Abstract
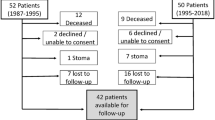
PURPOSE: The aim of this study was to assess any differences between the inclusion or omission of medical bowel confinement relative to postoperative morbidity and patient tolerance after anorectal reconstructive surgery. METHODS: Between January 1995 and February 1997 a prospective randomized trial was conducted for patients without stomas who underwent anorectal reconstructive surgery. All patients were randomly assigned either to medical bowel confinement (a clear liquid diet with loperamide 4 mg by mouth three times per day and codeine phosphate 30 mg by mouth four times per day until the third postoperative day) or to a regular diet, beginning the day of surgery. All patients in both groups underwent the identical preoperative oral mechanical preparation, preoperative oral and parenteral antibiotics, and postoperative antibiotics. Wound closure and wound care were identical in both groups. RESULTS: Fifty-four patients (46 females) were prospectively, randomly assigned to medical bowel confinement (n=27; 50 percent) or a regular diet (n=27; 50 percent); the mean ages were 51.0 (range, 28–80) and 47.2 (range, 23–87) years, respectively. Indications for surgery were fecal incontinence in 32 patients, complicated fistulas in 17 patients, anal stenosis in 4 patients, a Whitehead deformity in 1 patient, and a chronic unhealed fissure in 1 patient. Fifty-four patients underwent 55 procedures: 32 patients underwent sphincteroplasty, 18 patients underwent transanal advancement flaps, and 5 patients underwent anoplasties. There were no differences between the two groups in the incidence of either septic or urologic complications. Nausea and vomiting were recorded in seven (26 percent) medical bowel confinement and three (11 percent) regular-diet patients. The first postoperative bowel movement occurred at a mean of 3.9 days in the medical bowel confinement group and 2.8 days in the regular diet group (P<0.05). Fecal impaction occurred in seven (26 percent) of the patients in the medical bowel confinement group and two (7 percent) of the patients in the regular diet group. Hospital charges analysis showed a mean cost of hospitalization of $12,586.00 (range, $3,436.00−$20,375.00) for the medical bowel confinement group and $10,685.00 (range, $3,954.00−$18,574.00) in the regular diet group, representing a mean difference of $1,901.00 (P=0.06). Mean follow-up was 13 months for both groups (range, 1–24 months in the regular diet group and 2–25 months in the medical bowel confinement group). No statistical difference was shown in the functional outcome of sphincteroplasties between the medical bowel confinement group and the regular diet group. CONCLUSIONS: The outcome of reconstructive anorectal surgery was not adversely affected by the omission of medical bowel confinement. Moreover, cost savings can be achieved by the omission of routine bowel confinement.
Similar content being viewed by others
References
Asbury WH, Hooks VH, DiPiro JT, Bowden TA Jr. Use of oral opiates and diet modification as an alternative to surgical colostomy after complex anorectal procedures. Clin Pharm 1987;6:649–51.
Gordon PH. The chemically defined diet and anorectal procedures. Can J Surg 1976;19:511–3.
Cherry DA, Greenwald NM. Anal incontinence. In: Beck DE, Wexner SD, eds. Fundamentals of anorectal surgery. New York: McGraw-Hill, 1992:104–30.
Yajko RD, Norton LW, Bloemendal L,et al. Morbidity of colostomy closure. Am J Surg 1976;132:304–6.
Dolan PA, Caldwell FT, Thompson CH,et al. Problems of colostomy closure. Am J Surg 1979;137:188–91.
Palmer KR, Corbett CL, Holdsworth CD. Double-blind cross over study comparing loperamide, codeine and diphenoxylate in the treatment of chronic diarrhea. Gastroenterology 1980;79:1272–5.
Jones IT, Fazio VW, Jagelman DG. The use of transanal rectal advancement flaps in the management of fistulas involving the anorectum. Dis Colon Rectum 1987;30:919–23.
Ctercteko GC, Fazio VW, Jagelman DG, Lavery IC, Weakly FL, Melia M. Anal sphincter repair: a report of 60 cases and review of the literature. Aust N Z J Surg 1988;58:703–10.
Wexner SD, Marchetti F, Jagelman DG. The role of sphincteroplasty for fecal incontinence reevaluated: a prospective physiologic and functional review. Dis Colon Rectum 1991;34:22–30.
