Abstract
Background
Adenoid cystic cancer arising in the salivary glands has distinctive features such as perineural invasion, distant metastasis, and a variable prognosis. In salivary gland cancer, c-kit, EGFR, and VEGF are representative molecular markers that may predict remnant and recurrent tumors. In this study, the expression of c-kit, EGFR, and VEGF in adenoid cystic cancer was evaluated, and the relationships between the expression of these markers and the clinical findings were investigated.
Methods
The medical records of 48 patients who were treated for parotid adenoid cystic cancer from January 1990 to January 2006 were reviewed. The tumor location, size, histological subtypes, perineural invasion, the resected margin status, and lymph node metastasis were assessed. Immunohistochemical staining and semiquantitative analysis of c-kit, EGFR and VEGF were performed. The relationship between the expression of each marker and the clinicopathological factors were analyzed.
Results
Positive c-kit immunostaining was present in 45 patients (94%), with weak positivity (+1) in 23, moderate positivity (+2) in 19 and strong positivity (+3) in three. Positive EGFR immunostaining was observed in 27 (56%), with weak positivity (+1) in 19 and moderate positivity (+2) in eight with no strong positive staining. Positive VEGF immunostaining was present in 42 patients (88%) with weak positivity (+1) in 12, moderate positivity (+2) in 17, and strong positivity (+3) in 13. Only the expression of VEGF was significantly higher in parotid gland tumors than in any other gland (P = 0.032). Marginal involvement was associated with strong VEGF expression (P = 0.02). No marker was significantly correlated with recurrence or the survival rate. Lymph node status was related to the survival rate.
Conclusions
The expression of c-kit, EGRF, and VEGF had no predictive value for recurrence or the prognosis of adenoid cystic cancer. Only the lymph node status was related to the prognosis.
Similar content being viewed by others
Background
Adenoid cystic carcinoma is a relatively rare tumor in the parotid gland with a 10% incidence, compared with a 30% incidence in the minor salivary glands. Histologically, this tumor shows higher rates of local growth, perineural invasion and distant metastasis. Many cases of delayed recurrence after definite treatment have been reported, indicating the difficulty of treating and controlling this tumor. Factors related to the recurrence and prognosis of adenoid cystic carcinoma include tumor stage, histological classification, status of the resected tumor margin, lymph node metastasis, and perineural invasion [1–3]. Investigations of the molecular markers of this tumor and the development of targeted therapy are currently ongoing. Ki-67, p53, bcl-2, epidermal growth factor receptor (EGFR), human epidermal growth receptor-2 (HER2), proliferating cell nuclear antigen (PCNA), and Runt-related transcription factor-3 (RNUX3) are representative markers of adenoid cystic carcinoma [4–6]. The inhibition of vascular endothelial growth factor (VEGF) has also been reported to reduce local recurrence and distant metastasis [7].
The c-kit protein is a transmembrane receptor with a tyrosine kinase function. The overexpression of c-kit has been reported in various malignant tumors [8, 9], including adenoid cystic carcinoma and some salivary gland tumors [10, 11]. However, there is little information on the prognostic value of c-kit, and the therapeutic efficacy of a tyrosine kinase inhibitor (imatinib) is not well established [12]. EGFR is a transmembrane receptor found in epithelial cancers such as breast, lung, bladder, ovary, prostate, and head and neck cancers [3, 13]. The overexpression of EGFR in head and neck cancer is associated with an advanced stage, lymph node metastasis, low survival rate, and poor response to radiation therapy [14, 15]. Although many studies on the role of EGFR in salivary gland tumors have been reported, there is some debate about its prognostic significance [16]. VEGF is a major vascular formative factor in the process of epithelial carcinogenesis and tumor metastasis. It selectively functions in the vascular endothelial tissue and is expressed in various organs such as lung, breast and gastrointestinal organs [17]. The overexpression of VEGF is involved in perineural invasion and recurrence, and it heralds a poor survival rate [18]. In an animal study, the inhibition of VEGF expression reduced growth and distant metastasis of adenoid cystic cancer [19]. Clinical trials with a single inhibitor (imatinib for c-kit; trastuzumab or cetuximab for ErbB1 and ErbB2) have shown low response rates in salivary gland cancer [20]. Intriguingly, concomitant inhibition of EGF and VEGF reduced the growth and metastasis of adenoid cystic carcinoma in an animal model [19]. EGFR overexpression and the absence of c-kit expression are negative prognostic factors in adenoid cystic cancer [21]. Based on these reports, we hypothesized that the elucidation of the diverse changes in these proteins would improve treatment outcomes. In the present study, we evaluated the relationship between c-kit, EGFR, and VEGF expression and the survival or local control rate of adenoid cystic carcinoma.
