Abstract
Background
The significance of nodal metastases, very common in papillary thyroid cancer, and the role of lymph node dissection in the neoplasm management, are still controversial. The impact of lymph node involvement on local recurrence and long-term survival remains subject of active research. With the aim to better analyze the predictive value of lymph node involvement on recurrence and survival, we investigated the clinico-pathological patterns of local relapse following total thyroidectomy associated with lymph node dissection, for clinical nodal metastases papillary thyroid cancer, in order to identify the preferred surgical treatment.
Methods
Clinical records, between January 2000 and December 2006, of 69 patients undergoing total thyroidectomy associated with selective lymph node dissection for clinical nodal metastases papillary thyroid cancer, were retrospectively evaluated. Radioiodine ablation, followed by Thyroid Stimulating Hormone suppression therapy was recommended in every case. In patients with loco regional lymph nodal recurrence, a repeated lymph node dissection was carried out. The data were compared with those following total thyroidectomy not associated with lymph node dissection in 210 papillary thyroid cancer patients without lymph node involvement, at preoperative ultrasonography and intra operative inspection.
Results
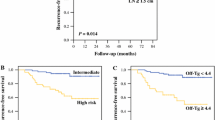
Incidence of permanent hypoparathyroidism (iPTH < 10 pg/ml) and permanent monolateral vocal fold paralysis were respectively 1.4 % (1/69) and 1.4% (1/69), similar to those reported after total thyroidectomy "alone". The rate of loco regional recurrence, with positive cervical lymph nodes, following 8 year follow-up, was 34.7% (24/69), higher than that reported in patients without nodal metastases (4.2%). A repeated lymph node dissection was carried out without significant complications.
Conclusions
Nodal metastases are a predictor of local recurrence, and a higher rate of lymph node involvement is expected after therapeutic lymph node dissection associated with total thyroidectomy. The prognostic significance of nodal metastases on long-term survival remains unclear, and more prospective randomized trials are requested to better evaluate the benefits of different therapeutic approaches.
Similar content being viewed by others
Introduction
Papillary and follicular variants are the most frequent differentiated thyroid neoplasms [1, 2], followed by medullary cancer, often part of the MEN-2 syndrome [3–5], and anaplastic carcinoma, associated with a prognosis similar to that reported in sarcomatoid carcinoma of other districts [6]. In the last ten years, ultrasound (US) guided fine-needle cytology (FNC) has allowed a more precocious diagnosis, identifying a higher number of small papillary cancer (SPC) [7–11]. Papillary thyroid cancer (PTC) prognosis is excellent, reflecting, with a 5- and 10-year survival of 90 and 95% [12], the favorable nature of the neoplasm. Recurrence develops in about 20% of patients, requiring additional treatment, responsible of significant morbidity, and PTC-related deaths are still reported [13, 14]. The risk of relapse, in negative nodes patients, ranges between 0 and 9%, while clinically and US positive node cases are associated with higher recurrence rates, 10-42%, and also "high volume" disease is another unfavorable factor [15]. Differently from data reported in the management of breast, colorectal, gastro-esophageal, pancreatic, genitourinary or pulmonary cancers, thyroid metastatic nodes are associated with a higher mortality risk only in selected cases [16]. Despite the notable progresses in oncology, the true significance of the lymph node involvement, so frequent in pediatric and geriatric patients, is unclear and object of active research. There is agreement about its impact on local recurrence [16] but, according to more recent data, nodal metastases may affect long-term survival only in high risk patients [17]. Also metastatic lymph node number and size may be of prognostic value [16], but unfortunately the extent of LD and its indications - routine vs therapeutic- are still matter of intensive research [15]. The analysis of the clinico- pathological patterns of local recurrence in patients undergone LD, associated with TT for N+ PTCs, and the predictive value of nodal metastasis on management outcomes were the main objectives of our retrospective study.
