Abstract
Plant sterols are naturally occurring molecules that humanity has evolved with. Herein, we have critically evaluated recent literature pertaining to the myriad of factors affecting efficacy and safety of plant sterols in free and esterified forms. We conclude that properly solubilized 4-desmetyl plant sterols, in ester or free form, in reasonable doses (0.8–1.0 g of equivalents per day) and in various vehicles including natural sources, and as part of a healthy diet and lifestyle, are important dietary components for lowering low density lipoprotein (LDL) cholesterol and maintaining good heart health. In addition to their cholesterol lowering properties, plant sterols possess anti-cancer, anti-inflammatory, anti-atherogenicity, and anti-oxidation activities, and should thus be of clinical importance, even for those individuals without elevated LDL cholesterol. The carotenoid lowering effect of plant sterols should be corrected by increasing intake of food that is rich in carotenoids. In pregnant and lactating women and children, further study is needed to verify the dose required to decrease blood cholesterol without affecting fat-soluble vitamins and carotenoid status.
Similar content being viewed by others
Background
Plant sterols are plant compounds with similar chemical structure and biological functions as cholesterol [1]. Plant sterols contain an extra methyl, ethyl group or double bond. The most abundant plant sterols are sitosterol, campesterol and stigmasterol [2]. The daily dietary intake of plant sterol is 160–400 mg among different populations [3–9]. However, in the earlier stages of human evolution, some 5–7 million years ago, plant sterol intake in Myocene diets would have been considerably higher, up to 1 g/d [10]. Dietary sources include vegetable oils (especially unrefined oils), nuts, seeds and grains [1]. Absorption efficiency for plant sterols in humans is considerably less than that of cholesterol. Percent absorption of the former is 2–5% [11] versus 60% for the latter [12]. Consequently, blood levels of plant sterols in humans are only 0.1–0.14% of cholesterol levels [13]. Due to their structural similarity to cholesterol, plant sterols were first and foremost studied for their cholesterol absorption inhibition properties. In addition to their cholesterol lowering effect, plant sterols may possess anti-cancer [14], anti-atherosclerosis [15, 16], anti-inflammation [17] and anti-oxidation activities [18]. The objective of the present review is to assess the evidence supporting the various physiological effects of plant sterols with emphasis on recent advances in knowledge.
Physiological effects of plant sterols
Cholesterol lowering actions
The cholesterol lowering effect of plant sterols is well documented in the literature. It is now accepted, after much earlier scientific debate and study, that 4-desmethyl plant sterols or stanols, either in their free or esterified form, decrease blood levels of total cholesterol and LDL-cholesterol through reduction of cholesterol absorption. Generally speaking, properly solubilized free sterols and esterified sterols possess similar cholesterol lowering ability [19, 20]. In some studies such comparisons have been flawed because the free sterols were not properly solubilized [21]. Ostlund et al. [22] showed that emulsions of sitostanol, mixed with lecithin containing 0.7 g of sterol, reduced cholesterol absorption considerably, whereas less effect was seen with sitosterol in crystalline form.
This review will focus on the effects of 4-desmethyl sterols, stanols, and esterified forms. Methylated sterols (4α-monomethyl and 4,4-dimethyl) in sources such as shea and M. alpina fungi for example, and those sterols esterified to non-fatty acids such as ferulate (such as the sterols in rice bran oil), may not be equivalent in cholesterol lowering ability compared with the forms present in tall and soybean oils [19, 20, 23–26].
Important issues that remain to be verified regarding the cholesterol lowering effect of plant sterols includes (i) efficacy of low dose of plant sterols, (ii) the effect diet background on plant sterol efficacy, (iii) the efficacy of plant sterols when incorporated in food other than fat spread (iv) the optimal number of plant sterols servings and (v) the relative efficacy of plant sterols among different populations.
Efficacy of low dose of plant sterols
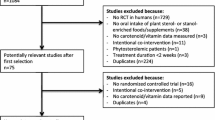
Tables 1 and 2 summarize recent human intervention clinical trials assessing the effects of 4-desmethyl free and esterified plant sterols. Doses of plant sterols reported in literature are often difficult to comprehend, particularly those reported in earlier literature. Herein, all doses refer to free plant sterol equivalent doses. If the contribution of naturally occurring plant sterols in the food vehicle was reported, this is then added to the free plant sterol dose. Ideally, the free plant sterol dose should be calculated experimentally using the average mol% of fatty acids relative to free sterols.
Selected studies 1990–1994
Vanhanen and Miettinen [27] in 1992 found a dose of 0.95 g of sitosterol per day, including the contribution of free sterols present in the canola oil used to prepare the basal spread, probably consumed in 2–3 doses, did not result in reduction in total cholesterol compared to control group. LDL cholesterol typically follows changes in total cholesterol, sometimes being more responsive to plant sterol modulation. Since the control spread contained 0.36 g of rape seed oil derived sterols, a level of consumption by vegetarians, the study is essentially comparing vegetarian levels of consumption of plant sterols to a 3-fold higher level. The conclusion from this study alone would be that a higher dose than 0.95 g of free sterols should be considered to achieve a more consistent and effective lowering of LDL cholesterol levels. In another study with a design similar to that of Vanhanen and Miettinen [27], the absolute reduction in LDL cholesterol was only statistically significant for the sitostanol esters, which showed slightly better efficacy than the free sterols and stanols [28]. The dose of 1.0 g sitosterol reduced cholesterol absorption more effectively than the control spread. This is not surprising because absorption is known to be an extremely sensitive marker that does not necessarily correlate to changes in LDL cholesterol levels [7, 29–31]. Even basal levels of consumption of plant sterol are correlated with cholesterol absorption.
Vanhanen et al [32] showed that in mildly hypercholesterolemic men and women of age 33–60, 1.2 g of free tall stanol equivalents in mayonnaise decreased LDL levels by 7.7%. Relative to starting levels for this group, this reduction was statistically significant, but the absolute lowering of LDL was not statistically significant after accounting for reductions in LDL cholesterol observed with the control group. The lack of statistical significance in LDL lowering is not surprising because the total sample size was only 15 persons, and there was appreciable plant sterol, about 0.4 g, in the control mayonnaise, which probably reduced LDL cholesterol as well. The quantity of plant sterols in the control spread complicates interpretation of results and makes comparisons to other scientific studies more difficult.
Selected studies 1995–1999
Pelletier et al. [33] demonstrated that 0.7 g of soy sterols in spreads fed to 12 normocholesterolemic individuals reduced LDL cholesterol by 15.2% relative to the control. In another study [20], a dose of 0.8 g of soy sterols fed to 76 normocholesterolemic individuals reduced LDL cholesterol by 6.1% relative to the control, and more importantly, did not reduce carotenoids or carotenoids normalized to cholesterol, as reported by Hendriks et al. [19] with a similar dose of soy free sterol equivalents, administered as an ester. The LDL reductions reported by Sierksma et al. [20] were less than that seen in the Pelletier et al. [33] study, which used a similar dosage. The reduction in LDL in the Seerksma study was not seen in all subjects because of the well-known within person LDL variation of 10% [34] or solubilization issues. Nevertheless, this 6% reduction in LDL correlates with a 15% reduction in CHD risk at age 40, and a 6% reduction at age 70 [35] or a 10% reduction [36].
Hendriks et al [19] showed that in men and women with a wide range of ages and starting total cholesterol from low/normal to high, 0.83 g of free soy sterol equivalents in spreads decreased LDL cholesterol 6.2%. Interestingly, 0.83 g was less effective than the two higher doses,1.6 and 3.2 g of sterol equivalents, at reducing LDL cholesterol, but the differences amongst the three doses were not statistically significant. This study thus gives strong indication that a 0.8 g free sterol equivalent dose of plant sterols can efficaciously diminish LDL cholesterol. Nevertheless, the authors concluded that the 1.6 g dosage is most desirable because of the lack of effect on lipid normalized carotene, and the quantitatively greater reduction in LDL cholesterol.
Selected studies 2000–2004
Hallikainen et al. [37] showed that in normal to mildly hypercholesterolemic men and women, 0.8 g of free tall/ vegetable stanol equivalents in spreads decreased LDL non-significantly by only 1.6%. This 0.8 g dose did reduce the number of apo B particles by 8.7%, indicating a reduced number of LDL particles. Similar to Vanhanen et al. [32], the higher dose of 1.6 g of stanol equivalents reduced LDL cholesterol to a greater extent of 6.1%, and two higher doses (2.4 and 3.2 g/d) reduced LDL cholesterol 10.6–11.5%. The three higher doses (1.6–3.2 g/d) lowered LDL cholesterol in a statistically significant manner. A caveat in this study was that the 0.8 g/d dose was given after cholesterol was already lowered by 3 subsequent plant sterol treatments, possibly producing bias against seeing a reduction in LDL cholesterol with 0.8 g/d. Albeit the above experimental weakness, the conclusion would be that the dose of 1.6 g/d of stanol equivalents is a more optimal dose for LDL cholesterol reduction.
Maki et al. [38] administered mildly hypercholesterolemic men and women 1.1 g/d of free tall sterol equivalents in spreads, fed as sterol esters in two doses, which decreased LDL levels by 4.9% while 2.2 g/d of sterol equivalents decreased LDL by 5.4%.
Christiansen et al. [39] reported an 11.3% reduction in LDL cholesterol after 6 months with 1.5 g/d of microcrystalline free sterols in spreads. No additional improvement was seen with 3.0 g/d of plant sterol.
Volpe et al. [40] reported a 6.3% placebo-adjusted decrease in LDL cholesterol after 4 wks with 1.0 g/d and a greater reduction of about 12.2% with 2 g/d after 4 wks. De Graaf et al. [105] found an intake of 1.8 g/d of free sterols in chocolates to decrease LDL cholesterol 8.9% relative to baseline.
Thomsen et al. [42] examined effects of non-esterified, non-hydrogenated, soy bean derived plant sterols, solubilized in a partly vegetable oil filled low fat milk on serum LDL cholesterol in 81 mildly hypercholesterolemic Danish patients, in a double-blind, randomised, placebo-controlled 3-arm cross-over study. Subjects consumed habitual diets, with some restrictions on consumption of fat and cholesterol rich foods. Subjects received 0, 1.2, or 1.6 g/d of sterols in two servings of 250 mL milk for 12 wks (4 wks/dose). The placebo-adjusted mean reduction in LDL was 7.1 ± 12.3 and 9.6 ± 12.4% (mean ± SD) for groups receiving 1.2 and 1.6 g of plant sterols, respectively, with no differences between sexes. There was no statistically significant difference in LDL lowering amongst the 1.2 and 1.6 g/d groups, although Apo B was decreased more with 1.6 than 1.2 g/d of sterols. Apo B is an index of LDL particle number, thus the higher dose may have decreased numbers of LDL particles more than the lower dose. Differences in numbers of small, dense, atherogenic LDL particles and LDL oxidization [43] are other important future parameters to assess. It is noteworthy that there were 20–23% non-responders in the two sterol groups, which was partially consistent with the large differences in cholesterol absorption inhibition observed with similar milk products containing plant sterols [44]. Thus, renewed attention should be given to the issue of non-responders. Another noteworthy observation was the randomization order in which the three milk products affected the magnitude of the LDL lowering results, but not the overall statistical findings. The placebo-adjusted mean percentage decrease in LDL was more pronounced with certain randomixation sequences compared to others. This consideration is typically ignored in reporting results of plant sterol clinical trials examining cholesterol lowering efficacy.
In a very recent study still in press [45], 72 men and women aged 20–73 received two 8 ounce servings of Minute Maid brand non-fat orange juice with breakfast and dinner meals, providing 2 g/d of Cargill CoroWise plant sterols for 8 wks. LDL was reduced 12.4% compared to baseline and placebo; HDL and triacylglycerol levels were not changed. The authors speculate that the fat in the meals may help to emulsify the plant sterols in the orange juice.