Methods
Patients and treatment
This retrospective study using medical chart reviews was performed after approved by the institutional review board of Asan Medical Center. Written informed consent was obtained from the patients for publication of this report and any accompanying images. We reviewed the medical records of 48 patients who were diagnosed with and treated for salivary adenoid cystic carcinoma from January 1990 to January 2006 at a single institute. The presence of lymph node metastasis was preoperatively evaluated by neck ultrasonography (US), computed tomography (CT), and magnetic resonance imaging (MRI). Tumor locations were divided into the submandibular, parotid, and minor salivary glands. Distant metastasis was identified with Tc99m bone scanning and F18-flurodeoxyglucose positron emission tomography (F18-FDG PET). We investigated tumor size, the histological pattern, the presence of perineural invasion, invasion of surgical margins, and lymph node metastasis according to the pathology reports. The histological patterns were classified as tubular, cribriform, and solid types on the basis of the WHO classification (2005). Marginal involvement included microscopic and macroscopic invasion of the margin of the specimen. When lymph node metastasis was confirmed on preoperative fine needle aspiration cytology with or without US, therapeutic neck dissection from level I to V was performed. Selective neck dissection, including levels I to III, was performed in cases of clinical T3, T4 or suspicious findings on radiology. Lymph node metastasis was defined when confirmed histologically after surgery. A close resection margin (<<1 cm from the tumor), an unclear margin, a perineural invasion, and an advanced stage (III, IV) were indications for adjuvant radiation therapy. We also checked for local recurrence, distant metastasis, and survival after treatment [22, 23]. The observation period was defined from the end point of treatment to the most recent follow-up date.
Tissue microarray blocks
Two tissue microarray blocks were made from the formalin-fixed, paraffin-embedded tissue of the 48 patients with adenoid cystic carcinoma. Each slide was reviewed under a microscope, and representative areas were selected for immunohistochemistry. These were marked on the slides stained with hematoxylin and eosin, and their corresponding areas on each block were punched using a tissue cylinder with a 0.6 mm diameter. These cores were transferred to the recipient blocks using a tissue-arraying instrument (Beecher Instruments, Silver Spring, MD, USA). Considering the heterogeneity of the tumor, the samples were arrayed in duplicate to avoid tissue loss.
Immunohistochemistry
Immunohistochemical staining for c-kit, EGFR, and VEGF was performed using a Benchmark automatic immunostaining device (Ventana Medical Systems, Tucson, AZ, USA). Tissue sections (4 μm thick) were deparaffinized in 10% xylene, dehydrated in 100%, 95%, and 75% ethanol solutions, and washed with distilled water. For antigen retrieval, the sections were immersed in 10 mM citrate buffer (pH 6.0) and microwaved for 10 min. Endogenous peroxidases activities and nonspecific antigens were eliminated with 3% hydrogen peroxide in methanol and AB blocker (Roche, Basel, Switzerland). The sections were incubated with primary antibodies against c-kit (CD117, 1:400 dilution; DAKO, Glostrup, Denmark), EGFR (1:500 dilution; DAKO), and VEGF (1:100 dilution; Zymed, South San Francisco, CA, USA). Immunodetection was performed with biotinylated anti-mouse immunoglobulin followed by peroxidase-labeled streptavidin, using a labeled streptavidin-biotin kit (DAKO). As a chromogen, 3,3’-diaminobenzidine was used, and the sections were counterstained with Harris hematoxylin. The intensity of the immunohistochemical staining of c-kit (membranous/cytoplasmic), EGFR (membranous), and VEGF (cytoplasmic) was semiquantitatively scored as 0 (reactivity in <5% of the tumor cells), 1+ (reactivity 5% - 1/3 of the tumor cells), 2+ (reactivity in 1/3 to 2/3 of the tumor cells), or 3+ (reactivity >2/3 of the tumor cells). Cases with scores of 2+ and 3+ were regarded as positive.
