Abstract
Background
The decline in efficacy of artesunate (AS) and mefloquine (MQ) is now the major concern in areas along the Thai-Cambodian and Thai-Myanmar borders.
Methods
The correlation between polymorphisms of pfatp6, pfcrt, pfmdr1 and pfmrp1 genes and in vitro sensitivity of Plasmodium falciparum isolates to the artemisinin-based combination therapy (ACT) components AS and MQ, including the previously used first-line anti-malarial drugs chloroquine (CQ) and quinine (QN) were investigated in a total of 119 P. falciparum isolates collected from patients with uncomplicated P. falciparum infection during 2006–2009.
Results
Reduced in vitro parasite sensitivity to AS [median (95% CI) IC50 3.4 (3.1-3.7) nM] was found in 42% of the isolates, whereas resistance to MQ [median (95% CI) IC50 54.1 (46.8-61.4) nM] accounted for 58% of the isolates. Amplification of pfmdr1 gene was strongly associated with a decline in susceptibility of P. falciparum isolates to AS, MQ and QN. Significant difference in IC50 values of AS, MQ and QN was observed among isolates carrying one, two, three, and ≥ four gene copies [median (95% CI) AS IC50: 1.6 (1.3-1.9), 1.8 (1.1-2.5), 2.9 (2.1-3.7) and 3.1 (2.5-3.7) nM, respectively; MQ IC50: 19.2 (15.8-22.6), 37.8 (10.7-64.8), 55.3 (47.7-62.9) and 63.6 (49.2-78.0) nM, respectively; and QN IC50: 183.0 (139.9-226.4), 256.4 (83.7-249.1), 329.5 (206.6-425.5) and 420.0 (475.2-475.6) nM, respectively]. The prevalence of isolates which were resistant to QN was reduced from 21.4% during the period 2006–2007 to 6.3% during the period 2008–2009. Pfmdr1 86Y was found to be associated with increased susceptibility of the parasite to MQ and QN. Pfmdr1 1034C was associated with decreased susceptibility to QN. Pfmrp1 191Y and 1390I were associated with increased susceptibility to CQ and QN, respectively.
Conclusion
High prevalence of CQ and MQ-resistant P. falciparum isolates was observed during the four-year observation period (2006–2009). AS sensitivity was declined, while QN sensitivity was improved. Pfmdr1 and pfmrp1 appear to be the key genes that modulate multidrug resistance in P. falciparum.
Similar content being viewed by others
Background
Southeast Asia, particularly the Thai-Cambodian border, is one of the malaria-endemic region where multidrug-resistant Plasmodium falciparum malaria has been reported [1]. In the 1960s and 1970s, chloroquine (CQ) resistance spread throughout the region and subsequently, in the 1980s, resistance to sulphadoxine and pyrimethamine was reported [2]. In 1984, mefloquine (MQ) was firstly introduced for clinical use as first-line treatment for uncomplicated multidrug-resistant P. falciparum malaria in Thailand, but MQ resistance was rapidly developed four years after its implementation. Following the decline in clinical efficacy of MQ, the artemisinin-based combination therapy (ACT) using the artesunate-mefloquine combination was introduced as first-line reatment in 1994 [3]. Cure rate was improved to over 90% and the incidence of P. falciparum malaria was markedly reduced [4, 5]. Artemisinin resistance however, initially occurred during 2006–2007 in areas along the Thai-Cambodian border [6]. With regard to the Thai-Myanmar border, treatment failure following ACT has been increasing especially in Tak province [7]. Studies during 2008–2009 showed a marked decline in the 42-day cure rate from 99.2 to 72.58% [8, 9]. It is unclear whether artemisinin resistance has spread from the eastern to the western border of the country. Monitoring and identifying factors contributing to this low cure rate is necessary for the country’s future perspective of malaria control policy. Applying genetic analysis as a tool for detecting the genetic change of malaria parasite genes that have been shown to link with the decline in efficacy of artesunate (AS) and MQ; i.e., pfmdr1[10], pfatp6[11] and pfmrp1[12–14], in association with the in vitro sensitivity of the parasite to both combination partners, would help to detect early changes in P. falciparum sensitivity to this combination therapy.
In the present study, the association between the polymorphisms of pfatp6, pfcrt, pfmdr1, and pfmrp1 genes and in vitro sensitivity of P. falciparum isolates to AS, MQ, as well as CQ and quinine (QN) was investigated in P. falciparum isolates collected from the Thai-Myanmar border. In addition, the change in parasite genetic patterns and in vitro sensitivity over the period 2006–2009 was also examined.
Methods
Blood samples
A total of 130 P. falciparum isolates were collected from patients with uncomplicated P. falciparum infection prior to treatment with a three-day combination regimen (25 mg/kg body weight MQ and 12 mg/kg body weight AS) for investigation of the polymorphisms of candidate molecular markers of anti-malarial drug resistance and in vitro parasite sensitivity. The study was conducted at Mae Tao clinic, Mae Sot District, Tak Province, Thailand during 2006–2009. Fifty-seven and 73 isolates were collected from patients during 2006–2007 and 2008–2009, respectively (Figure 1). The study protocol was approved by the Ethics Committee of the Ministry of Public Health of Thailand and written informed consents for study participations were obtained from all patients before study.
