Abstract
Background
Arthritis refers to inflammation of joints and includes common disorders such as rheumatoid arthritis (RA) and spondyloarthropathies (SpAs). These diseases differ mainly in terms of their clinical manifestations and the underlying pathogenesis. Glycoproteins in synovial fluid might reflect the disease activity status in the joints affected by arthritis; yet they have not been systematically studied previously. Although markers have been described for assisting in the diagnosis of RA, there are currently no known biomarkers for SpA.
Materials and methods
We sought to determine the relative abundance of glycoproteins in RA and SpA by lectin affinity chromatography coupled to iTRAQ labeling and LC-MS/MS analysis. We also used ELISA to validate the overexpression of VCAM-1, one of the candidate proteins identified in this study, in synovial fluid from RA patients.
Results and discussion
We identified proteins that were previously reported to be overexpressed in RA including metalloproteinase inhibitor 1 (TIMP1), myeloperoxidase (MPO) and several S100 proteins. In addition, we discovered several novel candidates that were overexpressed in SpA including Apolipoproteins C-II and C-III and the SUN domain-containing protein 3 (SUN3). Novel molecules found overexpressed in RA included extracellular matrix protein 1 (ECM1) and lumican (LUM). We validated one of the candidate biomarkers, vascular cell adhesion molecule 1 (VCAM1), in 20 RA and SpA samples using ELISA and confirmed its overexpression in RA (p-value <0.01). Our quantitative glycoproteomic approach to study arthritic disorders should open up new avenues for additional proteomics-based discovery studies in rheumatological disorders.
Similar content being viewed by others
Background
Bone is a specialized form of connective tissue which undergoes continuous remodelling throughout an individual’s life span [1]. This involves osteoclast-based removal of mineralized bone which is balanced by osteoblast-based bone mineralization [1]. The entire process of bone remodeling is regulated by several factors including immune mediators [1, 2]. In rheumatologic disorders, aberrant presence of these regulators may either lead to progressive and irreversible bone erosion or abnormal bone formation [1, 2]. Rheumatoid arthritis (RA) and spondyloarthropathies (SpA) are two chronic multi-system and complex autoimmune inflammatory disorders which are considerably affected by an abnormal bone remodelling cycle [2, 3]. RA is characterized by excessive bone degradation with relatively low bone formation targeting the small joints of the body in a symmetrical pattern [2, 4]. SpA, on the other hand, encompasses a number of disease subtypes including ankylosing spondylitis, reactive arthritis, arthritis associated with inflammatory bowel disease, psoriatic arthropathy and undifferentiated spondyloarthropathy [5]. Essentially, the major pathological changes in SpA are characterized by an aberrant bone formation that predominantly affects the spine and large joints asymmetrically [6, 7]. The diseases are associated with high morbidity due to pain and of restriction of joint movements resulting in depreciation of quality of life. In addition, these inflammatory autoimmune disorders are associated with increased mortality and reduced life span of almost 10–12 years resulting from cardiovascular and renal complications [8–11]. In light of the significant morbidity and mortality of rheumatological disorders, research into discovering biomarkers for early detection, differential diagnosis, prognosis and response to therapy is critical [12]. Despite the availability of multiple markers for the diagnosis of RA, their performance leaves room for discovering additional biomarkers with better sensitivity and specificity [13]. There are no molecular markers available for the diagnosis of SpA although expression of HLA-B27 has been shown to be associated with development of SpA [14]. Thus, the diagnosis of both of these disorders is largely made based on clinical criteria with serological and radiological markers providing supportive evidence [14, 15].
Generally, disease marker proteins secreted into the bloodstream by affected tissues or cells are expected to be present in relatively low concentration [16–18]. In contrast, proximal fluid obtained from the affected tissue/organ serve as the local environment where the disease manifests and are preferable for discovering disease marker proteins as they are likely to be more abundant [16–18]. In the field of rheumatology, the ideal proximal fluid is the synovial fluid collected by aspiration of affected joints [12]. The hyaluronic acid rich fluid produced by synovial membrane is an ultrafiltrate of blood released from the dense networks of capillaries present in the synovium [19, 20]. This fluid is a lubricant and provides nutrients to cells and tissues of the joints [21]. In the site of pathogenesis, mostly the knee joint, fluid accumulation increases with the severity of the disease [21].
Identification and validation of protein markers in synovial fluid using mass spectrometry is challenging and the major constraint is perhaps the dynamic and complex nature of this fluid, which increases with inflammation of the synovium [19, 22–24]. Previous reports have indicated an increased permeability of synovial membrane for selected plasma proteins during disease states, the majority of which are glycoproteins [25]. Glycoproteins are vital in many biological processes and have been considered critical for biomarker discovery to monitor disease progression and treatment [26]. Disease activity status of a patient could be monitored through the detection of specific glycoproteins released from affected tissues or cells into the proximal fluid [27]. Glycoproteins in particular, have been found to be overexpressed in serum and synovial fluid of RA patients compared to healthy individuals and have been considered critical for rheumatic diseases [28, 29]. Considering the functional importance and applications in biomarker discovery, we sought to determine the relative abundance of glycoproteins across RA and SpA. Essentially, differential expression patterns of proteins can be determined with iTRAQ, ICAT, SILAC or 18O labeling methods, among others [30–33]. To this end, we carried out multilectin affinity-based glycoprotein enrichment from synovial fluid followed by studying protein abundance patterns across RA and SpA by using an iTRAQ-based quantitative proteomics strategy. To our knowledge, this is the first quantitative glycoprotein profiling study of synovial fluid samples. A similar approach of comparative glycoprotein profiling by 18O labeling in hepatocellular cancer tissues and plasma samples by our group has already been reported [32].
In this study, we observed several previously reported marker proteins in addition to a number of novel proteins which could potentially accelerate biomarker discovery in rheumatologic diseases. Additionally, using ELISA, we validated the overexpression of the glycoprotein, VCAM-1, in RA. The use of comparative glycoproteomics for discovering biomarkers and therapeutic targets represents a novel approach that could be generally applied to a spectrum of autoimmune disorders.
