Abstract
Background
Foods enriched with phytosterols have been proven to be an effective therapy to improve blood lipid profiles. However, none of the studies have investigated the efficacy in lipid lowering of plant sterol esters (PSE) in capsule form. The objective of this study is to determine if the plant sterol esters (PSE) in capsule form (1.3 grams of PSE/day) lowered plasma cholesterol levels and lipid ratios in free-living hypercholesterolemic subjects during a 4-week intervention period.
Methods
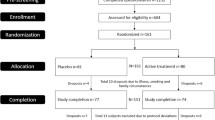
Sixteen subjects participated in a double-blind, placebo-controlled, sequential study with a 4-week placebo phase followed by a 2-week wash-out period and a 4-week treatment phase. Subjects were instructed to maintain stable diet pattern and physical activities. Blood samples were collected at 7, 21 and 28 days of each phase. The primary measurements were change in plasma total cholesterol (TC), HDL-cholesterol (HDL) and LDL-cholesterol (LDL) between phases and within each phase. The secondary measurements were change in triglycerides, lipoprotein ratios (TC/HDL, LDL/HDL) and C-reactive protein (CRP).
Results
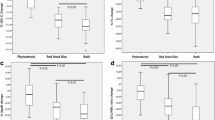
In comparison to placebo, LDL-cholesterol was significantly reduced by 7% and 4% (P < 0.05) at both week 3 and week 4; HDL at week 3 of the treatment was significantly increased by 9% (P < 0.01), but not at week 4 (4%); total cholesterol was not significantly different from placebo throughout the period, TC/HDL and LDL/HDL were significantly reduced by (8%, 8%, 6%, 10%, respectively) (P < 0.01) at both week 3 and week 4. CRP and triglycerides did not differ either between the two phases or during the treatment phase.
Conclusion
In conclusion, plant sterol ester capsule is effective in improving lipid profiles among hypercholesterolemic subjects in a free-living setting at the minimum dosage recommended by FDA. The significant improved lipid profiles were reached after three weeks of administration. To achieve better lipid lowering results, higher dosages and combination with diets low in saturated fat and cholesterol are recommended.
Similar content being viewed by others
Background
Elevated LDL-cholesterol is a significant risk factor for coronary artery disease. The use of statin drugs is the current therapeutic option for lowering LDL-cholesterol and improving lipid profile in hypercholesteremic patients. According to the American Heart Association guidelines, other options should be considered as well to treat or prevent hypercholesterolemia, including the use of phytosterols. Phytosterols, either as plant sterols or plant stanols, are natural cholesterol-like substances derived from plants [1]. The main mechanism by which phytosterols reduce blood cholesterol is to inhibit cholesterol absorption in the small intestine. Therefore, the physical forms, carriers and solubilization of the phytosterols are important characteristics to determine the efficacy of phytosterols on cholesterol lowering [2].
In terms of physical forms, free phytosterols are water and oil insoluble. The efficacy on lowering blood cholesterol of free phytosterols is often dependant on the dispersion capability in water and oil [3–5]. Recently, soy lecithin has been used to form more dispersible complexes with free sterol or stanol resulting in more bioavailable free sterol/stanol formulation than previous formulations [6–8]. However, the improved efficacy has only been confirmed in tablet forms, but not in the capsule form [7, 8]. Fatty acid esters of sterols or stanols, on the other hand, are oil soluble. Thus, they are more easily dispersible in oils than free sterols or stanols which make them a better choice for soft gel capsules than the free sterol/stanol.