Study design
Clinical records of PTC patients, undergoing TT associated with LD, between January 2000 and December 2006, for clinical metastatic nodes, identified at preoperative ultrasonography or intraoperative inspection, were analyzed. They were compared with those observed in a clinical series of 210 patients undergone TT without LD for N0 PTC. In every case, a preoperative diagnosis of PTC was obtained by US guided FNC. The preoperative work-up consisted of thyroid hormones, TSH, Tg and anti-Tg antibodies levels evaluation, and a high resolution ultrasonography of the neck. A pre- and postoperative fibrolaryngoscopy was performed in all patients. In 8 patients (11.5%) BRAF mutations were searched on tumor specimens. Tumor extent was evaluated according to the American Joint Committee on Cancer (AJCC) TNM Classification of Thyroid Cancer (7th edition, 2010). Postoperative diagnosis of lymph node recurrence was detected by US guided FNC, and Tg washing of FNC aspirates, performed in cases of enlarged lymph node ≥ 1 cm. Patient demographics, postoperative complications, including neck hematoma requiring reoperation, transient or permanent hypoparathyroidism, transient or permanent vocal cord palsy, distant and loco regional recurrence, detected by postoperative surveillance, were recorded. In case of a iPTH level < 10 pg/ml (normal value = 10-65), hypoparathyroidism was determined, and it was considered permanent if persisting for more than 6 months and requiring medical therapy. Vocal fold palsy, confirmed by fibrolaryngoscopy, was considered permanent when lasting for more than 6 months. Qualitative data were expressed in percent, while quantitative data as means.
Materials and methods
Tg and TSH was determined by Immunite immunoassay (Siemens Healthcare Diagnostics) with sensitivities of 0.2 ng/mL and 0.03 mIU/L, respectively. Anti-Tg antibodies were detected by Quanta Lite enzyme-linked immunosorbent assay (Inova Diagnostics), and we considered 40 UI/ml as cut-off value of Anti-Tg Abs (normal value = 0-60 UI/ml). Each surgeon participating to the study used a similar technique in performing TT, as well as central and lateral lymph node dissection. An ultrasonic scalpel, Harmonic Ace ® ( Ethicon Endosurgery) was utilized in 9 cases (13%), and in selected cases hemostasis was optimized by means of Floseal ® Hemostatic Matrix (Baxter Zurich- Switzerland). Routinely, recurrent laryngeal nerves were identified and exposed, as well as parathyroid glands were identified and preserved. In case of suspected devascularized or incidentally removed parathyroid glands, a muscular autoimplantation followed. Serum calcium and intact parathormone levels were assayed on the first postoperative day, and subsequently on a clinical basis evaluation. In case of loco regional recurrence, a selective central or ipsilateral (VI, III, IV,V) LD was performed according to the American Academy of Otolaryngology - Head and Neck Surgery [17]. After surgery, all patients underwent adjuvant RAI ablation (1850-3700 MBq-131I ). Apart from lymph node involvement, indications for postoperative 131I treatment are a tumor > 1.0 cm, extra-capsular thyroid invasion or loco regional extension, an unfavorable histological subtype (follicular, diffuse sclerosing or tall cells papillary cancer), multifocal disease, BRAF positive tumor specimens. To obtain adequate levels of endogenous TSH (>30 mU/ml), that are associated with an increased radioiodine uptake, patients stopped L-T4 replacement 3-4 weeks before radioiodine treatment; when L-T4 withdrawal was not indicated, TSH stimulation was achieved with Recombinant Human Thyrotropin (rhTSH) (Thyrogen ® - Genzyme corporation). Post-therapy whole-body scan was performed 4-7 days after RAI treatment. Neck ultrasonography and monitoring of serum Tg and Tg-antibodies levels, during suppressive l-tiroxine treatment, were carried out every 6 months. A serum Tg level ≤1 ng/ml was considered as undetectable. Surveillance for possible recurrence in patients considered disease-free was achieved by Tg detection after rhTSH stimulation (American Thyroid Association Guidelines 2009) and neck ultrasound. Diagnosis of disease recurrence in the cervical lymph nodes was based on US-guided FNC, Tg washing of FNC aspirates and serum Tg levels monitoring.
