Abstract
Background
We aim to establish the evidence base for the recognition and management of obstetric anal sphincter injury (OASI) and to compare this with current practice amongst UK obstetricians and coloproctologists.
Methods
A systematic review of the literature and a postal questionnaire survey of consultant obstetricians, trainee obstetricians and consultant coloproctologists was carried out.
Results
We found a wide variation in experience of repairing acute anal sphincter injury. The group with largest experience were consultant obstetricians (46.5% undertaking ≥ 5 repairs/year), whilst only 10% of responding colorectal surgeons had similar levels of experience (p < 0.001). There was extensive misunderstanding in terms of the definition of obstetric anal sphincter injuries. Overall, trainees had a greater knowledge of the correct classification (p < 0.01). Observational studies suggest that a new 'overlap' repair using PDS sutures with antibiotic cover gives better functional results. However, our literature search found only one randomised controlled trial (RCT) on the technique of repair of OASI, which showed no difference in incidence of anal incontinence at three months. Despite this, there was a wide variation in practice, with 337(50%) consultants, 82 (55%) trainees and 80 (89%) coloproctologists already using the 'overlap' method for repair of a torn EAS (p < 0.001). Although over 50% of colorectal surgeons would undertake long-term follow-up of their patients, this was the practice of less than 10% of obstetricians (p < 0.001). Whilst over 70% of coloproctologists would recommend an elective caesarean section in a subsequent pregnancy, only 22% of obstetric consultants and 14% of trainees (p < 0.001).
Conclusion
An agreed classification of OASI, development of national guidelines, formalised training, multidisciplinary management and further definitive research is strongly recommended.
Similar content being viewed by others
Background
The importance of highlighting the problem of incontinence to professionals, and the need to focus on reducing underlying causes is emphasised in recent Department of Health documents [1, 2]. Anal incontinence may be defined as 'faecal or flatus incontinence which is a social or hygienic problem' [3]. There is little doubt that vaginal delivery in general, and obstetric anal sphincter injury (OASI) in particular, are significant contributory factors in the development of anal incontinence [4]. In the UK, anal incontinence in the year after birth is thought to affect nearly 40,000 mothers (1 in 20) annually [5–9].
Post-partum anal incontinence may affect mothers psychologically as well as physically but many do not seek medical attention because of embarrassment [10] or because they are easily discouraged from discussing it [1]. In one study only one third of individuals with faecal incontinence had ever discussed the problem with a physician [11]. In recent correspondence to the Continence Foundation, a woman describes 'the eternal shame of being with another person when the worst occurs' [12]. The impact of this complication on the vulnerable postnatal mother and her baby is potentially catastrophic. Aside from the potential clinical and social implications [13] there are important medico-legal issues [14]. Furthermore, the treatment of postpartum anal incontinence itself is associated with very high cumulative costs [15]. Perineal trauma after childbirth is of further importance because it lies behind the growing clamour for the right of a woman to choose whether to deliver by elective caesarean section [16–18].
Obstetric anal sphincter injuries may be seen at the time of birth ('overt') or may be detected only after additional ultrasound investigation, after birth ('occult'). The incidence of 'overt' anal sphincter injury has previously been reported as being between 0.5–3% of vaginal deliveries [19, 20]. Until recently, anal incontinence not due to 'overt' anal sphincter injury was attributed to pelvic neuropathy [21]. The advent of anal endosonography altered this view by identifying further 'occult' obstetric trauma to the anal sphincter. This has been reported in 35% of primiparous women[22, 23] and a significant association has been demonstrated between these sonographic defects and anal incontinence. However, it has not been established whether these injuries were genuinely 'occult' or whether they had been missed by the doctor or midwife at delivery. There is evidence from one study [24] that perineal anatomy is poorly understood by midwives and trainee doctors, who perform the bulk of deliveries in the UK. In this study, 41% of trainees and 16% of midwives incorrectly classified a partial or complete tear of the EAS as 'second degree'. Inconsistency in classification of tears would allow many injuries to pass, unrecognised.
