Abstract
Background
Taking into account our rapidly ageing population, older people are of particular interest in studying health inequalities. Most studies of older persons only include measures of current socioeconomic status (SES) and do not take into account data from earlier stages of life. In addition, only classic SES measures are used, while alternative measures, such as car ownership and house ownership, might equally well predict health. The present study aims to examine the effect of midlife socioeconomic factors on mobility limitation and depressed mood three decades later.
Methods
Data were from 4,809 men and women aged 33–65 years who participated in the Reykjavik Study (1967–1992) and who were re-examined in old age in the Age, Gene/Environment Susceptibility (AGES) -Reykjavik Study (2002–2006).
Results
Education and occupation predicted mobility limitation and depressed mood. Independently, home and car ownership and the availability of housing features predicted mobility limitation. Shortages of food in childhood and lack of a car in midlife predicted depressed mood.
Conclusion
Socioeconomic factors from midlife and from childhood affect mobility limitation and depressed mood in old age. Prevention of health problems in old age should begin as early as midlife.
Similar content being viewed by others
Background
Socioeconomic health differences are consistent across different physical and mental health outcomes, countries and settings [1]. Taking into account our rapidly ageing population, older people are of particular interest in studying health inequalities. The origins of health inequalities in old age may not only be related to circumstances in old age, but may also be traced back to early life circumstances and experiences [2, 3]. For example, low socioeconomic status (SES) in childhood is associated with higher morbidity in adulthood, independent of SES in adulthood [4, 5].
In addition, there is an emphasis on classic SES measures (i.e. education, occupation, and income), while evidence exists that alternative measures, such as car ownership and house ownership, equally well predict health [6–8]. These measures may affect health via several pathways [7, 9, 10], independent of the classic SES measures. For example, the lack of a car may affect access to adequate health care and makes shopping for healthy foods more difficult. House ownership and lack of housing features are related to housing problems, overcrowding, and exposure to damp or cold and might consequently affect health [11]. Because the ownership of a car or a house might also be status symbols, psychosocial pathways can also not be excluded [12, 13].
From a life course perspective [14], it is of interest to study the independent effects of different socioeconomic factors from earlier stages of life on old age functioning, excluding the possibility of recall bias [15]. In the present study, we use almost three decades of follow-up data from the Age, Gene/Environment Susceptibility (AGES)-Reykjavik Study to examine the independent effects of different socioeconomic factors from childhood and midlife on mobility limitation and depressed mood in old age.
Methods
Design and study population
The AGES-Reykjavik Study is drawn from the Reykjavik Study, a population-based cohort established in 1967 by investigators at the Icelandic Heart Association (IHA) [16, 17]. This cohort originally comprised a random sample of 30,795 men and women born between 1907 and 1935, residing in Reykjavik, the capital of Iceland. A random sample of 27,281 persons was invited to participate and 19,381 individuals entered the study. As part of the Reykjavik study, participants completed questionnaires and participated in a standardized medical examination. Baseline measurements took place over a period of more than 20 years, from 1967 until 1992 [18].
The follow-up examination for AGES-Reykjavik started in 2002 by randomly selecting 8,030 individuals from the people who were still alive from the original Reykjavik-cohort (n = 11,459). A total of 5,764 individuals (58% women) entered the AGES-Reykjavik Study as participants. [18] The interval between the Reykjavik Study and the AGES-Reykjavik Study ranged from 13 to 38 years (mean = 28.8, SD = 5.6).
For the present study, persons older than 65 years at baseline (n = 109) or who had missing values on occupation (n = 107) or on one or more of the measures of health-related function (n = 431 for mobility limitation and n = 377 for depressed mood – partly overlapping persons) were excluded, leaving 4,809 participants for the current analyses. Forty-three percent of this population was men. At baseline, participants were aged between 33 and 65 years (mean age = 47.5, SD = 7.1). At follow-up, participants were aged between 66 and 93 years (mean age 76.3, SD = 5.32).
