Abstract
Background
Periprosthetic infection about the knee is a devastating complication that may affect between 1% and 5% of knee replacement. With over 79 000 knee replacements being implanted each year in the UK, periprosthetic infection (PJI) is set to become an important burden of disease and cost to the healthcare economy. One of the important controversies in treatment of PJI is whether a single stage revision operation is superior to a two-stage procedure. This study sought to systematically evaluate the published evidence to determine which technique had lowest reinfection rates.
Methods
A systematic review of the literature was undertaken using the MEDLINE and EMBASE databases with the aim to identify existing studies that present the outcomes of each surgical technique. Reinfection rate was the primary outcome measure. Studies of specific subsets of patients such as resistant organisms were excluded.
Results
63 studies were identified that met the inclusion criteria. The majority of which (58) were reports of two-stage revision. Reinfection rated varied between 0% and 41% in two-stage studies, and 0% and 11% in single stage studies. No clinical trials were identified and the majority of studies were observational studies.
Conclusions
Evidence for both one-stage and two-stage revision is largely of low quality. The evidence basis for two-stage revision is significantly larger, and further work into direct comparison between the two techniques should be undertaken as a priority.
Similar content being viewed by others
Background
Knee replacement is a widely performed procedure for the management of knee arthritis. According to the 9th National Joint Registry report 79,516 knee replacements were undertaken in the UK in 2011 [1].
Surgical site infection (SSI) is estimated to complicate around 1% [2] of knee replacement and is considered amongst the most devastating complications that can affect this procedure. Based upon high quality surveillance in national programs the true rate appears to be between 3.3% [3] and 4.19% [4].
Postoperative SSI is classified by the health protection agency on the basis of depth of infection. Superficial infections are limited to the incision and superficial tissues. Deep infections involve the fascial layers and may occur up to one year post operatively where an implant is in place [5] and influences surgical management strategy [6].
Non-operative management with antibiotics is often reserved for patients unable to undergo surgery [7] and may have additional associated complications of antibiotic related organ damage.
Certain prosthesis retaining strategies may be used such as arthroscopic debridement [8], open debridement with removal of the polyethylene spacer [9] and surgical debridement, antibiotics and implant retention (DAIR) [10]. However the efficacy is somewhat controversial [11] with a poorer rate of success at eradicating the infection than more radical strategies which involve implant removal followed by implantation of a new prosthetic joint.
The most widespread technique used to perform this knee revision surgery is the two-stage method. This involves an index procedure where thorough irrigation and debridement of infected tissue is performed and the infected prosthesis is removed from the joint. In its place is usually a cement ‘spacer’. The spacer is a block of cement, often containing antibiotics, that is placed in the remaining knee space to maintain the muscle and soft tissue tension. More recently articulating spacers have been used which allow a degree of movement at the knee joint. The spacer is left within the knee joint for a period of between 6 and 8 weeks during which the patient receives parenteral antibiotics [12]. After the 6-week interval a second procedure is carried out and a new definitive prosthesis is inserted. This procedure is currently considered gold standard. The disadvantages of two-stage surgery, include the need for two operations and a potentially lengthy inpatient stay. The interval between index and second procedure can impair mobility and soft tissue contractures may develop. Mobile articulating spacers have been developed to help reduce this problem. In addition there is a significant financial burden associated with this treatment protocol [13].
An alternative to the two-stage revision is a condensed ‘one-stage’ procedure that is growing in popularity [14]. This involves a single procedure in which the definitive revision prosthesis is inserted during the index operation after removal of the infected knee replacement and an extensive debridement of all infected tissue. The potential benefits of one-stage revision are reduced morbidity, improved functional outcome as well as economic benefits [14–16].
This paper seeks to systematically review the evidence for the use of both one-stage and two-stage revision for infected knee replacement.
Methods
A systematic review of the literature was undertaken according to the methods described in the Cochrane Handbook for Systematic Review of Interventions[17].
Research question
Participants
Any patient with infected knee replacement as defined by the study reviewed.
Intervention
Revision knee surgery where all infected tissue and components are removed and a new definitive implant inserted in a single procedure. Hereafter referred to as ‘One-stage’.
Comparator
Revision knee surgery where infected tissue and components are removed and definitive implants are inserted in a separate surgical session. Hereafter referred to as ‘Two-stage’.
Primary outcome
Reinfection rate
Secondary outcomes
Functional scores at last follow up
Range of movement at last follow up
Exclusion criteria
Studies were excluded where patients were selected on the basis of having a specific subset of periprosthetic joint infection e.g. antibiotic resistant organisms.
Studies were limited to those published in the English language and humans. If studies presented a mixed group of treatments e.g. arthrodesis, one-stage and debridement, they were excluded if the treatment specific outcome was not presented. Studies reporting data on both hip and knee revision were only included if data for the knee was available for independent analysis. Case studies, abstracts, reviews and unpublished data were not included. Studies with less than one-year minimum follow up and fewer than 5 patients were excluded. Our scoping review of the literature identified that very few studies identified whether the revision surgery was preceded by previous attempts at revision. It is therefore not possible, in the majority of cases, to identify whether the cases are recurrent infection, index infection or a mixture.
Statistics
Due to the anticipated clinical heterogeneity of the studies no summative statistics were performed. The outcomes of all studies are presented in independent forest plots, with a point estimate for re-infection rate at last follow-up. 95% confidence intervals were calculated using a normal approximation interval formula for binomial data.
