EDTA buffer (pH 8.0) in DNase/RNase-free microcentrifuge tubes, boiled for 10 minutes and frozen (−20 degrees Celsius) for 10 minutes. These boiling and freezing processes were repeated three times. To separate the DNA, the microtubes were centrifuged (12.000 rotations per minute for 5 minutes). Three microliters of the supernatant containing the DNA, 25 picomoles of each primer and 34 microliters of PCR Master Mix (2X)™ (Fermentas™, Thermo Fisher Scientific, Vilnius, Lithuania) were then combined for PCR. This reaction amplified a 439-bp fragment within the hsp65 gene using the primers Tb11 (5′–ACCAACGATGGTGTGTCCAT–3′) and Tb12 (5′–CTTGTCGAACCGCATACCCT–3′) [12].
The PCR protocol consisted of a denaturation step at 95 degrees Celsius for 10 minutes, followed by 45 cycles at 94 degrees Celsius for 1 minute, 60 degrees Celsius for 1 minute and 72 degrees Celsius for 1 minute and a final extension step at 72 degrees Celsius for 10 minutes (PTC-100 Thermal Cycler, MJ Research™, Basel, Switzerland). The electrophoresis of 3 microliters of the PCR product was then performed on an agarose gel (1 percent) using a 100-bp molecular-weight marker (Invitrogen™, Carlsbad, United States of America) to confirm the amplification of the 439-bp fragment. Ten to 15 microliters of the amplified product was digested with the BstEII and HaeIII restriction enzymes according to the manufacturer’s instructions (Fermentas™). The resulting restriction fragments were separated by electrophoresis on an agarose gel (4 percent) using 25- and 50-bp molecular-weight markers (Invitrogen™). The fragment sizes were estimated using Alpha Ease-Alpha Innotech software (version 6.0) [Alpha Innotech™, San Leandro, United States of America] and analyzed using internet Prasite [13].
The amplification of the hsp65 gene cannot differentiate between M. tuberculosis complex (MTBC) species due to these species’ close genetic relationship. Therefore, isolates belonging to the MTBC have been analyzed by amplifying a 1020-bp fragment of the gyrB gene using PRA [14]. In this case, 3 microliters of mycobacterial DNA was added to 44 microliters of PCR Master Mix (2X)™, and subjected to PCR using 10 picomoles of each of the primers MTUBf (5′–TCGGACGCGTATGCGATATC–3′) and MTUBr (5′–ACATACAGTTCGGACTTGCG–3′). The PCR protocol consisted of an initial denaturation step for 10 minutes at 95 degrees Celsius; 35 amplification cycles, each consisting of 1 minute at 94 degrees Celsius, 1 minute at 65 degrees Celsius and 1,5 minutes at 72 degrees Celsius; and a final extension step of 10 minutes at 72 degrees Celsius. Electrophoresis on an agarose gel (1 percent) confirmed the amplification of the fragment. The amplicon was further digested using the restriction enzymes RsaI, TaqI and SacII according to the manufacturer’s instructions (Fermentas™). The restriction digests were separated on an agarose gel (2 percent) using 50- and 100-bp DNA molecular-weight markers (Invitrogen™). The separated fragments of the gyrB gene were analyzed using Alpha Ease-Alpha Innotech software (version 6.0) [Alpha Innotech™] and compared with the patterns that were described by Chimara et al. [14].
Data analysis
For the data analysis, continuous variables were categorized based on their median values. The total volume milked per day was classified as high (>330 liters) or low (<330 liters), and the mean volume milked per day was classified as high (>12 liters) or low (<12 liters). The number of lactating animals in each herd was categorized as many (>11 cows) or few (<11 cows). Similarly, the number of farmers delivering milk to each collective bulk tank was separated into two categories: many (>14 farmers) or few (<14 farmers).
Summary statistics were calculated to describe the characteristics of the farms enrolled in the study. Chi-squared or Fisher’s exact tests were used to identify the farm-related factors that were associated with the isolation of Mycobacterium spp. A logistic regression was then used to estimate the adjusted associations in a multivariable model, and backward variable selection was used to select a possible final model. The data were analyzed using R software (version 2.15.1) [15].
