Abstract
Background
Left ventricular hypertrophy (LVH) is a powerful independent risk factor for cardiovascular morbidity and mortality among hypertensive patients. Data regarding relationships between diabetes and LVH are controversial and inconclusive, whereas possible gender differences were not specifically investigated. The goal of this work was to investigate whether gender differences in left heart structure and mass are present in hypertensive patients with type 2 diabetes.
Methods
Five hundred fifty hypertensive patients with at least one additional cardiovascular risk factor (314 men and 246 women, age 52 to 81, mean 66 ± 6 years), were enrolled in the present analysis. In 200 (36%) of them – 108 men and 92 women – type 2 diabetes mellitus was found upon enrollment. End-diastolic measurements of interventricular septal thickness (IVS), LV internal diameter, and posterior wall thickness were performed employing two-dimensionally guided M-mode echocardiograms. LVH was diagnosed when LV mass index (LVMI) was >134 g/m2 in men and >110 g/m2 in women.
Results
Mean LVMI was significantly higher among diabetic vs. nondiabetic women (112.5 ± 29 vs. 105.6 ± 24, p = 0.03). In addition, diabetic women presented a significantly higher prevalence of increased IVS thickness, LVMI and left atrial diameter on intra-gender comparisons. The age adjusted relative risk for increased LVMI in diabetics vs. nondiabetics was 1.47 (95% CI: 1.0–2.2) in females and only 0.8 (0.5–1.3) in males.
Conclusion
Type 2 diabetes mellitus was associated with a significantly higher prevalence of LVH and left atrial enlargement in hypertensive women.
Similar content being viewed by others
Introduction
Patients with overt diabetes and hypertension are exposed to an exceptionally high risk of cardiovascular death, and are generally thought to need a more intensive risk factor control [1]. Epidemiologic studies have shown that left ventricular hypertrophy (LVH) is the most powerful independent risk factor for cardiovascular morbidity and mortality in these patients. The prevalence of LVH in patients with essential hypertension is in average 40% (range 12% to 70%), depending to a large extent on the measurement technique used [2–6]. The relationships between glucose metabolism abnormalities and LVH have been described in several reports [7–10]. However, the findings were controversial and inconclusive [11]. The gender differences were not specifically investigated in this issue. The goal of this work was to elucidate whether gender differences in left heart structure and mass are present in hypertensive patients with type 2 diabetes.
Patients and methods
The International Nifedipine GITS Study of Intervention as a Goal in Hypertension Treatment (INSIGHT) Trial has studied hypertensive patients with at least one additional cardiovascular risk factor and thus with a clear-cut elevation in overall risk. The design of the INSIGHT study has been described elsewhere [12, 13]. The INSIGHT trial has also conducted a number of side arms in different countries to address several important issues for which information is still limited.
Over the course of 18 months 585 high risk patients with hypertension plus at least one additional risk factor who were recruited to the INSIGHT study in our region underwent echo-Doppler examination. A total of 25 patients dropped out during the recruitment because of the technical reasons (suboptimal echocardiographic images. Therefore, 560 patients (314 men and 246 women, age 52 to 81, mean 66 ± 6 years), were enrolled in the present analysis. In 200 (36%) of them – 108 men and 92 women – type 2 diabetes mellitus found upon enrollment (prevalent diabetes group). The remaining 360 patients without clinically manifested diabetes constituted the nondiabetic group.
The diagnosis of diabetes was made on the basis of the reported history and medical records.
Coronary artery disease (CAD) was diagnosed in accordance with the INSIGHT clinical trial protocol: documented previous myocardial infarction, obstruction equal or more than 70% in at least one of the major epicardial arteries on coronary angiography, percutaneous transcoronary angioplasty or coronary artery bypass grafting, and based on accepted reliable medical records (hospitalization summary and/or coronary angiography protocol.
Echo-Doppler-two dimensional echocardiography
Examinations were performed at baseline with a Hewlett-Packard ultrasound imaging system model SONOS 1000, 1500 or 2500 with a 2.5 and 3.5 Mhz transducer. Standard images were obtained from the left parasternal (long and short axis view), apical (long, two chamber and four chamber) and subcostal views.