Results and discussion
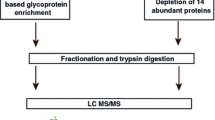
This study was conducted to identify differentially regulated glycoproteins between the two chronic diseases, RA and SpA. Because aspiration of synovial fluid samples from healthy individuals is not permitted for ethical reasons [34] and because molecular markers are required to distinguish different types of arthritis from each other and not from unaffected cases, we chose to compare RA with SpA. The strategy employed in this study is shown in Figure 1. Through this approach, we identified a total of 210 proteins out of which 164 proteins were quantified (35 proteins were identified from single peptide hits with more than one peptide- spectrum match (PSM) while the rest were with two or more peptide hits). From the list, 70 showed a ≥1.5-fold difference between the two groups (combined protein and peptide lists are provided in Additional file 1: Table S1). Gene Ontology-based molecular class and subcellular localization of the identified proteins are shown in Figures 2(A) and (B), respectively, and details provided in Additional file 2: Table S2.
Outline of the strategy implemented in the study. Synovial fluid samples from RA and SpA patients were subjected to multilectin affinity enrichment. Three lectins - Concanavlin A (C), Wheat Germ Agglutinin (W) and Jacalin (J) were pooled together and used for glycoprotein enrichment from synovial fluid samples of RA and SpA. The enriched proteins were trypsin digested followed by iTRAQ labeling (RA with 116 and SpA with 117). The labeled tryptic peptides were pooled and fractionated by SCX chromatography. The samples were then analyzed on an LTQ-Orbitrap Velos mass spectrometer coupled to a nano-HPLC unit. Data obtained were searched using SEQUEST and Mascot. Finally, an ELISA assay was carried out to validate the upregulation of sVCAM-1 in RA as compared to SpA.
Summary of bioinformatics analysis. Protein distribution based on molecular class (A) and subcellular localization (B). Secretory and membrane proteins were observed in the study and the majority was extracellular. Distribution of glycoproteins and non-glycosylated proteins, as illustrated in the form of pie charts (C) with an inset representing the overall distribution of the N-linked glycoproteins, O-linked and those with both types of linkages. From the total number of proteins identified, 62% are glycoproteins and 38% are non-glycoproteins.
Enrichment of glycoproteins
A combination of multiple lectins with different glycan specificities improves the repertoire of proteins containing both N- and O- linked glycoproteins [32]. Thus, we combined three types of lectins, Concanavalin A, Wheat germ agglutinin and Jacalin, to enhance the coverage of glycoproteins captured from the synovial fluid of RA and SpA patients. Of the 210 proteins identified, 131 (62%) were already reported to be glycosylated. The distribution is as illustrated in Figure 2 (C) and Additional file 2: Table S2.
Differentially expressed proteins identified in this study
The number of upregulated proteins in RA as compared to SpA was 44 while 26 proteins were more highly expressed in SpA. Partial lists of these upregulated proteins are provided in Tables 1 and 2, respectively. A brief description of the biological role of the different classes of proteins identified in our study is provided below.
Extracellular matrix proteins
Lumican (LUM) is a major proteoglycan component that binds to collagens in bones and its secretion reflects bone repair [35]. It has been implicated as an atherosclerotic marker that induces collagen fibrillogenesis in coronary atherosclerosis [36]. It was found to be 2-fold upregulated in RA (see Additional file 3: Figure S1A for a representative MS/MS spectrum) and has not previously been linked to this disease. Extracellular matrix protein1 (ECM1), which was >1.5-fold upregulated in RA may be considered as a novel matrix marker protein in RA. It is involved in regulation of endochondral bone formation and activation of the endothelial cell proliferation, thus inducing angiogenesis [37]. This family of extracellular matrix proteins is already reported to be widely studied in atherosclerosis [36, 38]. Further, upregulation of Keratin Type I cytoskeletal protein 14 (KRT14) by 2-fold in RA is in keeping with the already known overexpression of cytokeratins in synovial membranes of RA patients [39].
S100 protein family
We identified both S100A8 and S100A9 proteins as > 4-fold upregulated in RA. They are acidic proteins released by neutrophils and macrophages [40]. In RA, formation of the S100A8/S100A9 complex, also referred to as calprotectin, has been observed to significantly increase with the severity of the disease [41, 42]. It has been implicated in the conversion of normal synovium to a pseudotumoral one called pannus through activation of the Receptor for Advanced Glycation End products (RAGE) protein localized on synoviocytes, which is a receptor for S100 proteins [42]. An MS/MS spectrum of one of the representative peptides of protein S100A8 is shown in Additional file 3: Figure S1(B).
Inflammatory mediators
Among the complement proteins, the notable component identified was complement protein C3. This protein was identified to be 5-fold upregulated in SpA. C3 protein from synovial fluid of SpAs has been already observed to be higher than in RA [43]. It is also known to be elevated in ankylosing spondylitis and decreased in RA compared to unaffected joints [44, 45]. C3 is a central protein involved in the classical pathway of complement activation [46]. Complement component proteins have been considered as potential diagnostic markers for SpAs, which is in keeping with our findings [43]. CD44, commonly known as hyaluronic acid receptor, is an inflammatory marker that has been studied in RA was found to be 2-fold upregulated in RA [47]. It is also referred as osteocyte differentiation marker and plays a significant role in the inhibition of osteoclast differentiation [48]. Myeloperoxidase (MPO) was found to be 3-fold upregulated in RA and has been implicated in tissue damage caused by the release of oxidative radicals usually from neutrophils in RA patients [49].
Complement C5, the fifth component of the complement family of proteins, was observed to be upregulated by 4-fold in SpA (see a representative MS/MS spectrum in Additional file 3: Figure S1(C). In association with other complement proteins, C6, C7 and C8, its proteolytic fragment C5b forms a membrane attack complex to carry out cell lysis of pathogens [50]. It has not been previously associated with SpAs.