In terms of carriers, there is abundant evidence suggesting LDL-cholesterol lowering efficacy of phytosterols either as plant sterols or stanols in food forms, including water emulsions [3]; water as lecithin micelles [9]; yogurt [10, 11]; low fat milk [12, 13]; chocolate [14]; cereal; snack bars, breads, and beverages [15, 16]. However, there are very few studies that investigated if these compounds provided as pharmaceutical forms, such as tablets and capsules, offer the same benefits [2, 7, 8]. The information on non-food forms is essential for long term supplementation strategy. As indicated by Law et al, (1994 and 2003), to achieve life saving benefits from mortality associated with heart disease and stroke, the LDL-cholesterol lowering strategy needs to be maintained for at least two years, and preferably for five years [17, 18]. The pharmaceutical dosage forms, such as tablets and capsules, can provide more convenience and flexibility needed for the recommended long term usage than the traditional food applications [2]. Furthermore, these forms could be better delivery vehicles for phytosterols to be incorporated into the combination therapeutic strategy with pharmaceutical agents to provide an additional LDL-cholesterol lowering effect [19–21]. Unfortunately, none of the studies with these pharmaceutical forms used plant sterol esters [2, 8]. Considering plant sterol ester is a more dispersible form in oil than free phytosterols, phytosterol esters may be more suitable choice for soft gel capsules than free plant sterols/stanols.
The present study was designed to confirm the efficacy of the plant sterol esters (PSE) in capsule form on lipid profile lowering in free-living hypercholesterolemic subjects during a short term (4 weeks). The dosage used in the study, 1.3 g plant sterol ester (0.8 g free sterol equivalent), is the minimum dosage that is recommended by FDA's health claim [22]. The information will be essential for usage of plant sterol esters in supplement forms beyond current food applications.
Results
No subject was dismissed because of the inability to tolerate the treatment or placebo or because of an adverse action or event. The statistical evaluation was determined based upon the 16 remaining subjects who completed the total study.
Placebo vs. treatment
Total cholesterol was reduced, but not significantly, at the end of treatment period (5%) (P = 0.07) (Table 1, Figure 1). LDL-cholesterol, TC/HDL, LDL/HDL ratios were significantly reduced by 7% (P < 0.05), 8% (P < 0.01) and 6% (P < 0.01) at day 21, 4% (P < 0.05), 8% (P < 0.01) and 10% (P < 0.01) at day 28, respectively (Table 1, Figure 1). HDL at day 21 of the treatment was significantly higher in comparison to placebo (9%, P < 0.01), but not at day 28 (4%) (Table 1, Figure 2). CRP and triglycerides did not differ between placebo and treatment phase.
Within each phase
There was no significant change in any of the measurements within the placebo phase (Table 1). Within the treatment phase, in comparison to day 7, LDL was significantly reduced at day 21(P < 0.05), but not at day 28 (Table 1, Figure 1); HDL was significantly increased at both day 21 and 28 (P < 0.05) (Table 1, Figure 2); TC/HDL and LDL/HDL ratios were significantly reduced at both day 21 and 28 (P < 0.001) (Table 1). Total cholesterol was reduced throughout the treatment phase, but this reduction was not significant. CRP and triglycerides did not change during the treatment phase.
Discussion
The cholesterol lowering effect of plant sterols, either as free or esterified forms, is well documented in the literature. Most studies used food forms as delivery vehicles. There are only a few studies that have evaluated the effectiveness of phytosterols in tablet or capsule form, all of which used free stanols [7, 8, 23]. To our knowledge, the present study is the first study to demonstrate a significant reduction in plasma LDL cholesterol by 4% with plant sterol esters in capsules (P < 0.05). Epidemiological studies have shown that such a 4–5% reduction of LDL correlates with a 5–10% reduction in CHD risk in the first 5 years, and by 10% over a life time [24]. This result indicates that regular use of plant sterol esters in a soft gel capsule could contribute significant benefits to long term cholesterol management as the food delivery forms. Previous studies with phytosterol fortified foods have shown reductions of 5% or more in LDL cholesterol levels relative to a control. For example, in men and women with a wide range of age and baseline cholesterol levels, 0.8 g of free sterol equivalents administrated as sterol ester in spreads decreased LDL cholesterol by 6% [25], and 1.1 g/d of free sterol equivalents in spreads as plant sterol ester decreased LDL-cholesterol by 4.9% [26]. The significant 4% reduction in plasma LDL-C in the present study indicates that regular use of plant sterol esters is equally effective in a soft gel capsule form compared to food delivery forms of similar doses.
