Abstract
Background
This study tested the homeostatic model of subjective quality of life in a group of 47 short stay patients as they progressed through the stages of hospitalization for surgery.
Method
Participants completed a questionnaire measuring subjective quality of life, positive and negative affect, self-esteem, optimism and cognitive flexibility, the day prior to admission (T1), two days post-operation (T2) and one week after discharge (T3). Neuroticism and Extroversion were measured at Time 1.
Results
All variables remained stable across the three times, apart from positive affect, which dropped significantly post-operation but returned to its previous level post discharge.
Conclusion
Although the homeostatic model of subjective quality of life was supported at Time 1, the analyses raise doubts about the stability of personality. This finding is consistent with recent discussions of personality.
Similar content being viewed by others
Background
It has now been established that when population means are used as data, people are satisfied with their lives within the range of 70–80 percent of the measurement scale maximum score (percent of scale maximum or % SM: [1]). The consistency of such data is remarkable, and it has been argued [2, 3] that this restricted normative range indicates that subjective quality of life (SQOL) is actively managed by a homeostatic system. This idea has been extended in a number of useful ways. First, when the scores of individuals are used as data, the group mean remains at 75% SM but the normative range becomes 50–100% SM [4]. Thus, people who record a level of SQOL less than 50% SM can be considered to be experiencing homeostatic failure. Second, aggregate satisfaction with the seven life domains that comprise the Comprehensive Quality of Life Scale (to be used in this study) also conform with the above distributional characteristics [5]. Finally, a model for SQOL homeostasis has been published [6], and is shown in Figure 1.
This model depicts SQOL as the outcome from a combination of personality, which is proposed to provide affect balance, cognition involving the 'second order determinants' of self-esteem, optimism, and control, and interaction with the environment. At least since the time of Hall [7], it has been proposed that SQOL can be defined through these three elements. More recently SQOL has been confirmed as having a strong trait component (e.g. see [8] for a review) that explains around half of the SQOL variance [9], and with a heritability of around 80 percent [10]. The cognitive processes that involve self-esteem, perceived control, and optimism have also been proposed to be intimately involved in SQOL generation [11]. Feedback control for homeostatic maintenance is proposed to involve behavior [11]. That is, a system that produces overly high SQOL will result in magnified risk-taking behavior. This will result in an increased probability of personal failure which, when it occurs, will cause SQOL to be reduced. Conversely, if homeostasis fails, the person becomes depressed, and their behavioral withdrawal allows the homeostatic mechanisms of adaptation to regain control of SQOL.
The relative contribution of affect and cognition to the maintenance of SQOL, and the relationship between them, is uncertain. In particular the question as to whether cognition mediates affect and thus the two work as a single system, or whether affect can be experienced without cognition, and therefore, be considered as a separate system, remains unresolved. While Zajonc [12, 13] has argued for the independent systems approach and the primacy of affect, Parrott and Sabini [14] concluded that there is no compelling reason to suggest that affect is independent from cognition. In our view, cognition is influenced by the affective background level determined by personality (Figure 1).
Interestingly, different forms of psychopathology involve disorders of affect and cognition to varying degrees. In terms of affect, this concerns varying extents of heightened negative affect and reduced positive affect. The largest such changes occur in association with depression, and less change will be associated with disorders such as obsessive compulsive disorders where people generally experience more negative and less positive affect, but not necessarily to the point of depression. In terms of cognition, the disorders involve a syndrome of constricted cognitions in which the people concerned either are unable to focus on thoughts normally associated with positive affects ("happy thoughts") as occurs in depression, or are focused on very limited aspects of their interactions with the environment. This latter condition may occur for example, in anorexia nervosa, where cognitions are preoccupied with issues of food intake and body image. Moreover, since such cognitions are driven by a sense of dissatisfaction with weight gain and body image, they likely act to decrease SQOL.
Thus, the capacity to be cognitively flexible in interactions with the environment may be important in SQOL judgments, particularly when the person is under stress. It also is important to note, however, that SQOL is not susceptible to the influence of overall level of quality of cognition. The literature provides no support that IQ is linked in any simple way with SQOL, and indeed, people with an intellectual disability living in the community have an average SQOL lying within the normal range [15].