Two-dimensionally guided M-mode echocardiograms of the left ventricle (LV) were taken at cordal level, with the patient in partial left decubitus position, and three to five measurements were averaged. End-diastolic measurements of interventricular septal thickness (IVS), LV internal diameter, and posterior wall thickness (PWT) were carried out in accordance with the American Society of Echocardiography recommendations.[14] The left ventricular mass (LVM) was calculated by the formula introduced by Devereux and Reicheck [15] and was indexed for body surface area to obtain the LVM index (LVMI). Left ventricular hypertrophy was diagnosed when LVMI was >134 g/m2 in men and >110 g/m2 in women [16]. Only frames with optimal visualization of interfaces and showing the septum, LV internal diameter and posterior wall simultaneously were used for reading
All studies were recorded on a super-VHS tape and evaluated by 2 cardiologists with expertise in echocardiography, who were blinded to the presence or absence of diabetes. In case of disagreement, a third examiner was consulted
Statistical analysis
Data were analyzed using SAS software [17]. Comparisons of proportions were made using the chi-square test. Statistical analysis for inter- and intra-gender comparisons was performed using the Student's t test. A p value of less than 0.05 was considered statistically significant.
Results
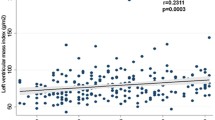
In inter-gender comparisons, men were older; the prevalence of smoking and proven CAD was significantly higher among them. Duration of hypertension was longer among women (Table 1). No inter-gender differences were found regarding systolic and diastolic blood pressures on inclusion. In patients of both genders (intra-gender comparisons) no differences were found regarding age, systolic and diastolic blood pressures on inclusion, duration of hypertension and prevalence of CAD. However, mean LVMI was significantly higher among diabetic women (112.5 ± 29 vs 105.6 ± 24, p = 0.03). Only among diabetic women a significantly higher prevalence of increased IVS thickness, LVMI and left atrial diameter was found on intra-gender comparisons (Table 2, Figures 1, 2, 3). The age adjusted relative risk for increased LVMI in diabetics vs nondiabetics was 1.47 (95% CI: 1.0–2.2) in females and only 0.8 (0.5–1.3) in males.
Discussion
In the present study diabetes mellitus was associated with increased prevalence of LVH (in terms of increased LVMI and IVS) in hypertensive women. LVH is more than just an adaptive response to hypertension. It is predictor a poor prognosis, independently of blood pressure levels. In the Framingham, the relative risk of cardiovascular mortality for every 50 g increment in echo LV mass was 1.73 in men and 2.12 in women, even after correction for risk factors such as blood pressure [2]. In patients with established CAD, the extra risk for cardiac death due to LVH is 2.8, when adjusted for age, gender and hypertension [3]. In these patients, this extra risk due to echo LVH appears to be greater than that for multivessel coronary disease or to LV dysfunction.
Recently, the close relationship between glucose metabolism abnormalities and other cardiovascular risk factors and diseases was emphasized [18–20]. In a previous study, LVH was present in 31% of diabetics, and systolic blood pressure was of no value in identifying those diabetics who had LVH [21], possibly because insulin resistance itself stimulates LVM growth [22]. Verdecchia et al. supposed that in addition to circulating insulin, insulin growth factor-1 is also an independent determinant of LVM and geometry in essential hypertension [9]. However, Galvin et al. concluded that insulin resistance and hyperinsulinemia are not independent predictors of left ventricular mass in humans [11]. In a relatively healthy, population-based sample of hypertensive adults, type 2 diabetes was associated with higher LVM, more concentric LV geometry, and lower myocardial function, independently of age, sex, body size, and arterial blood pressure [10]. In the present study, similarly to Framingham cohort [23], diabetes was associated with higher LV mass in women but not in men. In addition, the prevalence of patients with increased left atrium diameter was significantly higher among diabetic women. We assumed that the latter phenomenon may be associated with increasing left atrial filling pressure following more pronounced LVH-related diastolic dysfunction.
It is well established that diabetic women present a greater risk for cardiovascular morbidity and mortality compared to their male counterparts [24–26]. In this context, our findings could represent an important component of the underlying mechanism.