This study was conducted in free-living subjects without collection of dietary records at baseline or during the study. Subjects were advised to maintain regular dietary habits and physical activity. This practical approach was meant to mimic plant sterol capsules consumption under various background diets. Previously, plant sterols were said to be more effective when consumed with diets containing higher levels of cholesterol or fat [2, 27], more recent studies indicated that since plant sterols impair both dietary and bilary cholesterol absorption, they are effective even when consumed with low fat diets [28–30]. Thus, the delivery regimen for the plant sterols is more crucial than the background diet. In the present study, all subjects were advised to take the capsules with each meal (lunch and dinner). As long as plant sterols are taken with meals to stimulate the bilary flow, they can effectively lower cholesterol within the context of various diets and food forms [2].
The present study showed significantly (p < 0.01) improved lipid ratios (TC/HDL and LDL/HDL) either independent of placebo or relative to placebo. These results are in agreement with previous reported studies using free stanols [7, 8] or sterol esters [31]. The improved lipid ratios are due to reduced LDL, total cholesterol and increased HDL levels during the treatment phase. While most studies published to date have reported that phytosterols have little or no effect on HDL, even with long-term use [5, 32], in our study HDL level was increased during the treatment period as compared to placebo (P < 0.05). A recent study using orange juice with plant sterols also observed an increase in HDL [33], In studies using plant sterol esters in combination with exercise, significant increase in HDL was observed [34, 35]. Since this was a cross-over study and the effect was not observed during placebo phase, it is likely to be a consequence of plant sterol ester. A longer term administration is needed to further confirm the positive effect of plant sterol ester on HDL levels.
Due to the difference in physical and chemical characteristics between esterized and free forms, plant sterol esters may be a better choice for capsules than their free form. Theoretically, both esters and free forms should possess similar cholesterol lowering effect if the free sterols are properly solubilized. Improperly dispersed formulations, such as aqueous or oil-based suspensions of solid sterols, have been reported as unsuccessful in lowering LDL-cholesterol. These formulations included a crystalline aqueous suspension of sitosterol [36], capsules containing 3 g of stanol powder dispersed in safflower oil [23], or free sterols in beverages with low fat [6]. In addition to the dispersion factor, these studies suggested that the crystal form of free sterol/stanols may be another important factor determining their solubility in intestinal fluid and their effectiveness to inhibit cholesterol absorption [37]. To enhance its solubilization in water or oils, the free plant sterols or stanols are usually added to other substances and often require the presence of fat to facilitate the emulsion. Thus, the method of dispersion, processing, and use of emulsifiers, surfactants, and crystal habit modifiers plays a crucial role in delivering small crystals of free phytosterols over time to sufficiently maintain their bioavailability [2, 12, 13]. A recent breakthrough in formulation, using soy lecithin to form more water dispersible and bioavailable complexes with free stanol, has been demonstrated to lower plasma cholesterol and LDL in two recent studies in tablet form [7, 8]. In a placebo controlled, double-blind study by McPherson et al. [7], free stanols were emulsified with soy lecithin and the spray dried preparation was used to make tablet and capsule forms that were tested in 26 subjects per group over a 6-week period. The group that received tablet form experienced reduction in both LDL cholesterol and LDL/HDL ratio by 10.4% and 11.5% respectively. However, no reduction was observed in the group that received capsules [7]. The author attributed the difference in LDL reduction to the variation in disintegration times, in so far that the tablet disintegrated much faster than the capsule form (10 min. vs. 45 min., respectively).
Fatty acid esters of sterols or stanols are oil soluble. Thus, they are more easily dispersible in oils than free sterols or stanols. Additionally, plant sterol esters are well distributed in the small intestine providing ample surface area for incorporation into bile salt micelles through the digestive process in order to inhibit cholesterol absorption [2, 24]. Earlier evidence suggested that even though the cholesterol lowering effect is similar between free sterols and stanols, the saturation state of their esterified forms may affect the ability to reduce cholesterol absorption [38]. In a clinical study conducted by Jones et al. (2000), intake of plant sterol esters from margarine resulted in larger LDL reductions than margarine with stanol ester (13% vs. 8%, respectively) [38]. However, taking the totality of evidence into account, sterol and stanol esters are probably equal in their cholesterol-lowering effect. Nevertheless, plant sterol esters remain a better choice for soft gel capsules despite the improvements in free sterols formulation to increase the bioavailability.