AGES-Reykjavik was approved by the National Bioethics Committee in Iceland that acts as the institutional review board for the IHA (approval number VSN-00-063) and the National Institute on Aging Intramural Institutional Review Board. A multistage consent is obtained for AGES–Reykjavik to cover participation and access to administrative records. Release of data for analysis is governed by rules created by these bodies to protect the privacy of Icelandic participants [18].
Measures
Mobility limitation and depressed mood
Mobility limitation and depressed mood, as measured between 2002 and 2006, were used as indicators of physical and mental function, respectively. Mobility limitation was defined as report of any difficulty walking 500 meters or climbing 10 steps [19]. Depressed mood was measured using the 15-item version of the Geriatric Depression Scale (GDS) translated into Icelandic [20, 21]. A score of five or higher was used to indicate depressive symptoms [22].
Socioeconomic factors
Two classic measures of SES were extracted from the midlife questionnaire. Educational level was defined as the highest level of completed education among which primary school or less, secondary education, college education, and university education. Because of small numbers in the third and fourth categories, college and university levels were combined so that three categories remained for the analyses. Occupation was categorized into four (study-specific) groups. The first group was designated as ‘homemaker/miscellaneous’. For men, this group included persons identified as having jobs that did not fall into any other category. For women, this first group included homemakers only. The second group, ‘manual’, included participants engaged in heavy manual work, e.g. dockworkers, fishermen, cement workers, and farm workers. Group three, ‘service workers’, consisted of participants engaged in light skilled crafts, clerical work and services, e.g. salesmen, postal clerks, typists, and nurses. Group four, ‘professional’, were participants engaged in non-physical work, such as directors, managers, teachers, doctors, and priests.
Alternative socioeconomic factors included house ownership (tenant or owner) and car ownership (yes/no). Participants also were asked to indicate whether their home included: central heating, a water closet, a bathtub, a shower, piped cold water, and piped hot water. Three categories were then created: possession of all of these features, lack of one feature, or lack of two or more features. For the logistic regression analyses group two and three were combined due to small numbers in the last category. Finally, during the follow-up examinations, respondents were asked if they had enough to eat when growing up (‘sometimes or often not enough to eat’ versus ‘mostly to often enough to eat’).
Covariates
Covariates were derived from the midlife questionnaire and included sex, age (33–65 years), year of first examination (1967–1992), marital status (currently single/currently together with a partner), and the presence of one or more chronic diseases (currently under doctor’s care or diagnosed with one or more of the following diseases: diabetes, angina pectoris, disease of the heart valves, coronary thrombosis, another heart disease, disease of the lungs, disease of the kidneys, disease of the thyroid, disease of the stomach/intestines, osteoarthritis, glaucoma, cancer, asthma or COPD, and tuberculosis).
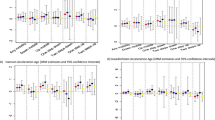
Statistical analyses
All analyses were performed using PASW version 19.0. Differences in main characteristics between men and women and educational levels were determined using chi-square tests for categorical variables and t-test and ANOVA based F-test statistics for continuous variables. Logistic regression analyses were performed to study whether socioeconomic factors were independently related to mobility limitation and depressed mood. The first model was adjusted for all covariates. The second model was additionally adjusted for all other socioeconomic factors. For all analyses, the most favorable socioeconomic position was used as a reference category.
Results
Most socioeconomic factors were distributed in the expected direction (Table 1). Men and women with lower educational levels were more likely to report performing manual jobs, lacking one or more housing features, not having a car, not having enough to eat when growing up, and to report mobility limitation and depressed mood, as compared to men and women with higher educational levels. With regard to sex differences, level of education was significantly higher in men compared with women. Seventy-four percent of women reported themselves as homemakers at the time of first examination and 38% of men were engaged in heavy manual jobs. Women were more likely than men to report not owning a car and to report mobility limitation.
Excluded persons with missing values on physical dysfunction or depressed mood at follow up were significantly more likely to be older (p < 0.001), lower educated and to do heavy manual jobs (p < 0.001) at baseline. Similarly, persons with missing values on SES at baseline were more likely to report mobility limitation at follow up (p < 0.001) (data not shown).