Vascular adhesion molecules
Vascular cell adhesion molecule 1 (VCAM1), was found to be 2-fold overexpressed in RA. Its expression, both at the mRNA level in synovial tissues and at the protein level in various sites including synovial membrane, synovial fluid and serum of RA cases, has already been reported [51–53]. In addition to its role in inflammation, VCAM-1 has also been implicated in angiogenesis [54] and in atherosclerosis [55]. We also identified the atherosclerotic marker, vascular endothelial-cadherin designated as cadherin 5 (CDH5), to be >1.5-fold upregulated in RA, providing further evidence for the association of atherosclerosis with RA [56]. In a previous study, TNF α stimulation was reported to induce the release of secretory form of this cadherin in RA patients [56].
Collagenases
Matrix metalloproteinase 9 (MMP9), or gelatinase, was >2-fold upregulated in SpA. This enzyme is a known disease activity marker for arthritis and its level increases with a corresponding increase in degradation of extracellular matrix. It has already been identified in RA and SpA cases [57, 58]. However, to the best of our knowledge, there are no reports on its relative expression across RA and SpA. Metalloproteinase inhibitor 1 (TIMP1) was found to be >1.5-fold upregulated in RA. Increased levels of TIMP-1 have been observed in synovial fluid samples of RA as compared to psoriatic arthritis and are thus in agreement with our data [59].
Membrane proteins
SUN domain-containing protein 3 (SUN3), is a nuclear membrane protein with transmembrane and C terminal SUN domains [60]. This protein binds to Klarsicht/ANC-1/Syne homologue domains thereby forming bridges between outer and inner membranes of a nucleus [60]. It was observed to be 3-fold upregulated in SpA and has not been previously associated with any form of arthritis.
Apolipoproteins
The proteins from serum amyloid protein family identified in this study include serum amyloid P component (APCS; 4-fold higher in SpA) and serum amyloid A (SAA1; 3-fold elevated in SpA). Amyloid deposits in organ systems lead to amyloidosis [61], which is a life-threatening complication in rheumatic diseases and has a prevalence of >5% in rheumatic diseases [61]. These proteins have already been reported in SpAs [62, 63].
Additionally, we identified apolipoprotein C-III, C-II and D proteins. A 2-fold upregulation of apolipoprotein D in RA was identified and it was not reported earlier. Apolipoproteins, C-II and C-III types were each found to be 3-fold downregulated in RA and were never identified in SpA. These proteins are critical in cholesterol metabolism and their increased levels in synovial fluid suggest a higher rate of triglyceride and cholesterol transport which increases the risk of atherosclerosis [64].
Other secretory proteins
Tetranectin (CLEC3B), a secretory glycoprotein of unknown function, was found to be 2-fold upregulated in RA. Its overexpression in serum and synovial fluid of RA as compared to osteoarthritis and SpA have been reported earlier [65]. Vitamin D binding protein (GC), a glycoprotein, was found to be >1.5-fold upregulated in RA and has been reported earlier in synovial fluid and serum samples of RA [66, 67]. These proteins are carrier proteins for 25-hydroxyvitamin D3, and are involved in regulation of bone mineral density [68]. Galectin-3 binding protein, (LGALS3BP), an N-linked glycoprotein, was found to be overexpressed 4-fold in SpA (Additional file 3: Figure S1D). This protein has already been identified in RA [69] although not described earlier in the context of SpA. It is considered as a disease activity marker and possibly plays vital role in the activation of synovial fibroblasts [69].
Validation by ELISA
VCAM-1 has been considered critical for T cell infiltration [70] and is an endothelial dysfunction marker of RA [71]. Elucidation of its dual role in inflammation and endothelial dysfunction in rheumatic disorders has been a major focus for researchers. There are no reports on its differential expression pattern in the synovial fluid in RA and SpA. Given its functional implication in RA and considering the high risk of cardiovascular manifestations, we hypothesized that there should be a significant difference in the expression levels of VCAM-1 across RA and SpA patients. Thus, we carried out sandwich ELISA-based quantification of VCAM-1 in synovial fluid samples of RA (n = 20) and SpA (n = 20) patients. We found that soluble VCAM-1 concentration in RA (2–8.3 μg/ml) was significantly higher than in SpA (1.2-5.7 μg/ml) with a (p-value = 0.002; Mann–Whitney U test). This finding validates our MS-based quantitative data that showed a higher level of VCAM-1 in RA. The MS/MS spectral representation of one of its peptides identified is provided in Figure 3(A) and the relative abundance pattern across RA and SpA from ELISA is shown in Figure 3(B). This data is in agreement with our hypothesis that VCAM-1 may actively participate in the pathogenesis of RA as compared to SpA.
Conclusions
We implemented a multilectin affinity approach to isolate and quantify glycoproteins from the synovial fluid of patients with RA and SpA. In addition to identifying a number of novel candidates, we found several molecules that were in agreement with previous reports. We validated the overexpression of VCAM-1, a potential inflammatory marker in RA with respect to SpA. In addition to VCAM-1, validation of the overexpression of ECM-1 and LUM in RA and ApoC-II, ApoC-III and complement protein C5 in SpAs could provide newer dimensions to biomarker discovery for rheumatological diseases. A combination of markers such as VCAM-1 and cadherin-5 and LUM and ECM-1 in synovial fluid of RA patients could potentially reflect progression of RA with a corresponding increase in atherosclerosis.
When we compared our data with that from pulldown studies with the lectin jacalin as reported by Saroha et al. [72], we observed that almost all of their data overlapped with the list of upregulated proteins in RA identified by our study. These proteins include protein families such as complement proteins, plasma protease C1 inhibitor, immunoglobulins, alpha glycoproteins and fibrinogen. Future studies could focus on peptide level enrichment, which could provide glycosylation sites in addition to potentially reducing any non-specifically bound proteins.