Effects of naturally occurring plant sterols
The effects of naturally-occurring plant sterols on cholesterol metabolism have also been studied in both older and more recent literature. It was reported that the differences between effects of different plant oils on blood lipid profiles may be related to their content of plant sterols [46–49]. Indeed, there has been renewed interest in the cholesterol lowering properties of speciality grains and unprocesses oils rich in plant sterols including amaranth oil [50, 51], rice bran oil [52] (Berger et al., submitted), avocado oil [53], extra virgin olive oil [54], macadamian nut [55], and argan oil [56].
Ostlund et al. [49] showed that doses as low as 150–300 mg of naturally present corn oil-derived phytosterols can reduce dietary cholesterol absorption. Also, it was shown that the consumption of original wheat germ, which contains about 328 mg plant sterols, reduced the cholesterol absorption by 42.8 % compared to plant sterol-free wheat germ [57]. These results indicate that naturally available plant sterols are biologically effective as plant sterol supplementation in reducing cholesterol absorption, and that natural plant sterols have important effects on cholesterol metabolism [57].
Summary of biologically active dose of plant sterols for optimal cholesterol lowering
Several studies [19, 20, 28, 32, 33, 40, 58] using intakes of 800–1000 mg of plant sterols per day have shown biologically/clinically significant (5% or more) reductions in LDL cholesterol levels, relative to control, or at least showed a statistically significant treatment effect relative to the starting LDL cholesterol level at the beginning of the treatment period, independent of control. Other studies [27, 37] with a similar dosage range did not meet the above criteria for biological reduction of LDL levels, or achieve statistical significance. Some studies showed that 800–1000 mg/d of free plant sterol equivalents can decrease the absorption of cholesterol, which is indicative, but not necessarily predictive, of actual LDL cholesterol lowering [22, 28, 32, 59].
It has been shown that increasing the dosage beyond 1000 mg per day of free sterol equivalents increased LDL cholesterol lowering efficacy or consistency of response leading to more statistically significant results [32, 37, 40]. Increasing the dosage beyond 1000 mg per day of free sterol equivalents did not further increase LDL cholesterol lowering efficacy [19].
In humans, there is a good likelihood that a dose of 0.8–1.0 g of free sterol equivalents per day, properly solubilized, administered in 2–3 servings with a meal, will reduce LDL cholesterol by 5% or more and that this reduction in LDL cholesterol will correlate with an approximate 6–10% reduction in CHD risk at age 70 [35, 36]. However, at this dosage level, it is likely that not all individuals will achieve a 5% reduction in LDL cholesterol [20].
Clinical relevance of LDL-cholesterol-lowering by plant sterols
As previously noted, it is generally agreed that high blood cholesterol level (especially LDL cholesterol) is a risk factor for coronary heart disease (CHD). Oxidation of excess LDL cholesterol leads to arterial wall plaque build up, which then restricts blood flow and increases blood pressure. Unless, hypercholesterolemia and hypertension are treated, these factors are associated with increased risk of coronary heart disease (myocardial infarction) and stroke [35].
Therefore, the clinical relevance of LDL-cholesterol lowering lies in the potential for plant sterols to reduce the actual risk of CHD. As already described, there is an impressive body of scientific data demonstrating cholesterol-lowering by plant sterols. However, it is pertinent to tease out from published studies, those providing the highest level of evidence for a clinically-important effect. Two reviews have addressed this issue [60, 61]. Law [60] estimated that consumption of 2 g of equivalents of plant sterol or stanol per day would reduce heart disease risk 25%. But only a randomized clinical trial using CHD as an endpoint, could provide certainty of the effectiveness of plant sterols in reducing heart disease incidence. But for a clinical trial to detect a 12–20% reduction in coronary heart disease incidence would require 10,000–15,000 patients with CHD (and more for healthy people). Even if such a trial were feasible, it would probably still be underpowered to detect any rare adverse events (undesirable side effects) [61]. Thus, we must judge the effectiveness of plant sterol doses on their theorized ability to reduce CHD incidence, using LDL cholesterol as a marker.
Low fat versus high fat background diet
Dietary cholesterol consumption is 250–500 mg/d, and normally half is absorbed, while bilary cholesterol production is 600–1000 mg/d. Since plant sterols impair the absorption of both bilary and dietary cholesterol, it is not surprising that they are effective even when consumed in low fat diets [62, 63], although evidence from some studies suggests them to be more effective when consumed with diets containing cholesterol [21, 64, 65]. In a study by Denke [21], plant stanols were given in capsules and not blended with fatty matrix, which limits their cholesterol-lowering action. In addition, compliance was monitored by capsule counting and not by direct supervision, which decreased compliance monitoring. Mussner et al. [65] found esterified phytosterols in spreads to reduce LDL cholesterol about 5.4%, but the reduction was 11.6% in those tertiles having the highest intake of dietary cholesterol. Recent studies have shown plant sterols to be effective even if consumed with Step I diets [38, 40, 66]. Similarly, Judd et al. [67] showed that high doses of vegetable oil sterol esters lowered LDL cholesterol to about the same level, whether the basal diet was a typical American diet or a Step I type of diet, suggesting dramatic changes in usual fat intake are not necessary, if plant sterols are consumed concurrently.
Vehicle for delivering plant sterol
Most clinical trials have been conducted using plant sterols or stanols added to spreads. As long as plant sterols are consumed with a meal to stimulate biliary flow, they can effectively lower LDL cholesterol on the background of various types of basal diets and food vehicles. Plant sterols are efficacious when consumed in: oil: water emulsions [68, 69]; water as lecithin micelles [22]; yogurt [40, 70]; low fat filled milks [42, 44, 71]; chocolate [105]; cereal; snack bars, breads, and beverages [66, 72]; and beef/hamburger [73, 74]. Efficacy of a soy stanol-lecithin powder in reducing cholesterol absorption and LDL-C has been evaluated in a randomized, double-blind parallel study [75]. The subjects who followed a Step I diet consumed soy stanol-lecithin powder in a beverage. The provided daily dose of plant stanols was 1.9 g. The reductions in blood cholesterol and LDL cholesterol were 10.1 and 14.4%, respectively. In another group of subjects, cholesterol absorption was measured using 625 mg stanols provided in beverage or egg whites. Stanol-lecithin reduced cholesterol absorption by 32.1% and 38.2 % when consumed in beverage and egg white, respectively.
The reduction in LDL cholesterol reported, using the previous different vehicles, ranged between 7–14 %, which is close to the reduction in LDL cholesterol reported in studies that used fat spread as a vehicle for delivering plant sterol [25, 37, 76–82]. A recent controlled clinical trial has shown that the intake of plant sterols provided in low-fat and non-fat beverages did not affect lipid profiles in moderately hypercholesterolemic individuals [83]. The finding of this study was contrary to the findings of other studies reporting that plant sterols were effective in reducing blood cholesterol even when incorporated into low-fat or non-fat foods [40, 42, 44, 70, 72]. This discrepancy may be related to the fact that the plant sterols must be added to the low or non fat food matrix in such a way that the plant sterols solubilize, or remain as small crystals over time. In products such as milk, the milk fat globule membrane components may enhance the absorption of cholesterol [44, 68, 69], but also aid in solubilization. Pouteau et al. [44] described a rapid filtration and detection method to quantify plant sterol crystals. The authors also used light scattering techniques to quantify the size of the crystals as a function of storage time of the milk products. The method of dispersion, processing, and use of emulsifiers, surfactants, and crystal habit modifiers will affect the success of plant sterols in non-spread vehicles [42, 44, 71, 84, 85].
Commercially, plant sterols are currently contained in bars (Logicol-Australia, Benecol-UK), vegetable oils (Ekona-Japan; NutraLease Canola Active-Israel), orange juice (Minute Maid Heart Wise containing Cargill CoroWise plant sterols) [45], mayonnaises (Logicol-Australia), milk (Benecol-UK, Logicol-Australia, SereCol-Argentenia), yogurt (Logicol-Australia; Benecol-UK), yogurt drinks (Benecol), soy milk (Pacific Foods), meat and soups (Raisio-Finland), and green teas (Chol zero, Korea). Plant sterols are also being sold or developed mixed with other functional ingredients such as: fiber (Unilever Fruit D'or-France); healthy oils (Benecol Olive Spread-UK); non-absorbable diacylglycerol (Kao-ADM Econa Healthy Cooking Oil; Enzymotec MultOil Platform, ArteriCare products, Israel); almonds, soy protein and viscous fibers [86]; and minerals [87–89]. There is also interest to combine plant sterols with antioxidants, such as flavonoids, quercetins, and catechin; and a spice mixture developed by Selako, and marketed as Flavomare in Scandanavia. It is only a matter of time before ingredients such as conjugated linoleic acid (CLA) are mixed with plant sterols in various vehicles (e.g., Clarinol's CLA has received GRAS status for addition to milks, yogurts, bars, etc.).
Various manufacturers also sell plant sterols in supplement form, and there is interest to develop plant sterols as drugs (e.g., Forbes' FM-VP4 drug candidate). Plant sterols may also be combined with other drugs that lower cholesterol through different mechanisms of action, including statins and ezetimibe [90, 91]. Recent evidence suggests that patients who had previous actue coronary syndrome benefited from aggressive LDL lowering with statins to levels subtstantially below current target levels [92, 93]. This finding provides enthusiasm for developing novel plant sterol-drug and drug-drug combined strategies to aggressively lower LDL cholesterol in some populations. Despite evidence that plant sterols can effectively reduce LDL cholesterol and inhibit cholesterol absorption in vehicles other than spread type vehicles, regulatory agencies have been slow to accept plant sterols in foods other than spreads in some countries such as the USA [94] and Australia [95]. Rigorous efforts underway by food companies and other highly respected organizations to allow claims for plant sterols in foods other than spreads.
Optimal number of servings
It has been suggested that plant sterols should be consumed at each cholesterol containing meal to achieve an optimal effect. A daily intake of 2.5 g plant stanol esters, either consumed once per day at lunch, or divided over three portions resulted in a similar decrease in serum total and LDL cholesterol levels [96]. Similar efficacy with a single larger dose sterol esters has also been demonstrated in two additional studies [73]. A single serving of yogurt, providing 1 g of pure free sterols, resulted in a placebo-adjusted reduction in LDL cholesterol of 6.3% [40]. Consumption of a single dose of 2.4 g/d plant sterols resulted in a 9.3 and 14.6 % reductions in blood total and LDL cholesterol levels, respectively, in hypercholesterolemic individuals [73]. Single doses of plant sterols may have sustained effects on cholesterol absorption via interactions with intestinal proteins (see Section 3.1.5.1 for details).
Nevertheless, as there are a plethora of studies showing the efficacy of plant sterols distributed in 2–3 meals [19, 25, 37, 38, 70, 76–82, 97–100], and only two studies to date demonstrating efficacy with a single larger serving [73, 96], it seems prudent to remain consistent with the more established, conservative recommendation of consuming plant sterols in 2–3 doses with food, as adopted by the United States FDA.
Population under study
Plant sterol for the adult population
Typically, cholesterol lowering properties of plant sterols are similar in both men and women, although recent studies highlight that plant sterols can diminish fat soluble vitamins only in women[37]. Mixed gender studies must possess the statistical power to separate men and women as a statistical covariant, otherwise, the researcher must assume an identical response across both sexes.