Subjective quality of life and illness
According to the theory of SQOL homeostasis (Figure 1), and in accordance with empirical data [16], there is no simple relationship between medical health and the level of subjective life quality. Provided that a medical condition does not overly tax the homeostatic system, adaptation to changed functional status will occur and the level of SQOL will reflect the set-point-range determined by each individual's personality. However, some aspects of injury and disease can defeat the homeostatic system. This is particularly the case where a sudden loss of functional status is experienced or where the medical condition involves substantial pain. Under such circumstances, and in accordance with Figure 1, the pathological condition (as the 'Third order determinant') dominates the system and drives SQOL down.
In this study, we set out to test the homeostatic model using a sample of surgery patients. We suggested that this sample would be quite heterogeneous with regard to SQOL. While all will be experiencing a substantial challenge to their homeostatic systems, some will be able to deal effectively with this challenge, while others will not. As a consequence it is anticipated that these patients will exhibit wide variation in their initial levels of SQOL. The relative proportion who are, and who are not, experiencing such compromise on admission is not known and will be an exploratory feature of this study. However, it is anticipated that effective treatment following admission and habitation to hospital routines will return many compromised patients back to within the normal 50–100% SM range.
The aims of this study were:
-
a.
to investigate the SQOL of patients with a medical condition requiring surgery, and to monitor it as they progress through the surgery process
-
b.
to test the predictive model proposed in Figure 1 at each stage of the treatment process
-
c.
to investigate whether cognitive flexibility makes a unique contribution to the prediction of subjective wellbeing.
Method
Participants
All short stay (less than one week) surgery patients (n = 148) at a regional hospital over a six-month period were invited to participate in the study. The majority were gynecological patients (n = 78) and orthopaedic patients (n = 52). The remainder were a mixed group of choleycyctectomy, varicose veins and mastectomy patients. Sixty-eight patients (64 females and 4 males) agreed to participate, and completed the questionnaires at their pre-admission assessment. Fifty-three of these patients agreed to complete the questionnaires again within two days post-operative and forty-seven completed them again within a week of discharge. Of these, 45 were female (mean age = 44.80, SD = 12.89) and two were male (aged 34 and 68).
Materials
A questionnaire package was developed for the purpose of the study. It consisted of a demographic sheet that recorded the participant's age, gender and case number, and the following standard scales, all of which have sound psychometric properties:
-
a.
The satisfaction subscale of the Comprehensive Quality of Life Scale (ComQol) – Adult version [17]. This instrument measures the level of perceived satisfaction with each of seven domains as follows: material wellbeing, health, productivity, intimacy, safety, community, and emotional wellbeing. This scale is psychometrically sound [18], and also produces a total score which falls within the gold-standard range for life satisfaction of 70–80% SM [5]. The possible range of scores is 0–100.
-
b.
The Cognitive Flexibility Scale [19]. This 8 item scale measures three components of cognitive flexibility (awareness of options and alternatives, willingness to be flexible and adaptable, and self-efficacy in being flexible). The authors report that the scale demonstrates good internal reliability, and construct and concurrent validity. Scores were calculated to range from 0–10.
-
c.
The Dispositional Mood Scale (reduced version) [20]. This is a standard instrument that measures trait mood using both poles (high and low) of positive and negative affect. The reduced version comprises 16 items. The authors of the original scale report internal consistency reliabilities ranging from .87 to .93. In this study, scores were calculated so that they ranged from 0–10.
-
d.
The Extroversion and Neuroticism subscales of the NEO Five-Factor Inventory [21]. Each subscale consists of 12 items and their reliability and validity are well-established. Internal consistency for the domain scales range from .76 to .93, and scores for adults are extremely stable with retest coefficients ranging from .63 to .83 [21]. Scores in this study were calculated so that they ranged from 0–10.
-
e.