Search strategy
The Embase and Medline databases were searched on the 15th December 2012 using the Ovid interface. The search strategy was modified from that used by Beswick and colleagues to identify similar papers regarding treatment of infected hip replacement [18]. See Additional file 1 for search terms used.
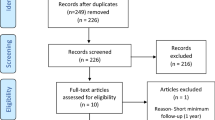
References were transferred into Endnote referencing software and duplicates were discarded. Firstly titles and abstracts were reviewed for relevance according to the research question. The remaining studies were analysed in their entirety. References of full texts were also reviewed to identify any other potentially relevant study. The acquisition of articles is summarised in a flow chart (Figure 1). Where there was discrepancy an agreement was reached by consensus.
Data were extracted by two reviewers (JM and NS), with discrepancies resolved by discussion. Authors were not contacted.
Results and discussion
The full text of 96 papers were reviewed along with an additional 13 studies identified from the review of references. There were 46 studies excluded for reasons detailed in Additional file 2. This left 58 studies of two-stage revisions (Table 1) and 5 studies of one-stage revisions (Table 2). Studies containing 45 patients or more were presented in the forest plot of two-stage studies. All studies are included in the results and discussion. The flow of this process is demonstrated in Figure 1.
No clinical trials were identified in the search; all studies found in this search were observational studies of patients who had undergone either treatment protocol. As no randomised studies were identified, no meta-analytical techniques were used due to the great clinical and statistical heterogeneity expected amongst the studies.
One-stage
Four studies (Table 2) described the outcomes of patients exclusively undergoing one-stage revision. The re-infection rates reported varied from 0% [19], 5% [20], 9.1% [21] and 11% [22].
The largest series of one-stage revisions was reported by Singer, which details the results of 63 infected knee arthroplasties. In patients with infected primary and unicompartmental knee arthroplasties (n = 43) there were no recurrences of infection within the 24 month follow up. The recurrences of infection were found in patients who had undergone previous revision surgery.
An earlier study by Buechel and colleagues found similar results; this case series of 21 patients demonstrated a re-infection rate of 9.1%.
In terms of functional outcomes, Singer et al. reported a mean Knee Society Score of 72 points after 24 months and a mean reported range of movement of 104°. Buechel et al. had a similar mean final postoperative knee score of 79.5 (range 35–94).
Two studies from the UK report a much earlier experience with the one-stage technique [19, 22] and present re-infection rates of 11% and 0%. No validated functional outcomes were reported, however the reports describe that all patients were walking and had flexion of greater than 90 and 70 degrees respectively.
One study contained cohorts of patients who had undergone one-stage and two-stage revision [23]. This study from 1987 had one patient who underwent a one-stage procedure as their index revision procedure; this patient successfully cleared the infection. One stage revision was also used in two patients who failed a prosthesis retaining debridement also successfully cleared the infection.
Two-stage revision was used as a primary revision technique in 9 patients with 1 failure. An additional two patients underwent two-stage revision having failed to clear infection after debridement. All patients in the two-stage group were identified as chronic infections. The authors report that acute infections occurring in less than two weeks were treated preferentially by component retention and debridement. This study has a single stage revision failure rate of 0/3 (0%) and a two stage failure rate of 1/11 (9%). These two results are split respectively across the two forest plots.
The re-infection rates with 95 percent confidence intervals show a very wide range (Figure 2). This highlights small study numbers.
Two-stage
58 studies reported the results of two-stage revision for infected total knee arthroplasty [12, 24–79]. Studies with greater than 45 knees are summarised in Table 1. The reinfection rates at final follow up are also summarised in Figure 3 presented with 95% confidence intervals. The remaining studies are included in the reference list.
Forest plot-two stage revisions. X-axis 1 Point estimate of reinfection rate at last follow-up which is variable (Mont 2000a-group 1 conventional two-stage revision, Mont 2000b-group 2 two stage revision with culture prior to reimplantation) ‘Borden 1987 c’ represents the two stage revision outcome presented in the paper. All estimates are presented with 95% confidence intervals.
Reinfection rates in all the studies identified range between 0 and 41%. Of the four case series with over 100 patients’ reinfection rates were 7% [51], 13% [35], 17% [44] and 28% [54]. Each of these four studies were published between 2011 and 2012.
The largest study, from Mahmud and colleagues was a retrospective review of 239 patients who underwent two-stage revision for infected TKA. The focus of this study was to establish infection free survivorship at medium interval, which was 85% at 5 years and 78% at 10 years.
They identified 16 patients who were revised for infection, but also identified 17 patients who developed aseptic causes for failure such as loosening, pain and extensor mechanism failure. The authors acknowledge that the diagnosis of periprosthetic infection is not sufficiently robust that they can guarantee these aseptic failures were indeed aseptic [51]. Those patients with successful eradication of infection also demonstrated an improvement in The WOMAC and The Knee Society Clinical Rating scores.
The preoperative WOMAC score, and The Knee Society Clinical Rating scores were 48 and 64, respectively. The postoperative WOMAC and The Knee Society Clinical Rating scores were 60 and 129, respectively.
Johnson et al. (2012) described the treatment of 110 patients (115 knees). Of these, 34 had dynamic spacers and 81 had static spacers. They had comparable rates of re-infection 6/34 (17%) in the dynamic and 14/81 (17%) in the static spacer group. However the authors acknowledge that the groups were unmatched and that the operating surgeon selected spacer type. This study also reports on a number of complications specific to dynamic spacers such as fracture and dislocation of the femoral component.