Finally, this study evaluated the effect of PSE on CRP, a proposed risk factor in cardiovascular disease [39]. All subjects in this study had low or average CRP levels (<3.0 mg/L) at baseline and PSE had no effect on CRP during the treatment phase. It has been demonstrated that diet can have a beneficial impact on CRP levels as observed in the "portfolio diet", a dietary prescription comprised of several foods and food components (including plant sterol esters) which are known to reduce cholesterol levels [40]. In the present study, due to the free-living study design, it is unlikely that CRP will be changed solely based on plant sterol ester treatment.
There are several limitations of this study. First, the study treatments were not randomized. The placebo and PSE treatment were conducted sequentially with wash-out period in between. There is some evidence suggesting a carry-over effect from phytosterol treatment to the placebo group [41] in randomized crossover design. The sequential design could minimize the carry-over effect since the placebo phase was performed first. To minimize the potential confounding effect due to the sequential design, such as time drifting effect, additional within group comparisons were conducted using repeated measure analysis. The results from placebo phase did not show any significant change within the 4-week period whereas significant changes were found within the treatment phase. This within group analyses confirmed that the significant changes were due to the treatment, not the time drifting effect.
Another limitation is the lack of true baseline measurements at the beginning of placebo and treatment phase. This was not intended for the original study design, but occurred during the study. To compensate for this limiting factor, the within group analyses were performed to compare measurements at day 21 and 28 to day 7 of each phase. The significant differences were only detected during the treatment phase, not the placebo phase. Additionally, there was no significant difference at day 7 of each phase between the placebo and treatment suggesting a significant treatment effect.
The number of subjects was calculated based on 10% reduction of total cholesterol. However, given the fact that the tested dose was 1.3 g plant sterol esters/day as 0.8 g free sterol equivalent/day, it is arguable that the above reduction is overestimated. Thus, the study may be underpowered which could explain the lack of significance in reduction of total cholesterol (-5%) (P = 0.07). More subjects are needed for further studies with the above dosage. Nevertheless, the present study showed a significant improvement in LDL-C occurred with the present number of subjects indicating that the effect of plant sterol ester is significant.
Conclusion
This study is the first study that confirmed regular use of plant sterol ester capsules is an effective strategy in improving lipid profiles, especially lipoprotein ratios, among hypercholesterolemic subjects in a free-living setting without dietary intervention. The clinical advantage of the capsule form is that it provides a convenient vehicle to consume without the dietary impact on calories. It can also easily be incorporated into a cholesterol-lowering regimen in standard clinical practice with counseling or therapeutic lifestyle changes including those recommended by the National Cholesterol Education Program [24, 42]. The significant improvement in LDL-C occurred in free-living subjects with little dietary control indicates that the effect of plant sterol ester is fairly significant regardless of the delivery vehicle and background diet. However, to achieve better lipid lowering effects, higher dosages and incorporation of cholesterol-lowering regimen are recommended. Further studies are needed to confirm the long term benefit of plant sterol ester capsules on blood cholesterol in populations with varying baseline cholesterol levels.
Methods
Subjects
The research protocol and informed consent were approved by the East Tennessee State University (ETSU) Institutional Review Board (IRB) Committee on Protection of Human Subjects.
Subject recruitment was conducted by campus advertisement. The questionnaire evaluation and hematological screening of potential subjects were conducted at the Nutrition Center in the Department of Internal Medicine. Inclusion criteria included men and women (not pregnant or breast feeding), borderline high or elevated serum lipid parameters, body mass index (BMI) < 30, ability to maintain stable diet and physical activity, and in otherwise healthy condition. Candidates were excluded from the study if they had
-
diseases or conditions requiring drug intervention;
-
been taking cholesterol lowering drugs, supplements or other practices, such as taking cloves of garlic every day
-
uncontrolled elevated blood pressure (systolic >160 mmHg or diastolic > 95 mmHg)
-
history or presence of drug or alcohol abuse, or alcohol intake >7 alcoholic beverages per week within the past 4 weeks
Power calculations based on expected 10% changes in total cholesterol levels determined that at least 16 subjects would be needed. Twenty subjects (total cholesterol 227–308 mg/dL, LDL 129–211 mg/dL and triglycerides 43–355 mg/dL) were included in the study. During the study phases, four subjects later withdrew due to either personal reasons or unable following restrictions, such as not taking cholesterol lowering supplements. The remaining sixteen subjects (12 female/4 male, age: 51 ± 13) (total cholesterol: 256 ± 24 mg/dL; LDL: 177 ± 23 mg/dL) completed the study. Table 2 presents the baseline means for the parameters of interest, including age and lipid values, for the 16 subjects who completed the study. Only data from the sixteen subjects were included for analysis.