Rosenberg Self-Esteem Scale [22]. This is a standard 10-item instrument for measuring self-esteem. It has sound psychometric properties, with test-retest correlations typically being in the range of .82 to .88, and Cronbach's alpha for various samples being in the range of .77 to .88 [23]. The scoring range for this study was 0–10.
-
f.
Primary and Secondary Cognitive Control Scale [24]. This is the third edition of this scale that has been in development since 1998. The Primary Control scale has seven items and the Secondary Control Scale has 17 items. These have a Cronbach alpha of .87 and .89 respectively. Scores for primary control range from 0–10 and for secondary control from 0–5.
-
g.
Revised Life Orientation Test [25]. This instrument measures optimism. Only the three positively worded items were used. These items have been shown to have a Cronbach alpha of 0.68 [26]. Scores were calculated to range from 0–10.
Three versions of the questionnaire were produced and colour-coded to differentiate the three administration times. The second and third versions of the questionnaire did not include the NEO-Five-Factor Inventory items, since there has been a broad consensus in the literature that personality is reasonably constant over the adult lifespan and is therefore a stable personal characteristic [28, 28]. On this basis, it was assumed that only one measure of personality was needed. This also reduced the burden on participants in terms of time and effort.
Procedure
Ethics approval for the project was obtained from Deakin University and the Healthcare Service that administers the hospital from which participants were recruited.
Patients presenting for surgery routinely report to the hospital for a pre-surgery assessment one to 10 days prior to admission. At this point, the surgery unit manager invited the patients to participate in the study, provided them with a statement that gave the details of the study, and the requirements of participants. If the patient agreed to participate in the study, they then completed the first version of the questionnaire.
Within two days after surgery, the patients were asked to complete the second version of the questionnaire. At discharge, they were asked to complete the third version of the questionnaire after one week, and return it via reply paid mail.
Statistical Analysis
SPSS version II was used to analyze the data, using descriptive and correlational analysis, multivariate analysis of variance, and regression analyses.
Results
Table 1 summarizes the mean scores on each of the variables at each assessment period. All analyses were based on the data provided by the 47 participants who completed the questionnaire on each of the three testing occasions. These participants were not different from the participants who commenced the study but did not complete it (n= 21), other than being marginally less extraverted (p = .04). That is, at the first point of data collection, there were no significant differences between those who went on to complete the study and those who did not, in relation to any of the variables measured, other than extraversion. While we realize that this number of participants is below the recommended number for using multivariate statistics, the results are fairly clear-cut such that the addition of a few more cases would be unlikely to change the outcome.
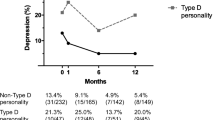
Multivariate Analysis of Variance, which tests the significance of differences between/within groups across time or variables, was applied to the data. The analysis indicated no significant effect for time (F [2,40] = .55). Post-hoc analyses indicated that only positive affect varied significantly over the three testing occasions. It decreased significantly immediately after the operation, but returned to its previous levels post-discharge.
The most critical value to note in Table 1 is the satisfaction score at Time 1 of 70.5 ± 18.8. Given the normative range of 70–80% SM [5, 2] this initial mean score indicates that the patients who agreed to take part in this study had, as a group, a level of subjective wellbeing that lies at the lower margin of the normative range. Thus, while some members of the group would have homeostatic failure, the majority would not, and so any intervention given to this majority would not be expected to increase their SQOL to any great extent. Indeed, the data displayed in Table 1 indicate that this is the case, as while SQOL scores increased by 2.9 percentage points over the course of this study, this increase was not significant.
Relationships between the variables
Table 2 shows the correlations between all variables at each of the times in the study. One observation that can be made in relation to Table 2 is that the average degree of correlation between the two measures of personality and the other variables systematically decreases from Time 1 to Time 3. In the case of Extroversion the average correlations (ignoring sign) with the other non-personality variables (1 and 4–10 in Table 2) are .43, .36, and .33 at Times 1, 2 and 3 respectively. This represents an average degree of shared variance of 18.3%, 12.7%, and 11.2% respectively. In the case of Neuroticism the decrease is even more marked (.46, .34, .23 or 21.1%, 11.3%, and 5.4%). There is a distinct possibility that this progressive disassociation may have been due to the fact that both personality variables were measured only once at Time 1. This limitation was imposed on the assumption that such personality measures should be stable over the few weeks of the study. In retrospect, however, this assumption may have been unwarranted and this progressive reduction in the degree of association with other variables could be a methodological artifact.
