Abstract
Background
Intravenous cannulation is a very common procedure. Venous aneurysm secondary to peripheral intravenous cannulation is extremely rare. Moreover, venous aneurysm can mimic other conditions and may confuse the issue.
Case presentation
We describe a case of a 45-year-old woman who was referred with the diagnosis of varicose vein of right arm. A history of intravenous cannulation at the same site was noted that raised suspicion. The swelling was compressible and turned out to be a venous aneurysm. The lesion was completely excised. Postoperative recovery was uneventful. Histology findings were in conformity with the preoperative diagnosis.
Conclusion
Caution should be exercised in diagnosing varicose vein at a site that bears a history of intravenous cannulation. The case also raises an important issue regarding consent. Should patients undergoing peripheral intravenous cannulation be warned of this rare complication?
Similar content being viewed by others
Background
Venous aneurysm is an uncommon condition that can present in a myriad of fashions and cause diagnostic challenge. We describe a rare case of symptomatic venous aneurysm of the median antecubital vein secondary to intravenous cannulation, which was initially referred by the general practitioner as a varicose vein. The aneurysm was excised successfully without any complication. Clinical features, treatment and complications of venous aneurysms have been discussed. The case raises the issue of warning patients of a rare complication of a common procedure. A review of literature has also been performed. The optimum management of venous aneurysms remains unclear. There are three objectives of reporting this case- i) to make readers aware of this rare but potentially serious condition; ii) to highlight the need for optimising treatment of venous aneurysms, and iii) to raise a debate whether such a complication should be routinely mentioned while obtaining consent for establishing peripheral cannulation.
Case presentation
A 45-year-old woman presented with a swelling in her right antecubital fossa. The only relevant past medical history was an episode of gastroenteritis and dehydration, for which she required hospital admission eight years previously. During that admission she had received intravenous fluid therapy via a cannula in the right antecubital fossa approximating to the same area as the swelling. She recalled developing the swelling few months following the episode. The swelling had steadily grown over time and become painful. There was no history suggestive of deep venous thrombosis of the right arm. There was no other significant past medical history.
General examination was unremarkable. Local examination showed a soft, non-tender, compressible lesion, 2 × 3 cm2 in size, just distal to the right antecubital fossa [Figure 1]. There was no audible bruit. All the pulses in the arm were easily palpable. She was normotensive and there was no difference in blood pressure between the two arms. There was no neurological deficit.
Routine laboratory investigations, including coagulation profile, were within normal limits. She underwent a duplex scan that showed a venous aneurysm in relation to a large median cubital vein. The vein appeared competent. There was no evidence of ectasia, varicosity or thrombosis of any of the surrounding arm veins.
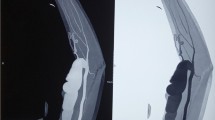
The aneurysm was explored under general anaesthetic and was completely excised. The key operative steps involved identification and ligation of tributaries feeding the aneurysm, prior to excision of the sac [Figure 2]. She made an uncomplicated recovery with complete resolution of her symptoms.
Histology of the aneurysmal sac showed periphery of the blood vessel with congested lumen and thickened media [Figure 3]. All three layers of the venous wall were preserved in the sac, which was suggestive of a true aneurysm. There was no element of endophlebosclerosis or endophlebohypertrophy.
Discussion
Venous aneurysms are relatively rare. An unrestricted electronic search of the Medline database till February 2007 showed that one case of pseudoaneurysm of the antecubital vein had been described in the literature [1].
A venous aneurysm is defined as a dilatation of a localised segment of vein. Unfortunately there are no universally agreed size criteria to define a venous dilatation as an aneurysm. Aneurysm can be congenital or acquired, though the exact aetiology remains unclear. It has been suggested that aneurysmal dilatation is a response to increased haemodynamic pressure at a site of mural weakness [2]. However, aneurysms in the neck, where the pressure is low, cannot be explained by such theory [3]. It is possible that both congenital and acquired factors are involved. Lev and Saphir noted certain changes in gross and microscopic structure of the popliteal vein with age [4]. They described these changes as endophlebohypertrophy (intimal hypertrophy) and endophlebosclerosis (loss of smooth muscle and elastic tissue with replacement by connective tissue). These changes were seen at points of stress adjacent to arteries and entry points of tributaries. Schatz and Fine noted similar findings in venous aneurysms [5]. They considered endophlebohypertrophy and endophlebosclerosis as important factors in the development of venous aneurysms in a way similar to that of arteriosclerosis in the formation of arterial aneurysms.