Materials
Both placebo (containing soybean oil) and matching plant sterol ester capsules were manufactured by Cardinal Health (Dublin, OH). The plant sterol esters (Vegapure® 95) were manufactured by Cognis Corporation (LaGrange, IL). The plant sterol esters were prepared by esterification of free plant sterols from a mixture of soy, rapeseed and other vegetable sources, with fatty acids from sunflower oil. Mixed tocopherols and ascorbyl palmitate are used in the formulation as antioxidants and chemical preservatives. Soybean oil is used as a coating agent and texturizer (see Table 3, Table 4).
Study design and intervention phases
The study was a double-blind, placebo-controlled, non-randomized, sequential study. After the initial baseline measurements which were conducted in late December, there was a six-week period before the placebo phase to minimize lipid profile variance. For this reason, the initial baseline data was not used for comparison to any data collected in placebo and treatment phases
Six weeks after the initial baseline measurement, all subjects were assigned to a placebo phase (soybean oil) for four weeks followed by a two-week, wash-out period before proceeding to a four-week treatment phase. Subjects were instructed to take 1 capsule at each of 2 meals per day (lunch and dinner) during each phase. The PSE treatment provided a total of 1.3 grams per day of sterol esters (0.8 grams free plant sterol equivalents). This amount is the minimum dose recommended in FDA's health claim for phytosterols [22].
At the beginning of each phase, each subject was given a bottle containing 60 capsules (56 capsules are needed for 4 weeks and 4 capsules are extra). Placebo capsules and plant sterol ester capsules were identical in terms of appearance and sensory characteristics. Compliance was monitored by counting extra capsules in the bottles at the end of each phase and questioning subjects regarding missed doses. Subjects were instructed to maintain their stable diet pattern and physical activity level during the study periods. Although general advice on healthy life style was given to subjects occasionally during their visit to the Nutrition Center, neither dietary advice was given, nor were food records collected.
Fasted blood samples were collected at 7, 21 and 28 days of each phase. The primary measurements were change of plasma total cholesterol (TC), HDL-cholesterol and LDL-cholesterol between placebo and treatment. The secondary measurements were changes of triglycerides, lipoprotein ratios (TC/HDL, LDL/HDL) and CRP.
Lipids and C-Reactive Protein (CRP) analyses
Fasted serum samples were analyzed for triglycerides (TG), total cholesterol (TC), high density lipoprotein cholesterol (HDL-C), low density lipoprotein cholesterol (LDL-C), and c-reactive protein (CRP). Total cholesterol, HDL, triglycerides and CRP were performed at Johnson City Medical Center Hospital (Johnson City, TN) using an automated clinical chemistry analyzer (Beckman Synchron LX20; Fullerton, CA). LDL-cholesterol was calculated using the Friedewald formula.
Statistical analysis
Data were analyzed to detect significant differences between placebo and treatment by ANOVA. Once the significant difference was detected, paired student t-tests was performed to compare the measurements at each blood collection time (7 day, 21 day and 28 day) between placebo and treatment group. Additional within-group analysis was performed by 1-way repeated measures analysis of ANOVA to compare measurements within placebo or treatment phase in order to make sure that the expected changes were not caused by time drift during each phase. Paired student t-tests were performed to compare measurements at each blood collection time.