Culture system and in vitro sensitivity assay
All parasite isolates were adapted to continuous culture according to the method of [15] with modification. The laboratory-adapted 3D7 (CQ-sensitive) and K1 (CQ-resistant) P. falciparum were used as control parasite clones. Susceptibility of P. falciparum isolates to AS, MQ, CQ and QN was investigated using SYBR Green I assay [16, 17]. Highly synchronous ring stage parasites were used in each assay. An aliquot of parasite inoculum (50 μl) with 2% parasitaemia and 1% haematocrit was added into each well of the 96-well microtitre plate. The plate was pre-dosed with each anti-malarial drug at eight final concentrations as follows: AS: 0.39, 0.78, 1.56, 3.13, 6.25, 12.5, 25, and 50 nM; MQ: 3.13, 6.25, 12.5, 25, 50, 100, 200, and 400 nM; CQ (3.13, 7.81, 15.63, 31.25, 62.5, 125, 250, and 500 nM); and QN: 7.81, 15.63, 31.25, 62.5, 125, 250, 500, and 1,000 nM. Standard compounds of all anti-malarial drugs were purchased from Sigma-Aldrich Co (St Louis, MO, USA). All were stored at −20°C as 10 mM stock solutions in 50% ethanol. The experiments were repeated three times, triplicate for each experiment. IC50 value (concentration that inhibits parasite growth by 50%) was used as an indicator for anti-malarial susceptibility and was determined from a log-dose response analysis using the CalcuSyn™ computer program (Biosoft, Cambridge, UK). The criterion used for susceptibility of the parasite isolates to CQ was as follow: sensitive (S: IC50 <25 nM), moderately resistant (MR: 25 ≤ IC50 <100 nM), and highly resistant (HR: IC50 ≥100 nM). QN susceptibility was categorized into two levels, i.e., S (IC50 <500 nM), and resistant (R: IC50 ≥500 nM). MQ susceptibility was categorized into two levels, i.e., “sensitive” (IC50 ≤24 nM) and “resistant” (IC50 >24 nM). For AS, the susceptibility was classified as “sensitive” (IC50 ≤ upper limit of 95% CI of the median IC50) and “declined sensitivity” (IC50 > upper limit of 95% confidence interval (CI) of the median IC50) [18].
Investigation of polymorphisms of pfcrt, pfmdr1, pfatp6, and pfmrp1 using PCR-RFLP
Genomic DNA was extracted from all samples (culture-adapted P. falciparum; Figure 1) using chelex resin modified technique [19]. Prior to being used as a DNA template, concentration of the malaria genomic DNA was determined by spectrophotometry (NanodropTM, Thermo fisher Scientific, Massachusetts, USA).
Previously published nested and PCR-RFLP methods were employed to detect the polymorphisms of pfcrt gene at amino acid residues 76, 220, 271, 326, 356, and 371 [20]; pfmdr1 gene at amino acid residues 86, 184, 1034, 1042, and 1246 [21, 22]; pfatp6 gene at amino acid residues 37, 693, 769, 898 [23]; pfmrp1 gene at amino acid residues 191 and 437 [24]; and pfmrp1 gene at amino acid residues 876, 1390 and 1466 [25].
Detection of pfatp6 and pfmdr1 gene copy number by SYBR Green I real-time PCR
Pfatp6 and pfmdr1 gene copy number in all samples (Figure 1) was determined by SYBR Green I real-time PCR (iCycler™, Bio-Rad, California, USA) using the default thermocycler program: 10min of pre-incubation at 95°C, followed by 40 cycles for 15 sec at 95°C and 1 min at 60°C. The oligonucleotide primers used were those previously designed by Ferreira et al.[26] with modification. Individual real-time PCR reaction was carried out in a 25 μl reaction volume in a 96-well plate containing 2 μl of DNA (50 ng), 1 μM each of sense and antisense primer and 12.5 μl of Platinum™ PCR SuperMix (Invitrogen, California, USA).
The 2-ΔΔCt method of relative quantification was adapted to estimate copy number in P. falciparum genes. The genomic DNA extracted from P. falciparum 3D7 clone known to harbour a single copy of each gene was used as a calibrator, while Pf-β-actin 1 served as the house-keeping gene in all experiments. Dd2 genomic DNA carrying four copies of pfmdr1 was used as a second calibrator. The threshold cycle (Ct) was determined as the increase in reporter signal, which was first detected above baseline. Results were analysed by a comparative Ct method based on the assumption that the target (pfatp6 and pfmdr1) and reference (pf-β-actin 1) genes were amplified with the same efficiency within an appropriate range of DNA concentrations.
The ΔΔCt calculation for the relative quantification of target was as follow: ΔΔCt = (Ct, target gene − Ct, Pf-β- actin1)x − (Ct, target gene − Ct, Pf-β-actin1)y, where x represents unknown sample and y represents P. falciparum 3D7 clone. Results for each sample was expressed as an N-fold change in χ target gene copies, normalized to Pf-β-actin-1 relative to the copy number of the target gene in P. falciparum 3D7 clone, according to the following equation: amount of target = 2-ΔΔCt. A minimum of two experiments were carried out for each gene and each sample. In each experiment, each individual sample was analysed in duplicate wells and the Ct of each well was recorded at the end of the reaction.
Statistical analysis
The association between in vitro sensitivity of P. falciparum isolates and polymorphisms of pfcrt, pfmdr1, pfmrp1, and pfatp6 was analysed using Chi-square and Mann–Whitney U tests. Correlation between the two quantitative variables was evaluated using Spearman correlation test. The qualitative variables are summarized as proportions and percentages and the quantitative variables are summarized as median (95% CI) values. Statistical significance level was set at α = 0.05 for all tests (SPSS version 15; SPSS, Chicago, Illinois, USA).
