Abstract
Background
Clinical, surgical, and percutaneous strategies similarly prevent major cardiovascular events in patients with stable coronary artery disease (CAD). The possibility that these strategies have differential effects on health-related quality of life (HRQoL) has been debated, particularly in patients treated outside clinical trials.
Methods
We assigned 454 patients diagnosed with CAD during an elective diagnostic coronary angiography to coronary artery bypass grafting (CABG), percutaneous coronary intervention (PCI), or optimal medical treatment (OMT), and followed them for an average of 5.2 ± 1.5 years. HRQoL was assessed using a validated Brazilian version of the 12-Item Short-Form Health Survey questionnaire. The association between therapeutic strategies and quality of life scores was tested using variance analysis and adjusted for confounders in a general linear model.
Results
There were no differences in the mental component summary scores in the follow-up evaluation by therapeutic strategies: 51.4, 53.7, and 52.3 for OMT, PCI, and CABG, respectively. Physical component summary scores were higher in the PCI group than the CABG and OMT groups (46.4 vs. 42.9 and 43.8, respectively); however, these differences were no longer different after adjustment for confounding variables.
Conclusion
In a long-term follow-up of patients with stable CAD, HRQoL did not differ in patients treated by medical, percutaneous, or surgical treatments.
Similar content being viewed by others
Background
Coronary artery disease (CAD) is expected to persist as a primary cause of death worldwide until at least 2030 [1]. Clinical, surgical, and percutaneous strategies have demonstrated effectiveness in relieving clinical manifestations and preventing recurrence and fatalities, particularly in acute events [2]. The identification of the best therapeutic strategy in patients with stable CAD, however, remains controversial.
Randomized controlled trials [3, 4] and their meta-analyses [5, 6] demonstrated no evidence of the superiority of interventional treatments over clinical treatment to prevent major cardiovascular (CV) events in patients with stable CAD. The ISCHEMIA and ISCHEMIA-CKD Trials reported that in patients with stable CAD and moderate or severe ischemia, an invasive strategy (coronary artery bypass grafting [CABG] or percutaneous coronary intervention [PCI]), compared with a conservative strategy (optimal medical therapy [OMT] only) did not reduce the incidence of CV events or death after a follow-up of approximately 3 years [7, 8].
However, most clinical trials evaluating strategies for management of chronic CAD compared patients submitted to CABG and percutaneous coronary intervention (PCI), but not medical treatment. Overall, these trials demonstrated no significant difference in mortality or myocardial infarction incidence in patients treated with either of the invasive options. However, surgical patients had lower rates of new revascularization procedures during follow-up [9,10,11].
On the other hand, observational studies comparing CABG with PCI suggested that the former can be more effective in preventing major CV events [12,13,14]. However, in studies that included patients treated clinically, the incidence of CV events was not substantially different from patients treated by CABG or PCI, as we demonstrated in a cohort study [15].
Independent of the effectiveness of therapies to prevent major CV outcomes, it is critical to determine whether patients treated with different strategies have better outcomes concerning the frequency of symptoms and quality of life (QoL). The COURAGE Trial [3] and the ISCHEMIA Trial [16] addressed these issues. These trials demonstrated a better health-related quality of life (HRQoL) in patients treated with invasive strategies than conservative strategies with OMT only. In comparing the effects of invasive strategies, CABG may have a more durable benefit over HRQoL than PCI, as demonstrated in a sub-analysis of the SYNTAX Trial [17].
