Abstract
Background
Type 1 neurofibromatosis (NF-1) is an autosomal dominant disorder with variable penetrance; approximately 50% of cases present as new mutations
Case report
We report a case of a 56 year-old man with Von Recklinghausen's disease, carcinoma of the ampulla of Vater and incidental benign gastrointestinal stromal tumours of the jejunum.
Conclusions
Coexistence between ampullary carcinoid, ectopic pancreatic tissue in the jejunum and neurofibroma of the jejunum in NF-1 has been previously described however; the association of synchronous carcinoma of the ampulla of Vater and gastrointestinal stromal tumour of the jejunum in NF-1 has not been previously reported.
Similar content being viewed by others
Background
Type 1 neurofibromatosis (NF-1) is an autosomal dominant disorder with variable penetrance; approximately 50% of the cases present as new mutations. The major diagnostic criterion includes multiple cutaneous neurofibromas, axillary or inguinal freckling, café au lait spots, Lisch nodules (pigmented iris hamartomas) and a first-degree family history of NF-1 [1]. The gene for NF-1 has been identified on chromosome 17. NF-1 gene encodes a GTPase activating protein that has the potential to regulate the activity of the p21 product of the ras oncogene and the gene has been suggested to play an important role in controlling cell proliferation and differentiation in a wide range of tissues [2]. Gastrointestinal tract lesions are not uncommon in NF-1, and typically vary from gut neural tissue hyperplasia to gastrointestinal stromal and endocrine cell tumours; there are only rare reports of a miscellaneous group of other malignant neoplasms [3]. Gastrointestinal stromal tumours (GIST) have been histologically identified as neurofibromas, leiomyomas, leiomyosarcomas, schwannomas, autonomic nerve tumours (GANT) and stromal tumours without any definite nerve or muscular differentiation, which have been hypothesised as originating from interstitial cells of Cajal (ICC) [3–6]. Gastrointestinal lesions associated with NF-1, although usually asymptomatic, may present as abdominal pain, dyspepsia, vomiting, anaemia, melaena, haematemesis, haematochezia, intussusception, volvulus, small bowel obstruction, fever and abdominal mass. The case reported by Karatzas et al., [7] mentions the coexistence between ampullary carcinoid, ectopic pancreatic tissue in the jejunum and neurofibroma of the jejunum in NF-1. The association of synchronous carcinoma of the ampulla of Vater and gastrointestinal stromal tumour of the jejunum in NF-1 has not been previously described.
Case Report
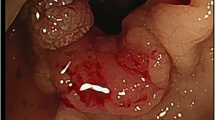
A 56-year-old man presented with history of obstructive jaundice. ERCP done two months earlier at the referring hospital showed a distal bile duct stricture that was stented. Jaundice had initially improved but recurred due to stent occlusion. Skin examination was remarkable for diffuse cutaneous neurofibromas and café au lait spots. CT scan showed a mass lesion in pancreatic head with no evidence of metastatic disease elsewhere. There was no histological/cytological diagnosis before the operation. With a provisional diagnosis of carcinoma head of the pancreas patient underwent laparotomy. At laparotomy, several nodules were seen on the serosal surface of the small bowel of which three yellowish serosal nodules from the jejunum were excised. A pylorus-preserving proximal pancreatic-duodenectomy was performed. Pathological examination of the resected pancreas showed a 33 mm, moderately differentiated invasive adenocarcinoma (Figure 1), arising from a severely dysplastic villous adenoma of the ampulla. Two intra-pancreatic lymph nodes showed metastatic carcinoma with extranodal spread (pT4N1bM0). The three small bowel serosal nodules were less than 5 mm in size and had similar appearances. Microscopically the lesions were composed of bland spindle cells arranged in a storiform pattern set within muscle wall (Figure 2a). No necrosis, mitotic figures or pleomorphism was seen. Tumour cells were positive for CD117 (Figure 2b) and CD34 (Figure 2d) but were negative for S100 protein (Figure 2c), neurofilament, synaptophysin, desmin, smooth muscle actin and calponin. These features were of benign gastrointestinal stromal tumours.