Results and discussion
Information regarding the daily total volume milked (in liters), the mean volume milked (in liters), the number of lactating animals, the breeds of the lactating animals, the presence of veterinary assistance and whether concerns existed about the prevention of tuberculosis in the herd was obtained for 228 of the 300 samples that were collected. This information was not collected for all of the samples because the informal milk sellers were not always aware of each product’s origin. The number of farmers who delivered milk to each collective bulk tank was also considered. The sampled population was highly heterogeneous, the descriptive analyses of these data are summarized in Table 1.
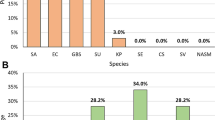
Of the 300 samples that were processed, 24 tested positive for Mycobacterium spp. Molecular methods identified 15 distinct species among the isolates, as shown in Table 2. One isolate belonged to the MTBC (M. bovis subsp. bovis), and the other isolates included the environmental nontuberculous mycobacteria (NTM) M. gordonae, M. fortuitum, M. intracellulare, M. flavescens, M. duvalii, M. haemophilum, M. immunogenum, M. lentiflavum, M. mucogenicum, M. novocastrense, M. parafortuitum, M. smegmatis, M. terrae and M. vaccae. The species that was most frequently isolated was M. gordonae type 9, and the second most frequent was M. haemophilum type 1.
Nine percent of the samples from the individual bulk tanks yielded Mycobacterium spp.-positive cultures, whereas 7 percent of the samples from the collective bulk tanks and 8 percent of the informal-trade samples resulted in positive cultures (Table 3). No statistically significant difference was observed between the number of samples that tested positive by mycobacterial culture and the epidemiological factors that were considered. These factors included the types of samples collected, the presence or absence of veterinary assistance on the farm, the concerns about tuberculosis prevention in the herd, the total volume milked per day, the mean volume milked per day, the number of lactating animals and the number of farmers delivering milk to each collective bulk tank, as shown in Table 3.
The screening tests of milk samples has been used to limit the spread of infectious diseases [16, 17], including certain diseases caused by mycobacteria, such as paratuberculosis [18]. As the use of bulk-tank milk samples for screening is less labor-intensive and more cost-effective than individual-tank sampling [19], this approach represents an important development in dairy research.
Previous studies have addressed the identification of mycobacteria in milk samples collected from both individual and collective bulk tanks. In one study, opportunistic mycobacteria were recovered from more than 55 percent of the samples collected from milking platforms [20]. In another study, in 1975, the presence of M. marinum, M. scrofulaceum, M. gordonae, M. flavescens and M. fortuitum was reported in 68.8 percent of 51 raw-milk samples [21]. Years later, researchers isolated mycobacteria from 4.3 percent of 209 milk samples collected from Indian farmers and traders [22]. In yet another study, saprophytic mycobacteria were identified in 13 percent of 285 milk samples [23]. Species from the MTBC have also been isolated from milk; in one case, 16 isolates of M. bovis and 8 isolates of M. tuberculosis were obtained from 543 milk samples collected from bulk tanks [24]. Additionally, a study conducted in Korea demonstrated that 4.5 percent of the collected milk samples tested positive for M. bovis. However, neither molecular characterization nor microbiological cultures of the samples were included by the researchers [19]. These data agree with the results obtained in the present study, in which both saprophytic and pathogenic mycobacteria were identified in bovine milk samples.
Species from the genus Mycobacterium are recognized as major pathogens transmitted between the environment, wildlife, livestock and humans. M. bovis represents a serious problem in the international trade of animals and animal products, resulting in great economic losses to livestock [25]. Zoonotic tuberculosis in man is attributed mainly to M. bovis and occasionally to M. tuberculosis, and this disease is mainly transmitted through milk. Therefore, certain habits, such as the consumption of raw bovine milk, may predispose individuals to these infections [26]. Although M. bovis does not multiply in milk or does so very slowly, the large number of mycobacteria that are secreted into the milk of one animal with tuberculous mastitis is generally sufficient render the homogenized milk from 100 lactating cows [6]. Given such risks and the fact that Brazil has the largest commercial cattle herd in the world, it is essential to ensure the high quality and low health risk of animal products destined for customers, who are increasingly exigent [8].