Observational studies with all comers could offer insights regarding the effect of therapies on HRQoL. There are a few observational studies comparing the effect of various treatment strategies in participants subjected to OMT, CABG, or PCI [18,19,20,21]. These studies had small sample sizes, high rates of loss to follow-up [18, 19], short follow-up [18, 21], used different scales for the assessment of HRQoL and were not adjusted for confounders [19,20,21]. A meta-analysis identified these and 30 other observational studies assessing the effect of different treatments over HRQoL [22]. Six studies compared HRQoL in patients treated with PCI or CABG [18,19,20,21, 23, 24], and the others reported the effect of individual therapies over HRQoL (after treatment of all participants). A systematic review did not precede this meta-analysis [22], and compared findings of different study arms without the methods recommended for network meta-analysis, separating arbitrarily for analysis studies with and without outliers. Herein, we report a comparison of QoL measurements in a cohort of patients with stable CAD treated with medical, percutaneous, or surgical strategies.
Methods
Details of the study protocol were described previously [15]. In summary, patients were referred by cardiologists and clinicians for elective diagnostic coronary angiography to a university-affiliated tertiary referral hospital from 2006 to 2014. All patients with a documented diagnosis of CAD were included irrespective of the type of treatment (OMT, PCI, or CABG). The SYNTAX score (SXscore) was calculated prospectively in all patients. Two interventional cardiologists, blinded to clinical characteristics and trained according to the SXscore tutorial, performed the visual angiographic analysis and calculated the scores. In case of disagreement, a third interventionist was consulted, and the final decision was reached by consensus. The option of the therapeutic strategy was chosen by the attending physician and, in more complex cases, after a discussion with a CV surgeon and an interventional cardiologist. We excluded patients with acute coronary syndromes, valvular heart disease, aortic diseases, previous coronary revascularization, class III or IV heart failure, chronic renal disease (previous medical diagnosis or serum creatinine greater than 1.5 mg/dL), history of cancer, or severe psychiatric illness.
A standardized questionnaire was provided immediately before the coronary angiography. This was considered the baseline interview, and it evaluated demographic information, educational history, lifestyle characteristics, and past medical history.
The follow-up of patients was performed through telephone interviews, medical records review, death certificates, and next-of-kin interviews. A combination of strategies was adopted to minimize losses, including contacting patients by registered letters and interviewing the attending physicians.
The outcome in this analysis was HRQoL, assessed using a validated Brazilian version of the 12-Item Short-Form Health Survey (SF-12) questionnaire [25], which uses 12 questions to assess the influence of eight health domains to score physical and mental health dimensions in the four weeks before the interview. The physical health-related domain investigated general health, physical functioning, physical role, and body pain. The mental health-related scales included vitality, social functioning, emotional role, and mental health. We also calculated physical component summary (PCS) and mental component summary (MCS) scores [26,27,28].
All data were evaluated by at least two authors independently, with quality control on data entry, and checking amplitude and consistency of the variables. For quality control of the team’s performance, 20% of the protocols were randomly selected to be reviewed by a senior investigator (SCF). The reporting was based on Strengthening the Reporting of Observational Studies in Epidemiology guidelines [29].
Statistical analysis
Results are expressed as mean ± standard deviation and number (percentage) for continuous and categorical variables, respectively. As appropriate, continuous and dichotomous variables were analyzed using the Student’s t test, one-way analysis of variance (ANOVA), or chi-square test. When necessary, the Bonferroni test was applied to identify differences in multiple comparisons. The association between therapeutic strategies and scores of HRQoL were tested by ANOVA and adjusted for confounding using a general linear model. Variables included in the model were theoretically associated with worse clinical outcomes in patients with coronary heart disease and, therefore, with the potential to confound the association of the interventions with scores of HRQoL. Statistical analyses were performed using SPSS, Version 18.0 (SPSS, Inc., Chicago, IL, USA).
Ethical aspects
The hospital's ethics committee approved the study protocol. The Office for Human Research Protections accredited the committee as an institutional review board, registered under no. 13–0171. All participants provided informed written consent.
