Abstract
Background
One third to two thirds of people with schizophrenia have persistent psychotic symptoms despite clozapine treatment. Under real-world circumstances, the need to provide effective therapeutic interventions to patients who do not have an optimal response to clozapine has been cited as the most common reason for simultaneously prescribing a second antipsychotic drug in combination treatment strategies. In a clinical area where the pressing need of providing therapeutic answers has progressively increased the occurrence of antipsychotic polypharmacy, despite the lack of robust evidence of its efficacy, we sought to implement a pre-planned protocol where two alternative therapeutic answers are systematically provided and evaluated within the context of a pragmatic, multicentre, independent randomised study.
Methods/Design
The principal clinical question to be answered by the present project is the relative efficacy and tolerability of combination treatment with clozapine plus aripiprazole compared with combination treatment with clozapine plus haloperidol in patients with an incomplete response to treatment with clozapine over an appropriate period of time. This project is a prospective, multicentre, randomized, parallel-group, superiority trial that follow patients over a period of 12 months. Withdrawal from allocated treatment within 3 months is the primary outcome.
Discussion
The implementation of the protocol presented here shows that it is possible to create a network of community psychiatric services that accept the idea of using their everyday clinical practice to produce randomised knowledge. The employed pragmatic attitude allowed to randomly allocate more than 100 individuals, which means that this study is the largest antipsychotic combination trial conducted so far in Western countries. We expect that the current project, by generating evidence on whether it is clinically useful to combine clozapine with aripiprazole rather than with haloperidol, provides physicians with a solid evidence base to be directly applied in the routine care of patients with schizophrenia.
Trial Registration
Clincaltrials.gov Identifier: NCT00395915
Similar content being viewed by others
Background
Schizophrenia is a disabling mental disorder [1]. It affects as much as 1% of the population worldwide and it is characterised by psychotic symptoms, including delusions and hallucinations, negative symptoms, characterised by "loss of function", and cognitive impairment [2].
A proportion of one fifth to one third of patients with schizophrenia derive little or no benefit from treatment with conventional or novel antipsychotics [3]. In these treatment-refractory patients, e.g. individuals who had not responded, or had intolerable side-effects, to conventional and novel agents, clozapine has been shown to be the treatment of choice [4–6]. Clozapine is, however, only effective in producing clinically significant symptom improvement in 30–50% of people receiving treatment. One third to two thirds of people still have persistent psychotic symptoms despite clozapine monotherapy of adequate dosage, or have unwanted side-effects that do not permit an adequate up titration of clozapine [7].
Under real-world circumstances, the need to provide effective therapeutic interventions to patients who do not have an optimal response to clozapine has been cited as the most common reason for simultaneously prescribing two or more antipsychotic drugs in combination treatment strategies [8]. Similarly, adopting a pragmatic attitude, European and American treatment guidelines recognize that the concurrent prescription of a second antipsychotic in addition to clozapine is a common-sense strategy in these partially responsive patients [9–12]. However, it remains unclear if there is an evidence base to support one specific antipsychotic in combination with clozapine [13–16]. In a clinical area where the pressing need of providing therapeutic answers has progressively increased the occurrence of antipsychotic polypharmacy, despite the lack of robust evidence of its efficacy, we sought to implement a pre-planned protocol where two alternative therapeutic answers are systematically provided and evaluated within the context of a pragmatic, multicentre, independent randomised study.
The article reported here aims at providing a description of the following background aspects related to the development and implementation of this project: (a) the Italian legislation on independent trials; (b) the concept of pragmatic trials; (c) the marketing of aripiprazole, a novel antipsychotic drug. We additionally provide a description of the main aspects related to the design and current status of the Clozapine plus Haloperidol or Aripiprazole Trial (CHAT).
Italian Legislation on Independent Trials
The Italian context of care is an ideal setting for independent randomised trials, given the implementation of a National Law (Decreto Ministeriale 17/12/04) that formally recognised the public health value of independent studies investigating the real-world effectiveness of already marketed pharmacological treatments. In 2004 a Ministerial Decree was issued establishing rules to help implement pragmatic independent phase IV clinical trials. In essence, the Decree states that if the following set of conditions are met, (i) the study coordinating centre is independent of drug company support, (ii) study results can be disseminated autonomously, (iii) there is no personal financial interest in studying the drugs included in the trial, (iv) the study drugs are licensed for the indication to be investigated, then the National Health Service (NHS) materially supports the conduct of the trial in three ways: (i) drug costs are paid by the NHS; (ii) there are no fees for submitting the study protocol to the local Ethics Committees; (iii) continuing medical education credits are provided to local investigators.