The ability of NTM to trigger disease is clearly documented in the literature, and concern about NTM is increasing, with isolates of different species now being researched in reference laboratories. Potentially pathogenic NTM that are present in the environment can be transmitted to humans or animals and can cause the onset of infection or disease [27]. Humans and animals are constantly exposed to NTM via inhalation or ingestion, resulting in the temporary or permanent colonization of the respiratory or digestive tract [28].
M. gordonae is extremely common in the environment and has been found predominantly in water. Although M. gordonae is considered to be a nonpathogenic bacterial species, infections have been reported in both immunocompromised and healthy patients [29]. Similarly, M. flavescens and M. lentiflavum have been frequently identified in clinical specimens, even without direct relation to disease. Nevertheless, studies refer M. flavescens in association with respiratory, skin and spread infections in humans, and M. lentiflavum causing fatal spread infections [30]. These data highlight the need for more research on these species [29, 31].
The habitat of M. mucogenicum remains unclear. Evidence suggests that this species exhibits a ubiquitous distribution and that water is the main route of transmission. M. mucogenicum has been isolated from municipal water distribution systems, in which this microorganism can form biofilms and also infect amoebae and protozoa [28, 32]. The high resistance of this species to chlorinated disinfectants and temperature extremes is notable, as these are major factors in the ecology of M. mucogenicum[32]. Although clinical isolates of this species are rare, these isolates have been associated with a wide spectrum of infections in both immunocompromised and healthy patients [30, 32].
Since the last decade, the isolation of M. vaccae from environmental sources (such as soil and ponds) as well as animals (such as udder and skin lesions in cattle) has been reported [30]. M. vaccae is considered to be a nonpathogenic type of NTM and was recently ranked as a bacterium that is beneficial to the central nervous system. More specifically, in 2010, the American Society for Microbiology reported growth stimulation in certain neuronal types and consequently increased serotonin levels and decreased anxiety in mice exposed to M. vaccae[33]. Similarly, M. parafortuitum is not considered to be a pathogenic species of NTM. Phenotypically, M. parafortuitum resembles M. fortuitum, but certain biochemical differences between the two species motivated the classification of M. fortuitum as a novel species in 1966 [34].
M. fortuitum has been recovered from tap water, water distribution systems and various types of soil. In humans, M. fortuitum is associated with skin lesions but rarely causes pulmonary lesions or spread infections [30]. This mycobacterial species is the most common type of mastitis-associated NTM and was reported to be the etiological agent in 17 cases of mastitis in cattle [35]. The bacterium has also been isolated from raw-milk samples collected from bulk tanks [36], and in Brazil, M. fortuitum has been isolated from milk samples from cows with a positive reaction to the tuberculin test [37]. The occurrence of chronic and fibrosing mastitis, which is associated with Mycobacterium spp., is typically due to the excessive intramammary use of oily or antimicrobial drugs for mastitis treatment or is secondary to severe cases of clinical mastitis, as these bacteria act as opportunistic pathogens [35, 38].
M. smegmatis also has been recovered from cattle with mastitis [39]. As the majority of the NTM, M. smegmatis is frequently found in water and soil [30]. Although this species may be associated with posttraumatic soft-tissue infections, M. smegmatis has not been described in disseminated infections, even in immunocompromised patients [30, 40].
M. immunogenum is a newly described species belonging to the M. chelonae-M. abscessus group. This species mainly causes hypersensitivity pneumonitis secondary to aerosol inhalation. M. immunogenum is also associated with disseminated skin infections, septic arthritis, keratitis and nosocomial infections [41, 42] and can form biofilms on environmental surfaces, such as pipes or equipment, resulting in a three- to 100-fold increase in disinfectant resistance [42].
M. haemophilum and M. duvalii are species associated with infection in immunocompromised patients or patients with human immunodeficiency virus (HIV) [30, 43]. In contrast, M. intracellulare is an etiological agent of disease in healthy patients [30] that has been found in various treated and untreated water sources, demonstrating the bacterium’s ability to survive in water for extended periods [44]. This species typically causes pulmonary disease, followed by lung damage or reduced lung function, or cervical lymphadenitis, and occasionally affects children [30]. In contrast, M. novocastrense, first described in 1997, is rarely reported in humans, although there is evidence of this bacterium’s involvement in certain diseases [45].