Results
In vitro sensitivity of Plasmodium falciparum isolates
In vitro sensitivity to AS, MQ, CQ, and QN was successfully evaluated in a total of 119 P. falciparum isolates (Figure 1 and Table 1), 56 and 63 isolates collected during 2006–2007 and 2008–2009, respectively (Figure 1 and Table 2). Isolates with declined sensitivity to AS [median (95% CI) 3.4 (3.1-3.7) nM] were observed in 42% (50 isolates). Fifty-eight per cent (69 isolates) were identified as MQ-resistant [median (95% CI) = 54.1 (46.8-61.4) nM]. Almost all (99.2%, 118 isolates) were identified as moderately and highly CQ-resistant; only one (0.8%) isolate was identified as CQ-sensitive (IC50 values = 9.6 nM). About 13% (16 isolates) were identified as QN-resistant [median (95% CI) = 648.9 (621.2-676.5) nM]. A positive significant correlation was observed between the IC50 values of MQ and AS (r = +0.662; p <0.001), MQ and QN (r = +0.750; p <0.001), and AS and QN (r = +0.625; p <0.001) (Figure 2). There was no significant difference in the IC50 values of all drugs between isolates collected during the two periods. However, the prevalence of QN-resistant isolates collected during 2008–2009 was significantly lower than during 2006–2007 (p = 0.016).
Candidate molecular markers of antimalarial drug resistance in Plasmodium falciparum isolates
Pfatp6 mutation
No mutation in pfatp6 at the target amino acid residues 37, 639 and 769 was found in any isolate (0/87, 0/130, and 0/108 isolate, respectively), whereas the mutation at 898 was detected in six out of 121 (5.0%) isolates. Almost all isolates collected during 2006–2007 (100%) and 2008–2009 (93.7%) carried wild type pfatp6 at the target amino acid residues 37, 639, 769, and 898. There was a significant difference in the prevalence of isolates collected during 2006–2007 (0%, 0/57) and 2008–2009 (9.4%, 6/64) with regard to the mutation at the amino acid residue 898 (p = 0.018).
Pfcrt mutation
Almost all isolates carried mutated pfcrt gene. The prevalence of gene mutation at codons 76T, 220S, 271E, 326S, and 371I was 99.2% (128/129), while the mutation at the codon 356T was 98.4% (127/129).
Pfmdr1 mutation
No mutation in pfmdr1 at the codons 1042D and 1246Y was observed (0/130 and 0/130) in any isolate collected during the two investigation periods. The prevalence of pfmdr1 wild type at the target amino acid residue 86 was significantly higher in isolates collected during 2008–2009 (100%, 73/73) compared with 2006–2007 (94.5%, 52/55) (p = 0.043). The prevalence of pfmdr1 wild type at the target amino acid residue 184 in isolates collected during 2006–2007 and 2008–2009 was 100% (57/57) and 94.5% (69/73), respectively. For the target amino acid residue 1034, mutant, heterozygous mutant and wild type isolates were detected in 15.8% (14/57), 56.6% (34/57) and 24.6% (9/57) of the isolates collected during 2006–2007, respectively. The prevalence of the mutant and heterozygous mutant at the same amino acid target was detected in 98.6 and 1.4% of the isolates collected during 2008–2009, respectively. No wild type isolate was found at this target amino acid. The prevalence of gene mutation at the amino acid residue 1034 was significantly higher in isolates collected between 2008–2009 compared with 2006–2007 (p < 0.001).
Pfmrp1 mutation
No mutation in pfmrp1 at the codon 1466R was observed (0/130) in any isolate collected during both periods. The mutations at amino acid residues 191, 437, 876, and 1390 were detected in 86.9% (113/130), 89.1% (115/129), 74.6% (97/130) and 26.2% (34/130), respectively. The prevalence of isolates with mutations at amino acid residues 191 and 437 collected during 2006–2007 vs 2008–2009 were 84.2% (48/57) vs 89.0% (65/73) and 85.7% (48/56) vs 91.8% (68/73), respectively. The prevalence of isolates with mutations at amino acid residues 876 (p < 0.001) and 1390 (p = 0.037) was significantly higher in 2008–2009 (42.5%, 31/73) compared with 2006–2007 (5.3%, 3/57).
Pfmdr1 copy number
Isolates which carried one, two, three, four, five, six and eight gene copies were found in 48.8% (60/123), 15.4% (19/123), 13.8% (17/123), 17.1% (21/123), 0.8% (1/123), 3.3% (4/123), and 0.8% (1/123), respectively. For the period 2006–2007, the isolates which carried one, two, three and four gene copies were found in 47.4% (27/57), 19.3% (11/57), 12.3% (7/57) and 21.1% (12/57), respectively. About 50% (33/66), 12.1% (8/66), 15.2% (10/66), 13.6% (9/66), 1.5% (1/66), 6.1% (4/66), and 1.5% (1/66) of the isolates collected during 2007–2008 carried one, two, three, four, five, six and eight gene copies, respectively. There was no significant difference in the prevalence of pfmdr1 gene copy in isolates collected during the two periods.
Pfatp6 copy number
All of the 67 isolates under the analysis from the two periods carried only one gene copy.
Association between polymorphisms of candidate molecular markers of anti-malarial drug resistance and in vitro sensitivity of Plasmodium falciparum isolates
The association between polymorphisms of candidate molecular markers of anti-malarial drug resistance and in vitro sensitivity to anti-malarial drugs was investigated in 119 matched-paired P. falciparum isolates (Figure 3).