Considering that all above mentioned criteria are met by CHAT, we took fully advantage of such legislation. In particular, drug costs (clozapine, aripiprazole and haloperidol) are covered by the local health authorities, with two advantages: first, we had the possibility to carry out this study on a low budget, independently from drug companies and from other agencies; second, the drugs under study are prescribed in a way that is identical to that normally followed under real-word circumstances, with obvious advantages in terms of generalisability of study findings.
Pragmatic Versus Explanatory Design
In recent years there has been a renewal of interest in pragmatic trials (also called practical, effectiveness or management trials), that is for studies that randomly assign real-world patients to licensed drugs with the aim of assessing their effectiveness [17–20]. While explanatory (or phase III) trials answer questions about whether an intervention can work under ideal conditions (efficacy), pragmatic (or phase IV) trials attempt to answer questions about whether an intervention will work in the real world. Explanatory trials are usually carried out by the pharmaceutical industry, while pragmatic trials are more often undertaken by groups of clinical researchers. Recent examples of pragmatic trials include the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) [21] and the Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study (CUtLASS) [22].
In Italy a seminal pragmatic study was an unblinded trial of intravenous streptokinase in early acute myocardial infarction that enrolled 11,806 patients in one hundred and seventy-six coronary care units [23]. The first report of this influential study was published in 1986 and in subsequent years there was an ongoing debate about the need to support such research.
In the field of mental health, however, only in very recent years criticism has focused on the current standard of the design of explanatory clinical trials. These studies typically enrol highly selected patients that are shortly followed and assessed with rating scales that are seldom used in clinical practice. In Italy this criticism has progressively led mental health professionals to constitute research networks with the aim of developing pragmatic studies. Such studies, ideally, are intended to answer real-world questions by enrolling everyday patients to be followed in the long-term using pragmatic outcome criteria commonly used in practice. Pragmatic measures include suicide attempts, treatment switching, hospitalization, school failure or truancy, job loss, or treatment discontinuation [17, 18, 24]. CHAT is the first Italian example of this new attitude [25], and other studies will soon follow [26].
Aripiprazole, a novel antipsychotic drug
In recent years the availability of newer antipsychotic agents has increased the therapeutic options available in the management of clozapine partial responders and, among these newer agents, anecdotal reports have hypothesised a promising role for aripiprazole [27, 28]. Aripiprazole is a potent (high-affinity) partial agonist at D2 and 5-HT1A receptors and a potent antagonist at 5-HT2A receptors. In contrast to some of the other atypical antipsychotic agents, treatment with aripiprazole appears to be associated with minimal weight gain and minimal negative impact on metabolic parameters, a key aspect given that these adverse effects might occur during clozapine treatment [29, 30]. In terms of positive symptoms, it has been suggested that the combination of clozapine and aripiprazole may lead to greater D2 receptor antagonism in mesolimbic pathways, and, additionally, may combine D2 and D4 antagonism (although the role of D4 receptors in antipsychotic efficacy is unclear). A challenging neurobiological rationale, with a highly synergistic antipsychotic potency without increasing the risk of adverse effects, has therefore been proposed [15]. Henderson and colleagues, who conducted a six-week open label trial to examine the effects of adjunctive aripiprazole in clozapine-treated subjects, showed that this combination had little or no effect in terms of psychotic symptoms, but was associated with a significant decrease in weight, body mass index, fasting total serum cholesterol and total triglycerides [31]. The only randomised placebo-controlled trial published so far, which included 62 clozapine-treated patients with refractory schizophrenia that were randomly assigned to double-blind combination treatment with aripiprazole or placebo, showed that aripiprazole did not lead to better control of symptom severity after 8 weeks of treatment, but benefits were observed in terms of negative symptoms [32].
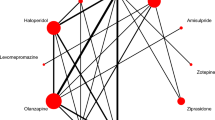
Other trials employed a design similar to that of CHAT, that is pragmatically assessed the relative efficacy of competitive combination strategies, including clozapine + risperidone versus clozapine + sulpiride, clozapine + quetiapine versus clozapine + amisulpiride, and clozapine + risperidone versus clozapine + ziprasidone [33–35].