M. terrae is often recovered from samples of soil, water and vegetables. Initially, this species was considered to be nonpathogenic, but several reports have associated this mycobacteria with cases of tenosynovitis and joint and pulmonary infections. Although M. terrae is rarely associated with disseminated infection, this species exhibits relatively high resistance to antimicrobial therapy [30, 46].
The current study is the first report of the presence of M. duvalii, M. haemophilum, M. immunogenum, M. lentiflavum, M. mucogenicum and M. novocastrense in bovine raw-milk samples. The contamination of raw milk by mycobacteria is apparently inevitable, even under sanitary conditions, due to the ubiquitous nature of these microorganisms. Only the heat treatment of raw milk using commercial pasteurization protocols ensures the adequate destruction of mycobacterial contaminants. Thus, the transmission of viable mycobacteria to humans through heat-treated bovine milk is unlikely, whereas the consumption of raw bovine milk and related dairy products represents a public-health risk [38].
The increasing number of individuals worldwide who are infected with HIV in the world predisposes the increase in the number of cases of diseases that have been recognized as emerging and re-emerging, which are mainly those diseases caused by opportunistic agents, such as Mycobacterium spp. For example, in many regions of the world, tuberculosis is a major cause of death in HIV-infected individuals [47]. Such mycobacterial infections in HIV patients are frequently disseminated, although the transmission route of the bacteria remains controversial. As infection can occur in the lungs and/or gastrointestinal tract of HIV patients, a wide range of mycobacterial sources and modes of transmission must be investigated [48]. In particular, unpasteurized, mycobacteria-contaminated milk poses a serious risk to HIV patients.
The ecology and physiology of mycobacteria are complex and differ between MTBC and NTM. In recent years, the intersection of human, animal and mycobacterial ecology has exposed humans and animals to mycobacteria and has impacted mycobacterial ecology [48]. Research on the possible association between mycobacteria and the epidemiological factors preceding mycobacterial infection will be necessary to reduce the risk of exposure and infection.
Conclusions
Microbiological cultures and PCR-based identification tests are possible tools for the investigation of the presence of Mycobacterium spp. in milk samples. Our data indicate that the Brazilian population may be exposed to mycobacteria through the consumption of raw bovine milk and related dairy products. These evidences reinforces the need to optimize quality programs of dairy products, to intensify the sanitary inspection of these products and the necessity of further studies on the presence of Mycobacterium spp. in milk and milk-based products.
Authors’ information
MMJF: M.V. M.Sc., School of Veterinary Medicine and Animal Science, Sao Paulo State University.
ACP: M.V. M.Sc. Ph.D., Professor at School of Veterinary Medicine and Animal Science, Sao Paulo State University.
MGR: M.V. M.Sc. Ph.D., Professor at School of Veterinary Medicine and Animal Science, Sao Paulo State University.
CQFL: Pharmaceutist, M.Sc. Ph.D., Professor at School of Pharmacy Sciences, Sao Paulo State University.
JCFP: M.V. M.Sc. Ph.D., Professor at School of Veterinary Medicine and Animal Science, Sao Paulo State University.
RGM: M.V. M.Sc., School of Veterinary Medicine and Animal Science, Sao Paulo State University.
ACBS: M.V. M.Sc. Ph.D., School of Pharmacy Sciences, Sao Paulo State University.
MM: Biologist M.Sc. Ph.D., School of Pharmacy Sciences, Sao Paulo State University.
FJPL: Laboratory Technician, School of Veterinary Medicine and Animal Science, Sao Paulo State University.
Abbreviations
- HIV:
-
Human immunodeficiency virus
- M.:
-
Mycobacterium
- MTBC:
-
Mycobacterium tuberculosis complex
- PCR:
-
Polimerase chain reaction
- PNCEBT:
-
‘Programa Nacional de Controle e Erradicação da Brucelose e Tuberculose’
- PRA:
-
Restriction enzyme pattern analysis polymerase chain reaction
- UNESP:
-
Sao Paulo State University
- NTM:
-
Environmental nontuberculous mycobacteria
- FAPESP:
-
‘Fundação de Apoio à Pesquisa do Estado de São Paulo’
- CNPq:
-
‘Conselho Nacional de Desenvolvimento Científico e Tecnológico’.