Results
Sixty-nine PTC patients, 45 women and 24 men (F/M ratio = 1.8/1), with a 34-year mean age (19-70) were submitted to TT associated to selective LD (Table 1). In 5/69 patients (7.24%), parathyroid tissue was implanted in the strap muscles, and in 9/69 cases (13%) parathyroid tissue was identified in the final pathology analysis. Incidence of surgical complications is reported in Table 2. The mean primary tumor size was respectively 1.36 cm (0.2-5) in TT and LD group and 1.4 cm (0.7-2.4) in TT patients, and a microcarcinoma (≤1 cm) was diagnosed in 6 patients (8.69 %) irrespective to 29% of TT group. Histotype was classic in 60 patients (86.9%), follicular variant in 9 (13%); 12 patients (17.39%) had multifocal tumors - 9/12 classic variant, 3/12 follicular variant vs 15.2% of TT group. Nine out of 69 patients (13%) had a loco regional infiltration (T3), vs 11.4% of TT patients, by classic variant tumor in 7 cases and by follicular variant tumor in 2 cases. A BRAF mutation was discovered in 1 out of 10 tested patients (10%). Patients pTNM Stage and pathological data are shown in Table 1. No patient developed distant recurrence during a 8-year mean follow-up (6-13).
Lymph nodal recurrence
Following TT associated with LD and RAI ablation, 24/69 cases (34.7%) of nodal recurrence - 6 central recurrence (VI) and 18 ipsilateral recurrence (III-IV) - were observed, representing a rate higher than reported in patients without preoperative clinical nodal metastases (4.2%). Demographic characteristics were the following: 14 males - median age 33.25 years (27-38) - and 10 females - median age 27.25 years (19-30) with a M/F ratio = 1.4/1. The median elapsed time between TT and lymph node recurrence was 44 months (4-85). Twenty-one patients had classic variant, 3 had follicular variant PTC; median Tg value was 2.74 ng/ml (0.1-13.1 ng/ml) ( Tg>2 ng/ml in 5 patients and <2 ng/ml in 19 patients) and Tg-antibodies value was > 40 UI/ml in 10 patients and <40 UI/ml in 14 (33.5-722 UI/ml). In every case, a repeated central and ipsilateral lymph node dissection (VI,III,IV,V) was performed, followed by another session of metabolic radiotherapy. Significant perioperative complications were not observed, and the mean number of removed lymph nodes, as documented by pathologists, was 16.5 (2-32). Metastases were reported in up to 2.8 (1-5) collected lymph nodes.
Discussion
According to our data, a higher loco regional recurrence rate with a statistically significant difference, 34.7 vs 4.2%, following TT associated with therapeutic selective LD, was observed irrespective to nodal relapse rate reported after TT, in absence of lymphatic involvement. Metastatic lymph node was a predictive factor, favoring recurrent disease after 8-year mean follow-up. In absence of suspected enlarged lymph node, identified by preoperative ultrasonography and intraoperative inspection, patients undergoing TT without routine central lymph node dissection (RCLD) have a low risk of lymph nodal recurrence. In the treatment of low-risk PTC patients, TT and RAI ablation allow favorable long-term results; regarding recurrence and survival, routine LD is not indicated and needs to be more intensively investigated. About recurrence, male gender (a male/female ratio of 1.4/1) and age <50 years were the main clinical features, while the follicular variant was frequently associated with lymph node relapse. Primary tumor mean size was <2 cm, with the lateral compartment mostly affected, and a median elapsed time between TT, associated with LD, and lymph node recurrence of 44 months (4-85). The prognostic impact of the postoperative RAI treatment, administered in all of the LD patients, as well as in most TT "alone" cases, must be considered similar in the two groups. The small number of examined N+ PTC cases, the absence of a control group of patients undergoing RCLD, and the inability to exactly distinguish between recurrent and persistent disease, were the main limitations of this retrospective analysis. PTC multifocal nature, the effectiveness of RAI treatment and the monitoring of serum thyroglobulin (Tg) levels during follow-up are evocated in favor of TT and of the TSH suppressive therapy. On the contrary, the role of the LD, regarding its indication- routine or therapeutic-, extension - ipsi or