Design and Methods
Design of The Clozapine Haloperidol Aripiprazole Trial (CHAT)
The principal clinical question to be answered by CHAT is the relative effectiveness and tolerability of combination treatment with clozapine plus aripiprazole compared to combination treatment with clozapine plus haloperidol in patients with an incomplete response to treatment with clozapine over an appropriate period of time. CHAT is a prospective, multicentre, randomized, parallel-group, superiority trial that follows patients over a period of 12 months. Consecutive patients meeting the trial entry criteria were randomly assigned to combination with aripiprazole or haloperidol. These patients constituted the randomised cohort (Figure 1). Patients meeting the trial entry criteria that were not randomly assigned to competitive treatments were followed under real-world circumstances. These patients constituted the observational cohort (Figure 1). In both the experimental and observational cohort patients and clinicians were not blind to pharmacological treatments provided during the trial. Patients will be assessed at baseline, at 3, 6 and 12 months using the instruments reported in Figure 2.
According to Italian legislation, ethics approval was received in each participating site. All phases of CHAT will be recorded following the Consolidated Standard of Reporting of Trials (CONSORT) statement [36].
Primary outcome
Withdrawal from allocated treatment within 3 months is the primary outcome. This outcome was selected because stopping or changing antipsychotic combination treatment is a frequent occurrence and major problem in the treatment of patients with schizophrenia. In addition, according to Lieberman and colleagues, this measure integrates patients' and clinicians' judgments of efficacy, safety, and tolerability into a global measure of effectiveness that reflects their evaluation of therapeutic benefits in relation to undesirable effects [21].
Secondary outcomes
Withdrawal from allocated treatment within 12 months, and time to withdrawal, are used to assess the overall acceptability and efficacy over a long period of time. Additionally, severity of illness is measured by means of the Brief Psychiatric Rating Scale (BPRS) [37]. The BPRS consists of 24 items measuring the following dimensions: positive symptoms, negative symptoms, depression/anxiety and disorganization. All investigators received training to use this rating scale. However, no formal inter-rater exercise has been performed.
Instead of measuring adverse events as observed and reported by the treating clinicians, CHAT measured the perspective of patients exposed to antipsychotic agents by means of the Liverpool University Neuroleptic Side-Effect Rating Scale (LUNSERS) [38]. LUNSERS is a self-rated, semi-structured interview consisting of 51 items that produces a total score that indicates the burden of side effects as perceived by patients (subjective tolerability).
Inclusion/exclusion criteria
Patients were recruited in Italy. Community psychiatric services agreeing to take part to the study were asked to recruit inpatients and outpatients meeting the inclusion/exclusion criteria over a period of 24 months. Patients meeting the eligibility criteria and the criteria for random allocation (see Additional file 1) were randomly allocated to either aripiprazole or haloperidol, in combination with clozapine, and will be followed for 12 months (experimental cohort). Patients meeting the eligibility criteria, but not the criteria for random allocation, will be followed for 12 months under real-world circumstances and assessed using the same assessment tools employed for patients included in the experimental cohort (observational cohort).
Pharmacological treatments
In the experimental cohort, in order to resemble everyday clinical practice, clinicians were allowed to prescribe the allocated pharmacological treatments (starting dose and dose changes) according to clinical status and circumstances. All dose changes will be recorded. Following randomization, treatment is to be taken daily for 1 year unless some clear reason to stop develops. Before random allocation, patients were asked to discontinue any antipsychotic drugs other than clozapine. Long-acting antipsychotic drugs needed to be discontinued for at least two weeks before random allocation. All other concomitant medications were permitted. Routine care outside the trial continued as usual. During the study, participants are seen as often as clinically indicated with no extra visits required for the trial.
Patients in the observational cohort received pharmacological and non-pharmacological treatment as clinically indicated. In addition, participants are seen as often as clinically indicated with no extra visits required.