Testing the Model
In order to test the proposed model for subjective wellbeing homeostasis, three hierarchical multiple regressions were conducted, one for each time period. Multiple regression analysis assesses the amount of variance in the dependent variable attributable to the independent variables. The hierarchical procedure used here assesses the additional variance in the dependent variable explained by particular independent variables after the variance accounted for by other independent variables entered at Step 1 etc has been controlled. A power statistic can be derived to assess whether the ratio between participants and number of variables in the model is adequate (>0.8). In the current analyses, the two personality variables were entered as the first step, the three buffers at Step 2 (Control, Optimism, and Self-Esteem), and Cognitive Flexibility at Step 3. The results of these analyses are provided in Table 3. The power statistic for the analysis at each time was 1.0 (p < 0.05), indicating that there were sufficient participants for the analyses in relation to the number of variables.
The following observations can be made:
-
1.
At Time 1 the variables together explained 71 percent of the variance. This value is high enough to expect that most of the measurable variance has been captured.
-
2.
At Time 1 the dominating variables are Extroversion and Neuroticism, just as predicted by the model.
-
3.
At Times 2 and 3, predictive dominance switches from personality to the buffers. By Time 3 the buffers are contributing over five times the unique predictive variance of personality (9.9 percent vs 1.8 percent).
-
4.
Of the three buffers, only self-esteem and optimism were able to contribute unique variance beyond that of the two personality variables. At Time 1 this unique contribution was limited to self-esteem, at Time 2 both variables contributed unique variance, while Time 3 was restricted to optimism.
-
5.
Cognitive Flexibility made no unique contribution to the predictive variance at any time.
Discussion
The aims of this study were threefold: to chart SQOL as patients progress through short stay hospitalization for surgery, to test the model of subjective wellbeing homeostasis at each stage of the process, and to determine whether cognitive flexibility makes a unique contribution to the prediction of wellbeing. The results are surprising and affirm some aspects of the homeostatic model of wellbeing, while also providing insights that will be useful to guide future research in this area.
Perhaps the most surprising result is that the patient group remained within the normal range of subjective wellbeing throughout the study. It is now well established that the normative range of subjective wellbeing in relation to group mean scores is 70 to 80% SM [5, 29]. This understanding allows a crucial level of interpretation to be applied to the current data. This is that, since this group of people commenced the study operating within this normative range, the majority of the patients were successfully maintaining their SQOL prior to surgery. Thus, for this group, the extent to which the subsequent treatment had the potential to elevate their SQOL was very limited. Cummins [6] has argued that people have a narrow 'set-point-range' within which the homeostatic system operates to control SQOL. This range may be around five percentage points. Thus, assuming that the pre-surgical circumstances were aversive enough to push this majority group's SQOL down towards the lower margin of their range, some slight increment might be achieved as a consequence of the surgery, but not of sufficient magnitude to be detected in a small sample above the 'noise' of individual differences in variation due to other factors. It is also notable that the standard deviation decreased by 2.8% SM during the study, which is consistent with the intervention being effective in allowing some patients to restore their homeostatic control of SQOL. However, over the whole sample, the number of patients was insufficient to demonstrate an overall SQOL change. This is an important vindication of theory and constitutes the basis for advice to future investigators who are seeking to demonstrate positive change in subjective wellbeing as a consequence of some form of intervention. If the target group members have an initial level of wellbeing that lies within the normative range of 70–80% SM, then the chances that the intervention will result in a demonstrable elevation of SQOL are slim unless the sample is large.