Statistical analysis
SPSS software (version 14.0; SPSS Inc., Chicago, IL, USA) was used for the statistical analysis. To identify relationships between clinical factors and immunostaining of markers, Fisher’s exact test was used for categorical data and the Mann–Whitney U test was used for continuous variables. Univariate and multivariate analyses using Cox’s proportional hazard model were performed with a backward, stepwise elimination approach. At each step, the least significant factor with P >0.10 was eliminated, and each remaining factor in the model was reassessed. The limit for including factors was set at 20%. To simplify binary logistic regression analyses, we divided the data into two groups based on immunoreactivity. The Kaplan-Meier method was used to analyze survival rates. Values of P below 0.05 indicated statistical significance.
Results
Study population
Forty-eight patients (19 males and 29 females) with adenoid cystic cancer in the salivary gland were enrolled. The average patient age was 49.7 years (± 21.9). The numbers of tumors that involved the submandibular gland, parotid gland, or minor salivary gland were 12 (25%), 18 (38%), and 18 (38%), respectively. The average tumor size was 2.6 cm (± 2.2). Twenty-seven cases were classified into three groups (tubular, two cases (4%); cribriform, 18 cases (38%); solid, seven cases (15%)) according to the histology, and 21 cases (44%) had no records or had unclear tumor types. Perineural invasion and cervical lymph node metastasis were identified in 22 (56%) and six (13%) cases, respectively. Twelve patients underwent PET, and the average standard uptake value in the primary lesion was 3.0 (± 2.1). Ten patients (21%) underwent only surgical management, while 32 (67%) received adjuvant radiation therapy after surgery. Concurrent chemoradiation therapy following surgery was administered in six cases (14%) (Table 1).
Immunohistological staining
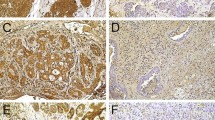
Forty-five cases (94%) showed c-kit immunoreactivity, with 23 weakly positive, 19 moderately positive, and three strongly positive cases. For EGFR, 27 cases (56%) were positive, comprising 19 weakly positive and eight moderately positive cases; no strongly positive cases were observed. Forty-two cases (88%) showed positive immunoreactivity for VEGF: 12 were weakly positive, 17 were moderately positive, and 13 were strongly positive (Figure 1). The patients were divided into two groups, a negative or weakly positive group and a more-than-moderately positive group, according to the staining intensity for c-kit and VEGF. For EGFR, patients were divided into negative and positive groups. There was no significant correlation between the staining intensity for each marker (c-kit and EGFR, P = 0.422; EGFR and VEGF, P = 0.499; VEGF and c-kit, P = 0.454). VEGF showed stronger expression in the parotid gland (P = 0.032) than in the other sites, and marginal invasion was frequent in cases with high VEGF expression (P = 0.02). The other makers showed no notable trends (Table 2).
Immunohistochemical staining of adenoid cystic carcinomas of the salivary gland. C-kit (CD 117) expression of weakly (1+, A), moderately (2+, B), and strongly positive (3+, C) cases; EGFR (epidermal growth factor receptor) expression of weakly (D) and moderately positive (E) cases; VEGF (vascular endothelial growth factor) expression of weakly (F), moderately (G), and strongly positive (H) cases. Expressions of c-kit (membranous/cytoplasmic), EGFR (membranous), and VEGF (cytoplasmic) were scored as follows: 0, reactivity in <5% of tumor cells; 1+, reactivity in 5% -1/3 of tumor cells; 2+, reactivity in 1/3 to 2/3 of tumor cells; 3+, reactivity >2/3 of tumor cells.