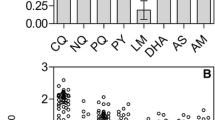
The relationship between median IC 50 values of quinine (QN), mefloquine (MQ) and chloroquine (CQ) and the mutations of pfmdr1 and pfmrp1 gene in Plasmodium falciparum isolates. Association between (A) QN IC50 and pfmdr1 N86Y (p = 0.015, Mann–Whitney U test), S1034C (p = 0.018, Kruskal-Wallis test) and pfmrp1 F1390I mutation (p = 0.039, Mann–Whitney U test); (B) MQ IC50 and pfmdr1 N86Y mutation (p = 0.005, Mann–Whitney U test); and (C) CQ IC50 and pfmrp1 H191Y mutation (p = 0.008, Mann–Whitney U test).
Pfatp6 mutation and pfatp6 copy number
No significant association was observed between pfatp6 mutation including pfatp6 copy number and in vitro sensitivity of P. falciparum isolates to all drugs.
Pfcrt mutation
Significant association was observed between CQ resistance and pfcrt mutations at codons 76T, 220S, 271E, 326S, and 371I. Only one CQ sensitive isolate (IC50 9.6 nM) carried wild type genotype at codons 76, 220, 271, 326, and 371 (p = 0.007).
Pfmdr1 mutation
The IC50 values of MQ and QN were significantly lower in the three (out of 117) isolates with 86Y mutation compared with those carried wild type (86 N) genotype [median (95% CI) MQ IC50: 30.4 (21.9-38.8) vs 8.1 (3.4-9.1) nM, p = 0.005; median (95% CI) QN IC50: 236.3 (195.7-276.9) vs 86.4 (32.2-119.1) nM, p = 0.015). The isolates carrying 1034S had significantly lower QN IC50 than that carrying 1034SC [IC50 (95%CI) 134.3 (46.3-222.6) vs 230.5(168.3-292.7) nM, p = 0.007].
Pfmrp1 mutation
CQ IC50 was significantly lower in isolates carrying 191Y compared with that carrying wild type (H) genotype [median (95% CI) IC50 81.4 (58.2-104.7) and 69.9 (65.0-74.9) nM, respectively; p = 0.008]. The QN IC50 was significantly lower in isolates carrying 1390I compared with that carrying wild type 1390F genotype [median (95% CI) QN IC50: 238.0 (191.0-285.1) vs 190.2 (100.7-279.8), p = 0.039].
Pfmdr1 copy number
A marked difference in IC50 values of AS, MQ and QN was observed among isolates carrying one, two, three, and ≥ four gene copies [median (95% CI) AS IC50: 1.6 (1.3-1.9), 1.8 (1.1-2.5), 2.9 (2.1-3.7) and 3.1 (2.5-3.7) nM, p < 0.001; MQ IC50: 19.2 (15.8-22.6), 37.8 (10.7-64.8), 55.3 (47.7-62.9) and 63.6 (49.2-78.0) nM, p < 0.001; and QN IC50: 183.0 (139.9-226.4), 256.4 (83.7-249.1), 329.5 (206.6-425.5) and 420.0 (475.2-475.6) nM, respectively, p < 0.001]. Significant positive correlation was found between the increased pfmdr1 copy number and in vitro sensitivity of P. falciparum isolates to AS (r = +0.47, p < 0.001), MQ (r = +0.65, p < 0.001), and QN (r = +0.50, p < 0.001), while a significant negative correlation was found with CQ (r = −0.19, p = 0.038) (Figure 4).
Discussion
The present study investigated the relationship between P. falciparum gene polymorphisms (pfatp6, pfcrt, pfmdr1, and pfmrp1) and in vitro sensitivity of P. falciparum isolates to the ACT combination partners AS and MQ, including CQ and QN in a multidrug-resistant area along the Thai-Myanmar border during the two periods (2006–2007 and 2008–2009). Results suggest a significant change in the prevalence and pattern of pfatp6, pfmdr1 and pfmrp1 gene polymorphisms with no change in the in vitro sensitivity profiles of the parasite during the two periods. Decline in sensitivity of P. falciparum to MQ was continuously reported during 1991–1994 when MQ monotherapy was employed in Thailand [27]. However, until a decade after the switch of first-line treatment to AS-MQ combination, high prevalence and intensity of MQ resistance was reported (32%, 46% and 58% during 1998–2005 [28], 2007–2008 [29], and 2006–2009 (the current study), respectively). While evidence of artemisinin resistance was documented in Western Cambodia during the period 2006–2007 [30, 31], sensitivity of P. falciparum isolates in this area to AS during the same period was generally considered satisfactory [18, 29, 32, 33]. Subsequent reports on a decline in AS sensitivity [7, 9] nevertheless, has created a major concern on the future use of AS in combination therapy. Without definite criteria for defining artemisinin resistance, the upper limit of 95% CI of median IC50 value of AS in isolates collected from all patients (2.3 nM) was used as a cut-off level of AS resistance in the present study. Based on this cut-off level, approximately 42% of the isolates were classified as declined sensitivity to AS. The prevalence of isolates with MQ resistance and declined sensitivity to AS observed in the present study were similar to that previously reported (58 vs 57.6% and 42 vs 36.7%, respectively) [34]. This cut-off criteria for defining AS resistance (the upper limit of 95% CI of median IC50 value of AS) was slightly lower in the current study (2.3 nM) compared with the previous study (2.8 nM) [34]. The sensitivity to AS (IC50: 2.0 vs 1.7 nM) and MQ (30.1 vs 34.0) were comparable with that reported in the isolates collected from Cambodia during the same period [35].
