Abstract
Background
Delirium is a common problem and associated with poor outcomes in intensive care unit (ICU) patients. Diagnosis of delirium in ICU patients is limited and usually underdiagnosed by physicians. The Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) is one of the most widely used screening methods for detection of ICU delirium. Our goal was to translate and validate the CAM-ICU for use in the Korean ICU setting.
Methods
Translation of the CAM-ICU was done according to the guidelines suggested by the Translation and Cultural Adaptation Group. For validation and interrater reliability assessment of the Korean CAM-ICU, two nurses independently assessed delirium in ICU patients and the results were compared with the reference evaluation, which was done by a psychiatrist using the Diagnostic and Statistical Manual of Mental Disorders IV (DSM-IV).
Results
Twenty-two patients were evaluated by two nurses and one psychiatrist expert independently. During the study period, we have continuously educated study nurses. Based on DSM-IV criteria, 16 out of 22 (72.7%) patients developed delirium. The sensitivities of the two nurses' evaluations using the Korean CAM-ICU were 89.80% for nurse 1 and 77.40% for nurse 2. Their specificities were 72.40% and 75.80% and their overall accuracy was 83.33% and 88.37% respectively. The Korean CAM-ICU was done with reasonable interrater reliability between nurse 1 and nurse 2 (κ = 0.81, p < 0.001).
Conclusions
The Korean CAM-ICU showed good validity and could be incorporated into clinical practice in Korean ICUs.
Trial registration
ISRCTN: ISRCTN50265663
Similar content being viewed by others
Background
Delirium is defined in the Diagnostic and Statistical Manual of Mental Disorders IV (DSM IV) as a disturbance of consciousness with inattention accompanied by a change in cognition or perceptual disturbance that develops over a short period and fluctuates over time [1]. Delirium is a common problem in patients in the intensive care unit (ICU) because of critical illness, medications, various procedures, and numerous risk factors [2]. Ely et al. reported that delirium occurred in between 81.7% and 87% of patients during their ICU stay [3–5]. Delirium itself is an independent predictor of mortality and longer hospital stay in ICU patients [5–7]. Therefore, the Society of Critical Care Medicine (SCCM) guidelines recommend routine assessment for the presence of delirium in ICU patients [8].
Despite the high prevalence and clinical importance of delirium in the ICU, detection of ICU delirium is limited, especially in mechanically ventilated patients, and delirium often goes undiagnosed by physicians [9, 10]. The Confusion Assessment Method for the ICU (CAM-ICU) is a valid, reliable tool for detection of ICU delirium and is also used in nonverbal mechanically ventilated patients. It is simple, can be assessed by nonpsychiatrists with minimal training and takes only a few minutes [3, 4, 11]. Because of these benefits, the CAM-ICU has been translated into over a dozen languages but a Korean version of the CAM-ICU is not yet available. In this study, we attempted to translate and validate the CAM-ICU for practical use in the Korean ICU setting.
Methods
Patients
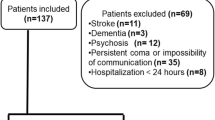
The Seoul National University Hospital institutional review board approved this study, and written informed consent was obtained from patients or their surrogates. The study population included both ventilated and nonventilated adult medical ICU patients admitted to the Seoul National University Hospital for longer than 24 hours. Exclusion criteria included patients who remained comatose throughout the investigation or were moribund, or who had a history of psychosis or neurologic disease that would confound the diagnosis of delirium. We also excluded the patient who had been already diagnosed as delirium before assessment and been prescribed antipsychotics. The study was conducted in March 2009.
Translation and Back-translation
After permission from Ely et al., translation of the instrument was carried out according to the guidelines suggested by the Translation and Cultural Adaptation group [12, 13]. The CAM-ICU was translated into Korean by the authors--doctors of pulmonology, psychiatrists and Masters students majoring in English. Each carried out their translation independently and then these were discussed. The final Korean version was given to a professional translator for back-translation to English without any information about the original version. The back-translated version was sent to Ely et al. for approval and acceptance of the Korean version.
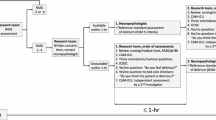
Validation of Delirium Assessment and Interrater Reliability
One research nurse and another experienced nurse specializing in intensive care independently conducted delirium assessment in the enrolled patients using the Korean version of the CAM-ICU (Korean CAM-ICU). For reference standard evaluation, an experienced psychiatrist (L-BJ) specializing in consultation psychiatrics independently assessed the delirium using the DSM-IV criteria. All assessments were done between three and seven o'clock in the afternoon to avoid any bias arising from changes in patients' condition.
To validate the Korean version, we compared the Korean CAM-ICU users to the psychiatrist ratings of delirium using the DSM-IV criteria as the reference standard. For interrater reliability, we compared the Korean CAM-ICU ratings between the two nurses by κ coefficient.