References
Di Pinto A, Ciccarese G, Forte TV, Bijo B, Shehu F, Tantillo G: Detection of mycobacterium tuberculosis complex in milk using polimerase chain reaction (PCR). Food Control. 2006, 17: 776-780. 10.1016/j.foodcont.2005.04.019.
Chye FY, Abdullah A, Ayob MK: Bacteriological quality and safety of raw milk in Malaysia. Food Microbiol. 2004, 21: 535-541. 10.1016/j.fm.2003.11.007.
American Veterinary Medical Association: One health: A new Professional Imperative. One Health Initiative Task Force: Final Report. One Health World – World Health Through Collaboration. https://www.avma.org/KB/Resources/Reports/Documents/onehealth_final.pdf.
Quinn PJ, Markey BK, Carter ME, Donnelly WJ, Leonard FC: MicrobiologiaVeterinária e Doenças Infecciosas. Porto Alegre: Artmed Press; 2005.
Bernard F, Vincent C, Matthieu L, David R, James D: Tuberculosis and brucellosis prevalence survey on dairy cattle in Mbarara Milk basin (Uganda). Prev Vet Med. 2005, 67: 267-281. 10.1016/j.prevetmed.2004.11.002.
De La Rua-Domenech R: Human Mycobacterium bovis infection in the United Kingdom: incidence, risks, control measures, and review of the zoonotic aspects of bovine tuberculosis. Tuberculosis. 2006, 86: 77-109. 10.1016/j.tube.2005.05.002.
Boland F, Kelly GE, Good M, More SJ: Bovine tuberculosis and milk production in infected dairy herds in Ireland. Prev Vet Med. 2010, 93: 153-161. 10.1016/j.prevetmed.2009.09.021.
Brazil. Ministry of Agriculture, Livestock and Supply: Instrução Normativa n° 2, de 10 de janeiro de. 2001, http://sistemasweb.agricultura.gov.br/sislegis/action/detalhaAto.do?method=consultarLegislacaoFederal.
Brazil. Ministry of Agriculture, Livestock and Supply: Instrução Normativa n∘ 62, de 29 de dezembro de. 2011, http://sistemasweb.agricultura.gov.br/sislegis/action/detalhaAto.do?method=consultarLegislacaoFederal.
Nero LA, Mattos MR, Beloti V, Barros MAF, Netto DP, Pinto JPAN, Andrade NJ, Silva WP, Franco BDGM: Hazards in non-pasteurized milk on retail sale in Brazil: prevalence of Salmonella spp, Listeria monocytogenes and chemical residues. Braz J Microbiol. 2004, 35 (3): 211-215. 10.1590/S1517-83822004000200007.
Balian SC, Pinheiro SR, Guerra JL, Morais ZM, Ferreira F, Ferreira Neto JS: Estudo comparativo de dois métodos de descontaminação na pesquisa de micobactérias. Arq Inst Biológico. 2002, 69 (2): 11-14.
Telenti A, Marchesi F, Balz M, Bally F, Botrger EC, Bodmer T: Rapid identification of mycobacteria to the species level by polymerase chain reaction and restriction enzyme analysis. J Clin Microbiol. 1993, 31: 175-178.
Prasite, Identification of Mycobacteria: http://app.chuv.ch/prasite/index.html.
Chimara E, Ferrazoli L, Leão SC: Mycobacterium tuberculosis complex differentiation using gyrb restriction fragment length polymorphism analysis. Mem Inst Oswaldo Cruz. 2004, 99 (7): 745-748. 10.1590/S0074-02762004000700014.
R Development Core Team: R: A language and environment for statisticalcomputing. Vienna, Austria: R Foundation for Statistical Computing; 2011. http://www.R-project.org.
Byrne WJ, McCormack R, Ball HJ, Brice N, Baker SE, Ayling RD, Nicholas AJ: Application of an indirect ELISA to milk samples to identify cows with Mycoplasma bovis mastitis. Vet Rec. 2000, 146 (13): 368-369. 10.1136/vr.146.13.368.
Sergeant ES, Nielsen SS, Toft N: Evaluation of test-strategies for estimatingt probability of low prevalence of paratuberculosis in Danish dairy herds. Prev Vet Med. 2008, 85: 92-106. 10.1016/j.prevetmed.2008.01.005.