Abbreviations
- BMI:
-
body mass index
- CHD:
-
coronary heart disease
- CRP:
-
c-reactive protein
- dL:
-
deciliter
- ETSU:
-
East Tennessee State University
- FDA:
-
Food and Drug Administration
- g:
-
gram
- GCP:
-
Good Clinical Practice
- GLP:
-
Good Laboratory Practice
- GRAS:
-
Generally Recognized as Safe
- HDLC:
-
high-density lipoprotein cholesterol
- HPLC:
-
High Performance Liquid Chromatography
- Hg:
-
mercury
- IRB:
-
Institutional Review Board
- L:
-
liter
- LDLC:
-
low density lipoprotein cholesterol
- mg:
-
milligram
- NCEP:
-
National Cholesterol Education Program
- PSE:
-
plant sterol esters
- TC:
-
total cholesterol
- TG:
-
triglycerides
References
Piironen V, Lindsay DG, Miettinen TA, Toivo J, Lampi AM: Plant sterols: biosynthesis, biological function and their importance to human nutrition. J Sci Food Agric. 2000, 80: 939-966. 10.1002/(SICI)1097-0010(20000515)80:7<939::AID-JSFA644>3.0.CO;2-C.
Berger A, Jones PJH, Abumweis SS: Plant sterols: factors affecting their efficacy and safety as functional food ingredients. Lipids Health Dis. 2004, 3: 5-24.
Gremaud G, Dalan E, Piguet C, Baumgartner M, Ballabeni P, Decarli B, Leser ME, Berger A, Fay LB: Effects of non-esterified stanols in a liquid emulsion on cholesterol absorption and synthesis in hypercholesterolemic men. Eur J Nutr. 2002, 41: 54-60.
Moreau RA, Whitaker BD, Hicks KB: Phytosterols, phytostanols, and their conjugates in foods: structural diversity, quantitative analysis, and health-promoting uses. Prog Lipid Res. 2002, 41: 457-500.
Ostlund RE: Phytosterols in human nutrition. Ann Rev Nutr. 2002, 22: 533-549. 10.1146/annurev.nutr.22.020702.075220.
Jones PJH, Vanstone CA, Raeini-Sarjaz M, St-Onge MP: Phytosterols in low and non-fat beverages as part of a controlled diet fail to lower plasma lipid levels. J Lipid Res. 2003, 44: 1713-1719.
McPherson TB, Ostlund RE, Goldberg AC, Bateman JH, Schimmoeller L, Spilburg CA: Phytostanol tablets reduce human LDL-cholesterol. J Pharm Pharmacol. 2005, 57: 889-96.
Goldberg AC, Ostlund RE, Bateman JH, Schimmoeller L, McPherson TB, Spilburg CA: Effect of plant stanol tablets on low-density lipoprotein cholesterol lowering in patients on statin drugs. Am J Cardiol. 2006, 97: 376-9.
Ostlund R, Spilburg CA, Stenson WF: Sitostanol administered in lecithin micelles potently reduces cholesterol absorption in humans. Am J Clin Nutr. 1999, 70: 826-831.
Volpe R, Nittynen L, Korpela R, Sirtori C, Bucci A, Fraone N, Pazzucconi F: Effects of yoghurt enriched with plant sterols on serum lipids in patients with moderate hypercholesterolaemia. Br J Nutr. 2001, 86: 233-239.
Doornbos AM, Meynen EM, Duchateau GS, van der Knaap HC, Trautwein EA: Intake occasion affects the serum cholesterol lowering of a plant sterol-enriched single-dose yoghurt drink in mildly hypercholesterolaemic subjects. Eur J Clin Nutr. 2006, 60: 325-33.
Thomsen AB, Hansen HB, Christiansen C, Green H, Berger A: Effect of free plant sterols in low-fat milk on serum lipid profile in hypercholesterolemic subjects. Eur J Clin Nutr. 2004,
Pouteau E, Monnard I, Piguet-Welsch C, Groux MJA, Sagalowicz L, Berger A: Non-esterified plant sterols solubilized in low fat milks inhibit cholesterol absorption: a stable isotope double blind crossover study. Eur J Nutr. 2003, 42: 154-164.
De Graaf J, De Sauvage Nolting PR, Van Dam M, Belsey EM, Kastelein JJ, Pritchard PH, Stalenhoef AF: Consumption of tall oil-derived phytosterols in a chocolate matrix significantly decreases plasma total and low-density lipoprotein-cholesterol levels. Br J Nutr. 2002, 88: 479-488.