Recurrence after treatment
The mean follow-up period was 70.9 months (range, 4.0 to 159.1 months). There were 19 patients (39.6%) with recurrence, and the average time until detection of recurrence was 24.9 months (range, 2.0 to 97.6 months). Four cases showed local recurrence, 10 showed distant metastasis (lung, nine cases; multiple, one case), and five showed both local and distant metastasis. Lymph node metastasis was closely related to recurrence after the initial treatment (P <0.001). However, recurrence was not associated with the staining intensity of c-kit (P = 0.987), EGFR (P = 0.747), or VEGF (P = 0.927) (Table 3).
Survival rate
Eleven patients died of the disease, and the mean survival period was 38.0 months (range, 4.4 to 144.2 months). The five-year survival rate was 88.2%, and the complete remission rate was 72.9%. No marker staining intensity was associated with a difference in survival rate based on the Kaplan-Meier survival curve, whereas lymph node metastasis was significantly related to survival rate (Figure 2). Using Cox’s proportional hazard model, we analyzed the factors that might have influenced the survival rate, and only lymph node metastasis showed a close relationship to the survival rate (P = 0.049). The expression of c-kit (P = 0.864), EGFR (P = 0.716), and VEGF (P = 0.198) did not show a close relationship with the survival rate (Table 4).
Discussion
The low response rate of adenoid cystic cancer to tyrosine kinase inhibitors and EGFR inhibitors indicates that no single molecule is dominant in tumor invasion and spread of this cancer [19–21, 24]. The class III receptor tyrosine kinase and c-kit is important for normal hematopoiesis, melanin production and reproductive cell production. Imatinib mesylate (Gleevec™), a tyrosine kinase inhibitor, is very effective in treating chronic myeloid leukemia and show good efficacy for the treatment of advanced gastrointestinal tumors with positive c-kit expression [24]. The expression of c-kit in salivary adenoid cystic cancer has been variably reported as 78% to 100%. The high c-kit expression in adenoid cystic cancer suggests that this cancer may respond to treatment with imatinib mesylate, although studies with imatinib have not shown consistent results [12, 25]. The relationship between c-kit expression and prognosis has been controversial, although the expression of c-kit was stronger in the tubular or cribriform type than in the solid type [21, 26]. The discrepancy might have been caused by differences in staining techniques and the lack of a standard method for evaluating staining intensity. In the present investigation, 94% of the tumors expressed c-kit, but no significant relationship with other clinical variables or prognosis was identified.
EGF is found in the primary duct and terminal buds, and its distribution and density decrease with aging [27]. EGFR is present in salivary gland tumors, with expression reported in 0% to 85% of adenoid cystic cancers [27]. In the present study, 56% of the tumors were positive for EGFR. The overexpression of EGFR is reportedly related to a poor prognosis in salivary gland cancer [21], which is different from our results. VEGF promotes vascular proliferation in tumors from peripheral tissue and enhances vessel permeability with a selective effect on vascular endothelial cells. VEGF expression is found in various tumors, such as those of esophageal cancer, small cell lung cancer, thyroid cancer, breast cancer, and cervical cancer [28], as well as head and neck cancer. VEGF expression is associated with cervical lymph node metastasis, higher cancer stage, perineural invasion, recurrence, and low survival [18, 28]. Higher VEGF expression was found in solid tumors compared with tubular or cribriform types, and the survival rate decreased with higher VEGF expression [29]. In the present study, there was no relationship between high VEGF expression and lymph node metastasis, recurrence, or survival, contrary to our expectations. This was possibly, attributable to the subjective assessment of the differences in immunostaining and the semiquantitative analysis. A few investigations on treatments targeting VEGF in salivary gland cancer have shown partial remission, suggesting the targeting of VEGF for the management of adenoid cystic cancer [30]. Negative results regarding the prognostic usefulness of molecular markers in the present study might have been due to the threshold criteria used for positive EGFR, c-kit, and VEGF on immunoreactivity [21]. The availability of normal tissue as a negative control would have helped in scoring positive immunochemical staining.