Power analysis for sample size calculation
At the time of development of the CHAT, only one antipsychotic trial employed discontinuation by any cause as the primary endpoint [21]. On the basis of this trial, it was initially hypothesised a withdrawal proportion from allocated treatment within 3 months (primary study endpoint) of 25% in the group treated with clozapine plus haloperidol (control group). Moreover, it was hypothesised that the augmentation with aripiprazole (experimental group) would show a clinically significant advantage by producing a withdrawal proportion of 10%. A sample size of 194 patients (97 in each group) was chosen since it achieves 80% power to detect a difference of 15% between the two withdrawal proportions. The test statistic used was the two-sided Z test with pooled variance. The significance level of the test was targeted at 5%. Having assumed that 10% of the participants could be lost within 3 months, or could not provide valid data at month 3, the target total sample size for CHAT was 216 (= 194/0.90) patients in order to obtain 194 evaluable subjects [39, 40].
Having considered the possibility that the target sample size could not be reached, we anticipated that the total sample size at the end of the enrolment period would be around 100 patients. With such a total sample size, CHAT achieves 80% power to detect a difference of 20% between the two withdrawal proportions (25% in the group treated with clozapine plus haloperidol versus 5% in the group treated with clozapine plus aripiprazole).
Random Allocation Procedure
Patients were randomly assigned to one of the two treatment groups with an equal probability of assignment to each treatment (allocation ratio 1:1). A centralised randomization procedure was employed. The trial biostatistician prepared the sequence of treatments randomly permuted in blocks of constant size. The site investigators did not know the block size. The allocation was stratified by living condition (residential facility versus all the other living conditions) because in patients with resistant schizophrenia this hard variable may be considered a proxy of severity of illness. Recruiting physicians were asked to contact an operator at the World Health Organisation Collaborative Centre of the University of Verona. The operator had access to a computerised system that provides, after information on the enrolled participant was entered, the patient's identification number (ID) and the allocated treatment. The operator had not access to the randomisation lists. This procedure of randomisation was developed to fully conceal treatment allocation [41].
Statistical consideration
The statistical analysis will be masked, i.e. the trial biostatistician will be blinded to the treatment groups until the analysis has been completed. Moreover, the trial biostatistician will not be involved in determining patients' eligibility, in administering the treatment, in measuring the outcomes or in entering data.
Two data locks will occur during the study. The first one will happen 3 months after the end of the enrolment period, when the information on the primary endpoint and on the short-term secondary endpoints will be available for all the participants. The second one will happen at the end of the study (12 months after the end of the enrolment period), when information on the long-term secondary endpoints will be available for all participants. Accordingly, two data analyses will be performed on an intention-to-treat (ITT) basis. All randomised participants who will receive at least one dose of the investigational drugs will be included in the ITT analysis. The outcomes of patients included in the non-randomized cohort will be presented descriptively. No formal statistical analysis has been planned to compare the randomized participants and the eligible, non-randomized patient cohort.
Analysis of the Primary Outcome
In the randomized cohort, the proportion of patients withdrawing from the assigned treatment within 3 months will be compared between the two groups of treatment through the chi-square test. Additionally, we will calculate risk ratios and their 95% confidence intervals to corroborate the main analysis. A multivariate analysis (secondary analysis) will be performed through a Poisson regression model with a robust error variance, given that this procedure allows to estimate relative risks directly [42].
Status of the trial and expected achievements
The recruitment phase started on September 1st 2006 and finished on December 31st 2008. During this period, 38 clinical sites across Italy actively participated in the study and recruited a total of 106 patients. This means that, despite the planned sample size of 216 patients has not been achieved, CHAT is the largest randomised study conducted so far in Western countries on this topic. Data collection, study monitoring and data management are performed by the coordinating centre (University of Verona). All study data are entered in a computerised database and stored by the World Health Organisation Collaborative Centre of the University of Verona. The person entering the data is not involved in determining patients' eligibility, administering treatment, or determining outcome. The correctness and consistency of the data is ensured by the double-entry technique and by a set of electronic and manual edit checks. The consistency of the data between the recruitment and follow-up forms and the computerised database are routinely verified. After each of the two data locks, masked data will be transferred to the Unit of Epidemiology and Medical Statistics of the University of Verona for statistical analysis.