The analyses also suggest that only the data at Time 1 can be considered to be a proper test-bed in relation to the model. The reason for this is that the two personality factors were measured only at Time 1, with the assumption that they would remain stable throughout the course of the study. It is apparent, however, that this assumption may have been false, and that there is evidence, to be discussed later, that personality may have been unstable across the three measurement times.
In terms of the data at Time 1, there is partial support for the model. Clearly extroversion and neuroticism dominated in their prediction of subjective wellbeing, and the only buffer to make an independent contribution to the predictive variance was self-esteem. It is notable, however, that the personality and buffer variables between them were able to explain a massive 71% of the variance in subjective wellbeing. What this indicates is the gross dominance of personality under such 'resting' conditions, where subjective wellbeing is not under threat and operating well within its normal range. It is possible that the buffers would play a more determined role in subjective wellbeing management under conditions of greater environmental challenge. This possibility is not testable here, not only due to the normative levels of subjective wellbeing, but also because personality was only measured at Time 1. Notably, cognitive flexibility scores were found to make no unique contribution to scores SQOL. This finding indicates that cognitive flexibility plays no role in the determination SQOL.
There has been a broad consensus in the literature that personality is a dispositional trait (eg. [30]) that is, therefore, held fairly constant over the adult lifespan as a stable personal characteristic [27]; [28]. This, however was not always the generally held belief, with some earlier authorities stating that in their view personality traits are quite ephemeral concepts (eg. [31]). While few contemporary authors would describe personality traits as 'ephemeral', the evidence is certainly mounting that neither are they rigidly fixed. In a review of the relationship between personality and subjective wellbeing, Diener, Suh, Lucas and Smith [32] conclude that while there is clearly a genetic influence of personality on subjective wellbeing, the estimates of the strength of this influence vary widely. Moreover, other literature is providing mounting evidence that the apparent stability may, at least in part, be a product of human conservatism. That is, people generally adopt a living environment to suit their personality, thus providing for themselves a fairly consistent framework of person-environment interactions.
This was also the conclusion drawn by Caspi and Roberts [33] in their review of personality development across the life-course. While they found the literature to generally support the stability of personality as people age, they are firm in their opinion that such general stability does not support the conclusion that personality becomes fixed at a certain age. If a person experiences severe environmental dislocation or a major life event, it is quite likely that their personality structure will change as a consequence. This view has been corroborated by Willebrand, Kildal, Anderson and Ekselius [34] who found that 3–19 years after traumatic burn injury, people had higher neuroticism than scale norms. Similar changes have been reported for people with severe arthritis [35]. Thus it seems that the conclusion reached by Roberts and DelVecchio [36] from their meta-analysis of personality trait consistency, represents the contemporary view. That is, while personality traits are mainly consistent in adulthood, they retain a dynamic potential in the face of severe environmental challenge.
So, the question now is whether the experience of hospitalization and surgery is sufficient to produce a change in personality along the lines that have been suggested. It seems that the answer may be in the affirmative. Personality change during the course of this study is evident through the diminishing strength of intercorrelations between the personality and other variables from Time 1 to Times 2 and 3. This suggestion of personality change is very interesting and raises the whole issue of the degree of environmental challenge that is capable of causing such alterations in the relationships between variables. Recall that subjective wellbeing remained within its normal range, so the nature of the medical condition and the experience of hospitalization were not sufficiently aversive to defeat subjective well being homeostasis. Such changes may, however, provide insight into the dynamics of homeostasis in terms of its internal management. Previous studies (e.g. [37]) have indicated the presence of 'domain compensation'. Here, as homeostasis is challenged but not defeated, satisfaction with those domains under most stress decreases, while satisfaction with other domains increases in a compensatory manner, thereby maintaining overall satisfaction within its normative range. It is quite possible that other forms of internal adjustment during times of stress might also involve personality. A future study will be required to test this by incorporating the sequential measurement of personality into a study such as we have performed.