Lombard JE, Byrem TM, Wagner BA, Mccluskey BJ: Comparison of milk and serum enzyme-linked imunossorbent assays for diagnosis of Mycobacterium avium subspecies paratuberculosis infection in dairy cattle. J Vet Diagn Invest. 2006, 18: 448-458. 10.1177/104063870601800504.
Jeon B-Y, Kim SC, Je S, Kwak J, Cho JE, Woo JT, Seo S, Shim HS, Park BO, Lee SS, Cho SN: Evaluation of enzyme-linked imunossorbent assay using milk samples as a potential screening test of bovine tuberculosis of dairy cows in Korea. Res Vet Sci. 2010, 88 (3): 390-393. 10.1016/j.rvsc.2009.12.002.
Roosevelt JJ, Jenkins DE, Hsu KHK: Raw milk as a source of mycobacteria. Can J Microbiol. 1965, 12 (10): 979-984.
Hosty TS, MacDurmont CI: Isolation of acid-fast organisms from milk and oysters. Health Lab Sci. 1975, 12 (1): 16-19.
Appuswamy S, Batish VK, Parkashi OM, Ranganathan B: Prevalence of mycobacteria in raw milk sampled in Karnal. India. J of Food Prot. 1980, 43 (4): 778-781.
Sanchez I, Rosell R: Principales fuentes de infeccion de micobacterias atipicas en unidades bovinas. Rev Cubana Cien Vet. 1983, 14 (1): 29-33.
Guindi SM, Ahmed OL, Awad WM, El-Saban MS, Saban MA: Incidence of bovine and human tubercle bacilli in milk and milk products. Agriculture Res Rev. 1980, 58 (1): 75-84.
Briet F, Boschiroli ML, Thorel MF, Guilloteau LA: Zoonotic aspects of Mycobacterium bovis and Mycobacterium avium-intracellulare complex (MAC). Vet Res. 2004, 36: 411-436.
Kleeberg HH: Human tuberculosis of bovine origin in relation to public health. Rev Sci Tech. 1984, 3: 11-76.
Secretaria Estadual da Saúde de São Paulo: Micobacterioses: recomendações para o diagnóstico e tratamento. ftp://ftp.cve.saude.sp.gov.br/doc_tec/tb/MNT_Final_9-12-05a.pdf
Primm TP, Lucero CA, Falkinham JO: Health impacts of environmental mycobacteria. Clin Microbiol Rev. 2004, 17 (1): 98-106. 10.1128/CMR.17.1.98-106.2004.
Weinberger M, Berg SL, Feuerstein IM, Pizzo PA, Witebsky FG: Disseminated infection with Mycobacterium gordonae: report of a case and critical review of the literature. Clin Infect Dis. 1992, 14 (6): 1229-1239. 10.1093/clinids/14.6.1229.
Leão SC, Martin A, Mejia GI, Palomino JC, Robledo J, Telles MAS, Portaels F: Practical handbook for the phenotypic and genotypic identification of mycobacteria. 2004
Suffys P, Rocha AS, Brandão A, Vanderborght B, Mijs W, Jannes G, Mello FCQ, Pedro HSP, Fonseca LS, Oliveira RS, Leão SC, Saad MHF: Detection of mixed infections with Mycobacterium lentiflavum and Mycobacterium avium by molecular genotyping methods. J Med Microbiol. 2006, 55: 127-131. 10.1099/jmm.0.46218-0.
Adékambi T: Mycobacterium mucogenicum group infections: a review. Clin Microbiol Infect. 2009, 15 (10): 911-918. 10.1111/j.1469-0691.2009.03028.x.
Can bacteria make you smarter?: http://www.sciencedaily.com.
Gangadharam PRJ, Jenkins PA: Mycobacteria: Basic aspects. New York:Chapman & Hall; 1998.
Wetzstein M, Greenfield J: Mastitis caused by a Mycobacterium sp. Can Vet J. 1992, 33 (9): 826.
Dunn BL, Hodgson DJ: “Atypical” mycobacteria in milk. J Appl Bacteriol. 1982, 52 (3): 373-376. 10.1111/j.1365-2672.1982.tb05067.x.
Pardo RB, Langoni H, Mendonça LJP, Chi KD: Isolation of Mycobacterium spp. in milk from cows suspected or positive to tuberculosis. Braz J Vet Res Anim Sci. 2001, 38 (6): 284-287. 10.1590/S1413-95962001000600007.
