Abstract
Objectives
To assess satisfaction of survivors of coronary artery diseases (CAD) with healthcare services and to determine whether specific components of standard health-related quality of life (HRQL) assessment tools might identify areas of satisfaction and dissatisfaction.
Method
A specific tool developed to provide a comprehensive assessment of healthcare needs was administered concomitantly with generic and specific HRQL instruments, on 242 patients with CAD, admitted to an acute coronary unit during a single year.
Results
92.5% of patients confirmed their trust in and satisfaction with the care given by their General Practitioner; even so, one third experienced difficulty getting an appointment and a quarter wanted more time for each consultation or prompt referral to a specialist when needed. Around a third expressed dissatisfaction with advice from the practice nurse or hospital consultant. Overall 54% were highly satisfied with services, 33% moderately satisfied and 13% dissatisfied.
Cronbach's alpha was 0.87; the corrected total-item correlation ranged between 0.55–0.75, with trivial 'floor' score and low 'ceiling' effect. Several domains in all three HRQL tools correlated with items relating to satisfaction. The Seattle Angina Questionnaire Treatment Score correlated significantly with all satisfaction items and with the global satisfaction score.
Conclusion
Cardiac patients' demanded better services and advice from, and more time with, health professionals and easier surgery access. The satisfaction tool showed acceptable psychometric properties. In this patient group, disease-specific HRQL tools seem more appropriate than generic tools for surveys of patient satisfaction.
Similar content being viewed by others
Introduction
The modern approach to healthcare seeks to engage the attention of both patients and public in developing healthcare services and equity of access, but this is not easy to achieve, requiring time, commitment, political support and cultural change to overcome barriers to change. [1] Improvement in selected aspects of health care delivery through quality assurance and outcome assessment has been driven by political expediency. While this is important, a 'bottom up' assessment of patient satisfaction seems preferable if service improvement is to be translated into improved quality of life. [2, 3]
Patients' satisfaction is related to the extent to which general health care needs and condition-specific needs are met. Evaluating to what extent patients are satisfied with health services is clinically relevant, as satisfied patients are more likely to comply with treatment [4, 5] and take an active role in their own care. [6] In addition, health professionals may benefit from satisfaction surveys that identify potential areas for service improvement and health expenditure may be optimised through patient-guided planning and evaluation. [7]
Critics draw attention to the lack of a standard approach to measuring satisfaction and of comparative studies [3] and so the significance of the results of surveys is often ignored. There is less controversy with respect to clinical outcome measures, as health-related quality of life (HRQL) is not only widely regarded as a robust measure of outcome but also is extensively used in several clinical areas. [8, 9]
We conducted a cross-sectional survey to establish, from a patient perspective, how satisfied survivors of coronary artery diseases (CAD) were with healthcare services. This might indicate areas that warranted review, evaluation and change where appropriate.
We also wanted to determine whether specific components of standard health-related quality of life (HRQL) assessment tools might identify areas of satisfaction and dissatisfaction. Identifying variables that link patient satisfaction and accepted measures of outcome might result in identifying areas for quality improvement.
Method
The health care needs of all patients with coronary artery disease (CAD) admitted to an coronary unit during a single year were established. Their consent to participate in the study was obtained. Diagnosis was based on clinical and angiographic features according to the Nottingham Heart Attack Register (NHAR), which categorised patients in five diagnostic groups: definite myocardial infarction, suspected MI, ischaemic heart disease, chest pain and symptoms not related to heart disease. [10, 11] Patients were sent a detailed questionnaire three to six months after discharge from hospital.
The methodology has been described in detail elsewhere, [12] but briefly a needs assessment questionnaire was developed following a rigorous review of expert opinion and the literature, discussions with medical staff and information compiled during face-to-face interviews with patients with CAD. After a pilot study, [13] a healthcare needs assessment (HNA) tool emerged, consisting of 48 questions in 5-score Likert scale (1 indicates more needs versus 5 with no needs) in five domains of 'physical needs, 'satisfaction', 'informational needs', 'social needs, and 'concerns'. Two generic (Short Form-12 and EuroQuol-5D) quality of life questionnaires were chosen to cover the limitations of each tools.; in addition one specific HRQL instrument (Seattle Angina Questionnaire) was administered concomitantly. The satisfaction component, which was included in the main health needs questionnaire, consisted of 11 questions mainly related to hospital-based services and health centres or family doctor surgeries (table 2). A global score in each domain was calculated to permit comparison with other variables. We compared satisfaction data with health-related quality of life information obtained from the same patients, which could be assumed as a 'gold standard'.