It was noted for the improvement of parasite sensitivity in this area to CQ and QN since the introduction of AS-MQ combination in Thailand in 1995. There was even one isolate that was sensitive to CQ. In 1991–1992 and 1994, the degree of CQ resistance in the country was high [median (95% CI) IC50 193.2 (148.24-251.85) and 157.0 (124.11-198.73) nM, respectively] [27], but was improved during the 1997, 1999 and 2004–2009 [median (95% CI) IC50: 157.0 (128.0–193.0), 120.5 (105.7–137.3) and 70.0 (10.0-183.0) nM, respectively] [18, 36, 37]. Molecular analysis in either laboratory or field P. falciparum isolates demonstrated the strong linkage between CQ resistance and pfcrt gene mutations [20, 22, 38]. Susceptibility of the parasite to CQ was also shown in this study to link with pfmrp1 polymorphism, of which the 191Y mutation resulted in increased susceptibility of the parasite to CQ. For QN, a decline in parasite sensitivity to the drug was obviously observed during 1991–1992 and 1994 [mean (95% CI) IC50 576.2 (460.51-720.99) and 403.9 (330.50-493.54) nM, respectively], but was improved during 1997–2008 [18, 36, 37, 39]. A total of 16 isolates were identified as QN resistance, 12 and four isolates collected during 2006–2007 and 2008–2009, respectively.
Pfmdr1 and pfmrp1 appear to be the key genes involved in resistance of P. falciparum to the commonly used anti-malarial drugs. The pfmdr1 86Y mutation leads to increase in susceptibility of the parasite to MQ compared with wild type genotype (IC50 of 8.1 and 30.4 nM, respectively) as well as the structurally related anti-malarial QN (IC50 of 86.4 and 236.3 nM). The results showed low prevalence of 184F allele in parasite isolates collected during the investigation period. The 184F allele was reported to be associated with increased IC50 of MQ. High prevalence of (~86%) of the 184F allele was reported in western Cambodia where the level of MQ resistance was significant. On the other hand, the prevalence of 184F allele in eastern Cambodia was low (~32%), which was also correlated with the reduced level of MQ resistance in this region [40]. Molecular analysis in the current study revealed an obvious involvement of pfmdr1 and pfmrp1 genes with QN-resistant P. falciparum[13, 14, 21, 41]. The pfmdr1 86Y and pfmrp1 1390I mutations resulted in an improvement of sensitivity of the parasite to QN compared with the wild type isolates [(86.4 vs 236.3 nM) and (190.2 vs 238.0 nM), respectively]. On the other hand, the mutation and heterozygous mutation of pfmdr1 1034C resulted in the decreased susceptibility of the parasite to QN (median IC50 of 230.5, 256.9 and 190.3 nM for mutated, heterozygous mutated and wild type genotypes, respectively). Interestingly, the prevalence of pfmrp1 1390 (I) in parasite isolates collected during 2008–2009 was higher than that collected during 2006–2007.
With regard to the pfatp6 polymorphisms, there were no mutations found at codons 37, 639 and 769 in samples collected during 2006–2009. The mutation at codon 898 was found in isolates collected from 2008–2009. Although this residue is silent mutation, this observation may imply on the influence of anti-malarial drug pressure on the parasite during that period. The finding was in agreement with that reported by Jambou and colleges for the isolates in Asia including Thailand [11]. It is noted however that in vitro cultivation may cause the poor fitness of the mutant genotypes, which may explain the observation of almost absence of the mutation in pfatp6 gene in this study [42].
The current results support the role of pfmdr1 amplification in modulating the degree of AS, MQ and QN susceptibility [43, 44] A trend of increasing number of gene copies and increasing IC50 values of AS, MQ and QN was clearly observed. Approximately 51% of the isolates carried pfmdr1 copy number ranging from two to eight copies. The study conducted during 1995–2007, the period of which the clinical efficacy of AS-MQ combination was satisfactory, showed the increase in pfmdr1 copy number from 30% (12/40) in 1996 to 53% (24/45) in 2006 [45]. Besides the high level of initial parasitaemia, prolongation of parasite clearance time and reduced in vitro parasite sensitivity to MQ, treatment failure following AS-MQ combination therapy was also associated with increased pfmdr1 copy number. Parasite isolates collected prior to treatment from patients with recrudescent response were found to carry higher number of pfmdr1 copies compared to those with sensitive response (mean copies of 2.7 vs 1.9). In addition, isolates collected on the day of recrudescence carried higher number of gene copies than the corresponding day 0 samples (mean copies 3.5 vs 2.6) [35]. In a previous study, about 70% of isolates collected from patients with recrudescence response before AS-MQ treatment was shown to carry more than 1 pfmdr1 copy number and increase in pfmdr1 copy number was associated with reduced parasite sensitivity to AS, or resistant to MQ, or both [34]. Although the artemisinin resistance has not been clearly defined in this study, results suggest that both the parasite (reduced in vitro sensitivity and increased pfmdr1 copy number) and host (pharmacokinetic variability) factors might contribute to artemisinin resistance [9, 46].