Whether diabetes is associated with changes in left heart structure independently of blood pressure and metabolic abnormalities remains to be elucidated in large prospective population-based studies.
Conclusion
Type 2 diabetes mellitus was associated with a significantly higher prevalence of LVH and left atrial enlargement in hypertensive women.
Abbreviations
- CAD:
-
coronary artery disease
- INSIGHT:
-
Intervention as a Goal in Hypertension Treatment
- IVS:
-
interventricular septal thickness
- LV:
-
left ventricle
- LVMI:
-
left ventricular mass index
- LVH:
-
left ventricular hypertrophy.
References
Tenenbaum A, Fisman EZ, Boyko V, Goldbourt U, Auerbach I, Shemesh J, Shotan A, Reicher-Reiss H, Behar S, Motro M: Prevalence and prognostic significance of unrecognized systemic hypertension in patients with diabetes mellitus and healed myocardial infarction and/or stable angina pectoris. Am J Cardiol. 1999, 84: 294-298. 10.1016/S0002-9149(99)00279-9.
Levy D, Garrison RJ, Savage DD, Kannel WB, Castelli WP: Prognostic implications of echocardiographically determined LV mass in the Framingham heart study. N Engl J Med. 1990, 322: 1561-1566.
Ghali JK, Liao Y, Simmons B, Castaner A, Cao G, Cooper RS: The Prognostic role of LVH in patients with or without coronary artery disease. Ann Intern Med. 1992, 117: 831-836.
Liao Y, Cooper RS, McGee DL, Mensah GA, Ghali J: The relative effects of LVH, coronary artery disease and ventricular dysfunction on survival among black adults. JAMA. 1995, 273: 1592-1597. 10.1001/jama.273.20.1592.
Okin PM, Devereux RB, Jern S, Kjeldsen SE, Julius S, Nieminen MS, Snapinn S, Harris KE, Aurup P, Edelman JM: Losartan Intervention for Endpoint reduction in hypertension Study Investigations. Regression of electrocardiographic left ventricular hypertrophy by losartan versus atenolol: The Losartan Intervention for Endpoint reduction in Hypertension (LIFE) Study. Circulation. 2003, 108: 684-690. 10.1161/01.CIR.0000083724.28630.C3.
Levy D, Anderson KM, Savage DD, Kannel WB, Christiansen JC, Castelli WP: Echocardiographically detected LVH: prevalence and risk factors: the Framingham heart study. Ann Intern Med. 1988, 108: 7-13.
Sasson Z, Rasooly Y, Bhesania T, Rasooly I: Insulin resistance is an important determinant of left ventricular mass in the obese. Circulation. 1993, 88: 1431-1436.
Watanabe K, Sekiya M, Tsuruoka T, Funada J, Kameoka H: Effect of insulin resistance on left ventricular hypertrophy and dysfunction in essential hypertension. J Hypertens. 1999, 17: 1153-1160. 10.1097/00004872-199917080-00015.
Verdecchia P, Reboldi G, Schillaci G, Borgioni C, Ciucci A, Telera MP, Santeusanio F, Porcellati C, Brunetti P: Circulating insulin and insulin growth factor-1 are independent determinants of left ventricular mass and geometry in essential hypertension. Circulation. 1999, 100: 1802-1807.
Palmieri V, Bella JN, Arnett DK, Liu JE, Oberman A, Schuck MY, Kitzman DW, Hopkins PN, Morgan D, Rao DC: Effect of type 2 diabetes mellitus on left ventricular geometry and systolic function in hypertensive subjects: Hypertension Genetic Epidemiology Network (HyperGEN) study. Circulation. 2001, 103: 102-107.
Galvan AQ, Galetta F, Natali A, Muscelli E, Sironi AM, Cini G, Camastra S, Ferrannini E: Insulin resistance and hyperinsulinemia: No independent relation to left ventricular mass in humans. Circulation. 2000, 102: 2233-2238.
Brown MJ, Castaigne A, Ruilope LM, Mancia G, Rosenthal T, de Leeuw PW, Ebner F: INSIGHT: International nifedipine GITS Study Intervention as a Goal in Hypertension Treatment. J Hum Hypertens. 1996, 10 (suppl 3): 157-160.