Methods
Collection and processing of synovial fluid samples
Approximately 2–4 ml of synovial fluid was aspirated from knees of 26 patients with RA and 26 patients with SpA and stored in vacutainers containing heparin (BD, NJ, USA) at 4°C. Clinical details of the patients used for are provided in Additional file 4: Table S3. The selection of patients was based on the American College of Rheumatology criteria for RA and on European Spondyloarthropathy Study Group criteria for SpA. The samples were obtained after informed consent from patients and after approval from the ethical committees of the Armed Forces Medical College, Pune, India and Fortis Hospitals, Bangalore, India. The samples were centrifuged at 1,500 g at room temperature for 15 minutes and the supernatants were filtered using 0.22 μm filters (Millipore, Ireland). The filtered samples were stored at −80°C until further analysis. MS-based iTRAQ labeling was performed using the multilectin affinity enriched proteins from 10 pooled synovial fluid samples from each of the two conditions.
Glycoprotein enrichment
Glycoprotein enrichment was carried out by using a mixture of three agarose bound lectins, Wheat germ agglutinin, Concanavalin A and Jacalin (Vector laboratories, USA), as previously described [32]. Agarose-bound lectins were washed and aliquots from each lectin were combined together to form a suspension. Thereafter, the pooled lectins were split equally and each fraction was mixed with synovial fluid containing 5 mg protein obtained from 10 pooled RA or SpA samples and made up to 5 ml using Tris buffered saline (0.05 M Tris–HCl, pH 7.5, 0.15 M NaCl). After overnight incubation at 4°C, the bound glycoproteins were eluted using competitive elution, performed by a mixture of sugars (100 mM each of M-pyranoside, galactose, melibiose and N-acetyl glucoseamine in Tris buffered saline, pH 7.5). The selection of sugars was based on their specificity towards the three lectins used as per the manufacturer’s instructions. The eluates were then washed and concentrated using 3 kDa MWCO filters (Amicon, Millipore, Ireland). The protein amount was estimated by Lowry’s assay using the Bio-Rad DC method (catalog number 500–0116) and the proteins were stored at −20°C until further use.
iTRAQ labeling
For each group, 100 μg of enriched glycoproteins were used for iTRAQ labeling. The labeling was carried out essentially as described previously [33]. Denaturation of proteins was carried out by 2% SDS followed by reduction and alkylation with reducing agent and cysteine blocking agents, respectively. Subsequently, the samples were than digested with the modified sequencing grade Trypsin (Promega, Madison, WI, USA) at 37°C overnight. The tryptic peptides from two different sets were labeled using iTRAQ reagents as per manufacturer’s instructions (iTRAQ Reagents Multiplex kit; Applied Biosystems/MDS Sciex, Foster City, CA). We used the 4plex kit for differential labeling; RA and SpA derived tryptic peptides were labeled with 116 and 117, respectively. Labeled peptides were pooled, vacuum-dried and reconstituted in 10 mM KH2PO4, 20% acetonitrile (pH 2.8) and fractionated by strong cation exchange (SCX) chromatography.
SCX- based fractionation
SCX chromatography was carried out essentially as described earlier [73]. Briefly, the tryptic peptides were fractionated on a PolySULFOETHYL A column (PolyLC, Columbia, MD, USA) with 200 Å, 5 μm, 200 × 2.1 mm dimensions, using an Agilent’s 1200 HPLC-system (Agilent Technologies Inc., Santa Clara, USA). A linear gradient of increasing solvent B (350 mM KCl in solvent A, pH 2.8) at a flow rate of 200 μl/min with over a period of 70 min was used for fractionation. Peptide fractions were collected using an automatic fraction collector. Complexity of each fraction was determined based on UV absorbance at 214 nm, finally leading to a total of 18 fractions. The fractions were cleaned using custom made C18 stage-tips (3 M Empore high-performance extraction disks) and were subsequently subjected to LC-MS/MS analysis.
LC-MS/MS analysis
The samples were analyzed on an LTQ-Orbitrap Velos mass spectrometer (Thermo Fisher Scientific Inc., Bremen, Germany) interfaced with Agilent’s 1200 nano-LC system for reverse phase separation of peptides and sample delivery (Agilent Technologies Inc. Santa Clara, USA). Peptides were first enriched on a trap column (75 μm × 2 cm, C18 material 5-10 μm, 100 Å) at a flow rate of 3 μl/min and resolved on a reverse phase analytical column (75 μm × 10 cm, C18 material 5 μm, 120 Å) at a flow rate of 300 nl/min. Peptides were eluted using a linear gradient of 5–30% acetonitrile over 60 min. The electrospray source was fitted with a 5 μm emitter tip (New Objective, Woburn, MA) maintained at 2 kV ion spray voltage. MS data was acquired in a data dependent manner with full scans acquired using the Orbitrap mass analyzer at a mass resolution of 60,000 at 400 m/z and MS/MS scans acquired at a mass resolution of 15,000 at 400 m/z. Twenty most intense precursor ions from a survey scan of each MS cycle, were selected for MS/MS. The fragmentation was carried out using higher-energy collision dissociation (HCD) using 40% normalized collision energy. The fragmented peptides were dynamically excluded for 30 sec. The automatic gain control for full FT-MS was set to 1 million ions and for FT-MS/MS was set to 0.1 million ions with a maximum accumulation time of 200 ms. The lock mass option (m/z, 445.120025) was enabled for accurate mass measurements.