Histological differentiation in adenoid cystic cancer is variable and reflects its malignant potential [31]. Indeterminate cases comprised 44% of all cases in the present study, and most of these were mixed type with no predominant type. This result was attributable to a lack of detailed pathologic reports on subtypes, which is a limitation of the present retrospective study. In addition, tumor size and involved sites were not recorded definitively enough to be analyzed. Lymph node metastasis alone was significantly associated with the prognosis. Previous studies have reported that perineural invasion had strong relationships to distant metastasis and the survival rate [32, 33]. These relationships were not significant in the present investigation because of the small number of cases. In earlier studies, cervical lymph node metastasis was present in 20% of adenoid cystic cancers and was related to a high recurrence rate and low survival rate [34, 35]. A similar pattern of metastasis was observed in the present study. Distant metastasis was observed in 10 cases, with the lung being the most frequently involved single site (n = 9). Multiple sites (lung, bone, and brain) were involved in one case.
Recurrence of adenoid cystic cancer has been found usually within 56 months. Death occurred within three years after the detection of distant metastasis in 54%, whereas survival in excess of 10 years was recorded in 10% of the patients [36, 37]. Considering that late recurrence is characteristic of adenoid cystic cancer, the analysis of recurrence during a short follow-up period is another limitation of the present study.
Lymph node metastasis is a key step in the development of metastasis and is a determining factor of prognosis. Traditionally, it has been thought that tumors spread to lymph nodes by direct extension in an orderly, defined manner based on mechanical considerations and transverse lymphatics [38]. However, lymph node metastasis cannot explain local recurrence, distant metastasis, or poor treatment outcomes. Based on clinical and laboratory research, Fisher has proposed that biological, rather than anatomical, factors may be responsible for the appearance of metastasis in certain nodes and the lack of metastasis in others, suggesting that cancer is not a local disease, but a systemic disease [39]. Oligometastasis implies a critical interaction between systemically disseminated cancer cells and the host; this concept leads to the notion that confined distant metastasis could be completely cured by local therapy in some cases [40]. Based on these ideas, we believe that lymph node metastasis is both a key step and coincident finding. Thus, an analysis of markers specific for lymph node metastasis may be useful for stratifying prognosis.
Anticancer radiation therapy for head and neck cancer can reduce local recurrence, but not distant metastasis [23, 41]. The molecular markers used in the present study are related to the prognosis of other head and neck malignancies, including salivary gland tumors. Although we did not identify the prognostic significance of these molecular markers, immunohistochemical staining revealed high expression levels of c-kit, EGFR and VEGF in the present study. These findings indicate a need for further research on these markers in adenoid cystic cancer.
Conclusions
Lymph node metastasis was the only factor that was related to recurrence and survival rate following treatment of salivary adenoid cystic cancer. Despite the high expression levels of c-kit, EGFR, and VEGF, these markers were not significantly correlated with recurrence and the prognosis of adenoid cystic cancer. However, the expression levels of c-kit, EGFR, and VEGF exhibited variable changes, suggesting that interrelationships among these proteins may provide approaches for molecularly targeted therapy for salivary adenoid cystic cancer.
References
Chen AM, Bucci MK, Weinberg V, Garcia J, Quivey JM, Schechter NR, Phillips TL, Fu KK, Eisele DW: Adenoid cystic carcinoma of the head and neck treated by surgery with or without postoperative radiation therapy: prognostic features of recurrence. Int J Radiat Oncol Biol Phys. 2006, 66: 152-159. 10.1016/j.ijrobp.2006.04.014.
Garden AS, Weber RS, Morrison WH, Ang KK, Peters LJ: The influence of positive margins and nerve invasion in adenoid cystic carcinoma of the head and neck treated with surgery and radiation. Int J Radiat Oncol Biol Phys. 1995, 32: 619-626. 10.1016/0360-3016(95)00122-F.
Mendenhall WM, Morris CG, Amdur RJ, Werning JW, Hinerman RW, Villaret DB: Radiotherapy alone or combined with surgery for adenoid cystic carcinoma of the head and neck. Head Neck. 2004, 26: 154-162. 10.1002/hed.10380.