Mancia G, Grassi G: The International Nifedipine GITS Study of Intervention as a Goal in Hypertension Treatment (INSIGHT) Trial. Am J Cardiol. 1998, 82: 23R-28R. 10.1016/S0002-9149(98)00753-X.
Sahn DJ, DeMaria A, Kisslo J, Weyman A: Standardization of the American Society of Echocardiography: recommendations regarding quantitation in M-mode echocardiography: results of a survey of echocardiographic measurements. Circulation. 1978, 58: 1072-1083.
Devereux RB, Reicheck N: Echocardiographic determination of left ventricular mass in man. Anatomic validation of the method. Circulation. 1977, 55: 613-618.
Savage DD, Garrison RY, Kannel WB, Levy D, Anderson SJ, Stokes J, Feinleib M, Castelli WP: The spectrum of left ventricular hypertrophy in a general population sample: the Framingham study. Circulation. 1987, 75 (Suppl I): 26-33.
SAS Institute Inc: SAS/STAT User's Guide. Version 6, Cary, NC: SAS Institute Inc. 1989, 2: Fourth
Tenenbaum A, Fisman EZ, Motro M: Metabolic syndrome and type 2 diabetes mellitus: focus on peroxisome proliferator activated receptors (PPAR). Cardiovasc Diabetol. 2003, 2: 4-10.1186/1475-2840-2-4.
Wilson PW, Grundy SM: The metabolic syndrome: practical guide to origins and treatment: Part I. Circulation. 2003, 108: 1422-1424. 10.1161/01.CIR.0000089505.34741.E5.
Fisman EZ, Motro M, Tenenbaum A: Cardiovascular diabetology in the core of a novel interleukins classification: the bad, the good and the aloof. Cardiovasc Diabetol. 2003, 2: 11-10.1186/1475-2840-2-11.
Rana BS, Band MM, Ogston S, Morris AD, Pringle SD, Struthers AD: Relation of QT dispersion to underlying cardiac abnormalities in diabetes mellitus. Am J Cardiol. 2002, 90: 483-487. 10.1016/S0002-9149(02)02518-3.
Phillips RA, Krakoff LR, Dunaif A, Finegood DT, Gorlin R, Schimabukuro S: Relation among LV mass, insulin resistance and BP in non-obese subjects. J Clin Endocrinol Metab. 1998, 83: 4284-4288. 10.1210/jc.83.12.4284.
Galderisi M, Anderson KM, Wilson PW, Levy D: Echocardiographic evidence for the existence of a distinct diabetic cardiomyopathy (the Framingham Heart Study). Am J Cardiol. 1991, 68: 85-89.
Galcera-Tomas J, Melgarejo-Moreno A, Garcia-Alberola A, Rodriguez-Garcia P, Lozano-Martinez J, Martinez-Hernandez J, Martinez-Fernandez S: Prognostic significance of diabetes in acute myocardial infarction. Are the differences linked to female gender?. Int J Cardiol. 1999, 69: 289-298. 10.1016/S0167-5273(99)00048-0.
Marks JB, Raskin P: Cardiovascular risk in diabetes: a brief review. J Diabetes Complications. 2000, 14: 108-115. 10.1016/S1056-8727(00)00065-9.
Hu G, DECODE Study Group: Gender difference in all-cause and cardiovascular mortality related to hyperglycaemia and newly-diagnosed diabetes. Diabetologia. 2003, 46: 608-617.
Acknowledgements
This work was supported in part by the Cardiovascular Diabetology Research Foundation (RA 58-040-684-1), Holon, Israel, and the Research Authority of Tel-Aviv University (grant 01250234).
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
None declared.
Authors' contributions
AT and JS envisioned the concept and prepared the initial draft of the article. AT, EZF and MM carried out the echocardiographic studies. EZF, ES, YA and MM critically revised the manuscript for important intellectual content. MB performed the statistical analysis. All authors read and approved the final version of the manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Tenenbaum, A., Fisman, E.Z., Schwammenthal, E. et al. Increased prevalence of left ventricular hypertrophy in hypertensive women with type 2 diabetes mellitus. Cardiovasc Diabetol 2, 14 (2003). https://doi.org/10.1186/1475-2840-2-14
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1475-2840-2-14