A similarly sized study from Mortazavi [54] detailed the re-infection rates of 117 knees and sought to identify operative and preoperative risk factors for failure. This group reported a relatively high re-infection rate of 28%. Using multivariate analysis to compare patients who failed two-stage treatment they identified culture negative samples, methicillin resistant organisms and increased re-implantation operative time as predictive of failure. The authors acknowledge that despite the second largest sample size in the literature presently, there is a possibility that the multivariate analysis may be underpowered for some, if not all of the variables under consideration. No functional parameters were reported in this study.
Gooding and colleagues present the outcomes from 115 infected knee replacements [35]. They sought to identify the re-infection rate and the functional outcomes with an articulating, antibiotic impregnated spacer. Fourteen of the 110 patients had a recurrence of infection of which 4 had recurrence with the same organism. 12 of the 14 failures were successfully treated with a further two-stage exchange arthroplasty. The functional arm of this study was limited by fewer than half of the cohort of patients responding to this component of follow up (n = 48). Of these 48 patients the team noted an improvement on SF-12, Oxford and WOMAC functional scores as well as an improvement in flexion deformity. Interestingly the use of logistic regression in this study failed to identify any variables that predicted failure.
An earlier study from 2000 from the same centre of 45 patients demonstrated a 91% infection clearance rate [36], with mean follow up of 48 months (20–112 months). Similarly Haleem and colleagues studied 96 knees in 94 patients with a median follow up of 7.2 years [37]. They reported 9 patients who required implant removal for reinfection. In addition they described a further 6 knees requiring revision for aseptic loosening.
Freeman and colleagues presented the results of 74 patients who underwent 76 two-stage revisions [34]. These patients were further stratified into those who received a static spacer n = 28 and those who received an articulating spacer in the interim period. They had a reinfection rate of 92.1% and 94.7% respectively. Functional comparison of these two groups by way of Knee Society Scores failed to reveal a significant difference in postoperative pain scores or functional scores. However given the limited sample size this may represent a type II error. Similarly there was no significant difference in final range of movement between the groups.
A similarly sized study [65] was the most recent of three studies from one group in the USA. This group’s most recent study of 75 knees in 72 patients had an infection eradication rate of 90.7%. This paper looked at the efficacy of the two-stage technique for antibiotic resistant infections. The eradication rate for resistant organisms was 91.2% (31/34), and 91.3% (42/46) for non-MDR organisms.
Goldman and colleagues report a reinfection rate of 9% in the 64 knees included in their study [12]. Functionally these patients achieved a mean Hospital for special surgery score of 78. Other functional assessments were made using the WOMAC tool, which was carried out in 40 of the studied cohort. 80% of the patients were satisfied with the result of their knee.
Eight studies of between 50 and 60 patients reported reinfection rates of 4% [52], 7% [32], 8% [33], 12% [59] and [70], 25% [40] and 28% [45].
Similarly to the study by Freeman and colleagues, Fehring [32] made a comparison between static (n = 25) and articulating spacers (n = 30). The reinfection rates for the different sub-types of spacer were 12% and 7% respectively. Of interest there was no significant difference in functional scores, and the final average range of movement was 98° in the static group and 105° in the articulating group.
In their cross-sectional study, Meek and colleagues identified a very low re-infection rate for their 54 patients (4%) who underwent two-stage revision with an articulating system [52]. The primary focus of this study was to compare functional outcomes in the septic revisions to those patients who underwent revision for aseptic indications. They found that those who underwent revision surgery for infection fared no worse than those who had surgery for aseptic failure. This was one of the only studies to undertake a power calculation when interpreting their comparison of functional outcomes.
By contrast the studies of Hirakawa [40] and Kalore [45] identified much higher re-infection rates of 25% and 28% respectively. These rates are among the highest of the studies identified by this systematic review.
Hirakawa’s study contained a mixed population of infected knee replacements.
The re-infection rates for two-stage revision of primary TKA was 8%, compared to 41% of the patients who underwent revision of a knee which had undergone multiple previous operations such arthroscopy and osteotomy. This was a significant difference.
Study design and quality
No study identified in this review used randomisation or blinding in treatment allocation. The overwhelming majority of studies included were single centre case series. The principle limitation of this study design is the lack of a control group for comparison of outcomes. Patient groups are further limited by surgeon selection. This makes generalisation of results difficult to the wider population. In addition a number of the studies are published from large centres; this reduces the external validity of the results.
The wide variation in re-infection rate reported in both one-stage and two-stage procedures may be explained by a number of factors. Firstly the variable definition of re-infection will affect reporting of this complication in the literature. This may be compounded by loss to follow-up and inadequate and absent data collection that frequently complicates retrospective research.
This low methodological quality means that the risk of bias in these studies is very high.
A number of studies undertook a post-hoc analysis of those who failed two-stage revision to identify any of the operative and patient based factors, which may have influenced their failure. Few showed a statistically significant difference, even with risk factors known to influence infection risk such as rheumatoid arthritis. However given the low numbers within each study, a type II error is the most likely explanation.
The forest plots for both one and two stage studies show wide ranging confidence intervals, further emphasising the difficulty in obtaining a true estimate of reinfection for each procedure. Given the gross clinical heterogeneity of the studies, any kind of meta-analysis was deemed to be of low value.