The recent study of Matvienko et al. [73] demonstrates that soy sterol esters can effectively decrease LDL cholesterol in young adults of age 23, suggesting age is not a very critical variable influencing LDL cholesterol lowering properties of plant sterols, as also confirmed in studies with children [101]. In contrast, the meta-analysis of Law [60] predicted that plant sterol and stanol esters would reduce LDL cholesterol more effectively at each dose in older compared with younger people. However, it should be taken into consideration that older people had higher starting circulating lipid levels, so the percent change did not differ across age ranges. A number of studies have shown that plant sterols effectively reduce blood cholesterol in normocholesterolemic [19, 22, 25, 37, 59, 76, 96, 102, 103], hypercholesterolemic subjects [37, 38, 40, 62, 72, 73, 76, 77, 80, 97, 104–106], subjects with familial hypercholesterolemia [78, 100], and in type II diabetic hypercholesterolemic patients [107, 108]. Further, in a type II diabetic population consuming statin, plant sterols had a combined effect on lowering LDL cholesterol an additional 27%, the combined effect being 44% [108]. The reduction in LDL cholesterol seems to be greater in hypercholesterolemic individuals with type II diabetes. Plant sterols decreased LDL cholesterol in hypercholesterolemic individuals with and without type II diabetes by 14.9 % and 29.8 %, respectively (Lau et al. unpublished data).
Plant sterols are not recommended for pregnant or lactating women. However, there has not been a systematic study testing this issue. Vegetarian women habitually consume up to 500 mg of plant sterols per day. There is no evidence that such women cannot have normal pregnancies. Certain ethnic groups are known to have high levels of plant sterol intake and their pregnancy outcome could be evaluated in future studies. For example, in 372 semiacculturated Tarahumara Indians in the Sierra Madre Occidental Mountains of Mexico, the diet was found to be high in fiber and to contain less than 100 mg/day of cholesterol and over 400 mg/day of plant sterols [4]. Further, in the earlier stages of human evolution, some 5–7 million years ago, plant sterol intake in Myocene diets would have been considerably higher, up to 1 g/d [10]. Such diets were not only rich in plant sterols, but also dietary fiber, vegetable protein, and associated phytochemicals; but low in saturated and trans-fatty acids [10]. To meet the body's needs for cholesterol, genetic differences and polymorphisms were conserved by evolution, tending to raise serum cholesterol levels.
Plant sterols likely interact with ATP-binding cassette (ABC) transport proteins to direct cholesterol back into the intestinal lumen, regulating absorption of cholesterol and plant sterols [109–113]. Plat and Mensink [114] first hypothesized that plant sterols increased the expression of ABCA1. Thereafter, based on an animal study, it was suggested that plant sterols are converted into a liver X receptor (LXR) agonist, which activates the expression of ABC proteins [115]. Mutations in ABC proteins are responsible for the rare disease sitosterolemia [116]; and polymorphisms of ABC proteins may affect cholesterol absorption based on a preliminary study [117]. Polymorphism of ABCG8 gene was found to contribute to blood plant sterol levels in healthy subjects [118] suggesting ABCG8 protein regulates non-cholesterol sterol absorption.
Apolipoprotein E phenotype was originally shown to be correlated with cholesterol absorption [119]. It was shown in one study [120] but not others [37, 99] to affect plant sterol cholesterol lowering efficacy in recent trials.
In addition to the above proteins, cholesterol absorption is likely controlled by additional proteins [121], as well a putative sterol transporter system [122]. In this context, the genotype of apolipoprotein A-IV, scavenger receptor-BI, 3-hydroxy-3-methyl-coenzyme A reductase, apolipoprotein E, and cholesterol ester transfer did not affect cholesterol lowering effects of plant stanol [122].
Plant sterols for children
Plant sterols are not recommended for normocholesterolemic children under five because children who are growing have a large need for cholesterol for normal development. There is also the fear that plant sterols, particularly esters, could affect the absorption of fat soluble vitamins. However, no direct evidence points at plant sterols being in some way dangerous for children. Studies with small amounts of plant sterols fed to infants have shown that neonates have the adaptive ability to increase their cholesterol synthesis [123–125]. In fact, infants are typically fed formula diets containing cholesterol concentrations 3–35 times lower than breast milk, with considerably higher levels of plant sterols [126]. There is the possibility that cholesterol, received in utero or administered to neonates, could affect gene expression and physiology later in life. This theory was initially based on the increased atherosclerosis incidence in adults fed formula rather than breast milk as infants [127], as well as higher cholesterol in men fed breast milk for less than 3 months as compared to more than 9 months [128]. This so called "cholesterol imprinting" hypothesis is now being explored in controlled animal models with microarrays [129]. Children with allergies to dairy routinely consume vegetable oils rich in plant sterols and less cholesterol, and thus have less cholesterol absorbed, but compensatory increases in cholesterol synthesis [130].
Most studies examining the effects of plant sterols in children have been conducted with hypercholesterolemic children [131–134]. Generally, plant sterols seem to be as effective in hypercholesterolemic children as in hypercholesterolemic adults. Some older studies in children must be interpreted with caution, as the preparations may have been crystalline [135]. Becker [132], for example, found that severely hypercholesterolemic children could be effectively treated with sitosterol, and that 3 g/d sitosterol combined with a half dose of bezafibrate was an effective way to reduce the bezafibrate dose. Intake of 1.7 g/d of plant sterols in ester form was effective in reducing total cholesterol levels, LDL cholesterol and apo B levels in children with familial hypercholesterolemia who followed Step I diet without any adverse effects [136]. No changes in concentration of lipid-adjusted carotenoids were reported except for lycopene, which decreased by 8.1%. This decrease was considered of minor biological and clinical importance[136]. The authors recommended an increase in the intake of fruit and vegetables to avoid the reduction in lycopene values when plant sterols were introduced to Step I diet of children with familial hypercholesterolemia.
In a crossover study, healthy 2–5 year old children consumed either 3 g/d plant stanol ester or 5 g/d insoluble wheat bran fiber for 2 weeks, then 10 g/d for the second two weeks [101]. Relative to baseline, LDL cholesterol levels were reduced 15.5% with stanol esters and 4% with the fiber diet. Stanol esters did not affect triacylglycerols or HDL cholesterol. The study showed that stanol esters reduced LDL cholesterol in normocholesterolemic children similarly to that found in normocholesterolemic adults and hypercholesterolemic adults and children. In healthy 6-year-old children who were on a low-saturated, low-cholesterol diet, daily intake of 1.5 g/d of plant stanol ester was effective in reducing total cholesterol and LDL cholesterol values by 5.4% and 7.5%, respectively [137]. The intake of plant stanol did not cause any adverse clinical effects, nor did it affect the levels of fat soluble vitamins; however, it did cause a 19% reduction in ratio of β-carotene to LDL cholesterol ratio.
Children consuming vegetable oil sterols in margarine for 13 months had serum concentrations of campesterol and sitosterol that were 75% and 44% higher than those in the control children, while serum cholesterol precursor sterol concentrations, indicative of cholesterol synthesis, did not differ between the two groups [138]. Thus, doubling dietary plant sterol intake almost doubles serum plant sterol concentrations in 13-mo-old children, but has no effect on endogenous cholesterol synthesis. Relative intestinal absorption of natural plant sterols from the diet in early childhood is similar to that in adults. In the older study of Mellies et al. [139], 300–900 mg/d of plant sterols led to a large accumulation of plant sterols in the plasma (0.44 mM) of normo and hypercholesterolemic children.
As in adults, in children, the apo E phenotype, could be a factor affecting the efficacy of plant sterols. Plant sterols, as an index of cholesterol absorption, were higher in adults or children with the E4/3 phenotype as compared with those with other phenotypes [140]. Lathosterol, an index of cholesterol synthesis, was also higher in children with E4/3 phenotype than in those with E3/3 or E3/2, indicating these children both absorb and synthesize more cholesterol [140]. The effect of phenotype of apo E on response to sterol intake was investigated in 6-year-old children [141]. Daily intake of 1.6 g of plant stanol was effective in reducing blood cholesterol and LDL cholesterol by 65 and 8%, respectively, in these children regardless of apo E phenotype. Thus, children with different apo E phenotype can achieve a reduction in their cholesterol levels by intake of plant sterol.
From the previous studies, it is clear that plant sterols are effective in reducing blood cholesterol in healthy as well as in hypercholesterolemic children. The only side effect reported is a reduction in levels in ratio of β-carotene to LDL cholesterol ratio and lycopene values, which could be balanced by increasing the intake of fruit and vegetable, especially those rich in carotenoids, as was the case in adult population [106].
Plant sterol intake and sitosterolemia
Sitosterolemia is a rare autosomal recessively inherited disorder which results from absorption of high amounts of plant sterol and cholesterol for unclear reasons linked to a locus at chromosome 2p21 [142–144] leading to development of coronary heart disease at young age, and development of tendon xanthomatosis. Various candidate genes involved in cholesterol absorption have been excluded at present [145]. Sitosterolemic persons should avoid food products containing plant sterols. Hydrogenated plant sterols may be safer than non-hydrogenated plant sterols for this population because the former is less absorbed, however, this argument is speculative. A recent study found that heterozygous subjects for sitosterolemia who received sterol esters in a spread providing 3.3 g of free sterol equivalents for 4 weeks, had a 10.6% reduction in LDL cholesterol [146]. Levels of campesterol and sitosterol were increased, but the magnitude of the increase was not much greater than that observed in normal subjects consuming similar spreads. In another recent study in 12 subjects who were obligate heterozygotes for sitosterolemia, consumption of plant sterol ester for 6 weeks resulted in an additional significant reduction of 5.9% in LDL cholesterol over that provided by a Step I diet alone, but no additional significant reduction was found after consumption of plant sterol ester for 12 weeks [147]. Although plasma levels of plant sterols concentration were elevated, the increase was similar to that reported in normal and mildly hypercholesterolemic subjects who consumed plant sterol esters [147]. The increase in plasma levels of plant sterols reached a plateau, which indicates that obligate heterozygotes eliminated the plant sterols from their body in order to prevent their accumulation. For prudency, it is nevertheless recommended that persons with sitosterolemia avoid plant sterols.
Anti-atherogenicity activity
In vitro studies have shown that plant sterols are effective in preventing hyperproliferation of vascular smooth muscle cell that play a role in atherosclerosis development [148]. Animal studies have shown that plant sterols also have anti-atherogenicity activity. In rabbits, sitosatanol feeding decreased plaque accumulation in coronary arteries within the ascending aorta [149]. Feeding plant sterols to apo E-deficient mice decreased platelet counts as well as the susceptibility of red blood cells to hemolysis, decreased plasma fibrinogen [16], and decreased formation of atherosclerotic lesions [15, 16, 150]. In healthy subjects who consumed 4 g/d of wood based stanol ester, the activity of antithrombin-III tended to increase compared to control group [99]. Thus, plant sterols may reduce atherosclerosis development not only by reducing blood cholesterol levels but also by possessing anti-atherogenicity activity.
Anti-cancer activity
The action of plant sterols as anticancer dietary components has been recently extensively reviewed [151]. Plant sterols can suppress tumor cell growth (LNCaP and HT-29) [152, 153]. Compared to cholesterol, β-sitosterol caused a 24% decrease in cell growth and a 4-fold increase in apoptosis. In the latter work, the authors were interested in the effects of β-sitosterol on the sphingomyelin cycle, and measured two keys enzymes: protein phosphatase 2A (PP 2A) and phospholipase D (PLD). A 50% increase was observed in PP 2A activity in media containing 16 μM of β-sitosterol; however, there were no changes in protein levels of PP 2A. PLD activity increased in presence of phorbol myristate and β-sitosterol. This study suggests that the sphingomyelin cycle, which increases cell apoptosis, is mediated by PLD, PP 2A, and possibly, incorporation of β-sitosterol into the membrane. Another possible mechanism by which β-sitosterol can protect against cancer is through down-regulation of cholesterol synthesis, as was found in MDA-MB-231 human breast cancer cells [14]. In an important in vivo study, SCID mice were xenografted with the human breast cancer cell line MDA-MB-231 [154]. Plant sterol-fed mice had a 33% smaller tumor size and 20% less metastases in lymph nodes and lungs than cholesterol-fed mice. This finding implied the possibility that plant sterols may retard the growth and spread of breast cancer cells. In addition to retarding the growth of breast cancer cells by plant sterols, there is some evidence that plant sterols can affect the development of prostate cancer [155]. In a meta-analysis, 519 men were studied in 4 randomized, placebo-controlled, double-blind trials. β-sitosterol improved urinary symptom scores and flow measures, suggesting that non-glucosidic forms of β-sitosterol improve urinary symptoms and flow measures. Long term effectiveness, safety, and ability to prevent benign prostatic hyperplasia complications are not known [155]. In another recent study, there was no evidence that plant sterol usage at dose of 300 mg/d, decreased risk of colon and rectal cancers [156]. A similar conclusion was reached following a rat study in which rats were given the carcinogen methyl-nitroso-urea and then monitored for tumor development [157].