Data analysis
Proteome Discoverer Beta Version 1.3 (Thermo Fisher Scientific Inc., Bremen, Germany) was used for database searches. A precursor mass range of 350–7000 Da and a signal to noise of 1.5 were used. A combined Mascot (Mascot version 2.2, Matrix Science) and SEQUEST search was done using the Proteome Discoverer suite against the NCBI Human RefSeq database 45 containing 32, 964 entries with known contaminants. Search parameters included trypsin as the enzyme with maximum 1 missed cleavage allowed; oxidation of methionine was set as a dynamic modification while alkylation at cysteine and iTRAQ modification at N-terminus of the peptide and lysine were set as static modifications. Precursor and fragment mass tolerance were set to 20 ppm and 0.1.Da, respectively. Peptide and protein data were fetched using high peptide confidence (1% FDR) and rank one peptide match filters. Reporter ion quantitation node was used for relative expression pattern of proteins based on the relative intensities of reporter ions for the corresponding peptides.
Enzyme linked immunosorbant assay (ELISA)
We determined the concentrations of sVCAM-1 in synovial fluid of RA and SpA cases using a commercially available ELISA kit (Invitrogen Corporation, Camarillo, CA, USA). Sandwich ELISA was performed with synovial fluid samples from 16 RA and 16 SpA cases, along with 4 additional samples each from the screening phase (thus, n = 20 in RA and SpA). The protocol implemented was as per the instructions given in the kit. The demographic details of the patients have been provided in the Additional file 5: Table S4. The sensitivity of the kit used was <0.5 ng/ml. Statistical analysis was done with the GraphPad Prism version 5.04 (San Diego California, USA). Statistically significant difference among the diseases was calculated by Mann–Whitney U test of the non-normally distributed data. A p-value of 0.05 or lesser was considered significant.
Bioinformatics analysis
To gain biological insights into the data derived, we carried out a bioinformatics analysis of the protein list. Proteins were classified based on the Gene Ontology (GO)-based molecular class and cellular component features using our in-house resource, Human Reference Protein database, HPRD (http://www.hprd.org/). To determine known glycoproteins in our list, we compared our data with HPRD and the publically available UniProt resource with published literature evidence (http://www.uniprot.org/).
Data availability
We used the two public data repositories for submitting our mass spec data. Raw files are available online and can be downloaded from Tranche (http://www.proteomecommons.org/tranche/) using the following hash: l + KH4WzubdLKlJnNx2NbDTmCC + Q2SL2SFzXHr4mAfghsZbOzYYBVa + VTOjfxnUg136ByJYXv1JDuZd + Kv8dQIGGbOeQAAAAAAAAIwQ== (URL-http://proteomecommons.org/dataset.jsp?i=77886).
Processed data and the search results including the detailed protein/peptide data can be downloaded from our own resource called the Human Proteinpedia (http://www.humanproteinpedia.org) [74].
References
Hadjidakis DJ, Androulakis II: Bone remodeling. Ann NY Acad Sci. 2006, 1092: 385-396. 10.1196/annals.1365.035
Walsh NC, Gravallese EM: Bone remodeling in rheumatic disease: a question of balance. Immunol Rev. 2010, 233: 301-312. 10.1111/j.0105-2896.2009.00857.x
Schett G: Joint remodelling in inflammatory disease. Ann Rheum Dis. 2007, 66 (Suppl 3): iii42-iii44.
Gough AK, Lilley J, Eyre S, Holder RL, Emery P: Generalised bone loss in patients with early rheumatoid arthritis. Lancet. 1994, 344: 23-27. 10.1016/S0140-6736(94)91049-9
Rothschild BM: What is this disease we call spondyloarthropathy?. Clin Exp Rheumatol. 2003, 21: 283-285.
Akdeniz O, Alayli G, Tosun FC, Diren B, Cengiz K, Selcuk MB, Sunter T, Canturk F: Early spondyloarthropathy: scintigraphic, biological, and clinical findings in MRI-positive patients. Clin Rheumatol. 2008, 27: 469-474. 10.1007/s10067-007-0730-y
Baeten D, De Keyser F: The histopathology of spondyloarthropathy. Curr Mol Med. 2004, 4: 1-12.
Mellana WM, Aronow WS, Palaniswamy C, Khera S: Rheumatoid arthritis: cardiovascular manifestations, pathogenesis, and therapy. Curr Pharm Des. 2012, 18: 1450-1456. 10.2174/138161212799504795
Bakland G, Gran JT, Nossent JC: Increased mortality in ankylosing spondylitis is related to disease activity. Ann Rheum Dis. 2011, 70: 1921-1925. 10.1136/ard.2011.151191
Tsybul’ko SV, Baranov AA, Korshunov NI, Kirdianov S, Abaitova NE, Borisova OL: Clinico-immunological aspects of renal lesions in rheumatoid arthritis. Klin Med (Mosk). 2001, 79: 52-57.
Haroon M, Adeeb F, Devlin J, D OG , Walker F: A comparative study of renal dysfunction in patients with inflammatory arthropathies: strong association with cardiovascular diseases and not with anti-rheumatic therapies, inflammatory markers or duration of arthritis. Int J Rheum Dis. 2011, 14: 255-260. 10.1111/j.1756-185X.2011.01594.x
Ruiz-Romero C, Calamia V, Carreira V, Mateos J, Fernandez P, Blanco FJ: Strategies to optimize two-dimensional gel electrophoresis analysis of the human joint proteome. Talanta. 2010, 80: 1552-1560. 10.1016/j.talanta.2009.05.022
Bizzaro N, Mazzanti G, Tonutti E, Villalta D, Tozzoli R: Diagnostic accuracy of the anti-citrulline antibody assay for rheumatoid arthritis. Clin Chem. 2001, 47: 1089-1093.
Novak S: The early diagnosis of spondyloarthritis. Reumatizam. 2011, 58: 47-50.
Firth J: Rheumatoid arthritis: diagnosis and multidisciplinary management. Br J Nurs. 2011, 20: 1179-1180. 1182, 1184–1175,
Venugopal A, Chaerkady R, Pandey A: Application of mass spectrometry-based proteomics for biomarker discovery in neurological disorders. Ann Indian Acad Neurol. 2009, 12: 3-11.