Clearly where an injury occurs, but is not detected, the incidence of anal incontinence may approach 100%. These women will frequently be referred to colorectal surgeons for further evaluation and possible 'secondary' repair. Even with recognition and 'primary' repair, the incidence of anal incontinence has been reported as over 50% [25] and the actual incidence may be even higher [26]. The reasons for the apparently poor outcome after primary repair are not clear, particularly as there is considerable controversy in the literature regarding the optimal obstetric management of OASI. Variation in outcome may be due to different methods and materials being used [27] or to deficiencies in skill and training [24]. Given the sub-optimal outcomes achieved when these injuries are repaired by obstetricians, it has been suggested that better results may be obtained if colorectal surgeons perform the primary surgery [28, 29].
The aims of this study were firstly, to establish the best available evidence for the management of OASI by conducting a systematic review of the literature. Secondly, we aimed to audit current practice amongst trainee and consultant obstetricians. Finally, we wished to explore the views of consultant colorectal surgeons with respect to optimal management of OASI.
Methods
Literature review [30]
The Cochrane Library and Cochrane Register of Controlled Trials were searched for relevant Randomised Controlled Trials (RCT), systematic reviews and meta-analysis. A search of MEDLINE and PUBMED (electronic databases) from 1966 up to April 2001 was also carried out. The databases were searched using the relevant MeSH terms, including all sub-headings and this strategy was combined with a Key-word search using – Human; Female; Childbirth; Obstetric; Perineum; Anal sphincter; Tear; Injury; Rupture; Damage; Incontinence; Faecal; Anal; Repair; Surgery; Sutures; Randomised controlled trials; Meta-analysis. The bibliographies of retrieved articles were searched manually as well as conference proceedings and abstracts from obstetrics and gynaecology and coloproctology meetings.
Survey participants
The study sample included all consultant obstetricians & gynaecologists in the Royal College of Obstetricians & Gynaecologists (RCOG) UK database. As a comprehensive national register of obstetric trainees is unavailable, we surveyed all trainee obstetricians in the two regions in which the authors are based (West Midlands and South West Thames regions). We also included all consultant members of the Association of Coloproctology of Great Britain and Ireland.
Development of a questionnaire
The postal questionnaire that was sent to the consultant and trainee obstetricians enquired about those aspects of knowledge and practice that our preliminary literature review suggested would be linked to outcome. Questions relating to current experience, classification of perineal injury, acute management, follow-up, management of subsequent deliveries and training received were all included. A similar questionnaire inquiring about the management of primary OASI repair was sent to the consultant coloproctologists.
Data processing and analysis
A Freepost envelope was included with the questionnaire. Non-responders received a second questionnaire. Data was entered onto an Access database. The software used for analysis was StatXact Turbo (CYTEL), Cambridge, Massachusetts. The Kruskal-Wallis test was used to compare ordinal data between the 3 groups and chi square tests were applied when the data were nominal.
In order to highlight the differences between current evidence and current practice we have presented the results of our literature search in combination with the results of the survey.
Results
Respondents
At the time of the survey, 1441 names appeared in the RCOG consultant database (UK) of whom 152 were non-practising obstetricians and 96 had retired. Of the 1193 consultants in active obstetric practice, 672 (56%) completed and returned the questionnaire. Of the 235 trainee obstetricians in the West Midlands and South West Thames regions, 148 (63%) completed and returned the questionnaire. Only 90 (23%) of the 385 members of the Association of Coloproctology replied, despite 2 mailings. The overall response rate was 50.2% (910/1813).
The majority of responding consultant obstetricians, 438 (65%) and coloproctologists, 53 (59%) had been in post for more than 5 years. Of the trainee obstetricians-108 (73%) were post-MRCOG.
The average numbers of acute OASI repairs (primary) performed annually by consultant obstetricians, obstetric trainees and colorectal surgeons are shown in Table 1. There were significant differences between the three groups.
Definition of OASI
The evidence
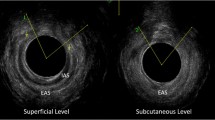
The literature review revealed a lack of consistency in the classification of OASI. One study, which examined all the obstetric texts (n= 65) in the RCOG library, found that 22% of authors classified anal sphincter injury as 'second degree' and a further 17% did not mention any classification [27]. Obstetric anal sphincter injury (OASI) is classified as a '3rd degree' tear when there is any involvement of the external anal sphincter (EAS) but when the anal epithelium is involved it is '4th degree' and this was incorporated in the RCOG guidelines on the management of perineal trauma [31]. The RCOG definitions of perineal injury, which are included in the Green Top Guidelines for the Management of Third and Fourth-Degree Perineal Tears Following Vaginal Delivery are shown in Table 2[32]. A more descriptive classification suggested by Sultan [3] was agreed at a recent consensus meeting on OASI [33] where third degree tears were further classified into three subgroups according to the extent of damage to the external anal sphincter (EAS) and internal anal sphincter (IAS) [3, 32].