Results
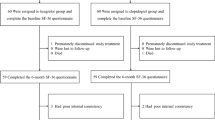
Among 1028 patients referred for elective diagnostic coronary angiography at our institution during the study period, 454 had a confirmed diagnosis of CAD and were treated by clinical, surgical, or percutaneous interventions. A total of 402 patients (88.5%) completed the HRQoL questionnaire with an average follow-up of 5.2 ± 1.5 years and were included in the analysis. Of these, 112 received OMT alone, 224 underwent PCI, and 66 underwent CABG; (Fig. 1). Participants were an average of 60.8 years old, and most were men (n = 258; 64%). The follow-up time by treatment was 5.1 ± 1.4 years for patients treated clinically (ranging 2.5–8.3 years), 5.3 ± 1.5 (ranging 2.5–8.4) years for patients treated with PCI, and 4.7 ± 1.4 (ranging 2.4–7.4) years for patients treated with CABG.
Table 1 shows that the characteristics of the study population were relatively similar across treatment groups. Differences that should be highlighted were the higher prevalence of women in the OMT group than the PCI and CABG groups (46.4% vs. 31.2% and 33.3%, respectively). Participants who reported a previous myocardial infarction more often underwent interventional treatment (60.6% and 48.7% vs. 31.3%, for CABG, PCI, and OMT alone, respectively). Patients treated with CABG had higher SXscores than the PCI and OMT alone groups (20.5, 9.3, and 6.6, respectively).
The unadjusted mean values of PCS and MCS scores according to treatment strategy are shown in Table 2. There was no difference in MCS among the three groups, with mean MCS for OMT alone, PCI, and CABG of 51.4, 53.7, and 52.3, respectively. PCS scores in patients treated by OMT alone, PCI, and CABG were shown in Fig. 2, and the score was significantly higher in the PCI group than the CABG or OMT groups. The statistically significant differences shown in Table 2 were no longer significant after adjusting for confounding factors (Table 3).
Discussion
In this cohort study of patients with stable CAD treated clinically or by invasive strategies, we found that all treatment options had similar effects on HRQoL after an average follow-up of 5.2 ± 1.5 years. The trend toward better HRQoL in patients treated through PCI was no longer significant after adjustment for the baseline severity of disease and other confounders.
HRQoL is a multidimensional concept that is subjectively perceived and embraces physical, social, emotional, and functional health [30]. Traditional outcomes of randomized controlled trials and cohort studies may not capture the impact of the intervention on HRQoL. Therefore, HRQoL assessment has become increasingly important in managing patients with CAD, a chronic disease that classically impairs functional capacity and HRQoL [19, 31]. Patients often consider the quality of the additional life-years gained as important as the length of life [32].
The COURAGE Trial was one of the first studies conducted in patients with stable CAD that evaluated HRQoL changes according to treatment strategies (PCI vs. OMT alone). In that trial, the initial improvement in HRQoL in patients treated with PCI was no longer detected after 12 months [3]. The benefit of invasive strategies over OMT in terms of HRQoL was reported in another study [33]. In another report, patients undergoing revascularization by CABG had more prolonged improvement in HRQoL than patients treated with PCI [34]. The effect of treatments over angina-related health status, assessed using the Seattle Angina Questionnaire (SAQ) and HRQoL, assessed by European Quality of Life–5 Dimensions in ISCHEMIA Trial, was an a priori sub-analysis specified by the protocol. Participants treated with CABG or PCI had higher SAQ summary scores than patients treated clinically during a follow-up of 36 months [16]. HRQoL, however, improved similarly during the period [16]. The loss of beneficial effects of invasive approaches over HRQoL with longer follow-up in the COURAGE and ISCHEMIA trials suggest that the short-term effects may be at least in part explained by a placebo effect. Our findings also suggest that any eventual benefit of PCI and CABG at short-term follow-up in the real-world care of patients also vanishes with longer follow-up.
Our findings are hardly comparable to the observational studies that assessed the effect of OMT, PCI, or CABG. In addition to the limitations of a few studies that compared the three strategies in contemporary cohorts [18,19,20,21], they included short follow-up. To the best of our knowledge, there is only one recent systematic review with meta-analysis addressing this topic [22]; however, non-adherence to the core methods of meta-analyses threatens its internal validity.