Summary
This systematic review of exchange arthroplasty for revision of infected knee arthroplasty included 63 original studies. The vast majority of the literature relates to a two-stage protocol (58 studies).
The 9th National Joint Registry of England and Wales report identified that 198 patients had undergone a one-stage revision for infection, compared to 493 patients who had the second of a two-stage revision for infection [1]. This demonstrates that whilst revision for infection might appear to be a marginal topic in the literature, it is a significant problem for practicing surgeons.
Re-infection rates for two-stage procedures varied between 0% and 41% and between 0% and 11% in one-stage procedures. The lower variability in revision rates for the one-stage procedures is likely to reflect the limited number of studies. The large variability between all the studies may also reflect the heterogeneous patients, surgeons and selection criteria. These existing studies are all susceptible to bias.
Diagnosis of infection
An important controversy in the field of SSI is diagnosis of infection. A number of parameters are usually measured in the serum, knee joint aspirate and tissue samples.
In an effort to provide a universally accepted diagnostic criteria for SSI a work group from the musculoskeletal infection society published a list of criteria based on the current evidence [80]. However this has yet to gain widespread acceptance. Newer techniques are emerging and may help with the current limitations [81, 82]. This lack of agreed definition is likely to have significant impact on the re-infection rates reported in the literature identified in our study.
A robust and widely accepted definition of periprosthetic infection will be fundamental to any future studies looking at the efficacy of any interventions for patient with this devastating complication.
Spacer type
The type of spacer used in two-stage revision was the source of interest in a number of comparative studies identified in this review [32, 34, 44, 56]. Cement spacers that allow the patient to move the knee whilst undergoing antibiotic therapy were introduced to prevent bone loss and soft tissue contraction associated with static spacer use and ultimately patient function [83].
Freeman et al. [34] found significantly more ‘excellent’ knee society scores in patients with dynamic spacers, but no difference in pain scores. Park et al. found their group of patients who received dynamic spacers to have a significantly better range of movement at final follow-up, but no significant difference in functional scoring [56].
Both Johnson [44] and Freeman [34] found no significant difference in functional scores or range of movement between the two groups.
All four of the studies identified comparable infection control between the different spacer types.
Acceptability to patient
The primary outcome measure of this systematic review is the re-infection rate. Whilst an undoubtedly important outcome in revision for infected knee arthroplasty, it is unable to describe patient satisfaction. With an ever increasing emphasis on patient reported outcomes and patient expectation any future work must take into account the acceptability to patients. Some specific work on functional outcomes in patients who have undergone two-stage revision identifies that even those who successfully cleared infection failed to return to vigorous activity [84]. A retrospective parallel case series looked at Oxford Knee score, EQ5D and satisfaction in patients who had undergone single stage and two stage revision [85]. They showed patients in each group to have similar outcomes in all measures used. The authors recommended decisions about technique should be based upon re-infection rate.
Economics
Kurtz and colleagues investigated the cost burden associated with the SSI [2]. They identified that knee arthroplasty associated with infection was associated with significantly longer inpatient stay and hospital charges. Whilst no sub-analysis was undertaken as to the different costs associated with one and two stage revision, there is likely an economic benefit to be had if one-stage revision can eradicate infection as reproducibly as two-stage revision.
Limitations
Limitations of this study relate to the narrative presentation of results that are necessarily selective. This is potentially a source of dispute and disagreement. Furthermore this study encompassed only English language studies, which was a practical limitation. We note that in previous reviews[14, 86] that there has been reference to a number of studies on single stage revision published in German [87] French[88] and Chinese [89].
Risk factors for failure and directions for future practice
Intuitively risk factors for failure of primary arthroplasty ought to remain true for revision arthroplasty. However this is less well proven in the literature. The review by Siva and colleagues in 2002 identifed gram-positive organisms, the absence of sinus formation, use of antibiotic-impregnated bone cement for fixation of the new prosthesis, and long-term use of antibiotic therapy as being associated with successful single stage revision [90]. A review of revision hip surgery alluded to similar risk factors for predicting success of single stage revision [91].
The study from Mortazavi and colleagues sought to identify risk factors for failure of two stage procedures. They identified ‘culture negative’ infection, methicillin resistant organism and extended reimplantation operative time were significantly associated with failure in their cohort [54].
Selecting patients for revision surgery should consider these factors. This has been recognized by proponents of single stage revision who advocate its use in immunocompetent patients with a known organism, in the absence of osteitis, sinus and bone loss [14, 15].
Conclusion
The perceived gold standard for revision of infected knee arthroplasty is the two-stage procedure. The studies identified in this systematic review demonstrate a much larger body of evidence to support the use of this technique over a single stage procedure. However none of the studies described here offer definitive evidence to support either technique.
Given the clear benefits for patients who befall this complication, if non-inferiority were demonstrated for the one-stage technique then one would expect the technique to gain wider acceptance. This would be best achieved in a large scale multicentre prospective randomised clinical trial.
References
National Joint Registry for England and Wales: 9th Annual report 2012. 2012, England
Kurtz SM, Lau E, Schmier J, Ong KL, Zhao K, Parvizi J: Infection burden for hip and knee arthroplasty in the United States. J Arthroplasty. 2008, 23: 984-991. 10.1016/j.arth.2007.10.017.