The survey
Two hundred and twenty (33%) consultant obstetricians and 30 (22%) trainees considered a complete or partial external sphincter tear to be 'second degree' (Table 3). There was widespread regional variation in the 'misclassification' of OASI as 'second degree'. This is emphasised by a ten-fold difference between some regions (higher in the northern regions) in rates of respondents considering a complete EAS tear to be 'second degree' (Table 4).
Technique of repair following OASI
The evidence
The most common type of repair is an end-to-end repair, where either interrupted or figure-of-eight sutures are inserted into the sphincter muscle. There is little variation on the standard technique reported. One study [34] described the end-to-end approximation of the anal sphincter, by suturing the outer fascial layer without inserting sutures in the muscle. However, this study has not been reproduced. When employed for secondary repair, mobilisation, scar excision and direct apposition lead to an incidence of sphincter repair disruption of 40% [35]. A modification of an overlapping technique for sphincter repair, described by Parks for the secondary repair of OASI [36], was first described for acute OASI by Sultan in 1999 [37]. The technique includes identifying the internal anal sphincter which, if torn, is repaired as a separate layer. Using this technique the authors found a significant reduction in anal incontinence (to 8%), which can be compared with 41%, seen in a previous study where the end-to-end technique was employed [19]. There is only one published, prospective randomised study, comparing end-to-end and the overlap techniques [38]. In this series of 112 primiparous women, no significant difference in continence was identified at 3 months' follow-up. The techniques used in this study were different to those described by Sultan [37]. In particular, internal sphincter injury was not identified and repaired separately. There are two ongoing randomised controlled trials comparing the two methods (in Stoke and Liverpool) registered in the Cochrane clinical trials register [30].
The survey
Coloproctologists favour the overlap technique for primary repair of OASI (Table 5). This technique is reportedly being used by large proportions of obstetricians particularly trainees. Over 55% of responding consultant obstetricians (375/672) and coloproctologists (60/90) said that they would be interested in participating in a trial to compare the two methods of repair.
Suture material
The evidence
No randomised controlled studies to assess the best suture material for sphincter repair were identified. Most texts that describe the repair still mention the use of chromic catgut [27]. However, monofilament suture materials, such as Polydioxanone (PDS) [37] or Polypropelene (Prolene) are thought to be better than catgut or Polyglactin (Vicryl) because of their longer half life. There is good evidence from randomised trials that synthetic materials such as Vicryl or Polyglycolic acid (Dexon) are preferable to catgut for repair of the perineum [39]. Catgut sutures, made from bovine intestinal material, have recently been withdrawn from UK and European countries.
The survey
Vicryl was the material most frequently used for sphincter repair (by 505 (75%) consultant obstetricians and 97 (66%) trainees). By contrast, only 22 (24%) coloproctologists used Vicryl, with greater numbers preferring PDS (41 (46%)). Obstetric experience with PDS was minimal (used by only 51 (8%) consultant obstetricians and 20 (14%) trainees).
Antibiotic usage
The evidence
Intra-operative and post-operative broad spectrum antibiotics are recommended because the development of infection may be linked to a breakdown of the anal sphincter repair [33, 40]. Although data exists relating to antibiotic prophylaxis in colorectal surgery [41] there are no randomised controlled studies which examine antibiotic use following OASI repair.
The survey
Peri-operative antibiotics were recommended by 82 (91%) coloproctologists and by 528 (79%) consultant obstetricians and 130 (88%) obstetric trainees.
Stool softeners
The evidence
A passage of a hard bolus of stool may disrupt repair and therefore most surgical textbooks and experts recommend use of laxatives. However the use of laxatives and stool softeners after OASI repair has not been evaluated in a randomised controlled trial. Indeed medical 'bowel confinement' practised by some colorectal surgeons following secondary anal sphincter repair, has been shown in a randomised trial to confer no benefit in terms of septic complications or functional outcomes [42].