contralateral- and outcomes, in terms of recurrence and survival, and postoperative RAI ablation are subject of active research. According to the recent American Thyroid Association (ATA) guide lines, RCLD is indicated in high risk patients with advanced primary tumors [17], but prospective randomized trials are needed to evaluate its benefits [19]. Relapse prevention, the high risk of positive lymph nodes and the lower morbidity rate of the first operation are evocated in favor of RCLD [20], often associated with an higher rate of complications, without demonstrable benefits in terms of long-term survival [21, 22]. The high rate of micro and clinical nodal metastases is in contrast with the low incidence of clinical recurrence following TT without LD, and remains an "obscure" issue in oncology. According to recent studies, nodal metastases may affect recurrence and survival rates especially in older patients [13]. Multifocal primary tumor, infiltration of thyroid capsule, patient age (pediatric or geriatric population), tumor size greater than 3 cm, several oncogenes (p53, BRAF), nodal metastases (number and size), as demonstrated in our series, are considered the main risk factors for local recurrence [16, 23]. Especially in male patients > 45 years, with aggressive histotypes, capsular or locoregional infiltration, incomplete tumor resection, BRAF positivity, a higher risk of loco regional and distant recurrence is reported, while in the management of low-risk patients, without suspected lymph node, TT, associated with a low morbidity, similar to that reported in parathyroid surgery [24–29], remains the operation of choice, as in most thyroid diseases [30–35]. RCLD, failed to demonstrate beneficial effects on recurrence and long-term survival, increasing the rates of permanent hypoparathyroidism and of unintentional permanent recurrent laryngeal nerve injury [15, 20, 36–38]. At the same time literature data demonstrated that reoperation (lymph node dissection) is not associated with a higher morbidity [39, 40], and we believe that, in absence of suspicious enlarged lymph node, routine central or lateral LD is not routinely indicated.
Conclusions
Our study supports the following data. Locoregional recurrence rate, mostly of the lateral compartment, frequently observed 2 years after surgery in young male patients, was higher in N+ patients undergone therapeutic selective LD. A lower relapse rate was observed in N0 PTC following TT alone, confirming the predictive value of risk of lymph node involvement. PTC classic variant, in every case less than 2 cm was the most frequent observed hystotype. In the treatment of low-risk PTC patients, routine LD is not indicated. Considering the controversial literature data, further prospective randomized studies are needed in the attempt to clarify the predictive value of lymph node involvement on long-term survival.
Authors' information
GC: Assistant Professor of Surgery at Second University of Naples
GD: Associate Professor of Surgery at Second University of Naples
DP: Assistant Professor of Endocrinology at Second University of Naples
CM: Surgical fellow at Second University of Naples
CG: Surgical fellow at Second University of Naples
DE: Surgical fellow at Second University of Naples
ET: Surgical fellow at Second University of Naples
CDP: Surgical fellow at Second University of Naples
SN: Surgical fellow at Second University of Naples
AR: Surgical fellow at University of Catanzaro
LS: Full Professor of Surgery at Second University of Naples
Abbreviations
- PTC:
-
papillary thyroid cancer
- LD:
-
lymph node dissection
- TT:
-
total thyroidectomy
- N+:
-
clinical nodal metastases
- RAI:
-
Radioiodine
- TSH:
-
Thyroid Stimulating Hormone
- US:
-
ultrasound
- FNC:
-
guided fine-needle cytology
- SPC:
-
small papillary cancer
- PTC:
-
Papillary thyroid cancer
- rhTSH:
-
Recombinant Human Thyrotropin
- RCLD:
-
routine central lymph node dissection
- Tg:
-
serum thyroglobulin
- ATA:
-
American Thyroid Association
References
Trimboli P, Ulisse S, Graziano FM, Marzullo A, Ruggieri M, Calvanese A, Piccirilli F, Cavaliere R, Fumarola A, D'Armiento M: Trend in thyroid carcinoma size, age at diagnosis and histology in a retrospective study of 500 cases diagnosed over 20 years. Thyroid. 2006, 16: 1151-1155. 10.1089/thy.2006.16.1151.