Plant sterols have also been found to have a protective effect against lung cancer [158]. In this study, intake of about 144 mg/d of plant sterols was associated with reduction in risk for lung cancer even after controlling of confounding factors, i.e. tobacco smoking, vegetables, fruits, and antioxidant substances. Total dietary plant sterol intake was found to be inversely associated with breast [159]), stomach [160], and esophageal [161] cancers. It was found that women with highest quartiles of total dietary intakes of plant sterols (>122 mg/d) had reduced risk of endometrial cancer [162], and intake of more than 521 mg/d reduced risk of ovarian cancer [163]. On the other hand, in a prospective epidemiological study, high dietary intake was not associated with reduced risk of colon and rectal cancers [156]. However, the intake of plant sterol might reduce the risk of more than one type of cancer.
Anti-inflammation activity of plant sterols
Bouic [17] and Bouic et al [164] have reviewed the possible roles of phytosterols in the etiology or preventive role of phytosterols in various diseases and conditions, including proliferative responses of lymphocytes, pulmonary tuberculosis, feline immunodeficiency virus and HIV, stress induced immune suppression, rheumatoid arthritis, and allergic rhinitis/sinusitis. The mechanisms by which plant sterols display their anti-inflammatory activity are thought to include inhibition of secretion of inflammatory mediators such as interleukin-6, and tumor necrosis factor-α by monocytes [17]. Most of the work has been conducted with animals. From these provocative results, it is not unlikely that plant sterols will be further used for purposes related to control of deveopment and spread of certain cancers in humans.
Anti-oxidant activity
Another possible effect of plant sterols is their antioxidant activity [165]. It was found that the methanol extract of soybean oil, which has a strong in-vitro protective effect against DNA damage in human endothelial cell, contains phytosterols in addition to tocopherols and n-3 polyunsaturated fatty acids (PUFA). Results suggest that the antioxidant activity of soybean oil may be in part related to sterol content. Moreover, in in-vitro conditions, sitosterol, and sitosterol glucoside were found to decrease lipid peroxidation of platelet membranes in the presence of iron [18] and in healthy human subjects a 2 and 3-g dose of stanol ester reduced oxidized LDL-C levels [82]. The authors suggested that the intake of stanol ester might protect LDL particles from oxidation. Thus, based on results from in vitro studies and on human study, there is a possibility that plant sterols may possess antioxidant properties. Such antioxidant protection could also benefit atherosclerosis [166] and cancer [167] disease state.
Anti-ulcer activity
In a recent study, phytosterol esters, but not sterols, in horse gram (an herb in the genus Dolichos cultivated in India for food and fodder) were protective in a pyloric ligation model of ulcer, whereas sterols were protective in acute ulcer models using ethanol-induced and cysteamine-induced ulceration [168]. Phospholipids were protective in both types of model. Thus, the presence of sterols, sterol esters, and phospholipids in food lipids in staple diets may account for the low prevalence of duodenal ulcer in certain geographical areas, despite a uniformly high prevalence of Helicobacter pylori infection.
Anti-fungal activity
Another area for future investigation is the anti-fungal activity of plant sterols and related triterpenes [169]. In this work, the anti-fungal activity of triterpenes in the mushroom species Ganoderma annulare was demonstrated.
Safety
It has been concluded that plant sterols, within the range that causes desirable reduction in blood levels of total cholesterol and LDL-cholesterol, are clinically safe. This conclusion has been reported in short-term studies [19, 39, 40, 170] as well as in long-term study that lasted for 1 year [81]. Since plant sterols decrease the absorption of cholesterol, they might also affect the absorption of fat-soluble vitamins. The scientific evidence for the impact of phytosterols on carotenoid status and fat soluble vitamins is summarized in Table 3. The effect of plant sterols on the blood levels of precursors of fat-soluble vitamins is a controversial issue. In some studies, plant sterols consumption has been shown to significantly reduce levels of carotenoids [25, 37, 38, 81, 170, 171], tocopherol [37], and lycopene [25, 38]. Other studies reported that the consumption of plant sterols does not affect blood levels of carotenoids [39, 72, 104, 172], tocopherol [19, 39, 173], and lycopene [19, 173].
In a recent trial comparing equal free sterol equivalent amounts (2.2 g/d) of esterified sterols and free sterols in milk, both forms of sterols decreased the absorption of β-carotene and α-tocopherol in normocholesterolemic men. The reduction in β-carotene bioavailability was significantly less pronounced with free plant sterols than with plant sterol esters However, there was no difference in cholesterol absorption between the two forms of plant sterols. [71]. Esters are presumed to have more of an effect on fat soluble vitamins because they partition into the oil phase of the intestine, whereas free sterol would partition into the micellar phase [174].
During plant sterol consumption, increasing the consumption of fruits and vegetables to be > five servings and including one or more carotenoid rich source would be enough to avoid reduction in carotenoid levels resulted from plant sterol intake [106].
Conclusions
Based on the positive results from studies examining the effects of low doses of free plant sterols and sterol esters, there is a good likelihood that a minimum dose of 0.8–1.0 g of free sterol and free sterol equivalents will reduce LDL cholesterol by 5% or more, and that this reduction in LDL cholesterol will correlate with an approximate 6–10% reduction in coronary heart disease risk at age 70 [35, 36]. There is also a good likelihood that the reduction in LDL cholesterol within this same dosage could be higher if full compliance of the plant sterol dosage were assured. In studies where subjects were monitored to ensure full compliance, efficacy with a 1.5 to 2 g/d dose ranged from 12–16%. For maximum efficacy of free plant sterols, the plant sterols must be administered in a soluble or microcrystalline form. Efforts must be taken to assure that the free plants sterols remain in this bio-efficacious form during the shelf life of the product. Our dosage recommendation of 0.8–1.0 g of free sterol and free sterol equivalents compares favorably with the FDA interim final rule 21 CFR 101.83 recommending 0.65 g of sterol esters per serving, twice per day in spreads, which is equivalent to 0.8 g of free sterol equivalents per day. As of January 2003, the FDA recognized that the scientific literature supports expanding the health claim to include free forms of plant sterols and stanols, and to include a wider range of products, including low-fat products. The FDA further stated that the science (as of January 2003) shows that the lowest effective daily intake of free phytosterols is 800 mg/d http://vm.cfsan.fda.gov/~dms/ds-ltr30.html.
In addition to their cholesterol lowering properties, plant sterols have other promising effects, including anti-cancer, anti-inflammation, anti-atherogenicity, and anti-oxidation activities. Despite the fact that plant sterols reduce the carotenoid levels in adults, it seems that an intake of plant sterols between 0.8–1.0 g is essential to prevent chronic diseases in adult population. The carotenoid lowering effect of plant sterols can be corrected by increasing intake of food that is rich in carotenoids. However, more studies are needed in pregnant and lactating women as well as on children in order to verify the dose required to decrease blood cholesterol without affecting fat-soluble vitamins and carotenoid status.
Plant sterols are naturally occurring molecules that humanity has evolved with, which partially counter the absorption of dietary cholesterol and have other important biological functions described above. The myriad of factors that can affect the efficacy of plant sterols have been explored. The resonating conclusion is that properly solubilized 4-desmetyl plant sterols, in ester or free form, in reasonable doses (0.8–1.0 g of equivalents per day) and in various vehicles including natural sources, and as part of a healthy diet and lifestyle, are important dietary components for maintaining good heart health. Consumption from natural sources should be encouraged for all persons, and consumption of plant sterols in enriched sources should be encouraged following consultation with a clinician. The clinician should be assured that the individual is a responder to plant sterols, and achieves a reduction in LDL cholesterol. Along these lines, it would be fruitful to monitor individuals for markers of cholesterol absorption before recommending consumption of enriched plant sterols. Those persons who are poor absorbers of dietary cholesterol (on the basis of low levels of serum cholestanol and plant sterols) [175] may not be ideal candidates for consuming plant sterols to lower plasma LDL cholesterol, but may still benefit from plant sterols' other positive effects.
Abbreviations
- ABC:
-
ATP-binding cassette
- apo:
-
apolipoprotein
- LDL:
-
Low density lipoprotein
- PLD:
-
phospholipase D
- PUFA:
-
polyunsaturated fatty acids.
References
Piironen V, Lindsay DG, Miettinen TA, Toivo J, Lampi A-M: Plant sterols: biosynthesis, biological function and their importance to human nutrition. J Sci Food Agric. 2000, 80: 939-966. 10.1002/(SICI)1097-0010(20000515)80:7<939::AID-JSFA644>3.3.CO;2-3. 10.1002/(SICI)1097-0010(20000515)80:7<939::AID-JSFA644>3.3.CO;2-3
Moreau R, Whitaker B, Hicks K: Phytosterols, phytostanols, and their conjugates in foods: structural diversity, quantitative analysis, and health-promoting uses. Prog Lipid Res. 2002, 41: 457- 10.1016/S0163-7827(02)00006-1
Ahrens EH Jr, Boucher CA: The composition of a simulated American diet. J Am Diet Assoc. 1978, 73: 613-620.
Cerqueira MT, Fry MM, Connor WE: The food and nutrient intakes of the Tarahumara Indians of Mexico. Am J Clin Nutr. 1979, 32: 905-915.
Nair PP, Turjman N, Kessie G, Calkins B, Goodman GT, Davidovitz H, Nimmagadda G: Diet, nutrition intake, and metabolism in populations at high and low risk for colon cancer. Dietary cholesterol, beta-sitosterol, and stigmasterol. Am J Clin Nutr. 1984, 40: 927-930.
Hirai K, Shimazu C, Takezoe R, Ozeki Y: Cholesterol, phytosterol and polyunsaturated fatty acid levels in 1982 and 1957 Japanese diets. J Nutr Sci Vitaminol (Tokyo). 1986, 32: 363-372.
Miettinen TA, Tilvis RS, Kesaniemi YA: Serum cholestanol and plant sterol levels in relation to cholesterol metabolism in middle-aged men. Metabolism. 1989, 38: 136-140. 10.1016/0026-0495(89)90252-7
Morton GM, Lee SM, Buss DH, Lawrance P: Intakes and major dietary sources of cholesterol and phytosterols in the British diet. J Hum Nutr Diet. 1995, 8: 429-440.
de Vries JHM, Jansen A, Kromhout D, van de Bovenkamp P, van Staveren WA, Mensink RP, Katan MB: The fatty acid and sterol content of food composites of middle-aged men in seven countries. J Food Comp Anal. 1997, 10: 115-141. 10.1006/jfca.1997.0525. 10.1006/jfca.1997.0525
Jenkins DJ, Kendall CW, Marchie A, Jenkins AL, Connelly PW, Jones PJ, Vuksan V: The Garden of Eden--plant based diets, the genetic drive to conserve cholesterol and its implications for heart disease in the 21st century. Comp Biochem Physiol A Mol Integr Physiol. 2003, 136: 141-151. 10.1016/S1095-6433(02)00345-8
Ostlund R E, Jr, McGill JB, Zeng CM, Covey DF, Stearns J, Stenson WF, Spilburg CA: Gastrointestinal absorption and plasma kinetics of soy Delta(5)-phytosterols and phytostanols in humans. Am J Physiol Endocrinol Metab. 2002, 282: E911-E916.