The main achievements of this ongoing projects include the following: (a) the implementation of the CHAT protocol provides evidence that it is possible to create a network of community psychiatric services that accept the idea of using their everyday clinical practice to produce randomised knowledge; (b) the possibility of producing knowledge from the practice of medicine does not necessarily require huge financial support, as long as a pragmatic attitude to the evaluation of competitive treatment strategies is adopted; (c) the multicentre design, nested into everyday clinical practice, has been creating a situation where investigators simultaneously act both as physicians and researchers; (d) the pragmatic attitude employed allowed to randomly allocate considerable number of individuals [43]; (e) the current project, by generating evidence on whether it is clinically useful to combine clozapine with aripiprazole rather than with haloperidol, is expected to provide physicians with a solid evidence base to be directly applied in the routine care of patients with schizophrenia.
References
Mueser KT, McGurk SR: Schizophrenia. Lancet. 2004, 363: 2063-2072. 10.1016/S0140-6736(04)16458-1.
Flaum M, Schultz SK: The core symptoms of schizophrenia. Ann Med. 1996, 28: 525-531. 10.3109/07853899608999116.
Conley RR, Kelly DL: Management of treatment resistance in schizophrenia. Biol Psychiatry. 2001, 50: 898-911. 10.1016/S0006-3223(01)01271-9.
Kane J, Honigfeld G, Singer J, Meltzer H: Clozapine for the treatment-resistant schizophrenic. A double-blind comparison with chlorpromazine. Arch Gen Psychiatry. 1988, 45: 789-796.
Rosenheck R, Cramer J, Xu W, Thomas J, Henderson W, Frisman L: A comparison of clozapine and haloperidol in hospitalized patients with refractory schizophrenia. Department of Veterans Affairs Cooperative Study Group on Clozapine in Refractory Schizophrenia. N Engl J Med. 1997, 337: 809-815. 10.1056/NEJM199709183371202.
Wahlbeck K, Cheine M, Essali A, Adams C: Evidence of clozapine's effectiveness in schizophrenia: a systematic review and meta-analysis of randomized trials. Am J Psychiatry. 1999, 156: 990-999.
Chakos M, Lieberman J, Hoffman E, Bradford D, Sheitman B: Effectiveness of second-generation antipsychotics in patients with treatment-resistant schizophrenia: a review and meta-analysis of randomized trials. Am J Psychiatry. 2001, 158: 518-526. 10.1176/appi.ajp.158.4.518.
Sernyak MJ, Rosenheck R: Clinicians' reasons for antipsychotic coprescribing. J Clin Psychiatry. 2004, 65: 1597-1600.
American Psychiatric Association: Practice guideline for the treatment of patients with schizophrenia. Am Fam Physician. 1997, 56 (4): 1217-1220.
National Collaborating Centre for Mental Health: Schizophrenia. Core interventions in the treatment and management of schizophrenia in primary and secondary care. 2002, London: National Institute for Clinical Excellence – NICE Guidelines
Miller AL, Hall CS, Buchanan RW, Buckley PF, Chiles JA, Conley RR: The Texas Medication Algorithm Project antipsychotic algorithm for schizophrenia: 2003 update. J Clin Psychiatry. 2004, 65: 500-508.
Clinical practice guidelines: Treatment of schizophrenia. Can J Psychiatry. 2005, 50: 7S-57S.
Correll CU, Rummel-Kluge C, Corves C, Kane JM, Leucht S: Antipsychotic Combinations vs Monotherapy in Schizophrenia: A Meta-analysis of Randomized Controlled Trials. Schizophr Bull. 2008, 35: 443-57. 10.1093/schbul/sbn018.
Kontaxakis VP, Ferentinos PP, Havaki-Kontaxaki BJ, Roukas DK: Randomized controlled augmentation trials in clozapine-resistant schizophrenic patients: a critical review. Eur Psychiatry. 2005, 20: 409-415. 10.1016/j.eurpsy.2004.12.007.
Mouaffak F, Tranulis C, Gourevitch R, Poirier MF, Douki S, Olie JP: Augmentation strategies of clozapine with antipsychotics in the treatment of ultraresistant schizophrenia. Clin Neuropharmacol. 2006, 29: 28-33. 10.1097/00002826-200601000-00009.
Paton C, Whittington C, Barnes TR: Augmentation with a second antipsychotic in patients with schizophrenia who partially respond to clozapine: a meta-analysis. J Clin Psychopharmacol. 2007, 27: 198-204. 10.1097/JCP.0b013e318036bfbb.