Interaction terms between sex and any of the socioeconomic factors on mobility limitation and depressed mood were not significant (p > 0.10). Consequently, overall (not sex-specific) results of the logistic regression analyses are presented in Table 2. Men and women with primary or secondary education or engaged in heavy manual work had the highest risk of reporting mobility limitation and depressed mood in old age.
Most other socioeconomic factors were related to an increased risk of mobility limitations and depressed mood. Even when adjusted for each other, lacking one or more housing features and not owning a car were significant predictors of mobility limitation. Not owning a car and reporting not to have enough to eat as a child were independent predictors of depressed mood three decades later.
Additional adjustment for behavioral factors (i.e. BMI, physical activity and smoking status), did not significantly change the results (data not shown).
Discussion
We were able to examine data from a cohort of 4,809 men and women with an average of 29 years of follow-up. Men and women from lower educational levels had the highest risk of mobility limitation and depressed mood almost three decades later. Independently, car ownership and the availability of housing features were predictors of mobility limitation. Recalled shortages of food in childhood and midlife car ownership were additional predictors of depressed mood.
Our findings support the hypothesis that various socioeconomic factors from childhood and midlife independently predict mobility limitation and depressed mood in old age. The independent effects of low educational and occupational level, not owning a car, lack of housing features, and shortages of food might imply different mechanistic pathways in which these factors affect health. While education relates to differences between people in terms of access to information and making (healthy) lifestyle choices, the possession of resources and the living environment may have direct effects on physical health. For example, through exposure to damp and cold, and access to fresh food [8, 23]. In addition, psychological pathways cannot be excluded either. Thus, instead of considering material factors such as car and home ownership, housing features and lack of food as ‘alternative’ measures of SES, or as mediators in the relation between SES and health, these measures could be an important, maybe the most toxic, part of the concept ‘SES’ itself.
Our findings also support the hypothesis that not only exposures during adulthood, but in early life as well are important for health in old age [3, 14]. In our study, recall of not having enough food in childhood emerged as an independent predictor of depressed mood in old age [3, 14]. The prevention of disability in old age should, at least, begin already in midlife (and perhaps even earlier) [3]. From a public health perspective, more research on this issue is needed to help develop adequate (environmental) interventions.
Strengths and limitations
The strengths of this study include a long follow-up period and the possibility to study the influence of various socioeconomic factors as measured in midlife. This study also has some limitations. First, no data on income was available which could have led to a potential for confounding by income in our analyses. For example, car and home ownership might be dependent upon income. Previous research by Macintyre and colleagues (1998), however, showed that housing tenure and car access were significant predictors of health, even after adjustment for income [7]. Also in our analyses, housing features and car ownership remained significant predictors of mobility limitation and depressed mood after adjustment for income-proxies, such as occupation and education.
Second, we were not able to exclude persons with prevalent physical dysfunction and depressed mood at baseline, however, all analyses were adjusted for the prevalence of chronic diseases at baseline. Third, socioeconomic factors and covariates were assessed only at baseline and these baseline data were collected over an unusually long period (20+ years). Socioeconomic factors could have easily changed during this time period. It is, however, unclear how these changes might have affected the results of our study. Finally, our research may be limited by potential selection biases. Excluded respondents (n = 955; described in the Methods section) were, for example, more likely to be older (p < 0.001), lower educated (p < 0.001), to report the lack of a car (p < 0.001), and not to own the house (p < 0.001), as compared to included respondents. Moreover, previous results from the Reykjavik Study [24] indicated that people from lower educational level were more likely to die prematurely. Consequently, the most disadvantaged persons may be underrepresented in the AGES-Reykjavik Study. This pattern of selective response and attrition may have led to an underestimation of the reported associations.
Conclusion
Our findings support the hypothesis that socioeconomic factors from midlife and even childhood affect mobility limitation and depressed mood in old age. Prevention of health problems in old age should thus begin as early as midlife. The independent effects of socioeconomic factors imply multiple starting points for action. More research is needed to help develop adequate environmental interventions.