The survey
Stools softeners or laxatives were advised by 70 (78%) coloproctologists. Six hundred and eighteen (94%) consultants and 121 (82%) trainee obstetricians routinely prescribed laxatives following repair.
Colostomy
The evidence
In a recent report comprising of 4 patients, temporary defunctioning colostomy has been described when failure to recognise and repair rectal mucosal injury lead to significant early perineal contamination [43]. We could find no studies to support colostomy in the management of acute OASI. A small randomised trial showed no conclusive evidence that a defunctioning stoma confers any benefit for those patients undergoing secondary repair in terms of functional outcome and may be associated with higher morbidity and longer hospital stays related to the stoma closure [44].
The survey
Twenty-seven (30%) coloproctologists recommend a covering colostomy for third and fourth degree tears (of whom 25 said 'only for 4th degree tears'). None of the obstetricians either performed or requested a colostomy for acute OASI.
Follow-up
The evidence
There are no controlled trials comparing different protocols. We found two publications suggesting that all women with OASI should be followed-up by coloproctologists [28, 29]. At a recent consensus meeting on OASI [33] follow up in a multidisciplinary clinic was recommended for women with persistent bowel symptoms after delivery.
The survey
Coloproctologists suggest a follow-up period of more than 12 months, compared to the majority of obstetricians who follow-up patients for only six weeks (Table 6).
Management of subsequent delivery
The evidence
There were no data in the literature from controlled studies regarding the best mode of subsequent delivery following OASI. Evidence that women who experience even transient anal incontinence after vaginal delivery may be at increased risk of faecal incontinence after a further vaginal delivery has lead to calls that such women should be offered caesarean section. However, compared with vaginal delivery caesarean section carries a higher mortality and other forms of morbidity and should therefore not be offered routinely to all women [45]. In the prospective study from Fynes and colleagues [46], women with transient anal incontinence or occult sphincter injury after first delivery were at high risk of faecal incontinence after a second vaginal delivery. Furthermore it is not clear whether or not pregnancy per se influences postpartum anal incontinence. Symptomatic anal incontinence has been reported after both elective and emergency caesarean deliveries.[9, 47, 48] An alternative approach may be to routinely assess function by means of a continence questionnaire, anorectal physiology tests and endosonography and selectively offer caesarean section to those women with some degree of compromised function. Clearly those who have had successful continence surgery should be delivered by caesarean section [45]. However it remains to be established whether caesarean section would be beneficial to pregnant women with severe incontinence who are due to have continence surgery some time after delivery.
The survey
In the present survey most coloproctologists recommended caesarean section. By contrast most obstetricians allowed vaginal delivery after a previous OASI. (Table 7)
Role of the coloproctologist in the management of OASI
The evidence
Although some authors suggest that coloproctologists are best trained to repair OASI, there are no data to support this statement and the debate continues [13, 28, 29].
The survey
In the present survey only small numbers of consultants (103 (15%)), and fewer trainees (5 (3%)), called a coloproctologist or a general surgeon to assist during acute OASI repair, the indication in these cases being 'severe anatomical disruption'. Few of the respondents believed that a coloproctologist should be routinely involved in acute management of OASI; 17 (19%) coloproctologists, 169 (25%) consultants and 16 (11%) trainees).
Training received in the management of OASI
The evidence
There are no research studies comparing different methods of training. There is only one study that has evaluated training in repair of OASI [24]. Ninety four percent reported unsatisfactory training at the time of performing their first unsupervised OASI repair.
The survey
445 (64%) consultants and 184 (64%) trainees reported either 'a lack of' or 'unsatisfactory' training in the management of OASI.
Discussion
Our literature review and national survey have shown that obstetric anal sphincter injury is an area of childbirth that has been largely ignored, in both research and educational terms. There is a poor evidence base for practice and there has been only one published randomised controlled trial in this area. Our survey had a good obstetric response rate but a poor response from the colorectal surgeons (this may be attributed to the fact that, only about one third of coloproctologists have a specialised interest in anorectal incontinence). Our survey shows wide variation within specialities, levels of seniority and different regions of the country. These findings were echoed at a national professional consensus which highlighted the importance of research into anal incontinence, including the problems of failed recognition and uncertainty about the best method of repair [33].