Bosner MS, Lange LG, Stenson WF, Ostlund Jr RE: Percent cholesterol absorption in normal women and men quantified with dual stable isotopic tracers and negative ion mass spectrometry. J Lipid Res. 1999, 40: 302-308.
Miettinen TA, Tilvis RS, Kesaniemi YA: Serum plant sterols and cholesterol precursors reflect cholesterol absorption and synthesis in volunteers of a randomly selected male population. Am J Epidemiol. 1990, 131: 20-31.
Awad AB, Roy R, Fink CS: Beta-sitosterol, a plant sterol, induces apoptosis and activates key caspases in MDA-MB-231 human breast cancer cells. Oncol Rep. 2003, 10: 497-500.
Moghadasian MH, McManus BM, Pritchard PH, Frohlich JJ: "Tall oil"-derived phytosterols reduce atherosclerosis in ApoE-deficient mice. Arterioscler Thromb Vasc Biol. 1997, 17: 119-126.
Moghadasian MH, McManus BM, Godin DV, Rodrigues B, Frohlich JJ: Proatherogenic and antiatherogenic effects of probucol and phytosterols in apolipoprotein E-deficient mice: possible mechanisms of action. Circulation. 1999, 99: 1733-1739.
Bouic PJ: The role of phytosterols and phytosterolins in immune modulation: a review of the past 10 years. Curr Opin Clin Nutr Metab Care. 2001, 4: 471-475. 10.1097/00075197-200111000-00001
van Rensburg SJ, Daniels WM, van Zyl JM, Taljaard JJ: A comparative study of the effects of cholesterol, beta-sitosterol, beta-sitosterol glucoside, dehydroepiandrosterone sulphate and melatonin on in vitro lipid peroxidation. Metab Brain Dis. 2000, 15: 257-265. 10.1023/A:1011167023695
Hendriks HF, Weststrate JA, van Vliet T, Meijer GW: Spreads enriched with three different levels of vegetable oil sterols and the degree of cholesterol lowering in normocholesterolaemic and mildly hypercholesterolaemic subjects. Eur J Clin Nutr. 1999, 53: 319-327. 10.1038/sj.ejcn.1600728
Sierksma A, Weststate JA, Meijer GW: Spreads enriched with plant sterols, either esterified 4, 4 dimethylsterols or free 4 desmethylsterols, and plasma total and LDL cholesterol concentrations. Br J Nutr. 1999, 82: 273-282.
Denke MA: Lack of efficacy of low-dose sitostanol therapy as an adjunct to a cholesterol-lowering diet in men with moderate hypercholesterolemia. Am J Clin Nutr. 1995, 61: 392-396.
Ostlund RE, Spilburg CA, Stenson WF: Sitostanol administered in lecithin micelles potently reduces cholesterol absorption in humans. Am J Clin Nutr. 1999, 70: 826-831.
Ikeda I, Nakashima-Yoshida K, Sugano M: Effects of cycloartenol on absorption and serum levels of cholesterol in rats. J Nutr Sci Vitaminol. 1985, 31: 375-384.
Kritchevsky D, Tepper SA, Czarnecki SK, Kyle DJ: Effects of 4-methylsterols from algae and of b sitosterol on cholesterol metabolism in rats. Nutr Res. 1999, 19: 1649-1654. 10.1016/S0271-5317(99)00120-7. 10.1016/S0271-5317(99)00120-7
Westrate JA, Meijer GW: Plant sterol-enriched margarines and reduction of plasma total and LDL-cholesterol concentrations in normocholesterolaemic and midly hypercholesterolaemic subjects. Eur J Clin Nutr. 1998, 52: 334-343. 10.1038/sj.ejcn.1600559
Vissers MN, Zock PL, Meijer GW, Katan MB: Effect of plant sterols from rice bran oil and triterpene alcohols from sheanut oil on serum lipoprotein concentrations in humans. Am J Clin Nutr. 2000, 72: 1510-1515.
Vanhanen HT, Miettinen TA: Effects of unsaturated and saturated dietary plant sterols on their serum contents. Clin Chim Acta. 1992, 205: 97-107.
Miettinen TA, Vanhanen H: Dietary sitostanol related to absorption, synthesis and serum level of cholesterol in different apolipoprotein E phenotypes. Atherosclerosis. 1994, 105: 217-226.
Tilvis RS, Miettinen TA: Serum plant sterols and their relation to cholesterol absorption. Am J Clin Nutr. 1986, 43: 92-97.
Miettinen TA, Kesaniemi YA: Cholesterol absorption: regulation of cholesterol synthesis and elimination and within-population variations of serum cholesterol levels. Am J Clin Nutr. 1989, 49: 629-635.
Pouteau E, Piguet-Welsch C, Berger A, Fay LB: Determination of cholesterol absorption in humans: from radiolabel to stable isotope studies. Isotopes Environ Health Stud. 2003, 39: 247-257. 10.1080/10256010310001621155
Vanhanen HT, Kajander J, Lehtovirta H, Miettinen TA: Serum levels, absorption efficiency, faecal elimination and synthesis of cholesterol during increasing doses of dietary sitostanol esters in hypercholesterolaemic subjects. Clin Sci. 1994, 87: 61-67.
Pelletier X, Belbraouet S, Mirabel D, Mordret F, Perrin JL, Pages X, Debry G: A diet moderately enriched in phytosterols lowers plasma cholesterol concentrations in normocholesterolemic humans. Ann Nutr Metab. 1995, 39: 291-295.
Smith SJ, Cooper GR, Myers GL, Sampson EJ: Biological variability in concentrations of serum lipids: sources of variation among results from published studies and composite predicted values. Clin Chem. 1993, 39: 1012-1022.
Law MR, Wald NJ, Thompson SG: By how much and how quickly does reduction in serum cholesterol concentration lower risk of ischaemic heart disease?. BMJ. 1994, 308: 367-372.
Stampfer MJ, Sacks FM, Salvini S, Willett WC, Hennekens CH: A prospective study of cholesterol, apolipoproteins, and the risk of myocardial infarction. N Engl J Med. 1991, 325: 373-381.
Hallikainen MA, Sarkkinen ES, Uusitupa MI: Plant stanol esters affect serum cholesterol concentrations of hypercholesterolemic men and women in a dose-dependent manner. J Nutr. 2000, 130: 767-776.
Maki KC, Davidson MH, Umporowicz DM, Schaefer EJ, Dicklin MR, Ingram KA, Chen S, McNamara JR, Gebhart BW, Ribaya-Mercado JD, Perrone G, Robins SJ, Franke WC: Lipid responses to plant-sterol-enriched reduced-fat spreads incorporated into a National Cholesterol Education Program Step I diet. Am J Clin Nutr. 2001, 74: 33-43.
Christiansen LI, Lähteenmäki PLA, Mannelin MR, Seppänen-Laakso TE, Hiltunen RVK, Yliruusi JK: Cholesterol-lowering effect of spreads enriched with microcrystalline plant sterols in hypercholesterolemic subjects. Eur J Nutr. 2001, 40: 66-73. 10.1007/s003940170017
Volpe R, Niittynen L, Korpela R, Sirtori C, Bucci A, Fraone N, Pazzucconi F: Effects of yoghurt enriched with plant sterols on serum lipids in patients with moderate hypercholesterolaemia. Br J Nutr. 2001, 86: 233-239.
Nguyen TT, Dale LC, von Bergmann K, Croghan IT: Cholesterol-lowering effect of stanol ester in a US population of mildly hypercholesterolemic men and women: a randomized controlled trial. Mayo Clin Proc. 1999, 74: 1198-2006.
Thomsen AB, Hansen HB, Christiansen C, Green H, Berger A: Effect of free plant sterols in low-fat milk on serum lipid profile in hypercholesterolemic subjects. Eur J Clin Nutr. 2004
Schwab US, Vogel S, Lammi-Keefe CJ, Ordovas JM, Schaefer EJ, Li ZG, Ausman LM, Gualtieri L, Goldin BR, Furr HC, Lichtenstein AH: Varying dietary fat type of reduced-fat diets has little effect on the susceptibility of LDL to oxidative modification in moderately hypercholesterolemic subjects. J Nutr. 1998, 128: 1703-1709.
Pouteau E, Monnard I, Piguet-Welsch C, Groux MJA, Sagalowicz L, Berger A: Non-esterified plant sterols solubilized in low fat milks inhibit cholesterol absorption: a stable isotope double-blind crossover study. Eur J Nutr. 2003, 42: 154-164.
Devaraj S, Jialal I, Vega S: Plant sterol-fortified orange juice effectively lowers cholesterol levels in mildly hypercholesterolemic healthy individuals. Arterioscler Thromb Vasc Biol. 2004, 24: e25- 10.1161/01.ATV.0000120784.08823.99
Howard BV, Gidding SS, Liu K: Association of apolipoprotein E phenotype with plasma lipoproteins in African-American and white young adults. The CARDIA Study. Coronary Artery Risk Development in Young Adults. Am J Epidemiol. 1998, 148: 859-868.
Pedersen A, Baumstark MW, Marckmann P, Gylling H, Sandstrom B: An olive oil-rich diet results in higher concentrations of LDL cholesterol and a higher number of LDL subfraction particles than rapeseed oil and sunflower oil diets. J Lipid Res. 2000, 41: 1901-1911.
Wagner KH, Tomasch R, Elmadfa I: Impact of diets containing corn oil or olive/sunflower oil mixture on the human plasma and lipoprotein lipid metabolism. Eur J Nutr. 2001, 40: 161-167. 10.1007/s003940170004
Ostlund RE, Jr, Racette SB, Okeke A, Stenson WF: Phytosterols that are naturally present in commercial corn oil significantly reduce cholesterol absorption in humans. Am J Clin Nutr. 2002, 75: 1000-1004.
Berger A, Gremaud G, Baumgartner M, Rein D, Monnard I, Kratky E, Geiger W, Burri J, Dionisi F, Allan M, Lambelet P: Cholesterol-lowering properties of amaranth grain and oil in hamsters. Int J Vitam Nutr Res. 2003, 73: 39-47.
Berger A, Monnard I, Dionisi F, Gumy D, Lambelet P, Hayes KC: Preparation of amaranth flakes, crude oils, and refined oils for evaluation of cholesterol-lowering properties in hamster. Food Chem. 2003, 81: 119-124. 10.1016/S0308-8146(02)00387-4. 10.1016/S0308-8146(02)00387-4
Trautwein EA, Schulz C, Rieckhoff D, Kunath-Rau A, Erbersdobler HF, de Groot WA, Meijer GW: Effect of esterified 4-desmethylsterols and -stanols or 4, 4'-dimethylsterols on cholesterol and bile acid metabolism in hamsters. Br J Nutr. 2002, 87: 227-238. 10.1079/BJNBJN2001509
Kritchevsky D, Tepper SA, Wright S, Czarnecki SK, Wilson TA, Nicolosi RJ: Cholesterol vehicle in experimental atherosclerosis 24: avocado oil. J Am Coll Nutr. 2003, 22: 52-55.
Perona JS, Canizares J, Montero E, Sanchez-Dominguez JM, Ruiz-Gutierrez V: Plasma lipid modifications in elderly people after administration of two virgin olive oils of the same variety (Olea europaea var. hojiblanca) with different triacylglycerol composition. Br J Nutr. 2003, 89: 819-826. 10.1079/BJN2003852
Garg ML, Blake RJ, Wills RB: Macadamia nut consumption lowers plasma total and LDL cholesterol levels in hypercholesterolemic men. J Nutr. 2003, 133: 1060-1063.