Lopez-Contreras J, Limon E, Matas L, Olona M, Salles M, Pujol M: Epidemiology of surgical site infections after total hip and knee joint replacement during 2007–2009: a report from the VINC at program. Enferm Infecc Microbiol Clin. 2012, 30 (Suppl 3): 26-32.
Tanner J, Padley W, Kiernan M, Leaper D, Norrie P, Baggott R: A benchmark too far: findings from a national survey of surgical site infection surveillance. J Hosp Infect. 2013, 83 (2): 87-91. 10.1016/j.jhin.2012.11.010.
Health Protection Agency: Surveillance of surgical site infections in NHS hospitals in England. 2011, London: HPA
Springer BD, Scuderi GR: Evaluation and management of the infected total knee arthroplasty. Instr Course Lect. 2013, 62: 349-361.
Tsukayama DT, Wicklund B, Gustilo RB: Suppressive antibiotic therapy in chronic prosthetic joint infections. Orthopedics. 1991, 14 (8): 841-844.
Dixon P, Parish EN, Cross MJ: Arthroscopic debridement in the treatment of the infected total knee replacement. J Bone Joint Surg Br. 2004, 86-B (1): 39-42.
Gardner J, Gioe TJ, Tatman P: Can this prosthesis be saved? implant salvage attempts in infected primary TKA. Clin Orthop Relat Res. 2011, 469: 970-976. 10.1007/s11999-010-1417-2.
Byren I, Bejon P, Atkins BL, Angus B, Masters S, McLardy-Smith P, Gundle R, Berendt A: One hundred and twelve infected arthroplasties treated with ‘DAIR’ (debridement, antibiotics and implant retention): antibiotic duration and outcome. J Antimicrob Chemother. 2009, 63 (6): 1264-1271. 10.1093/jac/dkp107.
Romano CL, Manzi G, Logoluso N, Romano D: Value of debridement and irrigation for the treatment of peri-prosthetic infections. A systematic review. Hip Int. 2012, 22 (Suppl 8): S19-S24.
Goldman RT, Scuderi GR, Insall JN: 2-stage reimplantation for infected total knee replacement. Clin Orthop Relat Res. 1996, 331: 118-124.
Oduwole KO, Molony DC, Walls RJ, Bashir SP, Mulhall KJ: Increasing financial burden of revision total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2010, 18 (7): 945-948. 10.1007/s00167-010-1074-8.
Gulhane S, Vanhegan IS, Haddad FS: Single stage revision: regaining momentum. J Bone Joint Surg Br. 2012, 94-B (11 Supple A): 120-122.
Vanhegan IS, Morgan-Jones R, Barrett DS, Haddad FS: Developing a strategy to treat established infection in total knee replacement: a review of the latest evidence and clinical practice. J Bone J Surg Br. 2012, 94 (7): 875-881.
Parkinson RW, Kay PR, Rawal A: A case for one-stage revision in infected total knee arthroplasty?. Knee. 2011, 18 (1): 1-4. 10.1016/j.knee.2010.04.008.
Cochrane Handbook for Systematic Reviews of InterventionsVersion 5.1.0. Edited by: Higgins JPT, Green S. 2011, The Cochrane Collaboration
Beswick A, Elvers K, Smith A, Gooberman-Hill R, Lovering A, Blom A: What is the evidence base to guide surgical treatment of infected hip prostheses? systematic review of longitudinal studies in unselected patients. BMC Med. 2012, 10 (1): 18-10.1186/1741-7015-10-18.
Freeman MAR, Sudlow RA, Casewell MW, Radcliff SS: The management of infected total knee replacements. J Bone Joint Surg Br. 1985, 67: 764-768.
Singer J, Merz A, Frommelt L, Fink B: High rate of infection control with one-stage revision of septic knee prostheses excluding MRSA and MRSE. Clin Orthop Relat Res. 2012, 470: 1461-1471. 10.1007/s11999-011-2174-6.
Buechel FF, Femino FP, D’Alessio J: Primary exchange revision arthroplasty for infected total knee replacement: a long-term study. Am J Orthop (Belle Mead, NJ). 2004, 33: 190-198.
Goksan SB, Freeman MAR: One-stage reimplantation for infected total knee arthroplasty. J Bone Joint Surg Br. 1992, 74: 78-82.
Borden LS, Gearen PF: Infected total knee arthroplasty. A protocol for management. J Arthroplasty. 1987, 2: 27-36. 10.1016/S0883-5403(87)80028-1.
Anderson JA, Sculco PK, Heitkemper S, Mayman DJ, Bostrom MP, Sculco TP: An articulating spacer to treat and mobilize patients with infected total knee arthroplasty. J Arthroplasty. 2009, 24: 631-635. 10.1016/j.arth.2008.04.003.
Babis GC, Zahos KA, Tsailas P, Karaliotas GI, Kanellakopoulou K, Soucacos PN: Treatment of stage III-A-1 and III-B-1 periprosthetic knee infection with two-stage exchange arthroplasty and articulating spacer. J Surg Orthop Advan. 2008, 17: 173-178.
Bengtson S, Knutson K, Lidgren L: Revision of infected knee arthroplasty. Acta Orthop Scand. 1986, 57: 489-494. 10.3109/17453678609014776.
Bose WJ, Gearen PF, Randall JC, Petty W: Long-term outcome of 42 knees with chronic infection after total knee arthroplasty. Clin Orthop Relat Res. 1995, 319: 285-296.