Nestel P, Cehun M, Pomeroy S, Abbey M, Weldon G: Cholesterol lowering effects of plant sterol esters and non-esterified stanols in margarine, butter and low-fat foods. Eur J Clin Nutr. 2001, 55: 1084-1090.
Maki KC, Shinnick F, Seeley MA, Veith PE, Quinn LC, Hallissey PJ, Temer A, Davidson MH: Food products containing free tall oil based phytosterols and oat beta-glucan lower serum total and LDL cholesterol in hypercholesterolemic adults. J Nutr. 2003, 133: 808-813.
Law MR, Wald NJ, Thompson SG: By how much and how quickly does reduction in serum cholesterol concentration lower risk of ischaemic heart disease?. Br Med J. 1994, 308: 367-372.
Law MR, Wald NJ, Rudnicka AR: Quantifying effect of statins on low density lipoprotein cholesterol, ischaemic heart disease, and stroke: systematic review and meta analysis. Br Med J. 2003, 326: 1423-1429. 10.1136/bmj.326.7404.1423.
Blair SN, Capuzzi DM, Gottlieb SO, Nguyen T, Morgan JM, Cater NB: Incremental reduction of serum total cholesterol and low-density lipoprotein cholesterol with the addition of plant stanol ester-containing spread to statin therapy. Am J Cardiol. 2000, 86: 46-52.
Simons LA: Additive effect of plant sterol-ester margarine and Cerivastatin in lowering low-density lipoprotein cholesterol in primary hypercholesterolemia. Am J Cardiol. 2002, 90: 737-740.
Manhas A, Farmer JA: Hypolipidemic therapy and cholesterol absorption. Curr Atheroscler Rep. 2004, 6: 89-93.
, : Food Labeling: Health Claims; Plant Sterol/Stanol Esters and Coronary Heart Disease. Interim Final Rule. 2000, 54685-54739.
Denke MA: Lack of efficacy of low dose sitostanol therapy as an adjunct to a cholesterol-lowering diet in men with moderate hypercholesterolemia. Am J Clin Nutr. 1995, 61: 392-396.
Katan MB, Grundy SM, Jones P, Law M, Miettinen T, Paoletti R: Efficacy and safety of plant stanols and sterols in the management of blood cholesterol levels. Mayo Clin Proc. 2003, 78: 965-978.
Hendriks HFJ, Weststrate JA, van Vliet T, Meijer GW: Spreads enriched with three different levels of vegetable oil sterols and the degree of cholesterol lowering in normocholesterolaemic and mildly hypercholesterolaemic subjects. Eur J Clin Nutr. 1999, 53: 319-327.
Maki KC, Davidson MH, Umporowicz DM, Schaefer EJ, Dicklin MR, Ingram KA, Chen S, McNamara JR, Gebhart BW, Ribaya-Mercado JD, Perrone G, Robins SJ, Franke WC: Lipid responses to plant-sterol-enriched reduced-fat spreads incorporated into a National Cholesterol Education Program Step I Diet. Am J Clin Nutr. 2001, 74: 33-43.
Mussner MJ, Parhofer KG, Von Bergmann K, Schwandt P, Broedl U, Otto C: Effects of phytosterol ester-enriched margarine on plasma lipoproteins in mild to moderate hypercholesterolemia are related to basal cholesterol and fat intake. Metabolism. 2002, 51: 189-94.
Hallikainen MA, Sarkkinen ES, Gylling H, Erkkila AT, Uusitupa MI: Comparison of the effects of plant sterol ester and plant stanol ester-enriched margarines in lowering serum cholesterol concentrations in hypercholesterolaemic subjects on a low-fat diet. Eur J Clin Nutr. 2000, 54: 715-25.
Hallikainen MA, Uusitupa MI: Effects of 2 low-fat stanol ester-containing margarines on serum cholesterol concentrations as part of a low-fat diet in hypercholesterolemic subjects. Am J Clin Nutr. 1999, 69: 403-10.