Conclusions
Based on results of the current observation on in vitro sensitivity and candidate molecular markers of resistance, it is concluded that high prevalence of MQ resistance still remained during the four years’ observation period (2006–2009). In addition, sensitivity of the parasite to AS appeared to be declining. Pfmdr1 gene copy number is the key molecular marker of resistance of P. falciparum isolates in this area to AS-MQ combination therapy.
References
Verdrager J: Epidemiology of the emergence and spread of drug-resistant falciparum malaria in South-East Asia and Australasia. J Trop Med Hyg. 1986, 89: 277-289.
Roper C, Pearce R, Nair S, Sharp B, Nosten F, Anderson T: Intercontinental spread of pyrimethamine-resistant malaria. Science. 2004, 305: 1124-10.1126/science.1098876.
Fontanet AL, Johnston DB, Walker AM, Rooney W, Thimasarn K, Sturchler D, Macdonald M, Hours M, Wirth DF: High prevalence of mefloquine-resistant falciparum malaria in eastern Thailand. Bull World Health Organ. 1993, 71: 377-383.
Nosten F, Luxemburger C, ter Kuile FO, Woodrow C, Eh JP, Chongsuphajaisiddhi T, White NJ: Treatment of multidrug-resistant Plasmodium falciparum malaria with 3-day artesunate-mefloquine combination. J Infect Dis. 1994, 170: 971-977. 10.1093/infdis/170.4.971.
Nosten F, van Vugt M, Price R, Luxemburger C, Thway KL, Brockman A, McGready R, ter Kuile F, Looareesuwan S, White NJ: Effects of artesunate-mefloquine combination on incidence of Plasmodium falciparum malaria and mefloquine resistance in western Thailand: a prospective study. Lancet. 2000, 356: 297-302. 10.1016/S0140-6736(00)02505-8.
Noedl H, Se Y, Sriwichai S, Schaecher K, Teja-Isavadharm P, Smith B, Rutvisuttinunt W, Bethell D, Surasri S, Fukuda MM, Socheat D, Chan Thap L: Artemisinin resistance in Cambodia: a clinical trial designed to address an emerging problem in Southeast Asia. Clin Infect Dis. 2010, 51: e82-e89. 10.1086/657120.
Na-Bangchang K, Karbwang J: Emerging artemisinin resistance in the border areas of Thailand. Expert Rev Clin Pharmacol. 2013, 6: 307-322. 10.1586/ecp.13.17.
Congpuong K, Bualombai P, Banmairuroi V, Na-Bangchang K: Compliance with a three-day course of artesunate-mefloquine combination and baseline anti-malarial treatment in an area of Thailand with highly multidrug resistant falciparum malaria. Malar J. 2010, 9: 43-10.1186/1475-2875-9-43.
Na-Bangchang K, Ruengweerayut R, Mahamad P, Ruengweerayut K, Chaijaroenkul W: Declining in efficacy of a three-day combination regimen of mefloquine-artesunate in a multi-drug resistance area along the Thai-Myanmar border. Malar J. 2010, 9: 273-10.1186/1475-2875-9-273.
Sanchez C, Dave A, Stein W, Lanzer M: Transporters as mediators of drug resistance in Plasmodium falciparum. Int J Parasitol. 2010, 40: 1109-1118. 10.1016/j.ijpara.2010.04.001.
Jambou R, Legrand E, Niang M, Khim N, Lim P, Volney B, Ekala MT, Bouchier C, Esterre P, Fandeur T, Mercereau-Puijalon O: Resistance of Plasmodium falciparum field isolates to in-vitro artemether and point mutations of the SERCA-type PfATPase6. Lancet. 2005, 366: 1960-1963. 10.1016/S0140-6736(05)67787-2.
Dahlstrom S, Ferreira PE, Veiga MI, Sedighi N, Wiklund L, Martensson A, Farnert A, Sisowath C, Osorio L, Darban H, Andersson B, Kaneko A, Conseil G, Björkman A, Gil JP: Plasmodium falciparum multidrug resistance protein 1 and artemisinin-based combination therapy in Africa. J Infect Dis. 2009, 200: 1456-1464. 10.1086/606009.
Raj DK, Mu J, Jiang H, Kabat J, Singh S, Sullivan M, Fay MP, McCutchan TF, Su XZ: Disruption of a Plasmodium falciparum multidrug resistance-associated protein (PfMRP) alters its fitness and transport of antimalarial drugs and glutathione. J Biol Chem. 2009, 284: 7687-7696. 10.1074/jbc.M806944200.
Veiga MI, Ferreira PE, Jornhagen L, Malmberg M, Kone A, Schmidt BA, Petzold M, Bjorkman A, Nosten F, Gil JP: Novel polymorphisms in Plasmodium falciparum ABC transporter genes are associated with major ACT antimalarial drug resistance. PLoS One. 2011, 6: e20212-10.1371/journal.pone.0020212.
Trager W, Jensen JB: Human malaria parasites in continuous culture. Science. 1976, 193: 673-675. 10.1126/science.781840.
Bennett TN, Paguio M, Gligorijevic B, Seudieu C, Kosar AD, Davidson E, Roepe PD: Novel, rapid, and inexpensive cell-based quantification of antimalarial drug efficacy. Antimicrob Agents Chemother. 2004, 48: 1807-1810. 10.1128/AAC.48.5.1807-1810.2004.
Smilkstein M, Sriwilaijaroen N, Kelly JX, Wilairat P, Riscoe M: Simple and inexpensive fluorescence-based technique for high-throughput antimalarial drug screening. Antimicrob Agents Chemother. 2004, 48: 1803-1806. 10.1128/AAC.48.5.1803-1806.2004.