Choi H-R, von Knoch F, Zurakowski D, Nelson SB, Malchau H: Can implant retention be recommended for treatment of infected TKA?. Clin Orthop Relat Res. 2011, 469: 961-969. 10.1007/s11999-010-1679-8.
Cordero-Ampuero J, Esteban J, Garcia-Cimbrelo E, Munuera L, Escobar R: Low relapse with oral antibiotics and two-stage exchange for late arthroplasty infections in 40 patients after 2–9 years. Acta Orthop. 2007, 78: 511-519. 10.1080/17453670710014167.
Cuckler JM: The infected total knee: management options. J Arthroplasty. 2005, 20: 33-36.
Durbhakula SM, Czajka J, Fuchs MD, Uhl RL: Antibiotic-loaded articulating cement spacer in the 2-stage exchange of infected total knee arthroplasty. J Arthroplasty. 2004, 19: 768-774. 10.1016/j.arth.2004.02.036.
Fehring TK, Odum S, Calton TF, Mason JB: Articulating versus static spacers in revision total knee arthroplasty for sepsis. Clin Orthop Relat Res. 2000, 380: 9-16.
Ferrari R, Castelli CC, Gregis G: Preformed articulated knee spacer for the infected TKA: more than 10 years experience. Eur Cell Mater. 2011, 21: 47-
Freeman MG, Fehring TK, Odum SM, Fehring K, Griffin WL, Mason JB: Functional advantage of articulating versus static spacers in 2-stage revision for total knee arthroplasty infection. J Arthroplasty. 2007, 22: 1116-1121. 10.1016/j.arth.2007.04.009.
Gooding CR, Masri BA, Duncan CP, Greidanus NV, Garbuz DS: Durable infection control and function with the PROSTALAC spacer in two-stage revision for infected knee arthroplasty. Clin Orthop Relat Res. 2011, 469: 985-993. 10.1007/s11999-010-1579-y.
Haddad FS, Masri BA, Campbell D, McGraw RW, Beauchamp CP, Duncan CP: The PROSTALAC functional spacer in two-stage revision for infected knee replacements. Prosthesis of antibiotic-loaded acrylic cement. J Bone Joint Surg Br. 2000, 82: 807-812. 10.1302/0301-620X.82B6.10486.
Haleem AA, Berry DJ, Hanssen AD: Mid-term to long-term followup of two-stage reimplantation for infected total knee arthroplasty. Clin Orthop Relat Res. 2004, 428: 35-39.
Hart WJ, Jones RS: Two-stage revision of infected total knee replacements using articulating cement spacers and short-term antibiotic therapy. J Bone Joint Surg Br. 2006, 88: 1011-1015. 10.2106/JBJS.D.02090.
Henderson MH, Booth RE: The use of an antibiotic-impregnated spacer block for revision of the septic total knee arthroplasty. Semin Arthroplasty. 1991, 2: 34-39.
Hirakawa K, Stulberg BN, Wilde AH, Bauer TW, Secic M: Results of 2-stage reimplantation for infected total knee arthroplasty. J Arthroplasty. 1998, 13: 22-28. 10.1016/S0883-5403(98)90071-7.
Hsu YC, Cheng HC, Ng TP, Chiu KY: Antibiotic-loaded cement articulating spacer for 2-stage reimplantation in infected total knee arthroplasty: a simple and economic method. J Arthroplasty. 2007, 22: 1060-1066. 10.1016/j.arth.2007.04.028.
Husted H, Toftgaard Jensen T: Clinical outcome after treatment of infected primary total knee arthroplasty. Acta Orthop Belg. 2002, 68: 500-507.
Jhao CM, Jiang CC: Two-stage reimplantation without cement spacer for septic total knee replacement. J Formos Med Assoc. 2003, 102: 37-41.
Johnson AJ, Sayeed SA, Naziri Q, Khanuja HS, Mont MA: Minimizing dynamic knee spacer complications in infected revision arthroplasty. Clin Orthop Relat Res. 2012, 470 (0075674, dfy): 220-227.
Kalore NV, Maheshwari A, Sharma A, Cheng E, Gioe TJ: Is there a preferred articulating spacer technique for infected knee arthroplasty? A preliminary study. Clin Orthop Relat Res. 2012, 470 (0075674, dfy): 228-235.
Kohl S, Evangelopoulos DS, Kohlhof H, Krueger A, Hartel M, Roeder C, Eggli S: An intraoperatively moulded PMMA prostheses like spacer for two-stage revision of infected total knee arthroplasty. Knee. 2011, 18: 464-469. 10.1016/j.knee.2010.09.002.
Lee JK, Choi CH: Two-stage reimplantation in infected total knee arthroplasty using a Re-sterilized tibial polyethylene insert and femoral component. J Arthroplasty. 2012, 27: 1701-10.1016/j.arth.2012.03.013.
Lonner JH, Beck TD, Rees H, Roullet M, Lotke PA: Results of two-stage revision of the infected total knee arthroplasty. Am J Knee Surg. 2001, 14 (b9q, 8804841): 65-67.
MacAvoy MC, Ries MD: The ball and socket articulating spacer for infected total knee arthroplasty. J Arthroplasty. 2005, 20: 757-762. 10.1016/j.arth.2004.11.014.