Gronborg M, Bunkenborg J, Kristiansen TZ, Jensen ON, Yeo CJ, Hruban RH, Maitra A, Goggins MG, Pandey A: Comprehensive proteomic analysis of human pancreatic juice. J Proteome Res. 2004, 3: 1042-1055. 10.1021/pr0499085
Good DM, Thongboonkerd V, Novak J, Bascands JL, Schanstra JP, Coon JJ, Dominiczak A, Mischak H: Body fluid proteomics for biomarker discovery: lessons from the past hold the key to success in the future. J Proteome Res. 2007, 6: 4549-4555. 10.1021/pr070529w
White RK: The rheology of synovial fluid. J Bone Joint Surg Am. 1963, 45: 1084-1090.
Levick JR: Microvascular architecture and exchange in synovial joints. Microcirculation. 1995, 2: 217-233. 10.3109/10739689509146768
Smith MD: The normal synovium. Open Rheumatol J. 2011, 5: 100-106. 10.2174/1874312901105010100
Jay GD, Torres JR, Warman ML, Laderer MC, Breuer KS: The role of lubricin in the mechanical behavior of synovial fluid. Proc Natl Acad Sci USA. 2007, 104: 6194-6199. 10.1073/pnas.0608558104
Schurz J, Ribitsch V: Rheology of synovial fluid. Biorheology. 1987, 24: 385-399.
Conrozier T, Mathieu P, Vignon E, Piperno M, Rinaudo M: Differences in the osteoarthritic synovial fluid composition and rheology between patients with or without flare: a pilot study. Clin Exp Rheumatol. 2012, 30: 729-734.
Nettelbladt E, Sundblad L: On the acid glycoproteins of serum and synovial fluid in rheumatoid arthritis. Arthritis Rheum. 1961, 4: 161-168. 10.1002/art.1780040205
Pan S, Chen R, Aebersold R, Brentnall TA: Mass spectrometry based glycoproteomics--from a proteomics perspective. Mol Cell Proteomics. 2011, 10: R110 003251-
Schiess R, Wollscheid B, Aebersold R: Targeted proteomic strategy for clinical biomarker discovery. Mol Oncol. 2009, 3: 33-44. 10.1016/j.molonc.2008.12.001
Kucharz E, Drozdz M, Gburek Z, Olczyk K, Machej M, Rendecka M: Serum glycoproteins and synovial fluid in seropositive and seronegative rheumatoid arthritis. Med Interne. 1984, 22: 253-257.
Kulkarni AV, Engineer JJ, Sequira RD, Borges NE, Joshi VR: Glycoproteins as markers of inflammation in rheumatic disorders. J Postgrad Med. 1986, 32: 89-93.
Zhong J, Kim MS, Chaerkady R, Wu X, Huang TC, Getnet D, Mitchell CJ, Palapetta SM, Sharma J, O’Meally RN: TSLP signaling network revealed by SILAC-based phosphoproteomics. Mol Cell Proteomics. 2012, 11: M112 017764-
Raghothama C, Pandey A: Absolute systems biology–measuring dynamics of protein modifications. Trends Biotechnol. 2003, 21: 467-470. 10.1016/j.tibtech.2003.09.009
Chaerkady R, Thuluvath PJ, Kim MS, Nalli A, Vivekanandan P, Simmers J, Torbenson M, Pandey A: O Labeling for a Quantitative Proteomic Analysis of Glycoproteins in Hepatocellular Carcinoma. Clin Proteomics. 2008, 4: 137-155. 10.1007/s12014-008-9013-0
Polisetty RV, Gautam P, Sharma R, Harsha HC, Nair SC, Gupta MK, Uppin MS, Challa S, Puligopu AK, Ankathi P: LC-MS/MS analysis of differentially expressed glioblastoma membrane proteome reveals altered calcium signaling and other protein groups of regulatory functions. Mol Cell Proteomics. 2012, 11: M111 013565-
Kaur H, Halliwell B: Evidence for nitric oxide-mediated oxidative damage in chronic inflammation. Nitrotyrosine in serum and synovial fluid from rheumatoid patients. FEBS Lett. 1994, 350: 9-12. 10.1016/0014-5793(94)00722-5
Raouf A, Ganss B, McMahon C, Vary C, Roughley PJ, Seth A: Lumican is a major proteoglycan component of the bone matrix. Matrix Biol. 2002, 21: 361-367. 10.1016/S0945-053X(02)00027-6
Onda M, Ishiwata T, Kawahara K, Wang R, Naito Z, Sugisaki Y: Expression of lumican in thickened intima and smooth muscle cells in human coronary atherosclerosis. Exp Mol Pathol. 2002, 72: 142-149. 10.1006/exmp.2002.2425
Mongiat M, Fu J, Oldershaw R, Greenhalgh R, Gown AM, Iozzo RV: Perlecan protein core interacts with extracellular matrix protein 1 (ECM1), a glycoprotein involved in bone formation and angiogenesis. J Biol Chem. 2003, 278: 17491-17499. 10.1074/jbc.M210529200
Botney MD, Kaiser LR, Cooper JD, Mecham RP, Parghi D, Roby J, Parks WC: Extracellular matrix protein gene expression in atherosclerotic hypertensive pulmonary arteries. Am J Pathol. 1992, 140: 357-364.
Chang X, Jian X, Yan X: Expression and citrullination of keratin in synovial tissue of rheumatoid arthritis. Rheumatol Int. 2009, 29: 1337-1342. 10.1007/s00296-009-0863-1
Sunahori K, Yamamura M, Yamana J, Takasugi K, Kawashima M, Yamamoto H, Chazin WJ, Nakatani Y, Yui S, Makino H: The S100A8/A9 heterodimer amplifies proinflammatory cytokine production by macrophages via activation of nuclear factor kappa B and p38 mitogen-activated protein kinase in rheumatoid arthritis. Arthritis Res Ther. 2006, 8: R69- 10.1186/ar1939
Perera C, McNeil HP, Geczy CL: S100 Calgranulins in inflammatory arthritis. Immunol Cell Biol. 2010, 88: 41-49. 10.1038/icb.2009.88
Steenvoorden MM, Toes RE, Ronday HK, Huizinga TW, Degroot J: RAGE activation induces invasiveness of RA fibroblast-like synoviocytes in vitro. Clin Exp Rheumatol. 2007, 25: 740-742.