Khallouki F, Younos C, Soulimani R, Oster T, Charrouf Z, Spiegelhalder B, Bartsch H, Owen RW: Consumption of argan oil (Morocco) with its unique profile of fatty acids, tocopherols, squalene, sterols and phenolic compounds should confer valuable cancer chemopreventive effects. Eur J Cancer Prev. 2003, 12: 67-75. 10.1097/00008469-200302000-00011
Ostlund R E, Jr, Racette SB, Stenson WF: Inhibition of cholesterol absorption by phytosterol-replete wheat germ compared with phytosterol-depleted wheat germ. Am J Clin Nutr. 2003, 77: 1385-1389.
Maki KC, Davidson MH, Umporowicz DM, Schaefer EJ, Diklin MR, Ingram KA, Chen S, McNamara Jr W, Gebhart B, Ribaya-Mercado JD, Perrone G, Robins SJ, Franke WC: Lipid responses to plant sterol-enriched reduced-fat spreads incorporated into a National Cholesterol Education step 1 diet. Am J Clin Nutr. 2001, 74: 33-43.
Mattson FH, Grundy SM, Crouse JR: Optimizing the effect of plant sterols on cholesterol absorption in man. Am J Clin Nutr. 1982, 35: 697-700.
Law M: Plant sterol and stanol margarines and health. Br Med J. 2000, 320: 861-864. 10.1136/bmj.320.7238.861. 10.1136/bmj.320.7238.861
Katan MB, Grundy SM, Jones P, Law M, Miettinen T, Paoletti R: Efficacy and safety of plant stanols and sterols in the management of blood cholesterol levels. Mayo Clin Proc. 2003, 78: 965-978.
Hallikainen MA, Uusitupa MIJ: Effects of 2 low-fat stanol ester-containing margarines on serum cholesterol concentrations as part of a low-fat diet in hypercholesterolemic subjects. Am J Clin Nutr. 1999, 69: 403-410.
Jones PJH, Ntamios FY, Mahmoud Raeini-Sarjaz C: Cholesterol-lowering efficacy of sitostanol-containing phytosterol mixture with a prudent diet in hyperlipidemic men. Am J Clin Nutr. 1999, 69: 1144-1150.
van Heyningen C: Cholesterol lowering margarine may not be useful in healthy fat modified diet. Brit Med J. 1999, 319: 186-
Mussner MJ, Parhofer KG, Von Bergmann K, Schwandt P, Broedl U, Otto C: Effects of phytosterol ester-enriched margarine on plasma lipoproteins in mild to moderate hypercholesterolemia are related to basal cholesterol and fat intake. Metabolism. 2002, 51: 189-194. 10.1053/meta.2002.29988
Maki KC, Shinnick F, Seeley MA, Veith PE, Quinn LC, Hallissey PJ, Temer A, Davidson MH: Food products containing free tall oil-based phytosterols and oat beta-glucan lower serum total and LDL cholesterol in hypercholesterolemic adults. J Nutr. 2003, 133: 808-813.
Judd JT, Baer DJ, Clevidence BA, Muesing RA, Chen SC, Meijer GW: Dietary fat and fatty acids and plasma lipid modifying effects of sterol esters. FASEB J. 2001, 15: A639-
Gremaud G, Piguet C, Baumgartner M, Pouteau E, Decarli B, Berger A, Fay LB: Simultaneous assessment of cholesterol absorption and synthesis in humans using on-line gas chromatography/combustion and gas chromatography/pyrolysis/isotope-ratio mass spectrometry. Rapid Commun Mass Spectrom. 2001, 15: 1207-1213. 10.1002/rcm.365
Gremaud G, Dalan E, Piguet C, Baumgartner M, Ballabeni P, Decarli B, Leser ME, Berger A, Fay LB: Effects of non-esterified stanols in a liquid emulsion on cholesterol absorption and synthesis in hypercholesterolemic men. Eur J Nutr. 2002, 41: 54-60. 10.1007/s003940200008
Mensink RP, Ebbing S, Lindhout M, Plat J, van Heugten MMA: Effects of plant stanol esters supplied in low-fat yoghurt on serum lipids and lipoproteins, non-cholesterol sterols and fat soluble antioxidant concentrations. Atherosclerosis. 2002, 160: 205-213. 10.1016/S0021-9150(01)00562-7
Richelle M, Enslen M, Hager C, Groux M, Tavazzi I, Godin JP, Berger A, Métairon S, Quaile S, Piguet C, Sagalowicz L, Green H, Fay LB: Both free and esterified plant sterols decrease the bioavailability of β-carotene and β-tocopherol, in normocholesterolemic humans. Am J Clin Nutr. 2004, (In press)-
Nestel P, Cehun M, Pomeroy S, Abbey M, Weldon G: Cholesterol-lowering effects of plant sterol esters and non-esterified stanols in margarine, butter and low-fat foods. Eur J Clin Nutr. 2001, 55: 1084-1090. 10.1038/sj.ejcn.1601264
Matvienko OA, Lewis DS, Swanson M, Arndt B, Rainwater DL, Stewart J, Alekel DL: A single daily dose of soybean phytosterols in ground beef decreases serum total cholesterol and LDL cholesterol in young, mildly hypercholesterolemic men. Am J Clin Nutr. 2002, 76: 57-64.
Carr TP, Cornelison RM, Illston BJ, Stuefer-Powell CL, Gallaher DD: Plant sterols alter bile acid metabolism and reduce cholesterol absorption in hamsters fed a beef-based diet. Nutr Res. 2002, 22: 745-754. 10.1016/S0271-5317(02)00389-5. 10.1016/S0271-5317(02)00389-5
Spilburg CA, Goldberg AC, McGill JB, Stenson WF, Racette SB, Bateman J, McPherson TB, Ostlund R E, Jr: Fat-free foods supplemented with soy stanol-lecithin powder reduce cholesterol absorption and LDL cholesterol. J Am Diet Assoc. 2003, 103: 577-581. 10.1053/jada.2003.50110
Hallikainen MA, Sarkkinen ES, Gylling H, Erkkilä AT, Uusitupa MIJ: Comparison of the effects of plant sterol ester and plant stanol ester-enriched margarines in lowering serum cholesterol concentrations in hypercholesterolaemic subjects on a low-fat diet. Eur J Clin Nutr. 2000, 54: 715-725. 10.1038/sj.ejcn.1601083
Jones PJ, Raeini-Sarjaz M, Ntanios FY, Vanstone CA, Feng J, Parsons WE: Modulation of plasma lipid levels and cholesterol kinetics by phytosterol versus phytostanol esters. J Lipid Res. 2000, 41: 697-705.
Neil HAW, Meijer GW, Roe LS: Randomised controlled trial of use by hypercholesterolaemic patients of a vegetable oil sterol-enriched fat spread. Atherosclerrosis. 2001, 156: 329-337. 10.1016/S0021-9150(00)00653-5. 10.1016/S0021-9150(00)00653-5
Ntanios FY, Homma Y, Ushiro S: A spread enriched with plant sterol-esters lowers blood cholesterol and lipoproteins without affecting vitamins A and E in normal and hypercholesterolemic Japanese men and women. J Nutr. 2002, 132: 3650-3655.
Cleghorn CL, Skeaff CM, Mann J, Chisholm A: Plant sterol-enriched spread enhances the cholesterol-lowering potential of a fat-reduced diet. Eur J Clin Nutr. 2003, 57: 170-176. 10.1038/sj.ejcn.1601531
Hendriks HF, Brink EJ, Meijer GW, Princen HM, Ntanios FY: Safety of long-term consumption of plant sterol esters-enriched spread. Eur J Clin Nutr. 2003, 57: 681-692. 10.1038/sj.ejcn.1601598
Homma Y, Ikeda I, Ishikawa T, Tateno M, Sugano M, Nakamura H: A randomized, placebo-controlled trial: Decrease in plasma low-density lipoprotein cholesterol, apolipoprotein B, cholesteryl ester transfer protein, and oxidized low-density lipoprotein by plant stanol ester-containing spread. Nutrition. 2003, 19:: 369-374. 10.1016/S0899-9007(02)00926-7
Jones PJH, Vanstone CA, Raieni-Sarjaz M, St-Onge M-P: Phytosterols in low-and non-fat beverages as part of a controlled diet fail to lower plasma lipid levels. J Lipid Res. 2003, 44: 1713-1719. 10.1194/jlr.M300089-JLR200
Groux MJA, Leser M, Berger A: Milk product comprising unesterified sterol. 2003, iPatent WO03009708, Nestle SA
von Bonsdorff-Nikander A, Karjalainen M, Rantanen J, Christiansen L, Yliruusi J: Physical stability of a microcrystalline beta-sitosterol suspension in oil. Eur J Pharm Sci. 2003, 19: 173-179. 10.1016/S0928-0987(03)00067-8
Jenkins DJ, Kendall CW, Marchie A, Faulkner D, Vidgen E, Lapsley KG, Trautwein EA, Parker TL, Josse RG, Leiter LA, Connelly PW: The effect of combining plant sterols, soy protein, viscous fibers, and almonds in treating hypercholesterolemia. Metabolism. 2003, 52: 1478-1483. 10.1016/S0026-0495(03)00260-9
Tikkanen MJ, Hogstrom P, Tuomilehto J, Keinanen-Kiukaanniemi S, Sundvall J, Karppanen H: Effect of a diet based on low-fat foods enriched with nonesterified plant sterols and mineral nutrients on serum cholesterol. Am J Cardiol. 2001, 88: 1157-1162. 10.1016/S0002-9149(01)02053-7
Vaskonen T, Mervaala E, Krogerus L, Karppanen H: Supplementation of plant sterols and minerals benefits obese zucker rats fed an atherogenic diet. J Nutr. 2002, 132: 231-237.
Vaskonen T, al. et: Effects of calcium and plant sterols on serum lipids in obese Zucker rats on a low-fat diet. Br J Nutr. 2002, 87: 239-246. 10.1079/BJNBJN2001508
Manhas A, Farmer JA: Hypolipidemic therapy and cholesterol absorption. Curr Atheroscler Rep. 2004, 6: 89-93.
Smart EJ, De Rose RA, Farber SA: Annexin 2-caveolin 1 complex is a target of ezetimibe and regulates intestinal cholesterol transport. Proc Natl Acad Sci U S A. 2004, 101: 3450-3455. 10.1073/pnas.0400441101
Cannon CP, Braunwald E, McCabe CH, Rader DJ, Rouleau JL, Belder R, Joyal SV, Hill KA, Pfeffer MA, Skene AM: Comparison of Intensive and Moderate Lipid Lowering with Statins after Acute Coronary Syndromes. N Engl J Med. 2004, 350: 15-10.1056/NEJMoa040583. 10.1056/NEJMoa040583
Topol EJ: Intensive Statin Therapy -- A Sea Change in Cardiovascular Prevention. N Engl J Med. 2004, 350: 15-10.1056/NEJMe048061. 10.1056/NEJMe048061
FDA: Food labeling: health claims; plant sterol/stanol esters and coronary heart disease. Food and Drug Admin Fed Reg. 2000, 65: 54686-54739, http://www.access.gpo.gov/su_docs/fedreg/a000908c.html
Australia New Zealand Food Authority ANZFA: Phytosterol esters derived from vegetable oils: Final Risk Analysis Report Application A410, 30/5/01. 2001, http://www.anzfa.gov.au/documents/A410_IR(FULL).pdf
Plat J, Van Onselen ENM, Van Heugten MMA, Mensink RP: Effects on serum lipids, lipoproteins and fat soluble antioxidant concentrations of consumption frequency of margarines and shortenings enriched with plant stanol esters. Eur J Clin Nutr. 2000, 54: 671-677. 10.1038/sj.ejcn.1601071
Jones PJ, Ntanios FY, Raeini-Sarjaz M, Vanstone CA: Cholesterol-lowering efficacy of a sitostanol-containing phytosterol mixture with a prudent diet in hyperlipidemic men. Am J Clin Nutr. 1999, 69: 1144-1150.