Our study has limitations that deserve mention. We did not assess the HRQoL at baseline, and this fact might introduce bias in the assessment of HRQoL at follow-up. Nonetheless, the underlying reasons for differences in HRQoL at the baseline were controlled in the multivariate analysis. Limited statistical power due to the sample size may have concealed a beta error. The study was carried out in only one center, which may reduce its external validity. Nevertheless, our service's patient characteristics and diagnostic and therapeutic practices do not differ substantially from those of other centers. The strengths of our study are that we studied all comers without limitations for participation in clinical trials, we compared three treatment strategies, and there was a prolonged follow-up.
Conclusion
The HRQoL of patients with stable CAD does not differ after treatment with CABG, PCI, or OMT alone after a relatively long follow-up period. Considering that these strategies have similar effectiveness in preventing major CV outcomes, the option for OMT alone appears to be adequate as the first option for the management of patients with stable CAD.
Availability of data and materials
All data relevant for this work are available to the community upon reasonable request to the corresponding author.
Abbreviations
- CABG:
-
Coronary artery bypass grafting
- CAD:
-
Coronary artery disease
- CV:
-
Cardiovascular
- EQ-5D:
-
European Quality of Life–5 Dimensions
- HRQoL:
-
Health-related quality of life
- MCS:
-
Mental Component Summary
- OMT:
-
Optimized medical therapy
- PCI:
-
Percutaneous coronary intervention
- PCS:
-
Physical component summary
- SAQ:
-
Seattle Angina Questionnaire
- SD:
-
Standard deviation
- SF-12:
-
12-Item Short-Form Health Survey
- STROBE:
-
Strengthening the Reporting of Observational Studies in Epidemiology
- SXscores:
-
Syntax Scores
References
Ayatollahi H, Gholamhosseini L, Salehi M. Predicting coronary artery disease: a comparison between two data mining algorithms. BMC Public Health. 2019;19(1):448.
Bagai A, Dangas GD, Stone GW, Granger CB. Reperfusion strategies in acute coronary syndromes. Circ Res. 2014;114(12):1918–28.
Boden WE, O'Rourke RA, Teo KK, Hartigan PM, Maron DJ, Kostuk WJ, et al. COURAGE Trial Research Group. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med. 2007;356(15):1503–16.
BARI 2D Study Group, Frye RL, August P, Brooks MM, Hardison RM, Kelsey SF, MacGregor JM, et al. A randomized trial of therapies for type 2 diabetes and coronary artery disease. N Engl J Med. 2009;360(24):2503–15.
Katritsis DG, Ioannidis JP. Percutaneous coronary intervention versus conservative therapy in nonacute coronary artery disease: a meta-analysis. Circulation. 2005;111(22):2906–12.
Stergiopoulos K, Boden WE, Hartigan P, Möbius-Winkler S, Hambrecht R, Hueb W, et al. Percutaneous coronary intervention outcomes in patients with stable obstructive coronary artery disease and myocardial ischemia. A collaborative meta-analysis of contemporary randomized clinical trials. JAMA Intern Med. 2014;174(2):232–40.
Maron DJ, Hochman JS, Reynolds HR, Bangalore S, O'Brien SM, Boden WE, et al. ISCHEMIA Research Group. Initial invasive or conservative strategy for stable coronary disease. N Engl J Med. 2020;382(15):1395–407.
Bangalore S, Maron DJ, O'Brien SM, Fleg JL, Kretov EI, Briguori C, et al. ISCHEMIA-CKD Research Group. Management of coronary disease in patients with advanced kidney disease. N Engl J Med. 2020;382(17):1608–18.
Hamm CW, Reimers J, Ischinger T, Rupprecht HJ, Berger J, Bleifeld W. For the German angioplasty bypass surgery investigation. A randomized study of coronary angioplasty compared with bypass surgery in patients with symptomatic multivessel coronary disease. N Engl J Med. 1994;331(16):1037–43.