Moller B, Kessler U, Braner A, Dielehner N, Kaltwasser JP: [Analysis of immunoglobulins and complement factors in synovial fluid and serum in rheumatoid arthritis, seronegative spondyloarthropathies and osteoarthritis: pathophysiology and retrospective analysis of clinical value]. Z Rheumatol. 2002, 61: 48-57. 10.1007/s003930200006
Brinch L, Vinje O, Teisberg P, Mellbye OJ, Aakesson I: The in-vivo metabolism of C3 in ankylosing spondylitis. Ann Rheum Dis. 1982, 41: 86-89. 10.1136/ard.41.1.86
Sheitanov I, Nikolov K, Petrova P: [CH50, C3 and C4 in the serum and synovial fluid of rheumatoid arthritis patients]. Vutr Boles. 1987, 26: 66-70.
Dunkelberger JR, Song WC: Role and mechanism of action of complement in regulating T cell immunity. Mol Immunol. 2010, 47: 2176-2186. 10.1016/j.molimm.2010.05.008
Yasuda T: Hyaluronan inhibits p38 mitogen-activated protein kinase via the receptors in rheumatoid arthritis chondrocytes stimulated with fibronectin fragment. Clin Rheumatol. 2010, 29: 1259-1267. 10.1007/s10067-010-1512-5
Hughes DE, Salter DM, Simpson R: CD44 expression in human bone: a novel marker of osteocytic differentiation. J Bone Miner Res. 1994, 9: 39-44.
Edwards SW, Hughes V, Barlow J, Bucknall R: Immunological detection of myeloperoxidase in synovial fluid from patients with rheumatoid arthritis. Biochem J. 1988, 250: 81-85.
Laursen NS, Magnani F, Gottfredsen RH, Petersen SV, Andersen GR: Structure, function and control of complement C5 and its proteolytic fragments. Curr Mol Med. 2012, 12: 1083-1097. 10.2174/156652412802480925
Kriegsmann J, Keyszer GM, Geiler T, Brauer R, Gay RE, Gay S: Expression of vascular cell adhesion molecule-1 mRNA and protein in rheumatoid synovium demonstrated by in situ hybridization and immunohistochemistry. Lab Invest. 1995, 72: 209-214.
Klimiuk PA, Sierakowski S, Latosiewicz R, Cylwik JP, Cylwik B, Skowronski J, Chwiecko J: Soluble adhesion molecules (ICAM-1, VCAM-1, and E-selectin) and vascular endothelial growth factor (VEGF) in patients with distinct variants of rheumatoid synovitis. Ann Rheum Dis. 2002, 61: 804-809. 10.1136/ard.61.9.804
Navarro-Hernandez RE, Oregon-Romero E, Vazquez-Del Mercado M, Rangel-Villalobos H, Palafox-Sanchez CA, Munoz-Valle JF: Expression of ICAM1 and VCAM1 serum levels in rheumatoid arthritis clinical activity: association with genetic polymorphisms. Dis Markers. 2009, 26: 119-126. 10.1155/2009/510104
Koch AE, Halloran MM, Haskell CJ, Shah MR, Polverini PJ: Angiogenesis mediated by soluble forms of E-selectin and vascular cell adhesion molecule-1. Nature. 1995, 376: 517-519. 10.1038/376517a0
Braun M, Pietsch P, Felix SB, Baumann G: Modulation of intercellular adhesion molecule-1 and vascular cell adhesion molecule-1 on human coronary smooth muscle cells by cytokines. J Mol Cell Cardiol. 1995, 27: 2571-2579. 10.1006/jmcc.1995.0044
Sidibe A, Mannic T, Arboleas M, Subileau M, Gulino-Debrac D, Bouillet L, Jan M, Vandhuick T, Le Loet X, Vittecoq O, Vilgrain I: Soluble VE-cadherin in rheumatoid arthritis patients correlates with disease activity: evidence for tumor necrosis factor alpha-induced VE-cadherin cleavage. Arthritis Rheum. 2012, 64: 77-87. 10.1002/art.33336
Gruber BL, Sorbi D, French DL, Marchese MJ, Nuovo GJ, Kew RR, Arbeit LA: Markedly elevated serum MMP-9 (gelatinase B) levels in rheumatoid arthritis: a potentially useful laboratory marker. Clin Immunol Immunopathol. 1996, 78: 161-171. 10.1006/clin.1996.0025
Chen CH, Lin KC, Yu DT, Yang C, Huang F, Chen HA, Liang TH, Liao HT, Tsai CY, Wei JC, Chou CT: Serum matrix metalloproteinases and tissue inhibitors of metalloproteinases in ankylosing spondylitis: MMP-3 is a reproducibly sensitive and specific biomarker of disease activity. Rheumatology (Oxford). 2006, 45: 414-420. 10.1093/rheumatology/kei208. 10.1093/rheumatology/kei208
Giannelli G, Erriquez R, Iannone F, Marinosci F, Lapadula G, Antonaci S: MMP-2, MMP-9, TIMP-1 and TIMP-2 levels in patients with rheumatoid arthritis and psoriatic arthritis. Clin Exp Rheumatol. 2004, 22: 335-338.
Tzur YB, Wilson KL, Gruenbaum Y: SUN-domain proteins: ‘Velcro’ that links the nucleoskeleton to the cytoskeleton. Nat Rev Mol Cell Biol. 2006, 7: 782-788. 10.1038/nrm2003
Zdrojewski Z: Amyloidosis in rheumatic diseases. Ann Acad Med Stetin. 2010, 56 (1): 7-15.