Photomicrograph showing Gastrointestinal stromal tumours a) Bland spindle cells arranged in a storiform pattern set within muscle wall with no necrosis, mitotic figures or pleomorphism seen. (Haematoxylin and Eosin × 100) b) Positive staining with CD 117 (×100) c) Negative staining with S100 (× 100) d) Positive staining with CD34 (× 100)
Postoperative period was uneventful. The patient was offered adjuvant therapy but refused it. Local recurrence was detected at one-year follow-up.
Discussion
Gastrointestinal (GI) involvement in von Recklinghausen's disease occurs in three principal forms i) hyperplasia of the submucosal and myenteric nerve plexuses and mucosal ganglioneuromatosis, which leads to disordered gut motility; ii) gastrointestinal stromal tumours showing varying degrees of neural or smooth muscle differentiation; and iii) a distinctive glandular, somatostatin-rich carcinoid in periampullary region of the duodenum that contains psammoma bodies and may be associated with phaeochromocytoma. NF-1 gene mutations involve GTPase activating protein-coding sequences. Aberrations in other parts of NF1 gene, or in other genes, may also be involved in the development of the varied clinical manifestations.
GISTs are the most common mesenchymal tumours of the gastrointestinal (GI) tract. They are defined as c-kit (CD117, stem cell/ mast cell growth factor receptor)-positive mesenchymal spindle cell, epithelioid or rarely pleomorphic neoplasms arising primarily in the gastrointestinal tract, omentum, and mesentery [8]. A distinctive histological finding, principally in lesions of the small intestine, is presence of scattered eosinophilic bodies that range from 35 to 50 μm in size. These stain with PAS and Masson's trichrome, and are interpreted as skeinoid fibres, the distinctive extracellular collagen globules originally described by Min [9]. Tumours with a high mitotic index (>5 mitoses/10 HPF), measuring more than 5 cms in diameter and extra-gastrointestinal spread are considered malignant [10, 11]. DNA studies show benign tumours to be euploid while the malignant tumours are aneuploid [12]. Intra-abdominal spread or liver metastasis occurs in 10%–30%.
The association of GIST with NF-1, skeinoid fibres and an ultrastructure suggestive of partial neural differentiation, could indicate a mixed neural ICC related phenotype or the possibility of ICC having neural phenotype [4]. GISTs differ clinically and pathogenetically from true leiomyosarcomas (rare in the GI tract) and leiomyomas. The latter occur in the GI tract, predominantly in the oesophagus (intramural tumours) and the colon and rectum (muscularis mucosae tumours). GISTs differ histologically, immunohistochemically and genetically from typical (oesophageal) leiomyomas that are negative for c-kit and CD34 and show neither DNA-loss at 14q, nor c-kit mutations. Schwannomas on the other hand are S100-positive benign spindle cell tumours and usually occur in stomach. GI autonomic nerve tumours (GANTs) are probably a subset of GIST, while angiosarcomas and metastatic melanomas, both of which are often c-kit positive should not be confused with GISTs [13].
Niv Y et al have reported a case of pancreatic cancer, duodenal cancer and liver metastasis in a patient with neurofibromatosis [14]. Though biopsies from all these lesions showed adenocarcinoma, the organ of origin could not be ascertained in their study [14]. Management of synchronous tumours present as a diagnostic and therapeutic dilemma, it is important to accurately distinguish between GIST, carcinoid tumours, and adenocarcinoma as the prognosis of these tumours differs significantly. Small benign tumours are often found incidentally during unrelated surgery or autopsy [15] as in the present case. As the occurrence is rare the optimal management still eludes surgeons.
References
Riccardi VM: Von Recklinghausen neurofibromatosis. N Engl J Med. 1981, 305: 1617-1627.