The Bypass Angioplasty Revascularization Investigation (BARI) Investigators. Comparison of coronary bypass surgery with angioplasty in patients with multivessel disease. N Engl J Med. 1996;335(4):217–25.
Serruys PW, Unger F, Sousa JE, Jatene A, Bonnier HJ, Schönberger JP, et al. Comparison of coronary-artery bypass surgery and stenting for the treatment of multivessel disease. N Engl J Med. 2001;344(15):1117–24.
Fortuna D, Nicolini F, Guastaroba P, De Palma R, Di Bartolomeo S, Saia F, et al.; RERIC (Regional Registry of Cardiac Surgery); REAL (Regional Registry of Coronary Angioplasties) Investigators. Coronary artery bypass grafting vs percutaneous coronary intervention in a 'real-world' setting: a comparative effectiveness study based on propensity score-matched cohorts. Eur J Cardiothorac Surg. 2013;44(1):e16–24.
Head SJ, Milojevic M, Daemen J, Ahn JM, Boersma E, Christiansen EH, et al. Mortality after coronary artery bypass grafting versus percutaneous coronary intervention with stenting for coronary artery disease: a pooled analysis of individual patient data. Lancet. 2018;391(10124):939–48.
Panoulas VF, Ilsley CJ, Kalogeras K, Khan H, Monteagudo Vela M, Dalby M, et al. Coronary artery bypass confers intermediate-term survival benefit over percutaneous coronary intervention with new-generation stents in real-world patients with multivessel coronary artery disease, including left main disease: a retrospective analysis of 6383 patients. Eur J Cardiothorac Surg. 2019;56(5):911–8.
Almeida AS, Fuchs SC, Fuchs FC, Silva AG, Lucca MB, Scopel S, Fuchs FD. Effectiveness of clinical, surgical and percutaneous treatment to prevent cardiovascular events in patients referred for elective coronary angiography: an observational study. Vasc Health Risk Manag. 2020;16:285–97.
Spertus JA, Jones PG, Maron DJ, O'Brien SM, Reynolds HR, Rosenberg Y, et al. ISCHEMIA Research Group. Health-status outcomes with invasive or conservative care in coronary disease. N Engl J Med. 2020;382(15):1408–19.
Abdallah MS, Wang K, Magnuson EA, Osnabrugge RL, Kappetein AP, Morice MC, et al. SYNTAX Trial Investigators. Quality of life after surgery or des in patients with 3-vessel or left main disease. J Am Coll Cardiol. 2017;69(16):2039–50.
Benzer W, Höfer S, Oldridge NB. Health-related quality of life in patients with coronary artery disease after different treatments for angina in routine clinical practice. Herz. 2003;28:421–8.
Lukkarinen H, Hentinen M. Treatments of coronary artery disease improve quality of life in the long term. Nurs Res. 2006;55(1):26–33.
Škodová Z, van Dijk JP, Nagyová I, Rosenberger J, Ondušová D, Middel B, et al. Psychosocial predictors of change in quality of life in patients after coronary interventions. Heart Lung. 2011;40(4):331–9.
Höfer S, Doering S, Rumpold G, Oldridge N, Benzer W. Determinants of health-related quality of life in patients with coronary artery disease. Eur J Cardiovasc Prev Rehabil. 2006;13(3):398–406.
Takousi MG, Schmeer S, Manaras I, Olympios CD, Makos G, Troop NA. Health-Related quality of life after coronary revascularization: a systematic review with meta-analysis. Hellenic J Cardiol. 2016;S1109–9666(16):30145–52.
Zhang Z, Mahoney EM, Stables RH, Booth J, Nugara F, Spertus JA, et al. Disease-specific health status after stent-assisted percutaneous coronary intervention and coronary artery bypass surgery: one-year results from the Stent or Surgery trial. Circulation. 2003;108(14):1694–700.