Lange U, Boss B, Teichmann J, Klor HU, Neeck G: Serum amyloid A–an indicator of inflammation in ankylosing spondylitis. Rheumatol Int. 2000, 19: 119-122. 10.1007/s002960050114
Fischer R, Trudgian DC, Wright C, Thomas G, Bradbury LA, Brown MA, Bowness P, Kessler BM: Discovery of candidate serum proteomic and metabolomic biomarkers in ankylosing spondylitis. Mol Cell Proteomics. 2012, 11: M111 013904-
Prete PE, Gurakar-Osborne A, Kashyap ML: Synovial fluid lipids and apolipoproteins: a contemporary perspective. Biorheology. 1995, 32: 1-16.
Kamper EF, Kopeikina LT, Trontzas P, Kyriazis NC, Vaiopoulos G, Stavridis J: Comparative study of tetranectin levels in serum and synovial fluid of patients with rheumatoid arthritis, seronegative spondylarthritis and osteoarthritis. Clin Rheumatol. 1998, 17: 318-324. 10.1007/BF01451013
Fairney A, Straffen AM, May C, Seifert MH: Vitamin D metabolites in synovial fluid. Ann Rheum Dis. 1987, 46: 370-374. 10.1136/ard.46.5.370
Kawai N, Matsumoto H: Vitamin-D binding protein levels in liver cirrhosis, chronic hepatitis, and rheumatoid arthritis. Nihon Hoigaku Zasshi. 1984, 38: 797-803.
Powe CE, Ricciardi C, Berg AH, Erdenesanaa D, Collerone G, Ankers E, Wenger J, Karumanchi SA, Thadhani R, Bhan I: Vitamin D-binding protein modifies the vitamin D-bone mineral density relationship. J Bone Miner Res. 2011, 26: 1609-1616. 10.1002/jbmr.387
Ohshima S, Kuchen S, Seemayer CA, Kyburz D, Hirt A, Klinzing S, Michel BA, Gay RE, Liu FT, Gay S, Neidhart M: Galectin 3 and its binding protein in rheumatoid arthritis. Arthritis Rheum. 2003, 48: 2788-2795. 10.1002/art.11287
Postigo AA, Garcia-Vicuna R, Diaz-Gonzalez F, Arroyo AG, De Landazuri MO, Chi-Rosso G, Lobb RR, Laffon A, Sanchez-Madrid F: Increased binding of synovial T lymphocytes from rheumatoid arthritis to endothelial-leukocyte adhesion molecule-1 (ELAM-1) and vascular cell adhesion molecule-1 (VCAM-1). J Clin Invest. 1992, 89: 1445-1452. 10.1172/JCI115734
Dessein PH, Joffe BI, Singh S: Biomarkers of endothelial dysfunction, cardiovascular risk factors and atherosclerosis in rheumatoid arthritis. Arthritis Res Ther. 2005, 7: R634-R643. 10.1186/ar1717
Saroha A, Kumar S, Chatterjee BP, Das HR: Jacalin Bound Plasma O-Glycoproteome and Reduced Sialylation of Alpha 2-HS Glycoprotein (A2HSG) in Rheumatoid Arthritis Patients. PLoS One. 2012, 7: e46374- 10.1371/journal.pone.0046374
Barbhuiya MA, Sahasrabuddhe NA, Pinto SM, Muthusamy B, Singh TD, Nanjappa V, Keerthikumar S, Delanghe B, Harsha HC, Chaerkady R: Comprehensive proteomic analysis of human bile. Proteomics. 2011, 11: 4443-4453. 10.1002/pmic.201100197
Mathivanan S, Pandey A: Human Proteinpedia as a resource for clinical proteomics. Mol Cell Proteomics. 2008, 7: 2038-2047. 10.1074/mcp.R800008-MCP200
Acknowledgements
We thank the Department of Biotechnology (DBT), Government of India for research support to the Institute of Bioinformatics, Bangalore. RS is a Research Associate supported by DBT, India. RV is a recipient of the Junior Research Fellowship of University Grants Commission (UGC), India. SR, SMP and NRS are recipients of the Senior Research Fellowship from the Council of Scientific and Industrial Research (CSIR), India. TSKP is supported by a research grant on “Development of Infrastructure and a Computational Framework for Analysis of Proteomic Data” from DBT. HCH is a Wellcome Trust/DBT India Alliance Early Career Fellow.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Competing interests
All the authors have read the manuscript and declare to have no competing interests.
Authors’ contributions
AP, SS, HCH and MB were involved in the conception and study design. MB and LB collected synovial fluid samples. MB, LB, RS, SR, STG and RG carried out the experiments. SMP and NRS were involved in fractionation and mass spectrometry-based data acquisition of the samples. MB, SS and AP wrote the manuscript. MB, SMP, JA and RS were involved in the data analysis and MB carried out data interpretation and statistical analysis. Synovial fluid samples were provided by SS and RJ. RV and MB performed the bioinformatics analysis. BN, TSKP, RJ and HCH critically read and provide input regarding data interpretation and the manuscript. All authors read and approved the final manuscript.
Rakesh Sharma, Renu Goel contributed equally to this work.
Electronic supplementary material
12014_2013_41_MOESM2_ESM.xlsx
Additional file 2: Table S2: Details on sub-cellular localization, functional class and whether or not reported as glycoproteins. (XLSX 23 KB)
12014_2013_41_MOESM3_ESM.eps
Additional file 3: Figure S1: Tandem mass spectra of representative peptides identified for Lumican (A), S100-A8 (B), Complement 5 (C) and Galectin-3 binding protein (D). (EPS 2 MB)
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Bhattacharjee, M., Sharma, R., Goel, R. et al. A multilectin affinity approach for comparative glycoprotein profiling of rheumatoid arthritis and spondyloarthropathy. Clin Proteom 10, 11 (2013). https://doi.org/10.1186/1559-0275-10-11
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1559-0275-10-11