There are two probable reasons for the underestimation of OASI. Firstly, as a result of lack of a consistent classification, OASI can be wrongly classified as a 2nd degree tear and therefore managed inappropriately. We found that 33% of consultants and 22% of trainees classified a partial or complete tear of the EAS as 'second degree' which echoes the previous smaller study by Sultan [24]. One reason for misclassification may be a degree of confusion created by popular obstetric texts [27]. Our analysis of the regional trends in classification (Figure 1) indicates that more consultants in the Northern regions of the country prefer to classify OASI as 2nd degree. This may reflect the teaching in a popular obstetric textbook [49]. To avoid confusion we support the unified and descriptive classification given by Sultan [3] in which third degree tears are further sub-classified into 3a (less than 50% of thickness of external sphincter torn), 3b (more than 50% of thickness of external sphincter torn) and 3c (internal sphincter torn).
Secondly, underestimation may be due to lack of recognition of OASI because of lack of training. A recent study [50] has shown that immediate assessment of all perineal tears following childbirth by a trained and experienced obstetrician can significantly increase the detection rate. In this study, rates of up to 15% were found, which might provide an explanation for the high incidence of 'occult' sphincter defects reported in previous prospective studies [22, 23]. We have recently presented national data showing nearly a hundred fold variation in detection rates of OASI [51].
The reason for the poor outcome following repair can be attributed to inappropriate technique or to lack of operator expertise or to a combination of these factors. Despite a primary repair of acute obstetric anal sphincter injury, up to 59% of women suffer from persistent anal incontinence [26] and persistent sonographic sphincter defects have been identified in over 80% [19, 52]. Anal incontinence may present for many years following OASI and can also deteriorate with time. Schofield and Grace [14] have looked at the differential rates of the components of anal incontinence (faecal incontinence and flatus and urgency) in five studies which examined these outcomes after primary repair of third degree tears. The intervals of follow-up ranged from 6 weeks to 10 years. The overall mean rates were 25% (flatus +/- urgency) and 9% (faecal incontinence). The longer the follow-up, the higher the rate of incontinence. We have identified another 11 studies with long term follow-up (a mean of 41 months) after 3rd degree tears and 20 to 59% (mean 40%) reported anal incontinence symptoms [53].
Responses to this national survey showed the principle area of disagreement to be 'the optimal method of repair'. However, the fact that half of all obstetricians now claim to be using the 'overlapping' method suggests that there is a change in practice taking place, despite the absence of good quality evidence to support this. Given that untutored use of the overlap method could potentially increase morbidity (as it requires more dissection and mobilisation prior to repair and could also result in a sphincter which is too tight), this may be considered an area of concern. In a recent 5 year follow-up study of incontinent women who had a secondary overlapping repair for obstetric trauma [54], although 50% improved only 4 of 38 patients were totally continent. The overall success of the overlap method 'seemed to deteriorate with time'. The authors wondered whether the technique itself contributed to this deterioration. Clearly there is an urgent need for further properly controlled trials of method of repair, with adequate long-term follow-up. As shown in our survey, there is a widespread interest in participating in a controlled trial in this area. If advantage is taken of this 'window of opportunity', considerable benefits for women should arise.
The finding that only one third of UK consultant obstetricians reported that they were adequately trained to perform anal sphincter repairs requires further attention as this may well have serious clinical and medico-legal implications [14]. We believe that obstetricians need more intensive and focused training in OASI and repair. A series of hands-on-workshops in the management of OASI, utilising a specifically designed model and animal models, has been initiated at St George's Hospital, London. Although it has been suggested that as colorectal surgeons are trained to perform a secondary sphincter repair they should be performing the primary repairs, there was little evidence that current systems could support such a significant change in organisation. Indeed, our survey showed that most coloproctologists have little or no experience of managing acute OASI. A lack of understanding of the circumstance of childbirth by coloproctologists may explain why 30% believed that a colostomy is appropriate management. Further interdisciplinary co-operation is clearly required.
It is apparent from our survey that most obstetricians use Vicryl sutures and antibiotics, and prescribe stool softeners after repair. The ideal suture material for primary sphincter repair is not known although good results have been described using a delayed absorbable monofilament material such as PDS [37] and some surgeons prefer prolene. Further research in this area is required.