Dodd RL, Slevin NJ: Salivary gland adenoid cystic carcinoma: a review of chemotherapy and molecular therapies. Oral Oncol. 2006, 42: 759-769. 10.1016/j.oraloncology.2006.01.001.
Elkin AD, Jacobs CD: Tamoxifen for salivary gland adenoid cystic carcinoma: report of two cases. J Cancer Res Clin Oncol. 2008, 134: 1151-1153. 10.1007/s00432-008-0377-3.
He JF, Ge MH, Zhu X, Chen C, Tan Z, Li YN, Gu ZY: Expression of RUNX3 in salivary adenoid cystic carcinoma: implications for tumor progression and prognosis. Cancer Sci. 2008, 99: 1334-1340. 10.1111/j.1349-7006.2008.00826.x.
Zhang J, Peng B, Chen X: Expressions of nuclear factor kappaB, inducible nitric oxide synthase, and vascular endothelial growth factor in adenoid cystic carcinoma of salivary glands: correlations with the angiogenesis and clinical outcome. Clin Cancer Res. 2005, 11: 7334-7343. 10.1158/1078-0432.CCR-05-0241.
DiPaola RS, Kuczynski WI, Onodera K, Ratajczak MZ, Hijiya N, Moore J, Gewirtz AM: Evidence for a functional kit receptor in melanoma, breast, and lung carcinoma cells. Cancer gene therapy. 1997, 4: 176-182.
Hirota S, Isozaki K, Moriyama Y, Hashimoto K, Nishida T, Ishiguro S, Kawano K, Hanada M, Kurata A, Takeda M, Muhammad Tunio G, Matsuzawa Y, Kanakura Y, Shinomura Y, Kitamura Y: Gain-of-function mutations of c-kit in human gastrointestinal stromal tumors. Science. 1998, 279: 577-580. 10.1126/science.279.5350.577.
Jeng YM, Lin CY, Hsu HC: Expression of the c-kit protein is associated with certain subtypes of salivary gland carcinoma. Cancer Lett. 2000, 154: 107-111. 10.1016/S0304-3835(00)00387-6.
Locati LD, Perrone F, Losa M, Mela M, Casieri P, Orsenigo M, Cortelazzi B, Negri T, Tamborini E, Quattrone P, Bossi P, Rinaldi G, Bergamini C, Calderone RG, Liberatoscioli C, Licitra L: Treatment relevant target immunophenotyping of 139 salivary gland carcinomas (SGCs). Oral Oncol. 2009, 45: 986-990. 10.1016/j.oraloncology.2009.05.635.
Hotte SJ, Winquist EW, Lamont E, MacKenzie M, Vokes E, Chen EX, Brown S, Pond GR, Murgo A, Siu LL: Imatinib mesylate in patients with adenoid cystic cancers of the salivary glands expressing c-kit: a Princess Margaret Hospital phase II consortium study. J Clin Oncol. 2005, 23: 585-590.
Dassonville O, Formento JL, Francoual M, Ramaioli A, Santini J, Schneider M, Demard F, Milano G: Expression of epidermal growth factor receptor and survival in upper aerodigestive tract cancer. J Clin Oncol. 1993, 11: 1873-1878.
Gupta AK, McKenna WG, Weber CN, Feldman MD, Goldsmith JD, Mick R, Machtay M, Rosenthal DI, Bakanauskas VJ, Cerniglia GJ, Bernhard EJ, Weber RS, Muschel RJ: Local recurrence in head and neck cancer: relationship to radiation resistance and signal transduction. Clin Cancer Res. 2002, 8: 885-892.
Xia W, Lau YK, Zhang HZ, Xiao FY, Johnston DA, Liu AR, Li L, Katz RL, Hung MC: Combination of EGFR, HER-2/neu, and HER-3 is a stronger predictor for the outcome of oral squamous cell carcinoma than any individual family members. Clin Cancer Res. 1999, 5: 4164-4174.
Sorensen KB, Godballe C, de Stricker K, Krogdahl A: Parotid carcinoma: expression of kit protein and epidermal growth factor receptor. J Oral Pathol Med. 2006, 35: 286-291. 10.1111/j.1600-0714.2006.00421.x.