Homma Y, Ishikawa T, Tateno M, Mitaniyama A, Sugano M: Cholesterol and apolipoprotein-lowering effect of plant stanol ester in healthy Japanese men and women. J Jpn Soc Nutr Food Sci. 2000, 53: 155-162.
Plat J, Mensink RP: Vegetable oil based versus wood based stanol ester mixtures : effects on serum lipids and hemostatic factors in non-hypercholesterolemic subjects. Atherosclerosis. 2000, 148: 101-112. 10.1016/S0021-9150(99)00261-0
Vanstone CA, Raeini-Sarjaz M, Parsons WE, Jones PJ: Unesterified plant sterols and stanols lower LDL-cholesterol concentrations equivalently in hypercholesterolemic persons. Am J Clin Nutr. 2002, 76: 1272-1278.
Williams CL, Bollella MC, Strobino BA, Boccia L, Campanaro L: Plant stanol ester and bran fiber in chilhood : effects on lipids, stool weight and stool frequency in preschool children. J Am Coll Nutr. 1999, 18: 572-581.
Miettinen TA, Puska P, Gylling H, Vanhanen H, Vartiainen E: Reduction of serum cholesterol with sitostanol-ester margarine in a mildly hypercholesterolemic population. N Engl J Med. 1995, 333: 1308-1312. 10.1056/NEJM199511163332002
Jones PJ, Howell T, MacDougall DE, Feng JY, Parsons W: Short-term administration of tall oil phytosterols improves plasma lipid profiles in subjects with different cholesterol levels. Metabolism. 1998, 47: 751-756.
Hallikainen MA, Sarkkinen ES, Uusitupa MIJ: Effects of low-fat stanol ester enriched margarines on concentrations of serum carotenoids in subjects with elevated serum cholesterol concentrations. Eur J Clin Nutr. 1999, 53: 966-969. 10.1038/sj.ejcn.1600882
De Graaf J, De Sauvage Nolting PR, Van Dam M, Belsey EM, Kastelein JJ, Pritchard PH, Stalenhoef AF: Consumption of tall oil-derived phytosterols in a chocolate matrix significantly decreases plasma total and low-density lipoprotein-cholesterol levels. Br J Nutr. 2002, 88: 479-488. 10.1079/BJN2002690
Noakes M, Clifton P, Ntanios F, Shrapnel W, Record I, McInerney J: An increase in dietary carotenoids when consuming plant sterols or stanols is effective in maintaining plasma carotenoid concentrations. Am J Clin Nutr. 2002, 75: 79-86.
Gylling H, Miettinen TA: Serum cholesterol and cholesterol and lipoprotein metabolism in hypercholesterolaemic NIDDM patients before and during sitostanol ester-margarine treatment. Diabetologia. 1994, 37: 773-780. 10.1007/s001250050178
Gylling H, Miettinen TA: The effects of inhibiting cholesterol absorption and synthesis on cholesterol and lipoprotein metabolism in hypercholesterolemic non-insulin dependent men. J Lipid Res. 1996, 37: 1776-1785.
Igel M, Giesa U, Lutjohann D, von Bergmann K: Comparison of the intestinal uptake of cholesterol, plant sterols, and stanols in mice. J Lipid Res. 2003, 44: 533-538. 10.1194/jlr.M200393-JLR200
Turley SD, Dietschy JM: Sterol absorption by the small intestine. Curr Opin Lipidol. 2003, 14: 233-240. 10.1097/00041433-200306000-00002
Field FJ, Born E, Mathur SN: LXR/RXR ligand activation enhances the basolateral efflux of {beta}-sitosterol in CaCo-2 cells. J Lipid Res. 2004, 45: 905-913. 10.1194/jlr.M300473-JLR200
Mutch DM, Anderle P, Fiaux M, Mansourian R, Vidal K, Wahli W, Williamson G, Roberts MA: Regional variations in ABC transporter expression along the mouse intestinal tract. Physiol Genomics. 2004, 17: 11-20. 10.1152/physiolgenomics.00150.2003
Scoggan KA, Gruber H, Lariviere K: A missense mutation in the Abcg5 gene causes phytosterolemia in SHR, stroke-prone SHR, and WKY rats. J Lipid Res. 2003, 44: 911-916. 10.1194/jlr.M200438-JLR200
Plat J, Mensink RP: Increased intestinal ABCA1 expression contributes to the decrease in cholesterol absorption after plant stanol consumption. FASEB J. 2002, 16: 1248-1253. 10.1096/fj.01-0718hyp
Kaneko E, Matsuda M, Yamada Y, Tachibana Y, Shimomura I, Makishima M: Induction of intestinal ATP-binding cassette transporters by a phytosterol-derived liver X receptor agonist. J Biol Chem. 2003, 278: 36091-36098. 10.1074/jbc.M304153200
Yu L, von Bergmann K, Lutjohann D, Hobbs HH, Cohen JC: Selective sterol accumulation in ABCG5/ABCG8 deficient mice. J Lipid Res. 2004, 45: 301-307. 10.1194/jlr.M300377-JLR200
Weggemans RM, Zock PL, Tai ES, Ordovas JM, Molhuizen HO, Katan MB: ATP binding cassette G5 C1950G polymorphism may affect blood cholesterol concentrations in humans. Clin Genet. 2002, 62: 226-229. 10.1034/j.1399-0004.2002.620307.x
Berge KE, von Bergmann K, Lutjohann D, Guerra R, Grundy SM, Hobbs HH, Cohen JC: Heritability of plasma noncholesterol sterols and relationship to DNA sequence polymorphism in ABCG5 and ABCG8. J Lipid Res. 2002, 43: 486-494.
Kesäniemi YA, Ehnholm C, Miettinen TA: Intestinal cholesterol absorption efficiency in man is related to apoprotein E phenotype. J Clin Invest. 1987, 80: 578-581.
Vanhanen HT, Blomqvist S, Ehnholm C, Hyvonen M, Jauhiainen M, Torstila I, Miettinen TA: Serum cholesterol, cholesterol precursors, and plant sterols in hypercholesterolemic subjects with different apoE phenotypes during dietary sitostanol ester treatment. J Lipid Res. 1993, 34: 1535-1544.
Kramer W, Girbig F, Corsiero D, Burger K, Fahrenholz F, Jung C, Muller G: Intestinal cholesterol absorption: identification of different binding proteins for cholesterol and cholesterol absorption inhibitors in the enterocyte brush border membrane. Biochim Biophys Acta. 2003, 1633: 13-26. 10.1016/S1388-1981(03)00068-4
Harris M, Davis W, Brown WV: Ezetimibe. Drugs Today (Barc). 2003, 39: 229-247.
Cruz ML, Wong WW, Mimouni F, Hachey DL, Setchell KD, Klein PD, Tsang RC: Effects of infant nutrition on cholesterol synthesis rates. Pediatr Res. 1994, 35: 135-140.
Alasmi M, Thorkelson T, Krug-Wispe S, Bayley TM, Jones PJH, Tsang RC: Cholesterol supplementation effect on cholesterol synthesis rates (FSR) in infants. Pediatr Res. 1996, 39: 116A-
Bayley TM, Alasmi M, Thorkelson T, Krugwispe S, Jones PJH, Bulani JL, Tsang RC: Influence of formula versus breast milk on cholesterol synthesis rates in four-month-old infants. Pediatr Res. 1998, 44: 60-67.
Huisman M, van Beusekom CM, Lanting CI, Nijeboer HJ, Muskiet FA, Boersma ER: Triglycerides, fatty acids, sterols, mono- and disaccharides and sugar alcohols in human milk and current types of infant formula milk. Eur J Clin Nutr. 1996, 50: 255-260.
Fall CH, Barker DJ, Osmond C, Winter PD, Clark PM, Hales CN: Relation of infant feeding to adult serum cholesterol concentration and death from ischaemic heart disease. Brit Med J. 1992, 304: 801-805.
Kolacek S, Kapetanovic T, Zimolo A, Luzar V: Early determinants of cardiovascular risk factors in adults. A. Plasma lipids. Acta Paediatr. 1993, 82: 699-704.
Palinski W, Napoli C: The fetal origins of atherosclerosis: maternal hypercholesterolemia, and cholesterol-lowering or antioxidant treatment during pregnancy influence in utero programming and postnatal susceptibility to atherogenesis. FASEB J. 2002, 16: 1348-1360. 10.1096/fj.02-0226rev
Joki P, Suomalainen H, Jarvinen KM, Juntunen-Backman K, Gylling H, Miettinen TA, Antikainen M: Cholesterol precursors and plant sterols in children with food allergy. Am J Clin Nutr. 2003, 77: 51-55.
Schlierf G, Vogel G, Heuck CC, Oster P, Raetzer H, Schellenberg B: [Dietary management of familial Hypercholesterolemia in Children and adolescents -- a feasibility study (author's transl)]. Monatsschr Kinderheilkd. 1977, 125: 770-773.
Becker M, Staab D, Von Bergman K: Long-term treatment of severe familial hypercholesterolemia in children: effect of sitosterol and bezafibrate. Pediatrics. 1992, 89: 138-142.
Gylling H, Siimes MA, Miettinen TA: Sitostanol ester margarine in dietary treatment of children with familial hypercholesterolemia. J Lipid Res. 1995, 36: 1807-1812.
Vuorio AF, Gylling H, Turtola H, Kontula K, Ketonen P, Miettinen TA: Stanol ester margarine alone and with simvastatin lowers serum cholesterol in families with familial hypercholesterolemia caused by the FH-North Karelia mutation. Arterioscler Thromb Vasc Biol. 2000, 20: 500-506.
Schlierf G, Oster P, Heuck CC, Raetzer H, Schellenberg B: Sitosterol in juvenile type II hyperlipoproteinemia. Atherosclerosis. 1978, 30: 245-248.
Amundsen ÅL, Ose L, Nenseter MS, Ntanios FY: Plant sterol ester-enriched spread lowers plasma total and LDL cholesterol in children with familial hypercholesterolemia. Am J Clin Nutr. 2002, 76: 338-344.
Tammi A, Rönnemaa T, Gylling H, Rask-Nissilä L, Viikari J, Tuominen J, Pulkki K, Simell O: Plant stanol ester margarine lowers serum total and low-density lipoprotein cholesterol concentrations of healthy children: The STRIP project. J Pediatr. 2000, 136: 503-510.
Tammi A, Rönnemaa T, Valsta L, Seppänen R, Rask-Nissilä L, Miettinen TA, Gylling H, Viikari J, Anttolainen M, Simell O: Dietary plant sterols alter the serum plant sterol concentration but not the cholesterol precursor sterol concentrations in young children (the STRIP Study). Special Turku Coronary Risk Factor Intervention Project. J Nutr. 2001, 131: 1942-1945.
Mellies M, Glueck CJ, Sweeney C, Fallat RW, Tsang RC, Ishikawa TT: Plasma and dietary phytosterols in children. Pediatrics. 1976, 57: 60-67.