Phompradit P, Wisedpanichkij R, Muhamad P, Chaijaroenkul W, Na-Bangchang K: Molecular analysis of pfatp6 and pfmdr1 polymorphisms and their association with in vitro sensitivity in Plasmodium falciparum isolates from the Thai-Myanmar border. Acta Trop. 2011, 120: 130-135. 10.1016/j.actatropica.2011.07.003.
Wooden J, Kyes S, Sibley CH: PCR and strain identification in Plasmodium falciparum. Parasitol Today. 1993, 9: 303-305. 10.1016/0169-4758(93)90131-X.
Fidock DA, Nomura T, Talley AK, Cooper RA, Dzekunov SM, Ferdig MT, Ursos LM, Sidhu AB, Naude B, Deitsch KW, Su XZ, Wootton JC, Roepe PD, Wellems TE: Mutations in the P. falciparum digestive vacuole transmembrane protein PfCRT and evidence for their role in chloroquine resistance. Mol Cell. 2000, 6: 861-871. 10.1016/S1097-2765(05)00077-8.
Duraisingh MT, Cowman AF: Contribution of the pfmdr1 gene to antimalarial drug-resistance. Acta Trop. 2005, 94: 181-190. 10.1016/j.actatropica.2005.04.008.
Duraisingh MT, Jones P, Sambou I, von Seidlein L, Pinder M, Warhurst DC: The tyrosine-86 allele of the pfmdr1 gene of Plasmodium falciparum is associated with increased sensitivity to the anti-malarials mefloquine and artemisinin. Mol Biochem Parasitol. 2000, 108: 13-23. 10.1016/S0166-6851(00)00201-2.
Ferreira ID, Martinelli A, Rodrigues LA, do Carmo EL, do Rosario VE, Povoa MM, Cravo P: Plasmodium falciparum from para state (Brazil) shows satisfactory in vitro response to artemisinin derivatives and absence of the S769N mutation in the SERCA-type PfATPase6. Trop Med Int Health. 2008, 13: 199-207. 10.1111/j.1365-3156.2007.01991.x.
Holmgren G, Gil JP, Ferreira PM, Veiga MI, Obonyo CO, Bjorkman A: Amodiaquine resistant Plasmodium falciparum malaria in vivo is associated with selection of pfcrt 76 T and pfmdr1 86Y. Infect Genet Evol. 2006, 6: 309-314. 10.1016/j.meegid.2005.09.001.
Pirahmadi S, Zakeri S, Afsharpad M, Djadid ND: Mutation analysis in pfmdr1 and pfmrp1 as potential candidate genes for artemisinin resistance in Plasmodium falciparum clinical isolates 4years after implementation of artemisinin combination therapy in Iran. Infect Genet Evol. 2013, 14: 327-334.
Ferreira I, do Rosário VE, Cravo P: Real-time quantitative PCR with SYBR Green I detection for estimating copy numbers of nine drug resistance candidate genes in Plasmodium falciparum. Malar J. 2006, 5: 1-10.1186/1475-2875-5-1.
Wongsrichanalai C, Wimonwattrawatee T, Sookto P, Laoboonchai A, Heppner D, Kyle D, Wernsdorfer W: In vitro sensitivity of Plasmodium falciparum to artesunate in Thailand. Bull World Health Organ. 1999, 77: 392-398.
Chaijaroenkul W, Bangchang KN, Mungthin M, Ward SA: In vitro antimalarial drug susceptibility in Thai border areas from 1998–2003. Malar J. 2005, 4: 37-10.1186/1475-2875-4-37.
Chaijaroenkul W, Wisedpanichkij R, Na-Bangchang K: Monitoring of in vitro susceptibilities and molecular markers of resistance of Plasmodium falciparum isolates from Thai-Myanmar border to chloroquine, quinine, mefloquine and artesunate. Acta Trop. 2010, 113: 190-194. 10.1016/j.actatropica.2009.10.016.
Dondorp A, Nosten F, Yi P, Das D, Phyo A, Tarning J, Lwin K, Ariey F, Hanpithakpong W, Lee S, Ringwald P: Artemisinin resistance in Plasmodium falciparum malaria. N Engl J Med. 2009, 361: 455-467. 10.1056/NEJMoa0808859.
Noedl H, Se Y, Schaecher K, Smith BL, Socheat D, Fukuda MM: Evidence of artemisinin-resistant malaria in western Cambodia. N Engl J Med. 2008, 359: 2619-2620. 10.1056/NEJMc0805011.
Noedl H, Faiz MA, Yunus EB, Rahman MR, Hossain MA, Samad R, Miller RS, Pang LW, Wongsrichanalai C: Drug-resistant malaria in Bangladesh: an in vitro assessment. Am J Trop Med Hyg. 2003, 68: 140-142.
Woitsch B, Wernsdorfer G, Prajakwong S, Rojanawatsirivet C, Kollaritsch H, Wernsdorfer WH: Comparative study of the in vitro sensitivity of Plasmodium falciparum to artemisinin in two border areas of Thailand. Wiener klinische Wochenschrift. 2004, 116 (Suppl 4): 35-40.
Na-Bangchang K, Muhamad P, Ruaengweerayut R, Chaijaroenkul W, Karbwang J: Identification of resistance of Plasmodium falciparum to artesunate-mefloquine combination in an area along the Thai-Myanmar border: integration of clinico-parasitological response, systemic drug exposure, and in vitro parasite sensitivity. Malar J. 2013, 12: 263-10.1186/1475-2875-12-263.