Pezzolla A, Docimo G, Ruggiero R, Monacelli M, Cirocchi R, Parmeggiani D, Conzo G, Gubitosi A, Lattarulo S, Ciampolillo A, Avenia N, Docimo L, Palasciano N: Incidental thyroid carcinoma: a multicentric experience. Recenti Prog.Med. 2010, 101 (5): 194-8.
Pasquali D, Di Matteo FM, Renzullo A, Accardo G, Esposito D, Barbato F, Colantuoni V, Circelli L, Conzo G: Multiple endocrine neoplasia, the old and the new: a mini review. G.Chir. 2012, 33 (11-12): 370-373. Nov.-Dec.
Conzo G, Circelli L, Pasquali D, Sinisi A, Sabatino L, Accardo G, Renzullo A, Santini L, Salvatore F, Colantuoni V: Lessons to be learned from the clinical management of a MEN 2A patient bearing a novel 634/640/700 triple mutation of the RET proto-oncogene. Clin Endocrinol (Oxf). 2012, 77 (6): 934-6. 10.1111/j.1365-2265.2012.04412.x. Dec doi: 10.1111/j.1365-2265.2012.04412.x
Conzo G, Musella M, Corcione F, De Palma M, Ferraro F, Palazzo A, Napolitano S, Milone M, Pasquali D, Sinisi AA, Colantuoni V, Santini L: Laparoscopic adrenalectomy, a safe procedure for pheochromocytoma. A retrospective review of clinical series. Int J Surg. 2013, 11 (2): 152-6. 10.1016/j.ijsu.2012.12.007.
Di Vizio D, Insabato L, Conzo Zafonte BT, Ferrara G, Pettinato G: Sarcomatoid carcinoma of the colon: a case report with literature review. Tumori. 2001, 87 (6): 431-435.
Conzo G, Troncone G, Docimo G, Pizza A, Sciascia V, Bellevicine C, Napolitano S, Della Pietra C, Palazzo A, Signoriello G, Santini L: Cytologically undetermined follicular lesions: surgical procedures and histological outcome in 472 cases. Ann Ital Chir. 2013, 84: 251-256. Sep 18, 83. doi:pii: S0003469X12020350
Troncone G, Volante M, Iaccarino A, Volante M, Iaccarino A, Zeppa P, Cozzolino I, Malapelle U, Palmieri EA, Conzo G, Papotti M, Palombini L: Cyclin D1 and D3 overexpression predicts malignant behavior in thyroid fine-needle aspirates suspicious for Hurtle cell neoplasms. Cancer Cytopathol. 2009, 117: 522-529.