Seattle Angina Questionnaire (SAQ)
This has well-established psychometric properties, measures broader aspects of the effects of coronary disease than other disease-specific tools and can detect physical limitations due to coronary disease. It is particularly useful in the presence of co-morbidity, [14] corresponding well with the Canadian Cardiovascular Society Classification. [15] It consists of 19 items grouped in five components: physical functioning (SAQ Phys), angina stability (AS), angina frequency (AF), treatment satisfaction (TS), and QOL perception (SAQ QOL).
Short Form 12 (SF-12)
This is an abridged form of the better-known Short Form 36 (SF-36) [16] which has produced consistent results in several European countries and in a diverse range of conditions. It contains 12 questions from which are derived physical and mental component scores (PCS & MCS); these are as precise as the SF-36 [17, 18].
EuroQoL (EQ-5D)
The EuroQol questionnaire defines health in terms of five dimensions: mobility, self-care, usual activities, pain or discomfort, and anxiety or depression in a three degree format that is no problem, moderate and severe. The greater the score, the worse the quality of life. Another question deals with overall health in a 0–100 scaling format. The validity and reliability of the EQ-5D questionnaire have been tested in a range of patient groups. [19, 20] There is a strong correlation between the EQ-5D and the SF-12 in adults,[21] but to our knowledge, there has been no published study of the EQ-5D in myocardial infarction.
Statistical analysis
SPSS version 11.0 was used for statistical purposes, using descriptive and correlation analysis, comparison of means, reliability and non-parametric (Mann Whitney-U) tests where indicated. Contingency tables were formed to look for any correlation and chi-square test was used to measure the association between variables. Psychometric analysis demonstrated acceptable properties, described elsewhere [12]; internal consistency in the five domains was quite high, ranging from 0.83 to 0.89 and specifically 0.87 in satisfaction domain. The corrected total-item correlation, as an indicator of item specificity, ranged between 0.55–0.75, with a trivial floor score of 0.4% and a ceiling effect of 8.7%. To compare satisfaction variables with HRQL and other HNA scores, correlation coefficients were computed, which was considered significant at p < 0.05. The regional ethical committee approved this survey.
Results
Demographic data
242 patients (59% male) returned the completed questionnaires; response rate was 93%. Ages ranged between 31–93 years (mean = 69.7, 95% CI: 68.2,71.2). Seventy-one percent (=169) left school at age 16 or less and 21% (=53) completed higher education. Table 1 describes the major demographic characteristics of all but 3 patients. Social class, derived from the last occupation, was determined in 223 patients. [22] 69 (31%) had non-manual and 154 (69%) manual jobs (table 1). Health-related quality of life were generally lower in women, especially in SAQ-AS and PCS (t = -2.04 and t = -1.99 respectively, P < 0.05) and in several domains of the three QOL tools in those over 65 years of age. [12]
Health needs
Elderly affected physical (p < 0.01) and social needs (p < 0.05) and women were more dissatisfied in general (p < 0.05). Lower social class was concomitant with more needs in all health needs domains (p < 0.01) although not statistically significant in satisfaction score. A unique score was calculated in each domain to facilitate comparisons among various variables. The mean score (mean 4, SD 0.76) was highly skewed towards higher level of satisfaction (measure of skewness: -4.53). [23]
Patients' satisfaction
Assessment of satisfaction was obtained from 11 scores contained within several HNA domains (table 2) dealing mainly with patients' perceptions of members of the health professions and the information and treatment provided. Scores less than 3 were categorised as 'poor' and a score of 4 or higher as 'reasonable' satisfaction with health services.