Macheras GA, Kateros K, Galanakos SP, Koutsostathis SD, Kontou E, Papadakis SA: The long-term results of a two-stage protocol for revision of an infected total knee replacement. J Bone Joint Surg Br. 2011, 93 (0375355, hk7): 1487-1492.
Mahmud T, Lyons MC, Naudie DD, MacDonald SJ, McCalden RW: Assessing the gold standard: a review of 253 two-stage revisions for infected TKA knee. Clin Orthop Relat Res. 2012, 470: 2730-2736. 10.1007/s11999-012-2358-8.
Meek RMD, Dunlop D, Garbuz DS, McGraw R, Greidanus NV, Masri BA: Patient satisfaction and functional status after aseptic versus septic revision total knee arthroplasty using the PROSTALAC articulating spacer. J Arthroplasty. 2004, 19: 874-879. 10.1016/j.arth.2004.06.028.
Mont MA, Waldman BJ, Hungerford DS: Evaluation of preoperative cultures before second-stage reimplantation of a total knee prosthesis complicated by infection. A comparison-group study. J Bone Joint Surg Am. 2000, 82-A: 1552-1557.
Mortazavi SMJ, Vegari D, Ho A, Zmistowski B, Parvizi J: Two-stage exchange arthroplasty for infected total knee arthroplasty: predictors of failure. Clin Orthop Relat Res. 2011, 469: 3049-3054. 10.1007/s11999-011-2030-8.
Ocguder A, Firat A, Tecimel O, Solak S, Bozkurt M: Two-stage total infected knee arthroplasty treatment with articulating cement spacer. Arch Orthop Trauma Surg. 2010, 130: 719-725. 10.1007/s00402-010-1054-y.
Park S-J, Song E-K, Seon J-K, Yoon T-R, Park G-H: Comparison of static and mobile antibiotic-impregnated cement spacers for the treatment of infected total knee arthroplasty. Int Orthop. 2010, 34 (grf, 7705431): 1181-1186.
Pitto RP, Castelli CC, Ferrari R, Munro J: Pre-formed articulating knee spacer in two-stage revision for the infected total knee arthroplasty. Int Orthop. 2005, 29 (grf, 7705431): 305-308.
Segawa H, Tsukayama DT, Kyle RF, Becker DA, Gustilo RB: Infection after total knee arthroplasty. A retrospective study of the treatment of eighty-one infections. J Bone Joint Surg Am. 1999, 81: 1434-1445.
Van Thiel GS, Berend KR, Klein GR, Gordon AC, Lombardi AV, Della Valle CJ: Intraoperative molds to create an articulating spacer for the infected knee arthroplasty. Clin Orthop Relat Res. 2011, 469: 994-1001. 10.1007/s11999-010-1644-6.
Villanueva-Martinez M, Rios-Luna A, Pereiro J, Fahandez-Saddi H, Villamor A: Hand-made articulating spacers in two-stage revision for infected total knee arthroplasty: good outcome in 30 patients. Acta Orthop. 2008, 79: 674-682. 10.1080/17453670810016704.
Volin SJ, Hinrichs SH, Garvin KL: Two-stage reimplantation of total joint infections: a comparison of resistant and non-resistant organisms. Clin Orthop Relat Res. 2004, 427: 94-100.
Walker RH, Schurman DJ: Management of infected total knee arthroplasties. Clin Orthop Relat Res. 1984, 186: 81-89.
Wan Z, Momaya A, Karim A, Incavo SJ, Mathis KB: Preformed articulating knee spacers in 2-stage total knee revision arthroplasty. Minimum 2-year follow-up. J Arthroplasty. 2012, 27: 1469-1473. 10.1016/j.arth.2012.01.027.
Wang CJ: Management of infected total knee arthroplasty. Chang Gung Med J. 1997, 20: 1-10.
Westrich GH, Walcott-Sapp S, Bornstein LJ, Bostrom MP, Windsor RE, Brause BD: Modern treatment of infected total knee arthroplasty with a 2-stage reimplantation protocol. J Arthroplasty. 2010, 25: 1015-1021. 10.1016/j.arth.2009.07.017.
Wilde AH, Ruth JT: Two-stage reimplantation in infected total knee arthroplasty. Clin Orthop Relat Res. 1988, 236: 23-35.
Huang H-T, Su J-Y, Chen S-K: The results of articulating spacer technique for infected total knee arthroplasty. J Arthroplasty. 2006, 21 (8): 1163-1168. 10.1016/j.arth.2006.01.028.
Rosenberg AG, Haas B, Barden R, Marquez D, Landon GC, Galante JO: Salvage of infected total knee arthroplasty. Clin Orthop Relat Res. 1988, 226: 29-33.
Whiteside LA: Treatment of infected total knee arthroplasty. Clin Orthop Relat Res. 1994, 299: 169-172.
Hofmann AA, Goldberg T, Tanner AM, Kurtin SM: Treatment of infected total knee arthroplasty using an articulating spacer: 2- to 12-year experience. Clin Orthop Relat Res. 2005, 430: 125-131.
Wilson MG, Kelly K, Thornhill TS: Infection as a complication of total knee-replacement arthroplasty. Risk factors and treatment in sixty-seven cases. J Bone Joint Surg Am. 1990, 72 (6): 878-883.
Rasul AT, Tsukayama D, Gustilo RB: Effect of time of onset and depth of infection on the outcome of total knee arthroplasty infections. Clin Orthop Relat Res. 1991, 273 (0075674, dfy): 98-104.