Cantisani V, Ulisse S, Guaitoli E, De Vito C, Caruso R, Mocini R, D'Andrea V, Ascoli V, Antonaci A, Catalano C, Nardi F, Redler A, Ricci P, De Antoni E, Sorrenti S: Q-elastography in the presurgical diagnosis of thyroid nodules with indeterminate cytology. PLoS One. 2012, 7 (11): e50725-10.1371/journal.pone.0050725. doi: 10.1371/journal.pone.0050725. Epub 2012 Nov 29. PubMed PMID: 23209819; PubMed Central PMCID: PMC3510167
Baldini E, Sorrenti S, Di Gioia C, De Vito C, Antonelli A, Gnessi L, Carbotta G, D'Armiento E, Miccoli P, De Antoni E, Ulisse S: Cervical lymph node metastases from thyroid cancer: does thyroglobulin and calcitonin measurement in fine needle aspirates improve the diagnostic value of cytology?. BMC Clin Pathol. 2013, 13: 7-10.1186/1472-6890-13-7. Feb 19, doi: 10.1186/1472-6890-13-7. PubMed PMID: 23421519; PubMed Central PMCID: PMC3583740
Bellevicine C, Malapelle U, Docimo G, Ciancia G, Mossetti G, Pettinato G, Troncone G: Multicentric encapsulated papillary oncocytic neoplasm of the thyroid: A case diagnosed by a combined cytological, histological, immunohistochemical, and molecular approach. Diagn Cytopathol. 2012, 40 (5): 450-454. 10.1002/dc.21828. May, doi: 10.1002/dc.21828. Epub 2011 Sep 30. PMID: 21965084
Falvo L, Catania A, D'Andrea V, Marzullo A, Giustiniani MC, De Antoni E: Prognostic importance of histologic vascular invasion in papillary thyroid carcinoma. Ann Surg. 2005, 241: 640-646. 10.1097/01.sla.0000157317.60536.08.
Hay ID, Hutchinson ME, Gonzalez-Losada T, McIver B, Reinalda ME, Grant CS, Thompson GB, Sebo TJ, Goellner JR: Papillary thyroid microcarcinoma: a study of 900 cases observed in a 60-year period. Surgery. 2008, 144: 980-987. 10.1016/j.surg.2008.08.035.
Pasquali D, Santoro A, Bufo P, Conzo G, Deery WJ, Renzullo A, Accardo G, Sacco V, Bellastella A, Pannone G: Upregulation of Endocrine Gland-Derived Vascular Endothelial Growth factor in Papillary thyroid Cancers Displaying Infiltrative Patterns, Lymph Node Metastases, and Braf mutation. Thyroid. 2011, 21 (4): 391-399. 10.1089/thy.2010.0168.
Conzo G, Pasquali D, Bellastella G, Esposito K, Carella C, De Bellis A, Docimo G, Klain M, Iorio S, Napolitano S, Palazzo A, Pizza A, Sinisi AA, Zampella E, Bellastella A, Santini L: Total thyroidectomy, without prophylactic central lymph node dissection, in the treatment of differentiated thyroid cancer. Clinical retrospective study on 221 cases. Endocrine. 2013,
Yip J, Orlov S, Orlov D, Vaisman A, Hernández KG, Etarsky D, Kak I, Parvinnejad N, Freeman JL, Walfish PG: Predictive value of metastatic cervical lymph node ratio in papillary thyroid carcinoma recurrence. Head Neck. 2013, 35 (4): 592-598. 10.1002/hed.23047. Apr, doi: 10.1002/hed.23047. Epub 2012 Jun 23
Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, Mazzaferri EL, McIver B, Pacini F, Schlumberger M, Sherman SI, Steward DL, Tuttle RM: Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2009, 19: 1167-1214. 10.1089/thy.2009.0110.
Robbins KT, Clayman G, Levine PA, Medina J, Sessions R, Shaha A, Som P, Wolf GT: Neck dissection classification update, revisions proposed by the American Head and Neck Society and the American Academy of Otolaryngology-Head and Neck Surgery. Arch Otolaryngol Head Neck Surg. 2002, 128: 751-758. 10.1001/archotol.128.7.751. American Head and Neck Society; American Academy of Otolaryngology--Head and Neck Surgery.
Carling T, Long WD, Udelsman R: Controversy surrounding the role for routine central lymph node dissection for differentiated thyroid cancer. Curr Opin Oncol. 2010, 22: 30-34. 10.1097/CCO.0b013e328333ac97.
White ML, Gauger PG, Doherty GM: Central lymph node dissection in differentiated thyroid cancer. World J Surg. 2007, 31: 895-904. 10.1007/s00268-006-0907-6.