Dvorak HF, Brown LF, Detmar M, Dvorak AM: Vascular permeability factor/vascular endothelial growth factor, microvascular hyperpermeability, and angiogenesis. Am J Pathol. 1995, 146: 1029-1039.
Lim JJ, Kang S, Lee MR, Pai HK, Yoon HJ, Lee JI, Hong SP, Lim CY: Expression of vascular endothelial growth factor in salivary gland carcinomas and its relation to p53, Ki-67 and prognosis. J Oral Pathol Med. 2003, 32: 552-561.
Younes MN, Park YW, Yazici YD, Gu M, Santillan AA, Nong X, Kim S, Jasser SA, El-Naggar AK, Myers JN: Concomitant inhibition of epidermal growth factor and vascular endothelial growth factor receptor tyrosine kinases reduces growth and metastasis of human salivary adenoid cystic carcinoma in an orthotopic nude mouse model. Mol Cancer Ther. 2006, 5: 2696-2705. 10.1158/1535-7163.MCT-05-0228.
Milano A, Longo F, Basile M, Iaffaioli RV, Caponigro F: Recent advances in the treatment of salivary gland cancers: emphasis on molecular targeted therapy. Oral Oncol. 2007, 43: 729-734. 10.1016/j.oraloncology.2006.12.012.
Ettl T, Schwarz S, Kleinsasser N, Hartmann A, Reichert TE, Driemel O: Overexpression of EGFR and absence of C-KIT expression correlate with poor prognosis in salivary gland carcinomas. Histopathology. 2008, 53: 567-577. 10.1111/j.1365-2559.2008.03159.x.
Beckhardt RN, Weber RS, Zane R, Garden AS, Wolf P, Carrillo R, Luna MA: Minor salivary gland tumors of the palate: clinical and pathologic correlates of outcome. Laryngoscope. 1995, 105: 1155-1160. 10.1288/00005537-199511000-00003.
Spiro RH: Management of malignant tumors of the salivary glands. Oncology (Williston Park). 1998, 12: 671-680. discussion 683
Blanke CD, Rankin C, Demetri GD, Ryan CW, von Mehren M, Benjamin RS, Raymond AK, Bramwell VH, Baker LH, Maki RG, Tanaka M, Hecht JR, Heinrich MC, Fletcher CD, Crowley JJ, Borden EC: Phase III randomized, intergroup trial assessing imatinib mesylate at two dose levels in patients with unresectable or metastatic gastrointestinal stromal tumors expressing the kit receptor tyrosine kinase: S0033. J Clin Oncol. 2008, 26: 626-632. 10.1200/JCO.2007.13.4452.
Alcedo JC, Fabrega JM, Arosemena JR, Urrutia A: Imatinib mesylate as treatment for adenoid cystic carcinoma of the salivary glands: report of two successfully treated cases. Head Neck. 2004, 26: 829-831. 10.1002/hed.20094.
Freier K, Flechtenmacher C, Walch A, Devens F, Muhling J, Lichter P, Joos S, Hofele C: Differential KIT expression in histological subtypes of adenoid cystic carcinoma (ACC) of the salivary gland. Oral Oncol. 2005, 41: 934-939. 10.1016/j.oraloncology.2005.05.005.
Tsukitani K, Tatemoto Y, Noda Y, Mori M, Hayashi T, Kato K: Immunohistochemical detection of human epidermal growth factor in submandibular glands and their tumors using a polyclonal antiserum and a monoclonal antibody. Histochemistry. 1987, 87: 293-300. 10.1007/BF00492581.
Warburton G, Nikitakis NG, Roberson P, Marinos NJ, Wu T, Sauk JJ: Jr, Ord RA, Wahl SM: Histopathological and lymphangiogenic parameters in relation to lymph node metastasis in early stage oral squamous cell carcinoma. J Oral Maxillofac Surg. 2007, 65: 475-484. 10.1016/j.joms.2005.12.074.