Schwartz D, Lellouch J: Explanatory and pragmatic attitudes in therapeutical trials. J Chronic Dis. 1967, 20: 637-648. 10.1016/0021-9681(67)90041-0.
March JS, Silva SG, Compton S, Shapiro M, Califf R, Krishnan R: The case for practical clinical trials in psychiatry. Am J Psychiatry. 2005, 162: 836-846. 10.1176/appi.ajp.162.5.836.
Barbui C, Veronese A, Cipriani A: Explanatory and pragmatic trials. Epidemiol Psichiatr Soc. 2007, 16: 124-125.
Zwarenstein M, Treweek S, Gagnier JJ, Altman DG, Tunis S, Haynes B: Improving the reporting of pragmatic trials: an extension of the CONSORT statement. BMJ. 2008, 337: a2390-10.1136/bmj.a2390.
Lieberman JA, Stroup TS, McEvoy JP, Swartz MS, Rosenheck RA, Perkins DO: Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. N Engl J Med. 2005, 353: 1209-1223. 10.1056/NEJMoa051688.
Jones PB, Barnes TR, Davies L, Dunn G, Lloyd H, Hayhurst KP: Randomized controlled trial of the effect on Quality of Life of second- vs first-generation antipsychotic drugs in schizophrenia: Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study (CUtLASS 1). Arch Gen Psychiatry. 2006, 63: 1079-1087. 10.1001/archpsyc.63.10.1079.
Gruppo Italiano per lo Studio della Streptochinasi nell'Infarto Miocardico (GISSI): Effectiveness of intravenous thrombolytic treatment in acute myocardial infarction. Lancet. 1986, 1: 397-402.
Barbui C, Cipriani A: Evidence-based psychopharmacology: a public health agenda for the future. Evid Based Ment Health. 2007, 10: 4-6. 10.1136/ebmh.10.1.4-a.
Barbui C, Cipriani A, Malvini L, Nose M, Accordini S, Pontarollo F: Turning clinical practice into research. An invitation to participate to the CHAT study. Psichiatria di Comunità. 2007, VI: 62-66.
Barbato A, D'Avanzo B, Ferrannini L, Parabiaghi A, Vaggi M: A chance for clinical research in Italy: The GiSAS study on aripirazole, olanzapine, and haloperidol in the treatment of schizophrenic disorders. Psichiatria di Comunità. 2008, VII: 46-54.
Marder SR, McQuade RD, Stock E, Kaplita S, Marcus R, Safferman AZ: Aripiprazole in the treatment of schizophrenia: safety and tolerability in short-term, placebo-controlled trials. Schizophr Res. 2003, 61: 123-136. 10.1016/S0920-9964(03)00050-1.
Bowles TM, Levin GM: Aripiprazole: a new atypical antipsychotic drug. Ann Pharmacother. 2003, 37: 687-694. 10.1345/aph.1C297.
McQuade RD, Stock E, Marcus R, Jody D, Gharbia NA, Vanveggel S: A comparison of weight change during treatment with olanzapine or aripiprazole: results from a randomized, double-blind study. J Clin Psychiatry. 2004, 65 (Suppl 18): 47-56.
El-Sayeh HG, Morganti C: Aripiprazole for schizophrenia. Cochrane Database Syst Rev. 2004, CD004578-2
Henderson DC, Kunkel L, Nguyen DD, Borba CP, Daley TB, Louie PM: An exploratory open-label trial of aripiprazole as an adjuvant to clozapine therapy in chronic schizophrenia. Acta Psychiatr Scand. 2006, 113: 142-147. 10.1111/j.1600-0447.2005.00612.x.
Chang JS, Ahn YM, Park HJ, Lee KY, Kim SH, Kang UG: Aripiprazole augmentation in clozapine-treated patients with refractory schizophrenia: an 8-week, randomized, double-blind, placebo-controlled trial. J Clin Psychiatry. 2008, 69: 720-731.
Zink M, Kuwilsky A, Krumm B, Dressing H: Efficacy and tolerability of ziprasidone versus risperidone as augmentation in patients partially responsive to clozapine: a randomised controlled clinical trial. J Psychopharmacol. 2008, 23: 305-14. 10.1177/0269881108089593.
Genc Y, Taner E, Candansayar S: Comparison of clozapine-amisulpride and clozapine-quetiapine combinations for patients with schizophrenia who are partially responsive to clozapine: a single-blind randomized study. Adv Ther. 2007, 24: 1-13. 10.1007/BF02849987.