Henry JF, Gramatica L, Denizot A, Kvachenyuk A, Puccini M, Defechereux T: Morbidity of prophylactic lymph node dissection in the central neck area in patients with papillary thyroid carcinoma. Langenbecks Arch Surg. 1998, 383: 167-169. 10.1007/s004230050111.
Mazzaferri EL, Doherty GM, Steward DL: The pros and cons of prophylactic central compartment lymph node dissection for papillary thyroid carcinoma. Thyroid. 2009, 19: 683-689. 10.1089/thy.2009.1578.
Bonnet S, Hartl D, Leboulleux S, Baudin E, Lumbroso JD, Al Ghuzlan A, Chami L, Schlumberger M, Travagli JP: Prophylactic lymph node dissection for papillary thyroid cancer less than 2 cm: implications for radioiodine treatment. J Clin Endrocrinol and Metab. 2009, 94: 1162-1167. 10.1210/jc.2008-1931.
Esposito MG, Cesare CM, De Santo RM, Cice G, Perna AF, Violetti E, Conzo G, Bilancio G, Celsi S, Annunziata F, Iannelli S, De Santo NG, Cirillo M, Livrea A: Parathyroidectomy improves the quality of sleep in maintenance hemodialysis patients with severe hyperparathyroidism. J Nephrol. 2008, 21 (Suppl 13): S92-S96.
Conzo G, Perna AF, Sinisi AA, Palazzo A, Stanzione F, Della Pietra C, Livrea A: Total parathyroidectomy without autotransplantation in the surgical treatment of secondary hyperparathyroidism of chronic kidney disease. J Endocrinol Invest. 2012, 35: 8-13.
Conzo G, Perna A, Avenia N, De Santo RM, Della Pietra C, Palazzo A, Sinisi AA, Stanzione F, Santini L: Evaluation of "putative" role of intraoperative intact parathyroid hormone assay during parathyroidectomy for secondary hyperparathyroidism. A retrospective study on 35 consecutive patients. Endocrine. 2012, 42 (3): 606-611. 10.1007/s12020-012-9648-5. Dec
Docimo G, Tolone S, Pasquali D, Conzo G, D'Alessandro A, Casalino G, Gili S, Brusciano L, Gubitosi A, del Genio G, Ruggiero R, Docimo L: Role of pre and post-operative oral calcium and vitamin D supplements in prevention of hypocalcemia after total thyroidectomy. G Chir. 2012, 33: 11-12. 1-5
Parmeggiani D, De Falco M, Avenia N, Sanguinetti A, Fiore A, Docimo G, Ambrosino P, Madonna I, Peltrini R, Parmeggiani U: Nerve sparing sutureless total thyroidectomy. Preliminary study. Ann Ital Chir. 2012, 83 (2): 91-96. Mar-Apr, PMID: 22462326
Avenia N, Sanguinetti A, Cirocchi R, Docimo G, Ragusa M, Ruggiero R, Procaccini E, Boselli C, D'Ajello F, Parmeggiani D, Rosato L, Sciannameo F, De Toma G, Noya G: Antibiotic prophylaxis in thyroid surgery: A preliminary multicentric italian experience. 2009 Ann Surg Innov Res. Aug 5, 3: 10-
Cirocchi R, Boselli C, Guarino S, et al: Total thyroidectomy with ultrasonic dissector for cancer: multicentric experience. World J Surg Oncol. 2012, 10: 70-10.1186/1477-7819-10-70.
Calò PG, Pisano G, Medas F, Tatti A, Tuberi M, Nicolosi A: The use of the harmonic scalpel in thyroid surgery. Our experience. Ann Ital Chir. 2012, 3: 7-12.
Docimo G, Ruggiero R, Gubitosi A, Docimo G, Ruggiero R, Gubitosi A, Casalino G, Bosco A, Gili S, Conzo G, Docimo L: Ultrasound scalpel thyroidectomy: prospective randomized study. Ann Ital Chir. 2012, 83 (6): 491-496. Nov-Dec
De Bellis A, Conzo G, Cennamo G, Pane E, Bellastella G, Colella C, Iacovo AD, Paglionico VA, Sinisi AA, Wall JR, Bizzarro A, Bellastella A: Time course of Graves' ophthalmopathy after total thyroidectomy alone or followed by radioiodine therapy: a 2-year longitudinal study. Endocrine. 2012, 41: 320-326. 10.1007/s12020-011-9559-x.