One-third reported difficulty getting an appointment with their GPs. About one-fourth were dissatisfied with the amount of time devoted to each visit and with their ability to see a consultant when needed. One-third expressed dissatisfaction with advice received from their GP, although more than 92% believed that theGP provided a good quality service (table 2).
Women (P < 0.05) and younger patients (<75) were more likely to be dissatisfied with their ability to get to see their GP (P = 0.01) or happy with their relationship with their GP (p < 0.05). 18 patients (8%) used the private sector as their main health provider; there were no significant differences in levels of satisfaction among those utilising public rather than private healthcare services. Patients who reported that they often had to ask for a home visit (12%; n = 28) also reported lower levels of satisfaction with the appointment process compared with patients who were able enough to get to the Health Centre (p < 0.05). 57% (n = 138) were quite confident that their GPs fully appreciated their health needs, but the remainder doubted their needs were appropriately recognised. Women in particular expected their GP to fully understand their needs (p = 0.001).
Mean satisfaction score
Overall women were less satisfied with healthcare services (P < 0.05), as were the under 75 s (mean rank 114.25 v 124.52), but this was not statistically significant. Social class did not appear to influence satisfaction.
Patients with co-morbid illness were significantly less satisfied than those suffering from coronary disease alone (P < 0.01). Mean satisfaction score was highly correlated with other HNA components (correlation coefficient ranged 0.26–0.70, p < 0.001). Comparison of score means indicated that patients with other physical, informational, social needs and medical concerns were more dissatisfied (p < 0.01). Overall, components of the HNA tool were indicative of overall levels of satisfaction with healthcare.
HRQL scores
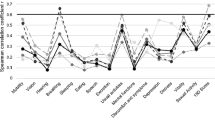
The SAQ-TS correlated significantly with all satisfaction items, while several domains in all three HRQL tools correlated with satisfaction scores (tables 3,4). Satisfied patients valued their health status higher in visual analogue score by 9 scores; that was 56 in dissatisfied versus 65 in satisfied patients (P < 0.001). Mean satisfaction score correlated moderately with EQ anxiety/depression (r = 0.40–0.59) and SAQ treatment satisfaction domains and correlated weakly with SF-12 domains, EQ self care and visual analogue scale and SAQ-QOL (r = 0.20–0.39). The remaining HRQL domains did not correlate with the mean satisfaction score.
Discussion
Patient satisfaction is considered by some to be of dubious benefit in facilitating the process of clinical care, as patients have no specific clinical expertise and are readily influenced by non-medical factors; in addition, there are few reports on the reliability of satisfaction surveys [3, 24, 25]. Nevertheless, satisfied patients are more likely to comply with medical treatment and therefore ought to have a better outcome. [3]
In the absence of an available instrument for assessing our patients' healthcare needs, we developed a healthcare needs assessment questionnaire. This included a series of questions relating to some aspect of satisfaction with clinical care. While its internal consistency (and therefore its reliability) was satisfactory, further studies are warranted to investigate as Guldvog suggests [6] whether it will retain its reliability over time and its validity when compared with other related tools. Health needs and satisfaction with clinical care are related to some extent-meeting other health needs increases the likelihood of overall satisfaction with healthcare services generally.
Patients did think highly of their General Practitioners (more so than other members of the medical and nursing staff) and were generally satisfied with the care they delivered. This confirms the General Practitioner's central role in delivering healthcare to cardiac patients and highlights the importance that patients place on the availability of first line health provision. Nevertheless, from a patient perspective, four main areas were identified where clinical care might be improved.
Patients wanted first an appointment system to improve the accessibility of the family doctor. Optimal medication is no guarantee that intermittent exacerbation of symptoms of coronary heart disease will be prevented and cardiac patients recognise that they require easy and prompt access to their principal primary carer, the GP. Second, patients have issues regarding immediate and future treatment they wish to discuss and expect more time for each consultation. Third, dissatisfied patients have greater need for information which is consonant with other results. [26] Fourth, according to our routine clinical experience, patients read in the media about many of the technical aspects of modern cardiological practice available in secondary care and expect referral to hospital for a specialist opinion. These study findings provide a snapshot of areas where patients consider services might be improved quite easily. Qualitative and quantitative studies are planned to investigate these further and to determine how satisfaction surveys can be introduced into routine clinical practice.