Given the large proportions of women who may suffer impaired anal continence even following repaired OASI, it is imperative to establish a system for follow-up. Further research into the most efficient and effective systems is required. Increasing awareness amongst women and community health professionals about the possible sequelae of OASI is important and easy access for appropriate follow-up and further investigation is essential. There is no evidence to indicate the ideal and safest mode of subsequent delivery. Until further research has been undertaken individual cases will need to be managed empirically. Where there has been secondary surgery or where symptoms have taken some time to improve the threshold for elective caesarean section will be lower.
Conclusions
To encourage women to consider vaginal delivery positively, adverse outcomes need to be minimised. The results of our literature review and professional survey are informing the development of national guidelines based on current available best evidence [32]. Support for research in this area has a broad mandate and reflects a need noted by both the research community and the research consumer [55]. Randomised controlled trials of overlap versus end-to-end repair are currently underway [30]. It is clearly of great importance that this research is supported and that further studies addressing the detail on training, prevention, recognition and management of OASI are commenced.
Appendix
What is known about the subject / What the paper adds
Appendix see Additional File: Appendix Anal Sphincter Paper
References
Department of Health: Good practice in continence services. London, Department of Health. 2000
Health outcome indicators: normal pregnancy and childbirth. Report of a working group to the Department of Health. Edited by: Troop P, Goldacre M, Mason A, Cleary R. 1999, Oxford, National Centre for Health Outcomes Development.
Sultan AH: Clinical Focus:ric perineal injury and faecal incontinence after childbirth – Editorial: Obstetrical perineal injury and anal incontinence. Clinical Risk. 1999, 5: 193-196.
Assassa R, Williams K, et al: Evaluation of services for urinary dysfunction. MRC Clinical Trials Directory. 2000, 74.
Macarthur C, Lewis M, Knox EG: Health after childbirth: an investigation of long term health problems beginning after childbirth in 11701 women. London: HMSO,. 1991, 83-103.
Glazener CMA, Abdalla M, Stroud P, Naji S, Templeton A, Russell IT: Postnatal maternal morbidity: extent, causes, prevention and treatment. Br J Obstet Gynaecol. 1995, 102: 282-287.
Glazener CMA: Sexual function after childbirth: women's experiences, persistent morbidity and lack of professional recognition. Br J Obstet Gynaecol. 1997, 104: 330-335.
Glazener CMA, Lang G, Wilson PD, Herbison GP, Macarthur C, Gee H: Postnatal incontinence: a multicentre randomised controlled trial of conservative treatment. Br J Obstet Gynaecol. 1998, 105 (117): 47.
Clarkson J, Newton C, Bick D, Gyte G, Kettle C, Newburn M, et al: Achieving sustainable quality in maternity services – using audit of incontinence and dyspareunia to identify shortfalls in meeting standards. BMC Pregnancy and Childbirth. 2001, 1: 4-10.1186/1471-2393-1-4.
Leigh RJ, Turnberg LA: Fecal incontinence: the unvoiced symptoms. Lancet. 1982, 1 (8285): 1349-1351. 10.1016/S0140-6736(82)92413-8.
Johanson JF, Lafferty J: Epidemiology of fecal incontinence: the silent affliction. American Journal of Gastroenterology. 1996, 91 (1): 33-6.
The Continence Foundation: Incontinence: a challenge and an opportunity for primary care. London, The Continence Foundation. 2000
Sultan AH, Kamm MA: Faecal incontinence after childbirth. Br J Obstet Gynaecol. 1997, 104 (9): 979-982.
Schofield PF, Grace R: Faecal Incontinence after childbirth. Clinical Risk. 1999, 5: 201-204.
Mellgren A, Jenson RN, Zetterstrom JP, Hofmeister JH, Wong WD, Lowry AC: Long term cost of faecal incontinence secondary to obstetric injuries. DIS Colon Rectum. 1998, 41: A54-A55.
Al-Mufti R, McCarthy A, Fisk NM: Obstetricians' personal choice and mode of delivery. The Lancet. 1996, 347: 544-10.1016/S0140-6736(96)91176-9.
Johanson RB, El-Timini S, Rigby C, Young PF, Jones PW: Caesarean section by choice could fulfil the inverse care law. European Journal of Obstetrics, Gynecology and Reproductive Biology. 2001, 97: 20-22. 10.1016/S0301-2115(01)00424-9.
Jarvis GJ: Perineal damage following childbirth. AVMA Medical & Legal Journal. 1999, 181-185.