The interesting understanding to emerge from this study is that the group of people who volunteered to be part of the study had a normal range SQOL. In other words, the less than life-threatening and non-traumatic nature of their medical conditions, and the surgical interventions required, did not represent environmental challenges of sufficient intensity to defeat homeostasis. Thus, no intervention was likely to raise their levels of well-being since their homeostatic systems were already effective. A more interesting group would be those people who enter hospital in conditions of homeostatic defeat, but how to ethically recruit such a sample is problematic. Clearly, a much larger sample than the one used in this study is required to adequately investigate the issues raised here.
Conclusions
Previous research investigating the relationships between illness and SQOL has produced equivocal results. Our study suggests that some conditions requiring surgery do not necessarily affect SQOL, and that for people who enter hospital with a normal range SQOL, their levels will remain fairly consistent through the surgery and recovery periods. Our findings support the homeostatic model of subjective wellbeing. However, personality may be a less stable characteristic, and the dynamics of the homeostatic model of wellbeing require further investigation.
References
Cummins RA: On the trail of the gold standard for life satisfaction. Soc Indicators Res 1995, 35: 179–200.
Cummins RA: The second approximation to an international standard of life satisfaction. Soc Indicators Res 1998, 43: 307–334. 10.1023/A:1006831107052
Cummins RA, Gullone E, Lau ALD: A model of subjective well being homeostasis: The role of personality. In The universality of subjective wellbeing indicators (Edited by: Gullone E, Cummins RA). Soc Indicators Res Ser 2002, 7–46.
Cummins RA: Normative life satisfaction: Measurement issues and a homeostatic model. Soc Indicators Res, in press.
Cummins RA: The domains of life satisfaction: An attempt to order chaos. Soc Indicators Res 1996, 38: 303–332.
Cummins RA: Personal income and subjective well-being: A review. J Happiness Studies 2000, 1: 133–158. 10.1023/A:1010079728426
Hall J: Measuring the quality of life using sample surveys. In Technology assessment of quality of life (Edited by: Stoker GJ, Schumacher D Elsevier). Scientific Publishing Company, Proceedings of the 4th General Conference of SAINT. Salzburg, Austria. 1973, 94–102.
McNeil JK, Stones MJ, Kozma A: Subjective well-being in later life: Issues concerning measurement and prediction. Soc Indicators Res 1986, 18: 35–70.
Tellegen A, Bouchard Jr TJ, Wilcox KJ, Segal NL, Lykken DT, Rich S: Personality similarity in twins reared apart and together. J Pers Soc Psychol 1998, 54: 1031–1039.
Lykken D, Tellegen A: Happiness is a stochastic phenomenon. Psychol Sci 1996, 7: 186–189.
Cummins RA, Nistico H: Maintaining life satisfaction: The role of positive cognitive bias. J Happiness Studies 2002, 3: 37–69. 10.1023/A:1015678915305
Zajonc RB: Feeling and thinking: Preferences need no inference. Am Psychol 1980, 35: 151–175. 10.1037//0003-066X.35.2.151
Zajonc RB: On the primacy of affect. Am Psychol 1984, 39: 117–123.
Parrott WG, Sabini J: On the "emotional" qualities of certain types of cognition: A reply to arguments for the independence of cognition and affect. Cognitive Ther Res 1989, 13: 49–65.
Verri AP, Cummins RA, Petito F, Vallero E, Monteath S, Gerosa E, Nappi G: An Italian-Australian comparison of life quality among intellectually disabled people living in the community. J Intellect Disabil Res 1999, 43: 513–522. 10.1046/j.1365-2788.1999.00241.x
Cummins RA: Objective and subjective quality of life: An interactive model. Soc Indicators Res 2000, 52: 55–72. 10.1023/A:1007027822521
Cummins RA: Comprehensive Quality of Life Scale. Adult Manual Fifth Edition Melbourne: Deakin University School of Psychology 1997.
Cummins RA, McCabe MP, Romeo Y, Gullone E: The Comprehensive Quality of Life Scale: Instrument development and psychometric evaluation on tertiary staff and students. Educ Psychol Meas 1994, 54: 372–382.
Martin MM, Rubin RB: A new measure of cognitive flexibility. Psychol Rep 1995, 76: 623–626.