Our results are consistent with previous reports in terms of the probability of dissatisfaction with healthcare services among younger patients [3] but contradict findings of even greater dissatisfaction among female patients [27]. Gender differences in HRQL perception have been reported before, [28, 29] which implies that measuring satisfaction in our study involved more than simply questioning patients about healthcare facilities. [27]
We had considered that readily available HRQL tools might be of value as surrogates for more detailed surveys of patient satisfaction. In our patients with coronary disease, satisfaction with the care process was closely correlated with some aspects of health-related quality of life, more so with the disease-specific than the generic tool-existing generic instruments are of limited application in the assessment of satisfaction with treatment.
There is at least a theoretical association between satisfaction and quality of life [3] and our study did find that the global satisfaction score showed moderate convergence with the treatment satisfaction domain in the SAQ. Even so, the association between satisfaction and health-related quality of life is not straightforward. An inverse relationship cannot be ruled out [3], nor can a causal relationship. In patients with mental disorders, the relationship may be direct [30] or inverse. [6]
Patient satisfaction is dependent upon a variety of personal, cultural, social, socio-economic and health-related factors, set against a background of previous exposure to, and experience of, health care services. Many of these may not be readily amenable to change, but where deficiencies are identified, such as in this study, alterations in services might well be rewarded with more satisfied patients.
References
DoH: Patient and public involvement in the new NHS. Department of Health 1999.
Ware J. E., Jr., Davies-Avery A, Stewart AL: The measurement and meaning of patient satisfaction. Health Med Care Serv Rev 1978, 1: 1, 3–15.
Aharony L, Strasser S: Patient satisfaction: what we know about and what we still need to explore. Med Care Rev 1993, 50: 49–79.
Von Essen L, Larsson G, Oberg K, Sjoden PO: 'Satisfaction with care': associations with health-related quality of life and psychosocial function among Swedish patients with endocrine gastrointestinal tumours. Eur J Cancer Care (Engl) 2002, 11: 91–99. 10.1046/j.1365-2354.2002.00293.x
Fitzpatrick R: Scope and measurement of patient satisfaction. Measurement of Patients' Satisfaction with Their Care (Edited by: Fitzpatrick R and Hopkins A). London, Royal College of Physicans of London 1993, 1–17.
Guldvog B: Can patient satisfaction improve health among patients with angina pectoris? Int J Qual Health Care 1999, 11: 233–240. 10.1093/intqhc/11.3.233
Donabedian A: The quality of care. How can it be assessed? Jama 1988, 260: 1743–1748. 10.1001/jama.260.12.1743
Oldridge N, Gottlieb M, Guyatt G, Jones N, Streiner D, Feeny D: Predictors of health-related quality of life with cardiac rehabilitation after acute myocardial infarction. J Cardiopulm Rehabil 1998, 18: 95–103. 10.1097/00008483-199803000-00002
Thompson DR, Meadows KA, Lewin RJ: Measuring quality of life in patients with coronary heart disease. Eur Heart J 1998, 19: 693–695.
Gray D, Hampton JR: Twenty years' experience of myocardial infarction: the value of a heart attack register. Br J Clin Pract 1993, 47: 292–295.
Gray D, Keating NA, Murdock J, Skene AM, Hampton JR: Impact of hospital thrombolysis policy on out-of-hospital response to suspected myocardial infarction. Lancet 1993, 341: 654–657. 10.1016/0140-6736(93)90420-L
Asadi-Lari M, Packham C, Gray D: Unmet health needs in patients with coronary heart disease: implications and potential for improvement in caring services. Health Qual Life Outcomes 2003, 1: 26. 10.1186/1477-7525-1-26
Asadi-Lari M, Gray D: Is quality of life measurement likely to be a proxy for health needs assessment in patients with coronary artery disease? Health Qual Life Outcomes 2003, 1: 50. 10.1186/1477-7525-1-50
Spertus JA, Winder JA, Dewhurst TA, Deyo RA, Fihn SD: Monitoring the quality of life in patients with coronary artery disease. Am J Cardiol 1994, 74: 1240–1244.