Sultan AH, Kamm MA, Hudson CN, Bartram CI: Third degree obstetric anal sphincter tears: risk factors and outcome of primary repair. BMJ. 1994, 308: 887-891.
Tetzschner T, Sorenson M, Lose G, Christiansen J: Anal and urinary incontinence in women with obstetric anal sphincter rupture. Br J Obstet Gynaecol. 1996, 103 (1034): 1040.
Snooks SJ, Setchell M, Swash M, Henry MM: Injury to the innervation of the pelvic floor sphincter musculature in childbirth. Lancet. 1984, 1: 546-550. 10.1016/S0140-6736(84)90766-9.
Sultan AH, Kamm MA, Hudson CN, Thomas JM, Bartram CI, Chir M: Anal sphincter disruption during vaginal delivery. New England Journal of Medicine. 1993, 329 (26): 1905-1911. 10.1056/NEJM199312233292601.
Donnelly V, Fynes M, Campbell D, Johnson H, O'Connell PR, O'Herlihy C: Obstetric events leading to anal sphincter damage. Obstet Gynecol. 1998, 92 (6): 955-961. 10.1016/S0029-7844(98)00255-5.
Sultan AH, Kamm MA, Hudson CN: Obstetric perineal trauma: an audit of training. Journal of Obstetrics & Gynaecology. 1995, 15: 19-23.
Fitzpatrick M, Fynes M, Cassidy M, Behan M, O'Connell PR, O'Herilhy C: Prospective study of the influence of parity and operative technique on the outcome of primary anal sphincter repair following obstetrical injury. European Journal of Obstetrics and Gynecology and Reproductive Biology. 2000, 89: 159-163. 10.1016/S0301-2115(99)00200-6.
Goffeng AR, Andersch B, Andersson M, Berndtsson I, Hulten L, Oresland T: Objective methods cannot predict anal incontinence after primary repair of extensive anal tears. Acta Obstet Gynecol Scand. 1998, 77 (4): 439-443. 10.1034/j.1600-0412.1998.770415.x.
Sultan AH, Thakar R: Lower genital tract and anal sphincter trauma. Bailliere's Best Practice & Research – Clinical Obstetrics and Gynaecology.
Walsh CJ, Mooney EF, Upton GJ, Motson RW: Incidence of third-degree perineal tears in labour and outcome after primary repair. Br J Surg. 1996, 83: 218-221. 10.1046/j.1365-2168.1996.02043.x.
Cook TA, Mortenson NJMC: Management of faecal incontinence following obstetric injury. Br J Surg. 1998, 85: 293-299. 10.1046/j.1365-2168.1998.00693.x.
Methods of repair for obstetric anal sphincter injury [Protocol]. In: The Cochrane Library, Issue 4, 2001. Oxford: Update Software. Oxford: Update Software,. 2000
Kettle C, Johanson RB: RCOG Green Top Guidelines: Materials and methods used in perineal repair. RCOG. 2000
Adams EJ, Fernando RJ: RCOG Green Top Guidelines: Management of third and fourth degree perineal tears following vaginal delivery. 2001 en Top Guidelines. 2001
Keighley MRB, Radley S, Johanson R: Consensus on prevention and management of post-obstetric bowel incontinence and third degree tear. Clinical Risk. 2000, 6: 231-237.
Fulsher RW, Fearl CL: The third degree lacerations in modern obstetrics. Am J Obstet Gynecol. 1955, 69: 786-793.
Blaisdell PC: Repair of the incontinent sphincter ani. Surg Gynecol Obstet. 1940, 70: 692-697.
Parks AC, McPartlin JF: Late repair of injuries of the anal sphincter. Proceedings of The Royal Society of Medicine. 1971, 64: 1187-1189.
Sultan AH, Monga AK, Kumar D, Stanton SL: Primary repair of obstetric anal sphincter rupture using the overlap technique. Br J Obstet Gynaecol. 1999, 106 (4): 318-323.
Fitzpatrick M, Fynes M, Cassidy M, Behan M, O'Connell PR, O'Herlihy C: A randomised controlled trial of primary repair of third degree perineal tears, comparing overlap and approximation techniques. Am J Obstet Gynecol. 2000, 183: 1220-1224. 10.1067/mob.2000.108880.