Zhang H, Su SW, Zheng Y, Wang L, Ma XD: Expression of nuclear factor-kappa B mRNA, inducible nitric oxide synthase and interleukin-6 in nasal polyp and its role. Zhonghua Er Bi Yan Hou Ke Za Zhi. 2003, 38: 455-458.
Rugo HS, Herbst RS, Liu G, Park JW, Kies MS, Steinfeldt HM, Pithavala YK, Reich SD, Freddo JL, Wilding G: Phase I trial of the oral antiangiogenesis agent AG-013736 in patients with advanced solid tumors: pharmacokinetic and clinical results. J Clin Oncol. 2005, 23: 5474-5483. 10.1200/JCO.2005.04.192.
Kokemueller H, Eckardt A, Brachvogel P, Hausamen JE: Adenoid cystic carcinoma of the head and neck-a 20 years experience. Int J Oral Maxillofac Surg. 2004, 33: 25-31. 10.1054/ijom.2003.0448.
Agarwal JP, Jain S, Gupta T, Tiwari M, Laskar SG, Dinshaw KA, Chaturvedi P, D’Cruz AK, Shrivastava SK: Intraoral adenoid cystic carcinoma: prognostic factors and outcome. Oral Oncol. 2008, 44: 986-993. 10.1016/j.oraloncology.2008.01.004.
Rapidis AD, Givalos N, Gakiopoulou H, Faratzis G, Stavrianos SD, Vilos GA, Douzinas EE, Patsouris E: Adenoid cystic carcinoma of the head and neck. Clinicopathological analysis of 23 patients and review of the literature. Oral Oncol. 2005, 41: 328-335. 10.1016/j.oraloncology.2004.12.004.
Le QT, Birdwell S, Terris DJ, Gabalski EC, Varghese A, Fee W, Goffinet DR: Postoperative irradiation of minor salivary gland malignancies of the head and neck. Radiother Oncol. 1999, 52: 165-171. 10.1016/S0167-8140(99)00084-5.
Spiro RH, Huvos AG: Stage means more than grade in adenoid cystic carcinoma. Am J Surg. 1992, 164: 623-628. 10.1016/S0002-9610(05)80721-4.
Li Q, Zhang XR, Liu XK, Liu ZM, Liu WW, Li H, Guo ZM: Long-term treatment outcome of minor salivary gland carcinoma of the hard palate. Oral Oncol. 2012, 48: 456-62. 10.1016/j.oraloncology.2011.12.005.
Spiro RH: Distant metastasis in adenoid cystic carcinoma of salivary origin. Am J Surg. 1997, 174: 495-498. 10.1016/S0002-9610(97)00153-0.
Halsted WS: The results of radical operations for the cure of carcinoma of the breast. Ann Surg. 1907, 46: 1-19. 10.1097/00000658-190707000-00001.
Fisher B: Biological research in the evolution of cancer surgery: a personal perspective. Cancer Res. 2008, 68: 10007-10020. 10.1158/0008-5472.CAN-08-0186.
Weichselbaum RR, Hellman S: Oligometastases revisited. Nature Rev Clin Oncol. 2011, 8: 378-382.
Ballonoff A, Raben D, Rusthoven KE, Bassetti M, Kane M, Song JI, Chen C: Outcomes of patients with n3 neck nodes treated with chemoradiation. Laryngoscope. 2008, 118: 995-998. 10.1097/MLG.0b013e31816a7120.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
All authors have no competing interests.
Authors’ contributions
SKL, MSK, and SYN participated in the design of the study, carried out the extraction and analysis of data, and wrote the manuscript. KJC reviewed pathology of the enrolled slides. YSL and SYN performed the critical review of the literature. KJC and SYK assisted in the collection of the clinical data and in reviewing the manuscript. SYN assisted in reviewing the manuscript. All authors have read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Lee, S.K., Kwon, M.S., Lee, Y.S. et al. Prognostic value of expression of molecular markers in adenoid cystic cancer of the salivary glands compared with lymph node metastasis: a retrospective study. World J Surg Onc 10, 266 (2012). https://doi.org/10.1186/1477-7819-10-266
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1477-7819-10-266