Dougherty CM, Dewhurst T, Nichol WP, Spertus J: Comparison of three quality of life instruments in stable angina pectoris: Seattle Angina Questionnaire, Short Form Health Survey (SF-36), and Quality of Life Index-Cardiac Version III. J Clin Epidemiol 1998, 51: 569–575. 10.1016/S0895-4356(98)00028-6
Brazier JE, Harper R, Jones NM, O'Cathain A, Thomas KJ, Usherwood T, Westlake L: Validating the SF-36 health survey questionnaire: new outcome measure for primary care. Bmj 1992, 305: 160–164.
Melville M, Asadi-Lari M, Brown N, Young T, Hampton JR, Gray D: Quality of life assessment using the SF-12 is as reliable and sensitive as the SF-36 in distinguishing symptom severity in myocardial infarction survivors. Heart 2003, 89: 1445–1446. 10.1136/heart.89.12.1445
Jenkinson C, Layte R, Jenkinson D, Lawrence K, Petersen S, Paice C, Stradling J: A shorter form health survey: can the SF-12 replicate results from the SF-36 in longitudinal studies? J Public Health Med 1997, 19: 179–186.
Kind P, Dolan P, Gudex C, Williams A: Variations in population health status: results from a United Kingdom national questionnaire survey. Bmj 1998, 316: 736–741.
van Agt HM, Essink-Bot ML, Krabbe PF, Bonsel GJ: Test-retest reliability of health state valuations collected with the EuroQol questionnaire. Soc Sci Med 1994, 39: 1537–1544. 10.1016/0277-9536(94)90005-1
Johnson JA, Coons SJ: Comparison of the EQ-5D and SF-12 in an adult US sample. Qual Life Res 1998, 7: 155–166. 10.1023/A:1008809610703
Standard occupational classification /Office for National Statistics. London, Stationery Office 2000.
Munro HB: Statistical methods for health care research. 4th Edition Philadelphia, Lippincott Williams & Wilkins 2001.
Nabati L, Shea N, McBride L, Gavin C, Bauer MS: Adaptation of a simple patient satisfaction instrument to mental health: psychometric properties. Psychiatry Res 1998, 77: 51–56. 10.1016/S0165-1781(97)00122-4
Bredart A, Razavi D, Robertson C, Batel-Copel L, Larsson G, Lichosik D, Meyza J, Schraub S, von Essen L, de Haes JC: A comprehensive assessment of satisfaction with care: preliminary psychometric analysis in French, Polish, Swedish and Italian oncology patients. Patient Educ Couns 2001, 43: 243–252. 10.1016/S0738-3991(00)00165-8
Larson CO, Nelson EC, Gustafson D, Batalden PB: The relationship between meeting patients' information needs and their satisfaction with hospital care and general health status outcomes. Int J Qual Health Care 1996, 8: 447–456. 10.1016/S1353-4505(96)00050-6
Pascoe GC: Patient satisfaction in primary health care: a literature review and analysis. Eval Program Plann 1983, 6: 185–210. 10.1016/0149-7189(83)90002-2
Chin MH, Goldman L: Gender differences in 1-year survival and quality of life among patients admitted with congestive heart failure. Med Care 1998, 36: 1033–1046. 10.1097/00005650-199807000-00010
Riedinger MS, Dracup KA, Brecht ML, Padilla G, Sarna L, Ganz PA: Quality of life in patients with heart failure: do gender differences exist? Heart Lung 2001, 30: 105–116. 10.1067/mhl.2001.114140
Wiersma D, van Busschbach J: Are needs and satisfaction of care associated with quality of life? An epidemiological survey among the severely mentally ill in the Netherlands. Eur Arch Psychiatry Clin Neurosci 2001, 251: 239–246. 10.1007/s004060170033
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Asadi-Lari, M., Packham, C. & Gray, D. Patients' satisfaction and quality of life in coronary artery disease. Health Qual Life Outcomes 1, 57 (2003). https://doi.org/10.1186/1477-7525-1-57
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1477-7525-1-57