Kettle C, Johanson RB: Absorbable synthetic versus catgut suture material for perineal repair (Cochrane Review). In: The Cochrane Library, Issue 4, Oxford: Update Software. 2001
Venkatesh KS, Ramanujam PS, Larson DH, Haywood NA: Anorectal complications of vaginal delivery. DIS Colon Rectum. 1989, 32: 1039-1041.
Keighley MRB, Williams NS: Sepsis and the use of antibiotic cover in colorectal surgery. In: Surgery of the colon rectum and anus. Edited by: Keighley MRB, Williams NS. 1999, London: Harcourt Brace & Co, 105-135.
Nessim A, Wexner SD, Agachan F, Alabaz O, Weiss EG, Nogueras JJ, et al: Is bowel confinement necessary after anorectal reconstructive surgery?. DIS Colon Rectum. 1999, 42: 16-23.
Cook TA, Deane D, Mortenson NJMcC: Is there a role for a colorectal team in the management of severe third degree vaginal tears. Colorectal Disease. 1999, 1: 263-266. 10.1046/j.1463-1318.1999.00083.x.
Hasegawa H, Yoshioka K, Keighley MRB: Randomised trial of faecal diversion for sphincter repair. DIS Colon Rectum. 2000, 43: 961-965.
Sultan AH, Stanton SL: Preserving the pelvic floor and perineum during childbirth – elective caesarean section?. Br J Obstet Gynaecol. 1996, 103: 731-734.
Fynes M, Donnelly V, Bohan M, O'Connoll PR, O'Herlihy C: Effect of second vaginal delivery on anorectal physiology and faecal continence: a prospective study. The Lancet. 1999, 354: 983-986. 10.1016/S0140-6736(98)11205-9.
Lal M, Mann C, Callender R, Radley S: Patterns of faecal incontinence following normal vaginal delivery, elective and emergency caesarean section. Colorectal Disease. 2000, 2: 178-178. 10.1046/j.1463-1318.2000.00160.x.
Macarthur C, Bick DE, Keighley MRB: Faecal incontinence after childbirth. Br J Obstet Gynaecol. 1997, 104: 46-50.
Donald I: Practical Obstetric Problems. Practical Obstetric Problems. London: Lloyd Luke. 1979, 811.
Groom KM, Paterson-Brown S: Third degree tears: are they clinically underdiagnosed?. Gastroenterology International. 2000, 13 (2): 76-76.
Johanson RB, Fernando RJ, Kettle C, Sultan A, Radley S, Lucking L, et al: The 'Repair' Survey of the incidence of 3rd degree perineal tears in UK hospitals. Proceedings of 29th British Congress of Obstetricians & Gynaecologists, Birmingham. 2001
Poen AC, Felt-Bersma RJF, Dekker GA, Deville W, Cuesta MA, Meuwissen SGM: Third degree obstetric perineal tears: risk factors and the preventative role of mediolateral episiotomy. Br J Obstet Gynaecol. 1997, 104: 563-566.
Sultan AH: Primary and secondary anal sphincter repairs. In, Female pelvic reconstructive surgery. Edited by: Stanton SL and Zimmer PE. 2001, Springer: London.
Malouf AJ, Norton CS, Engel AF, Nicholls RJ, Kamm MA: Long-term results of overlapping anal-sphincter repair for obstetric trauma. The Lancet. 2000, 355: 260-265. 10.1016/S0140-6736(99)05218-6.
Tallon D, Chard J, Dieppe P: Relation between agendas of the research community and the research consumer. Lancet. 2000, 355: 2037-2040. 10.1016/S0140-6736(00)02351-5.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1472-6963/2/9/prepub
Acknowledgements
This paper is dedicated to Richard Johanson, who died a few months before publication. General and Kidney Research Fund, Graduate Medical Centre, Queen's Hospital, Burton on Trent and REMEDI for the funding the survey.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
None declared.
Authors' contributions
This study was conceived by RF, RJ, AS and SR. RF, RJ, AS, SR and PJ contributed to the design of the study. RF carried out the survey and data collection. RF and PJ analysed the data. The paper was written jointly by all authors. RF and RJ act as guarantors for this paper.
Electronic supplementary material
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Fernando, R.J., Sultan, A.H., Radley, S. et al. Management of obstetric anal sphincter injury: a systematic review & national practice survey. BMC Health Serv Res 2, 9 (2002). https://doi.org/10.1186/1472-6963-2-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1472-6963-2-9