Abbreviations
- AGES:
-
Age, Gene/Environment, Susceptibility Study
- PASW:
-
Predictive analytics software (formerly known as SPSS)
- ANOVA:
-
Analysis of variance
- 95% CI:
-
95% confidence interval
- OR:
-
Odds ratio
- SES:
-
Socioeconomic status
- SD:
-
Standard deviation
- BMI:
-
Body mass index
- GDS:
-
Geriatric depression scale.
References
Adler NE, Ostrove JM: Socioeconomic status and health: what we know and what we don’t. Ann N Y Acad Sci. 1999, 896: 3-15. 10.1111/j.1749-6632.1999.tb08101.x.
Kuh D: A life course approach to healthy aging, frailty, and capability. J Geron: Med Sci. 2007, 62A (7): 717-721.
Murray ET, Hardy R, Strand BH, Cooper R, Guralnik JM, Kuh D: Gender and life course occupational social class differences in trajectories of functional limitations in midlife: findings from the 1946 British Birth Cohort. J Geron: Med Sci 2011. 1946, 66A (12): 1350-1359.
Galobardes B, Davey Smith G, Lynch JW: Systematic review of the influence of childhood socioeconomic circumstances on risk for cardiovascular disease in adulthood. Ann Epidemiol. 2006, 16 (2): 91-104. 10.1016/j.annepidem.2005.06.053.
Moody-Ayers S, Lindquist K, Sen S, Covisnky KE: Childhood social and economic well-being and health in older age. Am J Epidemiol. 2007, 166 (9): 1059-1067. 10.1093/aje/kwm185.
Macintyre S, Hiscock R, Kearns A, Ellaway A: Housing tenure and car access: further exploration of the nature of their relations with health in a UK setting. J Epidemiol Community Health. 2001, 55: 330-331. 10.1136/jech.55.5.330.
Macintyre S, Ellaway A, Der G, Ford G, Hunt K: Do housing tenure and car access predict health because they are simply markers of income or self esteem? A Scottish study. J Epidemiol Community Health. 1998, 52: 657-664. 10.1136/jech.52.10.657.
Dalstra JA, Kunst AE, Mackenbach JP: A comparative appraisal of the relationship of education, income and housing tenure with less than good health among the elderly in Europe. Soc Sci Med. 2006, 62 (8): 2046-2060. 10.1016/j.socscimed.2005.09.001.
Groffen DAI, Bosma H, van den Akker M, Kempen GIJM, Van Eijk JTM: Lack of basic and luxury goods and health-related dysfunction in older persons; Findings from the SMILE study. BMC Public Health. 2008, 8: 242-10.1186/1471-2458-8-242.
Pikhart H, Bobak M, Rose R, Marmot M: Household item ownership and self-rated health: material and psychosocial explanations. BMC Public Health. 2003, 3: 38-10.1186/1471-2458-3-38.
Macintyre S, Ellaway A, Hiscock R, Kearns A, Der G, McKay L: What features of the home and the area might help to explain observed relationships between housing tenure and health? Evidence from the west of Scotland. Health Place. 2003, 9 (3): 207-218. 10.1016/S1353-8292(02)00040-0.
Bosma H, Groffen DAI, Van den Akker M, Kempen GIJM, Van Eijk JTM: Better health reports when the grass is greener on your side of the fence? A cross-sectional study in older persons. Int J Public Health. 2010, In press
Ellaway A, McKay L, Macintyre S, Kearns A, Hisock R: Are social comparisons of homes and cars related to psychosocial health?. Int J Epidemiol. 2004, 33: 1065-1071. 10.1093/ije/dyh197.
Kuh D, Ben-Shlomo Y, Lynch JW, Hallqvist J, Power C: Life course epidemiology. J Epidemiol Community Health. 2003, 57: 778-783. 10.1136/jech.57.10.778.