Boso M, Cipriani A, Barbui C: Clozapine combined with different antipsychotic drugs for treatment resistant schizophrenia. Cochrane Database Syst Rev. 2007, CD006324-1
Moher D, Schulz KF, Altman DG: The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomised trials. Lancet. 2001, 357: 1191-1194. 10.1016/S0140-6736(00)04337-3.
Ruggeri M, Koeter M, Schene A, Bonetto C, Vazquez-Barquero JL, Becker T: Factor solution of the BPRS-expanded version in schizophrenic outpatients living in five European countries. Schizophr Res. 2005, 75: 107-117. 10.1016/j.schres.2004.05.017.
Morrison P, Gaskill D, Meehan T, Lunney P, Lawrence G, Collings P: The use of the Liverpool University Neuroleptic Side-Effect Rating Scale (LUNSERS) in clinical practice. Aust N Z J Ment Health Nurs. 2000, 9: 166-176. 10.1046/j.1440-0979.2000.00181.x.
Chow SC, Shao J, Wang H: Sample size calculations in clinical research. 2003, New York: Marcel Dekker
Accordini S: An introduction to sample size calculations in clinical trials. Epidemiol Psichiatr Soc. 2007, 16: 299-301.
Altman DG, Schulz KF: Statistics notes: Concealing treatment allocation in randomised trials. BMJ. 2001, 323: 446-447. 10.1136/bmj.323.7306.224.
Zou G: A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004, 159: 702-706. 10.1093/aje/kwh090.
Barbui C, Signoretti A, Mule S, Boso M, Cipriani A: Does the Addition of a Second Antipsychotic Drug Improve Clozapine Treatment?. Schizophr Bull. 2008, 35: 458-68. 10.1093/schbul/sbn030.
Acknowledgements
We are grateful to the Fondazione Cariverona, who provided a three-year Grant to the WHO Collaborating Centre for Research and Training in Mental Health and Service Organization at the University of Verona, directed by Professor Michele Tansella. We additionally thank Donatella Castiglioni for her invaluable help as study secretary. We are indebted with T. Scott Stroup, Associate Professor of Psychiatry at the University of North Carolina at Chapel Hill, and John R. Geddes, Professor of Epidemiological Psychiatry at the University of Oxford, for their useful comments and suggestions on the drafted study protocol.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
CB, AC, SA, MN, MT participated in the conception and design of the trial. SA is the trial statistician and he made substantial contributions to the study design. AC, AV, FP, EE, SM helped manage the trial, collect reports and design data extraction sheets. PA4, FB5, RB6, DB7, GB8, BB9, AB10, RB9, FB11, MB5, AB12, PB13, MC14, LC10, LC15, GC15, PC16, BDS4, MDF17, GDL18, WDM10, GD19, AEr20, LF3, FF21, AF22, NF23, VFP24, MF20, FG25, NG26, AG19, GG17, LG9, NG20, LG23, GG27, FL12, EL25, CL26, FM28, LM21, LM29, AM30, MCM31, AM14, MM, GM32, MM3, DM22, SN8, FN33, GO13, AMP29, SP23, MP16, EP34, CP32, RP35, RQ36, LRi6, FR29, RR33, PR11, SR19, MR31, GRi6, GR30, AS25, CS36, GS23, AS19, FS34, SS4, TS36, AS18, SS25, GT9, AT35, RT17, RT23, SZ13 participated in enrolling patient (details on superscripts are fully reported in the front page of the manuscript). MN drafted the manuscript. CB and AC critically reviewed the manuscript. All authors saw and approved the final version of the manuscript. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Electronic supplementary material
13063_2009_319_MOESM1_ESM.ppt
Additional File 1: CHAT inclusion and exclusion criteria (both for the randomised and for the observational cohort). The data provided represent the trial inclusion and exclusion criteria. (PPT 97 KB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Nosè, M., Accordini, S., Artioli, P. et al. Rationale and design of an independent randomised controlled trial evaluating the effectiveness of aripiprazole or haloperidol in combination with clozapine for treatment-resistant schizophrenia. Trials 10, 31 (2009). https://doi.org/10.1186/1745-6215-10-31
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1745-6215-10-31