Martin GA, Viskochil D, Bollag G, McCabe PC, Crosier WJ, Haubruck H, Conroy L, Clark R, O'Connell P, Cawthon RM: The GAP-related domain of the neurofibromatosis type 1 gene product interacts with ras p21. Cell. 1990, 63: 843-890.
Fuller CE, Williams GT: Gastrointestinal manifestations of type 1 neurofibromatosis (von Recklinghausen's disease). Histopathology. 1991, 19: 1-11.
Boldorini R, Tosoni A, Leutner M, Ribaldone R, Surico N, Comello E, Min KW: Multiple small intestinal stromal tumours in a patient with previously unrecognised neurofibromatosis type 1: immunohistochemical and ultrastructural evaluation. Pathology. 2001, 33: 390-395. 10.1080/00313020120063054.
Sircar K, Hewlett BR, Huizinga JD, Chorneyko K, Berezin I, Riddell RH: Interstitial cells of Cajal as precursors of gastrointestinal stromal tumours. Am J Surg Pathol. 1999, 23: 377-389. 10.1097/00000478-199904000-00002.
Hirota S, Koji I, Moriyama Y, Hashimoto K: Gain of function mutations of c-kit in human gastrointestinal stromal tumors. Science. 1998, 279: 577-580. 10.1126/science.279.5350.577.
Karatzas G, Kouraklis G, Karayiannakis A, Patapis P, Givalos N, Kaperonis E: Ampullary carcinoid and jejunal stromal tumour associated with von Recklinghausen's disease presenting as gastrointestinal bleeding and jaundice. Eur J Surg Oncol. 2000, 26: 428-429. 10.1053/ejso.1999.0911.
Miettinen M, Lasota J: Gastrointestinal stromal tumours (GISTs): definition, occurrence, pathology, differential diagnosis and molecular genetics. Pol J Pathol. 2003, 54: 3-24.
Min KW: Small intestinal stromal tumours with skeinoid fibres: clinicopathologic, immunohistochemical, and ultrastructural investigations. Am J Surg Pathol. 1992, 16: 145-155.
Adani GL, Marcello D, Sanna A, Mazzetti J, Anania G, Donini A: Gastrointestinal stromal tumours: evaluation of biological and clinical current opinions. Chir Ital. 2002, 54: 127-131.
Fletcher CD, Berman JJ, Corless C, Gorstein F, Lasota J, Longley BJ, Miettinen M, O'Leary TJ, Remotti H, Rubin BP, Shmookler B, Sobin LH, Weiss SW: Diagnosis of gastrointestinal stromal tumours: a consensus approach. Int J Surg Pathol. 2002, 10: 81-89.
Sapi Z, Kovacs RB, Bodo M: Gastrointestinal stromal tumours. Observations on the basis of 29 cases. Orv Hetil [Hungarian]. 2001, 142: 2479-2485.
Miettinen M, Lasota J: Gastrointestinal stromal tumours – definition, clinical, histological, immunohistochemical, and molecular genetic features and differential diagnosis. Virchows Arch. 2001, 438: 1-12. 10.1007/s004280000338.
Niv Y, Abu-Avid S, Oren M: Adenocarcinoma of pancreas and duodenum associated with cutaneous neurofibromatosis. Am J Med. 1987, 82: 384-385.
Miettinen M, Majidi M, Lasota J: Pathology and diagnostic criteria of gastrointestinal stromal tumours (GISTs): a review. Eur J Cancer. 2002, 38 (Suppl 5): S39-S51.
Author information
Authors and Affiliations
Corresponding author
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Behranwala, K.A., Spalding, D., Wotherspoon, A. et al. Small bowel gastrointestinal stromal tumours and ampullary cancer in Type 1 neurofibromatosis. World J Surg Onc 2, 1 (2004). https://doi.org/10.1186/1477-7819-2-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1477-7819-2-1