Coughlin SS: Recall bias in epidemiologic studies. J Clin Epidemiol. 1990, 43: 87-91. 10.1016/0895-4356(90)90060-3.
Bjornsson O, Davidsson D, Olafsson H, Olafsson O, Sigfusson N, Thorsteinsson T: Report ABC XVIII Health Survey in the Reykjavik Area - Men Stages I-III 1967–1969 1970–1971 and 1974–1976 Participants Invitation Response etc. 1979
Bjornsson G, Bjornsson O, Davidsson D, Kristjansson B, Olafsson O, Sigfusson N, Thorsteinsson T: Report ABC XXIV Health Survey in the Reykjavik Area - Women Stages I-III 1968–1969 1971–1972 and 1976–1978 Participants Invitation Response etc. 1982
Harris TB, Launer LJ, Eiriksdottir G, Kjartansson O, Johnsson PV, Sigurdsson G, Thorgeirsson G, Aspelund T, Garcia ME, Cotch MF: Age, gene/environment susceptibility-reykjavik study: multidisciplinary applied phenomics. Am J Epidemiol. 2007, 165 (9): 1076-1087. 10.1093/aje/kwk115.
Koster A, Penninx BW, Bosma H, Kempen GIJM, Harris TB, Newman AB, Rooks RN, Rubin SM, Simonsick EM, Van Eijk JTM: Is there a biomedical explanation for socioeconomic differences in incident mobility limitation?. J Gerontol A Biol Sci Med Sci. 2005, 60: 1022-1027. 10.1093/gerona/60.8.1022.
Sheikh JA, Yesavage JA: Geriatric Depression Scale (GDS): recent findings and development of a shorter version. Clinical Gerontology: A Guide to Assessment and Intervention. Edited by: Brink TL. 1986, New York: Howarth Press
Valdimarsdóttir M, Jónsson JE, Einarsdóttir S, Tómasson K: Validation of an Icelandic version of the Geriatric Depression Scale (GDS). Laeknabladid. 2000, 86 (5): 344-348.
Almeida OP, Almeida SA: Short versions of the geriatric depression scale: a study of their validity for the diagnosis of a major depressive episode according to ICD-10 and DSM-IV. Int J Geriatr Psychiatry. 1999, 14 (10): 858-865. 10.1002/(SICI)1099-1166(199910)14:10<858::AID-GPS35>3.0.CO;2-8.
Galobardes B, Lynch JW, Davey Smith G: Measuring socioeconomic position in health research. Br Med Bull. 2007, 81–82: 21-37.
Hardarson T, Gardarsdottir M, Gudmundsson KT, Thorgeirsson G, Sigvaldason H, Sigfusson N: The relationship between educational level and mortality. The Reykjavik Study. J Int Med. 2001, 249: 495-502. 10.1046/j.1365-2796.2001.00834.x.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2458/13/101/prepub
Acknowledgments
The Age, Gene/Environment Susceptibility Reykjavik Study is funded by NIH contract N01-AG-12100, the NIA Intramural Research Program, Hjartavernd (the Icelandic Heart Association), and the Althingi (the Icelandic Parliament).
The researchers are indebted to the participants for their willingness to participate in the study.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Competing interest
The authors declare that they have no competing interests.
Authors’ contributions
DG performed the statistical analyses and drafted the manuscript. AK helped to interpret the data. DG and HB formulated the hypotheses. TBH, VG, PVJ and LJL were responsible for the design of the AGES-Reykjavik Study. GE and TA were responsible for data management of the AGES-Reykjavik study. KS, PVJ were responsible for data acquisition and data preparation. All authors (DG, AK, HB, MvdA, TA, KS, GIJMK, JThMvE, GE, PVJ, LJL, VG, TBH) edited and approved the final manuscript.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Groffen, D.A., Koster, A., Bosma, H. et al. Socioeconomic factors from midlife predict mobility limitation and depressed mood three decades later; Findings from the AGES-Reykjavik Study. BMC Public Health 13, 101 (2013). https://doi.org/10.1186/1471-2458-13-101
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2458-13-101