During the study period, we had times to discuss about the rating results with two nurses and the psychiatrist. In addition, we continuously educated study nurses regarding any mistakes or misconceptions. However, any rating results which had been already made were not changed after these processes.
Results
Patient Characteristics
During the 1-month study period, assessments were conducted for 16 days and 22 patients were analyzed. On each assessment day, we screened all patients admitted to medical ICU and enrolled patients who were satisfied with inclusion criteria.
The baseline characteristics of the patients are summarized in Table 1. Most patients (63.6%) were male and the median age was 68 years (range: 19-87). The most common cause of ICU admission (40.9%) was acute respiratory distress syndrome (ARDS). The median APACHE (Acute Physiology and Chronic Health Evaluation) II at admission was 25.5 (range: 9-39). Based on DSM-IV criteria, 16 out of 22 (72.7%) enrolled patients developed delirium at least once during the evaluation period.
Interrater reliability and validity of the Korean CAM-ICU
Ninety-six paired comparisons were conducted in 22 patients. Every enrolled patient was assessed more than once. Average number of assessments per patients was 4.7 and three patients were assessed more than 10 times.
For interrater reliability, nurse2 recorded feature 1 as positive in all ratings, so we were unable to determine the kappa value of feature 1. There were disagreements about the feature 1 in 22 out of 96 cases (23%) between two nurses. The kappa values of the other features were 0.91, 0.60 and 0.64 respectively (Table2). The Korean CAM-ICU was done with reasonable interrater reliability, considering all 4 items, between nurse 1 and nurse 2 (κ = 0.81, p < 0.001).
Validity of the Korean CAM-ICU
Patients who were admitted to the medical ICU more than 24 hours previously were evaluated. During the study period, 74 paired evaluations were done between nurse 1 and the psychiatric expert and 86 paired evaluations were done between nurse 2 and the psychiatric expert. The sensitivities of the two nurses' evaluations using the Korean CAM-ICU compared with the reference standard were 89.80% for nurse 1 and 77.40% for nurse 2. Their specificities were 72.40% and 75.80% and their overall accuracies were 83.33% and 88.37% respectively (Table 3).
Discussion
The sensitivity and specificity of the Korean CAM-ICU was 89.8% and 77.4%, respectively, for nurse 1 and 72.4% and 75.8% for nurse 2. Overall agreement (κ) between nurse 1 and nurse 2 was 0.81 (p < 0.001). Compared with the original validation study of the CAM-ICU (sensitivity = 100%, 93%, specificity = 98%, 100%) [3], the Korean CAM-ICU showed a little lower sensitivity, specificity and kappa value. Ely et al., who originally devised the CAM-ICU, explained that the assessors also interviewed patients' family members to estimate their baseline mental status [3, 4]. In practice, interviews with patients' families are not easy and our study nurses could not perform such family interviews. Feature 1 is the one of 2 essential components for diagnose delirium using the CAM-ICU. Therefore, knowing the patient's baseline mental status is very important thing. In this study, we couldn't get direct information of patients' baseline mental status from patients' family and just presumed from previous medical records. That might be one of limitations of this study.
Ely et al. conducted a study to determine the feasibility of implementing the CAM-ICU [14]. Overall agreement (κ) between two different hospitals (one the hospital where the original validation study of the CAM-ICU was performed) was initially very low (κ = 0.2, 0.03). However, this was much improved (κ = 0.92, 0.75, respectively) through an education period.
We have several limitations in this study. First, we don't have exact number and detailed clinical information of excluded patients even though we screened all patients admitted to medical ICU. This may have an effect on the representativeness of enrolled patients and the results of this study. Second, most patients had been assessed several times and the data might be correlated and independent. Third, the time between the assessments was various. While some patients had been evaluated for 3 to 4 consecutive days, other patients were evaluated at admission and then just before leaving the ICU due to their medical conditions.
Conclusions
The Korean version of the CAM-ICU showed good validity and could be incorporated into clinical practice in Korean ICUs. However, we should remember that sufficient education and a feedback process are needed during the introductory period. We hope that the Korean CAM-ICU will help clinicians detect delirium in the ICU and eventually improve the outcome of patients in the ICU through reducing the incidence of delirium and its potential complications.
Abbreviations
- ICU:
-
Intensive Care Unit
- CAM-ICU:
-
The Confusion Assessment Method for the Intensive Care Unit
- DSM-IV:
-
The Diagnostic and Statistical Manual of Mental Disorders IV
- APACHE II:
-
Acute Physiology And Chronic Health Evaluation II
- ARDS:
-
Acute Respiratory Distress Syndrome.