Huelsman TJ, Nemanick Jr RC, Munz DC: Scales to measure four dimensions of dispositional mood: Positive energy, tiredness, negative activation, and relaxation. Educ Psychol Meas 1998, 58: 804–819.
Costa Jnr PT, McCrae RR: Neo Five-Factor Inventory Odessa, Fl: Psychological Assessment Resources Inc 1991.
Rosenberg M: Conceiving the self New York: Basic Books 1979.
Blascovich J, Tomaka J: Measures of Self-Esteem. In Measures of Personality and Social Psychological Attitudes 3 Edition (Edited by: Robinson JP, Shaver PR, Wrightsman LS, Ann Arbor). Institute for Social Research 1993, 115–160.
Heeps L, Cummins RA, Croft C: The Primary and Secondary Control Scale Melbourne: Deakin University School of Psychology 2000.
Scheier MF, Carver CS: Optimism, coping, and health: Assessment and implications of generalized outcome expectancies. Health Psychol 1985, 4: 219–247. 10.1037//0278-6133.4.3.219
Lai JCL: Differential predictive power of the positively versus the negatively worded items of the life orientation test. Psychol Rep 1994, 75: 1507–1515.
Headey B, Wearing A: Personality, life events, and subjective well-being: Toward a dynamic equilibrium model. J Pers Soc Psychol 1989, 57: 731–739. 10.1037//0022-3514.57.4.731
McCrae RR, Costa Jnr PT: Trait explanations in personality psychology. Eur J Personality 1995, 9: 231–252.
Cummins RA, Eckersley R, Lo SK, Okerstrom E, Hunter B, Davern M: Australian Unity Wellbeing Index: Report 6.0 – The Wellbeing of Australians – The Impact of the Iraq Situation Melbourne: Australian Centre on Quality of Life, School of Psychology, Deakin University 2003.
Brief AP, Butcher AH, George JM, Link KE: Bottom-up and top-down theories of subjective well-being: The case of health. J Pers Soc Psychol 1993, 64: 646–653. 10.1037//0022-3514.64.4.646
Mischel W: Personality and assessment New York: Wiley 1968.
Diener E, Suh EM, Lucas RE, Smith HL: Subjective well-being: Three decades of progress. Psychol Bull 1999, 125: 276–302. 10.1037//0033-2909.125.2.276
Caspi A, Roberts BW: Personality development across the life course: The argument for change and continuity. Psychol Inq 2001, 12: 49–67. 10.1207/S15327965PLI1202_01
Willebrand M, Kildal M, Andersson G, Ekselius L: Long-term assessment of personality after burn trauma in adults. J Nerv Ment Dis 2002, 190: 53. 10.1097/00005053-200201000-00015
Germano D, Misajon R, Cummins RA: Quality of life and sense of coherence in people with arthritis. J Clin Psychol Med S 2001, 8: 253–261. 10.1023/A:1011964729100
Roberts BW, DelVecchio WF: The rank-order consistency of personality traits from childhood to old age: A quantitative review of longitudinal studies. Psychol Bull 2000, 126: 3–25. 10.1037//0033-2909.126.1.3
Best C, Cummins RA, Lo SK: The quality of rural and metropolitan life. Aust J Psychol 2000, 52: 69–74.
Author information
Authors and Affiliations
Corresponding author
Additional information
Authors' contributions
David Mellor and Robert Cummins conceived the study, participated in the design of the study, conducted the statistical analyses, and drafted the manuscript. Evelyn Karlinski participated in the design of the study and oversaw the collection of data. Shane Storer participated in the coordination of the study. All authors read and approved the fund manuscript.
David J Mellor, Robert A Cummins, Evelyn Karlinski and Shane P Storer contributed equally to this work.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Mellor, D.J., Cummins, R.A., Karlinski, E. et al. The management of subjective quality of life by short-stay hospital patients: An exploratory study. Health Qual Life Outcomes 1, 39 (2003). https://doi.org/10.1186/1477-7525-1-39
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1477-7525-1-39