Sites of aneurysm can be grouped as (i) central thoracic (e.g., superior vena cava); (ii) visceral (e.g., portal, superior mesenteric, splenic, renal); and (iii) cervical (e.g., jugular, facial, subclavian) and (iv) peripheral (e.g., cephalic, iliac, femoral, saphenous, popliteal) [6].
A venous aneurysm can present as a soft, compressible, subcutaneous mass that decompresses with elevation and enlarges with dependency and the Valsalva manoeuvre [6]. It can be detected as an incidental finding on an imaging study or diagnosed during investigations of a venous thromboembolic event. In the upper limb it is most likely to present as a soft tissue swelling that may or may not result in compressive symptoms [7–9].
Reported histology has varied from the presence of an anomalous muscular layer to a diminution of muscle and elastin fibres [10, 11]. It is not always possible to be certain whether a venous aneurysm is truly a primary phenomenon or results from a previous but long-forgotten minor trauma. The variation in pathological diagnosis may be representative of a difference in aetiology.
The complications of venous aneurysms include embolism, thrombosis and rupture [12–14]. Venous aneurysms of the portal system can be associated with portal hypertension and gastrointestinal bleeding [6, 12].
Duplex scanning, Computed Tomography, Magnetic Resonance Imaging (MRI) and venography are important diagnostic modalities [15]. Isotopic 99mTc human serum albumin angiography has also been used in certain circumstances [6]. Krinsky et al. describe the 'layered gadolinium sign' on MRI scanning [16]. Duplex scanning remains the first investigation of choice for most of the upper limb venous aneurysms.
The treatment of venous aneurysms depends on the site and associated symptomatology. Many symptom-free, superficial, small fusiform aneurysms without thrombus are deemed to carry a low risk of complications and therefore may remain under close surveillance with duplex scanning. Symptomatic, enlarging, popliteal and saccular aneurysms of any size or those with large fusiform aneurysms should undergo surgery [17, 18]. There is no agreed size criterion that defines an aneurysm 'small' or 'large'. However, Sessa et al. had stated 20 mm as a cut-off limit for repair of popliteal venous aneurysms [15].
Surgical options for repairing venous aneurysms include: (i) excision; (ii) aneurysmorrhaphy; (iii) resection with end-to-end anastomosis and (iv) resection with interposition graft [2]. In the absence of a randomised control trial it is difficult to assess efficacy of one procedure over another. The rarity of the condition would almost preclude such a trial. There is a high incidence of postoperative venous thrombosis, particularly in popliteal venous aneurysm resection [19]. Anticoagulation should be considered to prevent post-operative venous thrombosis in selected cases. In the case described, the patient had undergone excision of the aneurysm and therefore did not merit any anticoagulation. Venous pseudoaneurysm had been successfully treated by radiological intervention (e.g., coil embolisation) [1]. Surgical excision was performed in our case because she experienced pain in the arm. The pain resolved completely after surgery.
An unrestricted search of the Medline database (from 1950 to February 2007) was performed by using the keywords 'peripheral', 'venous' and 'aneurysm'. A total of 172 articles were cited. However, only one article reported a case of venous pseudoaneurysm following venupuncture, where the patient was on long term anticoagulation [1]. While arterial pseudoaneurysms are encountered more commonly in anticoagulated patients, there is no documented relationship between venous aneurysm formation and state of coagulation profile [20]. Given this background, the present case, to our knowledge, is the first report of a true venous aneurysm formation following intravenous cannulation. This makes our case report unique.
Usually, verbal consent is obtained while establishing a peripheral cannula. According to General Medical Council, patients must be given sufficient information...to enable them to exercise their right to make informed decisions about their care [21]. This raises the question whether venous aneurysm, a rare but potentially serious complication, should be mentioned while obtaining consent for intravenous cannulation. Herein lays the importance of publishing such rare complications, as more reporting of similar cases may help provide an answer.
Conclusion
Aneurysms of the venous system can be potentially dangerous in view of possible complications. A symptomatic acquired aneurysm of the antecubital vein secondary to intravenous cannulation has been described that was excised without any complications. Further considerations are warranted to clarify the optimum management of this rare condition and address the issue of consent.
Abbreviations
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- GMC:
-
General Medical Council
References
Chakraborty S, McGann G, Coen LD: Embolization of iatrogenic venous pseudoaneurysm. Br J Radiol. 1999, 72: 311-312.
Dahl JR, Freed TA, Burke MF: Popliteal vein aneurysm with recurrent pulmonary thromboemboli. JAMA. 1976, 236: 2531-2532. 10.1001/jama.236.22.2531.
Cheatle TR, Perrin M: Primary venous aneurysms of the popliteal fossa. Phlebology. 1993, 8: 82-85.