Barrack RL, Engh G, Rorabeck C, Sawhney J, Woolfrey M: Patient satisfaction and outcome after septic versus aseptic revision total knee arthroplasty. J Arthroplasty. 2000, 15 (jay, 8703515): 990-993.
Pascale V, Pascale W: Custom-made articulating spacer in two-stage revision total knee arthroplasty. An early follow-up of 14 cases of at least 1 year after surgery. HSS J. 2007, 3 (2): 159-163. 10.1007/s11420-007-9048-1.
Rand JABR: Reimplantation for the salvage of an infected total knee arthroplasty. J Bone Joint Surg Am. 1983, 65 (8): 1081-1086.
Insall JN, Thompson FM, Brause BD: Two-stage reimplantation for the salvage of infected total knee arthroplasty. J Bone Joint Surg Am. 1983, 65: 1087-1098.
Su Y-P, Lee OK, Chen W-M, Chen T-H: A facile technique to make articulating spacers for infected total knee arthroplasty. J Chin Med Assoc. 2009, 72 (3): 138-145. 10.1016/S1726-4901(09)70039-5.
Kurd MF, Ghanem E, Steinbrecher J, Parvizi J: Two-stage exchange knee arthroplasty: does resistance of the infecting organism influence the outcome?. Clin Orthop Relat Res. 2010, 468: 2060-2066. 10.1007/s11999-010-1296-6.
Evans RP: Successful treatment of total hip and knee infection with articulating antibiotic components: a modified treatment method. Clin Orthop Relat Res. 2004, 427: 37-46.
Parvizi J, Zmistowski B, Berbari EF, Bauer TW, Springer BD, Della Valle CJ, Garvin KL, Mont MA, Wongworawat MD, Zalavras CG: New definition for periprosthetic joint infection: from the workgroup of the musculoskeletal infection society. J Arthroplasty. 2011, 26 (8): 1136-1138.
Parvizi J, McKenzie JC, Cashman JP: Diagnosis of periprosthetic joint infection using synovial C-reactive protein. J Arthroplasty. 2012, 27 (8 Suppl): 12-16.
Trampuz A, Piper KE, Jacobson MJ, Hanssen AD, Unni KK, Osmon DR, Mandrekar JN, Cockerill FR, Steckelberg JM, Greenleaf JF: Sonication of removed hip and knee prostheses for diagnosis of infection. N Engl J Med. 2007, 357 (7): 654-663. 10.1056/NEJMoa061588.
Jaekel DJ, Day JS, Klein GR, Levine H, Parvizi J, Kurtz SM: Do dynamic cement-on-cement knee spacers provide better function and activity during two-stage exchange?. Clin Orthop Relat Res. 2012, 470 (9): 2599-2604. 10.1007/s11999-012-2332-5.
Kim TWB, Makani A, Choudhury R, Kamath AF, Lee G-C: Patient-reported activity levels after successful treatment of infected total knee arthroplasty. J Arthroplasty. 2012, 27 (8, Supplement): 81-85. 10.1016/j.arth.2012.03.045.
Baker P, Petheram TG, Kurtz S, Konttinen YT, Gregg P, Deehan D: Patient reported outcome measures after revision of the infected TKR: comparison of single versus two-stage revision. Knee Surg Sports Traumatol Arthrosc. 2012
Jamsen E, Stogiannidis I, Malmivaara A, Pajamaki J, Puolakka T, Konttinen YT: Outcome of prosthesis exchange for infected knee arthroplasty: the effect of treatment approach. Acta Orthop. 2009, 80: 67-77. 10.1080/17453670902805064.
Von Foerster G, Kluber D, Kabler U: Mid- to long-term results after treatment of 118 periprosthetic infections after knee-joint replacement using one-stage revision arthroplasty. Orthopade. 1991, 20: 244-252.
Bauer T, Piriou P, Lhotellier L, Leclerc P, Mamoudy P, Lortat-Jacob A: Results of reimplantation for infected total knee arthroplasty: 107 cases. Rev Chir Orthop Reparatrice Appar Mot. 2006, 92: 692-700. 10.1016/S0035-1040(06)75930-X.
Lu H, Kou B, Lin J: One-stage reimplantation for the salvage of total knee arthroplasty complicated by infection. Zhonghua wai ke za zhi [Chinese journal of surgery]. 1997, 35: 456-458.
Silva M, Tharani R, Schmalzried TP: Results of direct exchange or debridement of the infected total knee arthroplasty. Clin Orthop Relat Res. 2002, 404: 125-131.
Jackson WO, Schmalzried TP: Limited role of direct exchange arthroplasty in the treatment of infected total hip replacements. Clin Orthop Rel Res. 2000, 381: 101-105.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2474/14/222/prepub
Acknowledgement
Samantha Johnson- University librarian.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
JM and NS designed the search strategy, conducted the search and collected the studies. Where discrepancies arose agreement was reached by discussion. JM drafted the manuscript with NS. HP did the statistical analyses and produced the forest plots. MR and PF provided critical revisions to the pre-submission manuscript. AS conceived of the study, supporting JM and NS throughout the conduct of the review process. AS also provided important critical revisions. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Masters, J.P., Smith, N.A., Foguet, P. et al. A systematic review of the evidence for single stage and two stage revision of infected knee replacement. BMC Musculoskelet Disord 14, 222 (2013). https://doi.org/10.1186/1471-2474-14-222
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2474-14-222