Holsinger VH, Rajkowski KT, Stabel JR: Milk pasteurization and safety: a brief history and update. Sci Tech Rev. 1997, 12 (2): 441-451.
Richardson A: Bovine mastitis associated with Mycobacterium smegmatis and an untypable Mycobacterium. Vet Rec. 1970, 86: 497-498. 10.1136/vr.86.17.497.
Bohsali A, Abdalla H, Velmurugan K, Briken V: The non-pathogenic mycobacteria M. smegmatis and M. fortuitum induce rapid host cell apoptosis via a caspase-3 and TNF dependent pathway. BMC Microbiol. 2010, 10: 237.
Sampaio JLM, Nassar D, De Freitas D, Höfling-Lima AN, Miyashiro K, Alberto FL, Leão SC: An outbreak of Keratitis caused by mycobacterium immunogenum. J Clin Microbiol. 2006, 44 (9): 3201-3207. 10.1128/JCM.00656-06.
Falkinham JO: Effects of biocides and other metal removal fluid constituents on Mycobacterium immunogenum. Appl Environ Microbiol. 2009, 75 (7): 2057-2061. 10.1128/AEM.02406-08.
Singh S, Krishnamoorthy G, Shahdad S, Kaur M, Singh B, Sharma P: Nontuberculous infections in Indian AIDS patients detected by a novel set of ESAT-6 polimerase chain reaction primers. Jpn J Infect Dis. 2007, 60: 14-18.
Tuffley RE, Holbeche JD: Isolation of the Mycobacterium avium-M. intracellulare-M. scrofulaceum complex from tank water in Queensland, Australia. Appl Environ Microbiol. 1980, 39 (1): 48-53.
Shojaei H, Hashemi A, Heidarieh P, Naser AD: Mycobacterium novocastrense–associated pulmonary and wound infections [letter]. Emerg Infect Dis. 2011, 17 (3): 550-551. 10.3201/eid1703.101400.
Smith S, Lindholm-Levy P, Huitt GA, Heifets LB, Cook JL: Mycobacterium terrae: case reports, literature review, and in vitro antibiotic susceptibility testing. Clin Infect Dis. 2000, 30 (3): 444-453. 10.1086/313693.
Washington W, Stephen A, William J, Koneman E, Procop G, Schreckenberger P, Woods G: Koneman Diagnóstico Microbiológico Texto e Atlas Colorido. Rio de Janeiro: Guanabara-Koogan; 2006.
Falkinham JO: Epidemiology of infection by nontuberculous mycobacteria. Clin Microbiol Rev. 1996, 9: 177-215.
Acknowledgements
To ‘Fundação de Apoio à Pesquisa do Estado de Sao Paulo–FAPESP’ (process number 2010/18209–5) and to ‘Conselho Nacional de Desenvolvimento Científico e Tecnológico-CNPq’ (process number 146975/2010-3) for the financial support.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
MMJF: Conducted the mycobacterial culture-based procedures and the molecular identification of the species. Participated in the statistical analysis of the data. Drafted the manuscript. Read and approved the final manuscript. ACP: Conceived of and designed the study. Helped to draft the manuscript. Generally supervised the research group. Read and approved the final manuscript. MGR: Conceived of and designed the study. Helped to draft the manuscript. Generally supervised the research group. Read and approved the final manuscript. CQFL: Participated in the molecular identification of the species. Generally supervised the research group. Read and approved the final manuscript. JCFP: Performed the statistical analysis of the data. Read and approved the final manuscript. RGM: Acquired the samples and data on the population characteristics. Read and approved the final manuscript. ACBS: Participated in the molecular identification of the species. Read and approved the final manuscript. MM: Participated in the molecular identification of the species. Read and approved the final manuscript. FJPL: Participated in the mycobacterial culture-based procedures. Read and approved the final manuscript.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Franco, M.M.J., Paes, A.C., Ribeiro, M.G. et al. Occurrence of mycobacteria in bovine milk samples from both individual and collective bulk tanks at farms and informal markets in the southeast region of Sao Paulo, Brazil. BMC Vet Res 9, 85 (2013). https://doi.org/10.1186/1746-6148-9-85
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1746-6148-9-85