D'Ajello F, Cirocchi R, Docimo G, Catania A, Ardito G, Rosato L, Avenia N: Thyroidectomy with ultrasonic dissector: a multicentric experience. 2010 Il Giornale di chirurgia. 31 (6-7): 289-292.
Docimo G, Tolone S, Gili S, d'Alessandro A, Casalino G, Brusciano L, Ruggiero R, Decimo L: Minimally Invasive Thyroidectomy (MIT): indications and results. Ann Ital Chir.
Pacini F, Schlumberger M, Dralle H, Ilisea R, Smith Y, Viersinga V: European consensus for the management of patients with differentiated thyroid carcinoma of the follicular epithelium. Eur J Endocrinol. 2006, 154: 787-803. 10.1530/eje.1.02158.
Carling T, Carty SE, Ciarleglio MM, Cooper DS, Doherty GM, Kim LT, Kloos RT, Mazzaferri EL, Peduzzi PN, Roman SA, Sippel RS, Sosa JA, Stack BC, Steward DL, Tufano RP, Tuttle RM, Udelsman R: American Thyroid Association design and feasibility of a prospective randomized controlled trial of prophylactic central lymph node dissection for papillary thyroid carcinoma. Thyroid. 2012, 22 (3): 237-244. 10.1089/thy.2011.0317. American Thyroid Association Surgical Affairs Committee
Conzo G, Stanzione F, Palazzo A, Brancaccio U, Della Pietra C, Esposito MG, Celsi S, Livrea A: La linfectomia nel cancro differenziato della tiroide. Chirurgia Italiana. 2009, 16: 539-544.
Conzo G, Docimo G, Ruggiero R, Napolitano S, Palazzo A, Gambardella C, Mauriello C, Tartaglia E, Cavallo F, Santini L: Surgical treatment of papillary thyroid carcinoma without lymph nodal involvement. Giornale di chirurgia. 2012, 33 (10): 339-342.
Shen WT, Ogawa L, Ruan D, Suh I, Duh QY, Clark OH: Central neck lymph node dissection for papillary thyroid cancer: the reliability of surgeon judgment in predicting which patients will benefit. Surgery. 2010, 148: 398-403. 10.1016/j.surg.2010.03.021.
Declaration statement
Publication of this article was funded by personal funds.
This article has been published as part of BMC Surgery Volume 13 Supplement 2, 2013: Proceedings from the 26th National Congress of the Italian Society of Geriatric Surgery. The full contents of the supplement are available online at http://www.biomedcentral.com/bmcsurg/supplements/13/S2
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
GC: conception, design, and execution of the study; critical revision; analysis and interpretation of data; drafting and editing of the manuscript; given final approval of the version to be published.
GD: conception, design, and execution of the study; analysis and interpretation of data; drafting and editing of the manuscript.
DP: conception, design, and execution of the study; analysis and interpretation of data; drafting and editing of the manuscript.
DE: conception, design, and execution of the study
ET: conception, design, and execution of the study
CDP: conception, design, and execution of the study; analysis and interpretation of data.
SN: conception, design, and execution of the study
AR: conception, design, and execution of the study
LS: conception and design of the study, given final approval of the version to be published.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an open access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Conzo, G., Docimo, G., Pasquali, D. et al. Predictive value of nodal metastases on local recurrence in the management of differentiated thyroid cancer. Retrospective clinical study. BMC Surg 13 (Suppl 2), S3 (2013). https://doi.org/10.1186/1471-2482-13-S2-S3
Published:
DOI: https://doi.org/10.1186/1471-2482-13-S2-S3