Jones PJ, Ntanios FY, Raeini-Sarjaz M, Vanstone CA: Cholesterol-lowering efficacy of a sitostanol-containing phytosterol mixture with a prudent diet in hyperlipidemic men. Am J Clin Nutr. 1999, 69: 1144-50.
Matvienko OA, Lewis DS, Swanson M, Arndt B, Rainwater DL, Stewart J, Alekel DL: A single daily dose of soybean phytosterols in ground beef decreases serum total cholesterol and LDL cholesterol in young, mildly hypercholesterolemic men. Am J Clin Nutr. 2002, 76: 57-64.
Moruisi KG, Oosthuizen W, Opperman AM: Phytosterols/stanols lower cholesterol concentrations in familial hypercholesterolemic subjects: a systematic review with meta-analysis. J Am Coll Nutr. 2006, 25: 41-8.
Devaraj S, Autret BC, Jialal I: Reduced-calorie orange juice beverage with plant sterols lowers C-reactive protein concentrations and improves the lipid profile in human volunteers. Am J Clin Nutr. 2006, 84: 756-61.
Marinangeli CP, Varady KA, Jones PJ: Plant sterols combined with exercise for the treatment of hypercholesterolemia: overview of independent and synergistic mechanisms of action. J Nutr Biochem. 2006, 17: 217-24.
Varady KA, Houweling AH, Jones PJ: Effect of plant sterols and exercise training on cholesterol absorption and synthesis in previously sedentary hypercholesterolemic subjects. Transl Res. 2007, 149: 22-30.
Pollak OJ: Effect of plant sterols on serum lipids and atherosclerosis. Pharmacol Ther. 1985, 31: 177-208.
Christiansen LI, Lahteenmaki PL, Mannelin MR, Seppanen-Laakso TE, Hiltunen RV, Yliruusi JK: Cholesterol lowering effect of spreads enriched with microcrystalline plant sterols in hypercholesterolemic subjects. Eur J Nutr. 2001, 40: 66-73.
Jones PJ, Raeini-Sarjaz M, Ntanios FY, Vanstone CA, Feng JY, Parsons WE: Modulation of plasma lipid levels and cholesterol kinetics by phytosterol versus phytostanol esters. J Lipid Res. 2000, 41: 697-705.
Mitka M: Biomarkers for coronary heart disease: predictive value or background noise?. JAMA. 2004, 292: 2824-2825.
Jenkins DJA, Kendall CWC, Marchie A, Faulkner DA, Wong JMW, deSouza R, Emam A, Parker TL, Vidgen E, Lapsley KG, Trautwein EA, Josse RG, Leiter LA, Connelly PW: Effects of a dietary portfolio of cholesterol-lowering foods vs lovastatin on serum lipids and C-reactive protein. JAMA. 2003, 290: 502-510.
Neil HAW, Meijer GW, Roe LS: Randmoised controlled trial of use by hypercholesterolaemic patients of a vegetable oil sterol-enriched fat spread. Atherosclerosis. 2001, 156: 329-337.
Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III): Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP). JAMA. 2001, 285: 2486-2497.
Acknowledgements
We thank Johnson City Medical Center hospital for providing in-patient support and lipids analysis; Dr. John Kalbfleisch for performing the power analyses. We thank Christina Weidner from Cognis Deutschland GmbH & Co. KG for extensive literature search and study evaluation. We acknowledge Cognis Corp. for providing test materials and overall sponsorship.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
All authors have read and approved this manuscript. RVA and ZPD do not have competing interests from the sponsor. DJC and DB are research scientists at Cognis Corp. (USA) and Cognis Deutschland GmbH & Co. KG, respectively, who were involved in interpreting the data and preparing the manuscript, but were not involved in conducting the study.
Authors' contributions
RVA established the study design, obtained study funding and contributed to data interpretation. ZPD recruited subjects, completed instrumental analysis and data collection. DJC wrote the manuscript, conducted statistical analysis, contributed to data interpretation and final revision. DB contributed to data interpretation and revised the manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Acuff, R.V., Cai, D.J., Dong, ZP. et al. The lipid lowering effect of plant sterol ester capsules in hypercholesterolemic subjects. Lipids Health Dis 6, 11 (2007). https://doi.org/10.1186/1476-511X-6-11
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1476-511X-6-11