Kempen HJ, de-Knijff P, Boomsma DI, Van der, V, Gevers Leuven JA, Havekes L: Plasma levels of lathosterol and phytosterols in relation to age, sex, anthropometric parameters, plasma lipids, and apolipoprotein E phenotype, in 160 Dutch families. Metabolism. 1991, 40: 604-611. 10.1016/0026-0495(91)90102-3
Tammi A, Ronnemaa T, Miettinen TA, Gylling H, Rask-Nissila L, Viikari J, Tuominen J, Marniemi J, Simell O: Effects of gender, apolipoprotein E phenotype and cholesterol-lowering by plant stanol esters in children: the STRIP study. Special Turku Coronary Risk Factor Intervention Project. Acta Paediatr. 2002, 91: 1155-1162. 10.1080/080352502320777379
Miettinen TA: Phytosterolaemia, xanthomatosis and premature atherosclerotic arterial disease: a case with high plant sterol absorption, impaired sterol elimination and low cholesterol synthesis. Eur J Clin Invest. 1980, 10: 27-35.
Miettinen HE, Gylling H, Miettinen TA, Viikari J, Paulin L, Kontula K: Apolipoprotein A-IFin. Dominantly inherited hypoalphalipoproteinemia due to a single base substitution in the apolipoprotein A-I gene. Arterioscler Thromb Vasc Biol. 1997, 17: 83-90.
Patel SB, Salen G, Hidaka H, Kwiterovich PO, Stalenhoef AF, Miettinen TA, Grundy SM, Lee MH, Rubenstein JS, , , Brownstein MJ: Mapping a gene involved in regulating dietary cholesterol absorption. The sitosterolemia locus is found at chromosome 2p21. J Clin Invest. 1998, 102: 1041-1044.
Patel SB, Honda A, Salen G: Sitosterolemia: exclusion of genes involved in reduced cholesterol biosynthesis. J Lipid Res. 1998, 39: 1055-1061.
Stalenhoef AF, Hectors M, Demacker PN: Effect of plant sterol-enriched margarine on plasma lipids and sterols in subjects heterozygous for phytosterolaemia. J Intern Med. 2001, 249: 163-166. 10.1046/j.1365-2796.2001.00788.x
Kwiterovich P O, Jr, Chen SC, Virgil DG, Schweitzer A, Arnold DR, Kratz LE: Response of obligate heterozygotes for phytosterolemia to a low-fat diet and to a plant sterol ester dietary challenge. J Lipid Res. 2003, 44: 1143-1155. 10.1194/jlr.M200455-JLR200
Awad AB, Smith AJ, Fink CS: Plant sterols regulate rat vascular smooth muscle cell growth and prostacyclin release in culture. Prostaglandins Leukot Essent Fatty Acids. 2001, 64: 323-330. 10.1054/plef.2001.0273
Ntanios FY, Jones PJ, Frohlich JJ: Dietary sitostanol reduces plaque formation but not lecithin cholesterol acyl transferase activity in rabbits. Atherosclerosis. 1998, 138: 101-110. 10.1016/S0021-9150(98)00008-2
Ntanios FY, van de Kooij AJ, de Deckere EA, Duchateau GS, Trautwein EA: Effects of various amounts of dietary plant sterol esters on plasma and hepatic sterol concentration and aortic foam cell formation of cholesterol-fed hamsters. Atherosclerosis. 2003, 169: 41-50. 10.1016/S0021-9150(03)00132-1
Awad AB, Fink CS: Phytosterols as anticancer dietary components: evidence and mechanism of action. J Nutr. 2000, 130: 2127-2130.
Awad AB, von Holtz RL, Cone JP, Fink CS, Chen YC: beta-sitosterol inhibits growth of Ht-29 human colon cancer cells by activating the sphingomyelin cycle. Anticancer Res. 1998, 18: 471-473.
Awad AB, Gan Y, Fink CS: Effect of b-sitosterol, a plant sterol, on growth, protein phosphatase 2A, and phospholipase D in LNCaP cells. Nutr Cancer. 2000, 36: 74-78. 10.1207/S15327914NC3601_11
Awad AB, Downie A, Fink CS, Kim U: Dietary phytosterol inhibits the growth and metastasis of MDA-MB-231 human breast cancer cells grown in SCID mice. Anticancer Res. 2000, 20: 821-824.
Wilt T, Ishani A, MacDonald R, Stark G, Mulrow C, Lau J: Beta-sitosterols for benign prostatic hyperplasia. Cochrane Database Syst. 2: Rev 2000; CD001043 Review
Normén AL, Brants HA, Voorrips LE, Andersson HA, van den Brandt PA, Goldbohm RA: Plant sterol intakes and colorectal cancer risk in the Netherlands Cohort Study on Diet and Cancer. Am J Clin Nutr. 2001, 74: 141-148.
Quilliot D, Boman F, Creton C, Pelletier X, Floquet J, Debry G: Phytosterols have an unfavourable effect on bacterial activity and no evident protective effect on colon carcinogenesis. Eur J Cancer Prev. 2001, 10: 237-243. 10.1097/00008469-200106000-00006
Mendilaharsu M, De Stefani E, Deneo-Pellegrini H, Carzoglio J, Ronco A: Phytosterols and risk of lung cancer: a case-control study in Uruguay. Lung Cancer. 1998, 21: 37-45. 10.1016/S0169-5002(98)00044-0
Ronco A, De Stefani E, Boffetta P, Deneo-Pellegrini H, Mendilaharsu M, Leborgne F: Vegetables, fruits, and related nutrients and risk of breast cancer: a case-control study in Uruguay. Nutr Cancer. 1999, 35: 111-119. 10.1207/S15327914NC352_3
De Stefani E, Boffetta P, Ronco AL, Brennan P, Deneo-Pellegrini H, Carzoglio JC, Mendilaharsu M: Plant sterols and risk of stomach cancer: a case-control study in Uruguay. Nutr Cancer. 2000, 37: 140-144. 10.1207/S15327914NC372_4
De Stefani E, Brennan P, Boffetta P, Ronco AL, Mendilaharsu M, Deneo-Pellegrini H: Vegetables, fruits, related dietary antioxidants, and risk of squamous cell carcinoma of the esophagus: a case-control study in Uruguay. Nutr Cancer. 2000, 38: 23-29. 10.1207/S15327914NC381_4
McCann SE, Freudenheim JL, Marshall JR, Brasure JR, Swanson MK, Graham S: Diet in the epidemiology of endometrial cancer in western New York (United States). Cancer Causes Control. 2000, 11: 965-974. 10.1023/A:1026551309873
McCann SE, Freudenheim JL, Marshall JR, Graham S: Risk of human ovarian cancer is related to dietary intake of selected nutrients, phytochemicals and food groups. J Nutr. 2003, 133: 1937-1942.
Bouic PJ, Clark A, Brittle W, Lamprecht JH, Freestone M, Liebenberg RW: Plant sterol/sterolin supplement use in a cohort of South African HIV-infected patients--effects on immunological and virological surrogate markers. S Afr Med J. 2001, 91: 848-850.
Wang T, Hicks KB, Moreau R: Antioxidant activity of phytosterols, oryzanol, and other phytosterol conjugates. J Am Oil Chem Soc. 2002, 79: 1201-1206.
Loscalzo J: Oxidant stress: a key determinant of atherothrombosis. Biochem Soc Trans. 2003, 31: 1059-1061.
Quong J, Eppenberger-Castori S, Moore D, 3rd, Scott GK, Birrer MJ, Kueng W, Eppenberger U, Benz CC: Age-dependent changes in breast cancer hormone receptors and oxidant stress markers. Breast Cancer Res Treat. 2002, 76: 221-236. 10.1023/A:1020886801674
Paul Jayaraj A, Tovey FI, Hobsley M: Duodenal ulcer prevalence: research into the nature of possible protective dietary lipids. Phytother Res. 2003, 17: 391-398. 10.1002/ptr.1310
Smania EF, Delle Monache F, Smania A, Jr, Yunes RA, Cuneo RS: Antifungal activity of sterols and triterpenes isolated from Ganoderma annulare. Fitoterapia. 2003, 74: 375-377. 10.1016/S0367-326X(03)00064-9
Davidson MH, Maki KC, Umporowicz DM, Ingram KA, Dicklin MR, Schaefer E, Lane RW, McNamara JR, Ribaya-Mercado JD, Perrone G, Robins SJ, Franke WC: Safety and tolerability of esterified phytosterols administered in reduced-fat spread and salad dressing to healthy adult men and women. J Am Coll Nutr. 2001, 20: 307-319.
Plat J, Mensink RP: Effects of plant stanol esters on LDL receptor protein expression and on LDL receptor and HMG-CoA reductase mRNA expression in mononuclear blood cells of healthy men and women. FASEB J. 2002, 16: 258-260. 10.1096/fj.01-0718hyp
Ntanios FY, Duchateau GS: A healthy diet rich in carotenoids is effective in maintaining normal blood carotenoid levels during the daily use of plant sterol-enriched spreads. Int J Vitam Nutr Res. 2002, 72: 32-39.
Raeini-Sarjaz M, Ntanios FY, Vanstone CA, Jones PJ: No changes in serum fat-soluble vitamin and carotenoid concentrations with the intake of plant sterol/stanol esters in the context of a controlled diet. Metabolism. 2002, 51: 652-656. 10.1053/meta.2002.32021
Nissinen M, Gylling H, Vuoristo M, Miettinen TA: Micellar distribution of cholesterol and phytosterols after duodenal plant stanol ester infusion. Am J Physiol Gastrointest Liver Physiol. 2002, 282: G1009-10015.
Miettinen TA, Gylling H, Lindbohm N, Miettinen TE, Rajaratnam RA, Relas H: Serum noncholesterol sterols during inhibition of cholesterol synthesis by statins. J Lab Clin Med. 2003, 141: 131-137. 10.1067/mlc.2003.9
Heinemann T, Leiss O, von Bergmann K: Effect of low-dose sitostanol on serum cholesterol in patients with hypercholesterolemia. Atherosclerosis. 1986, 61: 219-223.
Howell TJ, MacDougall DE, Jones PJ: Phytosterols partially explain differences in cholesterol metabolism caused by corn or olive oil feeding. J Lipid Res. 1998, 39: 892-900.
Gylling H, Miettinen TA: Cholesterol reduction by different plant stanol mixtures and with variable fat intake. Metabolism. 1999, 48: 575-580.
Normen L, Dutta P, Lia A, Andersson H: Soy sterol esters and β-sitostanol ester as inhibitors of cholesterol absorbtion in human small bowel. Am J Clin Nutr. 2000, 71: 908-913.
Homma Y, Ikeda I, Ishikawa T, Tateno M, Sugano M, Nakamura H: Decrease in plasma low-density lipoprotein cholesterol, apolipoprotein B, cholesteryl ester transfer protein, and oxidized low-density lipoprotein by plant stanol ester-containing spread: a randomized, placebo-controlled trial. Nutrition. 2003, 19: 369-374. 10.1016/S0899-9007(02)00926-7
Gylling H, Puska P, Vartiainen E, Miettinen TA: Retinol, vitamin D, carotenes and alpha-tocopherol in serum of a moderately hypercholesterolemic population consuming sitostanol ester margarine. Atherosclerosis. 1999, 145: 279-285. 10.1016/S0021-9150(99)00078-7
Acknowledgements
The authors thank Hilary Green of the Nestlé Research Center (NRC) in Lausanne, Switzerland for proof reading and improving the manuscript. AB completed parts of this review at the NRC, as a Senior Project Leader for plant sterol research.
Author information
Authors and Affiliations
Corresponding author
Additional information
Authors' contributions
AB completed the first draft of the article and tables. PJHJ and SSH then contributed substantially to the text and tables, expanding the initial concept, and elaborating and updating specific themes. AB updated the final text. All authors improved overall flow.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Berger, A., Jones, P.J. & Abumweis, S.S. Plant sterols: factors affecting their efficacy and safety as functional food ingredients. Lipids Health Dis 3, 5 (2004). https://doi.org/10.1186/1476-511X-3-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1476-511X-3-5