Cohen DJ, Van Hout B, Serruys PW, Mohr FW, Macaya C, den Heijer P, et al. Synergy between PCI with Taxus and Cardiac Surgery Investigators. Quality of life after PCI with drug-eluting stents or coronary-artery bypass surgery. N Engl J Med. 2011;364(11):1016–26.
Trevisol DJ, Moreira LB, Fuchs FD, Fuchs SC. Health-related quality of life is worse in individuals with hypertension under drug treatment: results of population-based study. J Hum Hypertens. 2012;26(6):374–80.
Ware JE, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–33.
Ware J, Kosinski M, Turner-Bowker DM, Gandek B. How to score version 2 of the SF-12 Health Survey (with a supplement documenting version 1). Boston: Quality-Metric Incorporated; 2004.
Gandek B, Ware JE, Aaronson NK, Apolone G, Bjorner JB, Brazier JE, et al. Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: results from the IQOLA project. J Clin Epidemiol. 1998;51(11):1171–8.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453–7.
Coelho R, Ramos SC, Prata J, Bettencourt P, Ferreira A, Cerqueira-Gomes M. Heart failure and health related quality of life. Clin Pract Epidemiol Ment Health. 2005;1:19.
Goyal TM, Idler EL, Krause TJ, Contrada RJ. Quality of life following cardiac surgery: impact of the severity and course of depressive symptoms. Psychosom Med. 2005;67(5):759–65.
Thompson DR, Yu CM. Quality of life in patients with coronary heart disease. I: assessment tools. Health Qual Life Outcomes. 2003;1:42.
Investigators TIME. Trial of invasive versus medical therapy in elderly patients with chronic symptomatic coronary-artery disease (TIME): a randomised trial. Lancet. 2000;358(9286):951–7.
Cohen DJ, Van Hout B, Serruys PW, Mohr FW, Macaya C, den Heijer P, Vrakking MM, et al. Synergy between PCI with Taxus and Cardiac Surgery Investigators. Quality of life after PCI with drug-eluting stents or coronary-artery bypass surgery. N Engl J Med. 2011;364(11):1016–26.
Funding
This study was financed in part by the Programa de Excelência Acadêmica (PROEX), from the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (Coordination for the Improvement of Higher Education Personnel; CAPES)—Brasil—Finance Code 001; (Lucas Molinari Veloso da Silveira received a fellowship from the Programa de Bolsa Espescial—Doutorado em Pesquisa Médica Nº 62/2014; Sandra C. Fuchs received a fellowship from the National Council for Scientific and Technological Development (CNPq), number: 309023/2015–7; Flavio D. Fuchs received a fellowship from the National Council for Scientific and Technological Development (CNPq), number: 302966/2019–6. In addition, the Hospital de Clínicas de Porto Alegre also provided financial support (Fundo de Incentivo à Pesquisa e Eventos; FIPE/HCPA), number: 13–0171. Aline Gonçalves da Silva and Samuel Scopel received undergraduate fellowships from PROBIC FAPERGS-HCPA. The sponsors had no participation in the design or conduct of the study or preparation and approval of the manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study's conception and design. Material preparation, data collection and analysis were performed by LMVdS, ASA, AGS, MBL, and SS. LMVdS wrote the first draft of the manuscript, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Hospital das Clínicas de Porto Alegre Ethics Committee approved the study, registered under No. 13-0171. The Office for Human Research Protections accredited this committee as an institutional review board. All participants provided written informed consent.
Consent for publication
All authors consented to the publication of the final version of the article.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
da Silveira, L.M.V., Almeida, A.S., Fuchs, F.C. et al. Quality of life in patients with stable coronary artery disease submitted to percutaneous, surgical, and medical therapies: a cohort study. Health Qual Life Outcomes 19, 261 (2021). https://doi.org/10.1186/s12955-021-01886-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12955-021-01886-7