Lev M, Saphir O: Endophlebohypertrophy and phlebosclerosis. I. The popliteal vein. AMA Arch Pathol . 1951, 51 (2): 154-178.
Schatz IJ, Fine G: Venous aneurysms. N Engl J Med. 1962, 266: 1310-1312.
Castle JM, Arous EJ: Femoral vein aneurysm: a case report and review of the literature. Cardiovasc Surg. 1995, 3: 317-319. 10.1016/0967-2109(95)93883-Q.
Kassabian E, Coppin T, Combes M, Julia P, Fabiani JN: Radial nerve compression by a large cephalic vein aneurysm: case report. J Vasc Surg. 2003, 38: 617-619. 10.1016/S0741-5214(03)00290-8.
Marquardt G, Angles SM, Leheta FD, Seifert V: Median nerve compression caused by a venous aneurysm. Case report. J Neurosurg. 2001, 94 (4): 624-626.
Wang ED, Li Z, Goldstein RY, Hurst LC: Venous aneurysms of the wrist. J Hand Surg. 2001, 26 (5): 951-955. 10.1053/jhsu.2001.26326.
Acin F, De Benito L, Guilleuma J, Alvarez R: Primary axillary venous aneurysm. Ann Vasc Surg. 1999, 13 (5): 539-540. 10.1007/s100169900294.
Goto Y, Sakurada T, Nanjo H, Masuda H: Venous aneurysm of the cephalic vein: report of a case. Surg Today. 1998, 28 (9): 964-966. 10.1007/s005950050263.
Calligaro KD, Ahmad S, Dandora R, Dougherty MJ, Savarese RP, Doerr KJ, McAffee S, Delaurentis DA: Venous aneurysms: surgical indications and review of the literature. Surgery. 1995, 117: 1-6. 10.1016/S0039-6060(05)80222-3.
De Waele JJ, Calle PA, Vermassen FE: Thrombosis of an aneurysm of the basilic vein upper extremity venous aneurysm. Acta Chirurgica Belgica. 2001, 101 (6): 308-309.
Taira A, Akita H: Ruptured venous aneurysm of the persistent left superior vena cava. Angiology. 1981, 32 (9): 656-659.
Sessa C, Nicolini P, Perrin M, Farah I, Magne J, Guidicelli H: Management of symptomatic and asymptomatic popliteal venous aneurysms: A retrospective analysis of 25 patients and review of the literature. J Vasc Surg. 2000, 32: 902-911. 10.1067/mva.2000.110353.
Krinsky G, Johnson G, Rofsky N, Shapiro R, Yang B, Weinreb J: Venous aneurysms: MR diagnosis with the 'layered gadolinium' sign. J Comput Assist Tomogr. 1997, 21 (4): 623-627. 10.1097/00004728-199707000-00019.
Helsted M, Vilmann P, Jacobsen B, Christoffersen JK: Popliteal venous aneurysms with or without pulmonary embolism. Eur J Vasc Surg. 1991, 5: 333-342. 10.1016/S0950-821X(05)80518-3.
Aldridge SC, Comerota AJ, Katz ML, Wolk JH, Goldman BI, White JV: Popliteal venous aneurysm: report of two cases and review of the world literature. J Vasc Surg. 1993, 18: 708-715. 10.1067/mva.1993.45736.
Ross GJ, Violi L, Barber LW, Vujic I: Popliteal venous aneurysm. Radiology. 1988, 168: 721-722.
Lenartova M, Tak T: Iatrogenic Pseudoaneurysm of Femoral Artery: Case Report and Literature Review. Clin Med Res. 2003, 1: 243-247.
General Medical Council: Seeking patients' consent: the ethical considerations. [http://www.gmc-uk.org/guidance/current/library/consent.asp]
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2482/7/9/prepub
Acknowledgements
Written consent was obtained from the patient for publication.
We would like to thank the vascular studies unit at The Royal Free Hospital, London, UK, for performing the duplex scan.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
DD: Performed the surgery, designed the case report, collated the information, searched literature and drafted the manuscript.
SW: Assisted with the surgery, involved in all investigations, assisted in providing a critical appraisal and review of the manuscript.
EM: Made the histological diagnoses and prepared the pathology images, advised on the format and design and assisted in providing a critical appraisal of the manuscript.
FM: Supervised and assisted with the surgery, involved in all investigations, assisted in literature search, writing and editing of the manuscript.
All authors have reviewed and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Debnath, D., Wallace, S., Mylona, E. et al. Aneurysm of antecubital vein: an unusual complication of peripheral intravenous cannulation. BMC Surg 7, 9 (2007). https://doi.org/10.1186/1471-2482-7-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2482-7-9