Rogers WO, Sem R, Tero T, Chim P, Lim P, Muth S, Socheat D, Ariey F, Wongsrichanalai C: Failure of artesunate-mefloquine combination therapy for uncomplicated Plasmodium falciparum malaria in southern Cambodia. Malar J. 2009, 8: 10-10.1186/1475-2875-8-10.
Wongsrichanalai C, Lin K, Pang L, Faiz M, Noedl H, Wimonwattrawatee T, Laoboonchai A, Kawamoto F: In vitro susceptibility of Plasmodium falciparum isolates from Myanmar to antimalarial drugs. Am J Trop Med Hyg. 2001, 65: 450-455.
Attlmayr B, Kollaritsch H, Wernsdorfer W, Miller R, Sirichaisinthop J, Noedl H: Drug sensitivity of Plasmodium falciparum along the Thai-Myanmar border using the new field-deployable HRP2 in vitro assay. Wien Klin Wochenschr. 2005, 117: 35-38.
Djimde A, Doumbo OK, Cortese JF, Kayentao K, Doumbo S, Diourte Y, Dicko A, Su XZ, Nomura T, Fidock DA, Wellems TE, Plowe CV: A molecular marker for chloroquine-resistant falciparum malaria. N Engl J Med. 2001, 344: 257-263. 10.1056/NEJM200101253440403.
Lim P, Wongsrichanalai C, Chim P, Khim N, Kim S, Chy S, Sem R, Nhem S, Yi P, Duong S: Decreased in vitro susceptibility of Plasmodium falciparum isolates to artesunate, mefloquine, chloroquine, and quinine in Cambodia from 2001 to 2007. Antimicrob Agents Chemother. 2010, 54: 2135-2142. 10.1128/AAC.01304-09.
Vinayak S, Alam MT, Sem R, Shah NK, Susanti AI, Lim P, Muth S, Maguire JD, Rogers WO, Fandeur T, Barnwell JW, Escalante AA, Wongsrichanalai C, Ariey F, Meshnick SR, Udhayakumar V: Multiple genetic backgrounds of the amplified Plasmodium falciparum multidrug resistance (pfmdr1) gene and selective sweep of 184 F mutation in Cambodia. J Infect Dis. 2010, 201: 1551-1560. 10.1086/651949.
Sidhu AB, Valderramos SG, Fidock DA: pfmdr1 mutations contribute to quinine resistance and enhance mefloquine and artemisinin sensitivity in Plasmodium falciparum. Mol Microbiol. 2005, 57: 913-926. 10.1111/j.1365-2958.2005.04729.x.
Legrand E, Volney B, Meynard JB, Mercereau-Puijalon O, Esterre P: In vitro monitoring of Plasmodium falciparum drug resistance in French Guiana: a synopsis of continuous assessment from 1994 to 2005. Antimicrob Agents Chemother. 2008, 52: 288-298. 10.1128/AAC.00263-07.
Price RN, Cassar C, Brockman A, Duraisingh M, van Vugt M, White NJ, Nosten F, Krishna S: The pfmdr1 gene is associated with a multidrug-resistant phenotype in Plasmodium falciparum from the western border of Thailand. Antimicrob Agents Chemother. 1999, 43: 2943-2949.
Price RN, Uhlemann AC, Brockman A, McGready R, Ashley E, Phaipun L, Patel R, Laing K, Looareesuwan S, White NJ, Nosten F, Krishna S: Mefloquine resistance in Plasmodium falciparum and increased pfmdr1 gene copy number. Lancet. 2004, 364: 438-447. 10.1016/S0140-6736(04)16767-6.
Carrara VI, Zwang J, Ashley EA, Price RN, Stepniewska K, Barends M, Brockman A, Anderson T, McGready R, Phaiphun L, Proux S, van Vugt M, Hutagalung R, Lwin KM, Phyo AP, Preechapornkul P, Imwong M, Pukrittayakamee S, Singhasivanon P, White NJ, Nosten F: Changes in the treatment responses to artesunate-mefloquine on the northwestern border of Thailand during 13 years of continuous deployment. PLoS One. 2009, 4: e4551-10.1371/journal.pone.0004551.
Krishna S, Kremsner PG: Antidogmatic approaches to artemisinin resistance: reappraisal as treatment failure with artemisinin combination therapy. Trends Parasitol. 2013, 29: 313-317. 10.1016/j.pt.2013.04.001.
Acknowledgements
The study was supported by The Commission on Higher Education, Ministry of Education of Thailand, the National Research University Project of Thailand (NRU), Office of Higher Education Commission, The Royal Golden Jubilee PhD Programme, Thailand Research Fund - Thammasat University Joint Fund and Graduated Student Grant to P. Phompradit, Thammasat University.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
KN was involved in providing the conception, design of the study and revised the manuscript critically for intellectual content and approved the final version of the manuscript. PP, PM and RW performed the investigation on the polymorphisms of pfatp6, pfcrt, pfmdr1 and pfmrp1 genes and in vitro sensitivity test. PP and WC performed data analysis and interpretation. PP drafted the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Phompradit, P., Muhamad, P., Wisedpanichkij, R. et al. Four years’ monitoring of in vitro sensitivity and candidate molecular markers of resistance of Plasmodium falciparum to artesunate-mefloquine combination in the Thai-Myanmar border. Malar J 13, 23 (2014). https://doi.org/10.1186/1475-2875-13-23
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1475-2875-13-23