Jorge JM, Wexner SD. Etiology and management of fecal incontinence. Dis Colon Rectum 1993;36:77–97.
Cohen SM, Wexner SD, Binderow SR,et al. A prospective, randomized, endoscopic-blinded trial comparing precolonoscopy bowel cleansing methods. Dis Colon Rectum 1994;37:689–96.
Oliveira L, Wexner SD, Daniel N,et al. Mechanical bowel preparation for elective colorectal surgery: a prospective, randomized, surgeon-blinded trial comparing sodium phosphate and polyethylene glycol based oral lavage solutions. Dis Colon Rectum 1997;40:585–91.
Abbott WO, Pendergrass EP. Intubation studies of the human small intestine: V. The motor effects of single clinical doses of morphine sulphate in normal subjects. Am J Roentgenol 1936;35:289–99.
Goodman, Gilman A, Rall TW, Nies AS, Taylor P. Antidiarrheal agents. In: Goodman and Gilman's the pharmacologic basis of therapeutics, 8th ed. New York: Pergamon Press, 1990:924–5.
Harford WV, Krejs GJ, Santa Ana CA, Fordtran JS. Acute effect of diphenoxylate with atropine (Lomotil) in patients with chronic diarrhea and fecal incontinence. Gastroenterology 1980;78:440–3.
Physician's desk reference, 47th ed. Montvale, NJ: Medical Economics Data, 1993:2265.
Yagasaki O, Suzuki H, Sohji Y. Effects of loperamide on acetylcholine and prostaglandin release from isolated guinea pig ileum. Jpn J Pharmacol 1978;28: 8:73–82.
Sentovich SM, Falk PM, Christensen MA, Thorson AG, Blatchford GJ, Pitsch RM. Operative results of house advancement anoplasty. Br J Surg 1996;83:1242–4.
Abcarian H. Anal stricture (stenosis). In: Cameron JL, ed. Current surgical therapy, 2nd ed. St. Louis: Mosby-Year Book, 1986:139–43.
Fleshman JW. Fissure in ano and anal stenosis. In: Beck DE, Wexner SD, eds. Fundamentals of anorectal surgery. New York: McGraw-Hill, 1992:170–82.
Pearl RK, Hooks VK III, Abcarian H, Orsay CP, Nelson RL. Island flap anoplasty for the treatment of anal stricture and mucosal ectropion. Dis Colon Rectum 1990;33:581–3.
Christensen MA, Pitsch RM Jr, Cali RL, Blatchford GJ, Thorson AG. “House” advancement pedical flap for anal stenosis. Dis Colon Rectum 1992;35:201–3.
Lowry AC. Rectovaginal fistulas. In: Beck DE, Wexner SD, eds. Fundamentals of anorectal surgery. New York: McGraw-Hill, 1992:145–56.
Lewis P, Bartolo DC. Treatment of trans-sphincteric fistulae by full thickness anorectal advancement flaps. Br J Surg 1990;77:1187–9.
Abrams AA. Anal incontinence. In: Cameron JL, ed. Current Surgical Therapy, 4th ed. St. Louis: Mosby-Year Book, 1992:239–44.
Morgado Nieves P, Gonzales Valles T, Aranguren G, Maldonado D. Gracilis muscle transplant for correction of traumatic anal incontinence: report of a case. Dis Colon Rectum 1975;18:349–54.
Fang DT, Nivatvongs S, Vermeulen FD, Herman FN, Goldberg SM, Rothenberger DA. Overlapping sphincteroplasty for acquired anal incontinence. Dis Colon Rectum 1984;27:720–2.
Ingham CL, Rihani H., Nicholls RJ,et al. Perioperative management of patients undergoing anal sphincter repair [abstract]. Br J Surg 1997;84:38–9.
Author information
Authors and Affiliations
Additional information
Supported in part by a generous educational grant from the Caporella family.
Read at the meeting of The American Society of Colon and Rectal Surgeons, Philadelphia, Pennsylvania, June 21 to 27, 1997.
About this article
Cite this article
Nessim, A., Wexner, S.D., Agachan, F. et al. Is bowel confinement necessary after anorectal reconstructive surgery?. Dis Colon Rectum 42, 16–23 (1999). https://doi.org/10.1007/BF02235177
Issue Date:
DOI: https://doi.org/10.1007/BF02235177