References
American Psychiatric Association: Diagnostic and statistical manual of mental disorders (DSM-IV). 1994, Washington, DC: American Psychiatric Association, 4
Girard TD, Pandharipande PP, Ely EW: Delirium in the intensive care unit. Crit Care. 2008, 12 (Suppl 3): S3-
Ely EW, Inouye SK, Bernard GR, Gordon S, Francis J, May L, Truman B, Speroff T, Gautam S, Margolin R, Hart R, Dittus R: Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU). JAMA. 2001, 286: 2703-2710. 10.1001/jama.286.21.2703.
Ely EW, Margolin R, Francis J, May L, Truman B, Dittus R, Speroff T, Gautman S, Bernard GR, Inouye SK: Evaluation of delirium in critically ill patients: validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). Crit Care Med. 2001, 29: 1370-1379. 10.1097/00003246-200107000-00012.
Ely EW, Shintani A, Truman B, Speroff T, Gordon SM, Harrell FE, Inouye SK, Bernard GR, Dittus RS: Delirium as a predictor of mortality in mechanically ventilated patients in the intensive care unit. JAMA. 2004, 291: 1753-1762. 10.1001/jama.291.14.1753.
Lin SM, Liu CY, Wang CH, Lin HC, Huang CD, Huang PY, Fang YF, Shieh MH, Kuo HP: The impact of delirium on the survival of mechanically ventilated patients. Crit Care Med. 2004, 32: 2254-2259.
Thomason JW, Shintani A, Peterson JF, Pun BT, Jackson JC, Ely EW: Intensive care unit delirium is an independent predictor of longer hospital stay: a prospective analysis of 261 non-ventilated patients. Crit Care. 2005, 9: R375-R381. 10.1186/cc3729.
Jacobi J, Fraser GL, Coursin DB, Riker RR, Fontaine D, Wittbrodt ET, Chalfin DB, Masica MF, Bjerke HS, Coplin WM, Crippen DW, Fuchs BD, Kellenher RM, Marik PE, Nasraway SA, Murray MJ, Peruzzi WT, Lumb PD: Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med. 2002, 30: 119-141. 10.1097/00003246-200201000-00020.
Peterson JF, Pun BT, Dittus RS, Thomason JW, Jackson JC, Shintani AK, Ely EW: Delirium and its motoric subtypes: a study of 614 critically ill patients. J Am Geriatr Soc. 2006, 54: 479-484. 10.1111/j.1532-5415.2005.00621.x.
Ely EW, Stephens RK, Jackson JC, Thomason JW, Truman B, Gordon S, Dittus RS, Bernard GR: Current opinions regarding the importance, diagnosis, and management of delirium in the intensive care unit: a survey of 912 healthcare professionals. Crit Care Med. 2004, 32: 106-112. 10.1097/01.CCM.0000098033.94737.84.
Inouye SK, Bogardus ST, Williams CS, Leo-Summers L, Agostini JV: The role of adherence on the effectiveness of nonpharmacologic interventions: evidence from the delirium prevention trial. Arch Intern Med. 2003, 163: 958-964. 10.1001/archinte.163.8.958.
Beaton DE, Bombardier C, Guillemin F, Ferraz MB: Guidelines for the process of cross-cultural adaptation of self-report measures. Spine. 2000, 25: 3186-3191. 10.1097/00007632-200012150-00014.
Wild D, Grove A, Martin M, Eremenco S, McElroy S, Verjee-Lorenz A, Erikson P: Principles of Good Practice for the Translation and Cultural Adaptation Process for Patient-Reported Outcomes (PRO) Measures: Report of the ISPOR Task Force for Translation and Cultural Adaptation. Value Health. 2005, 8: 94-104. 10.1111/j.1524-4733.2005.04054.x.
Pun BT, Gordon SM, Peterson JF, Shintani AK, Jackson JC, Foss J, Harding SD, Bernard GR, Dittus RS, Ely EW: Large-scale implementation of sedation and delirium monitoring in the intensive care unit: a report from two medical centers. Crit Care Med. 2005, 33: 1199-1205. 10.1097/01.CCM.0000166867.78320.AC.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-244X/11/94/prepub
Acknowledgements and Funding
This work was supported by a Grant (04-2008-006-0) from the Seoul National University Hospital Research Fund. We thank Professor E. Wesley Ely for his approval and research nurse specialists for their support in the ICU Delirium and Cognitive Impairment Study Group. We are grateful to the doctors and nurses of the medical intensive care units and all the translators. No authors have financial interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
HEY: analysis of data and manuscript preparation. LBJ and HBJ: assessment of delirium and analysis of data. SHE and LHA: important contribution to acquisition of data. YCG, KYW HSK and SYS: interpretation of data and manuscript review. LSM: study design, interpretation of data and manuscript preparation.
All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Heo, E.Y., Lee, BJ., Hahm, BJ. et al. Translation and validation of the Korean confusion assessment method for the intensive care unit. BMC Psychiatry 11, 94 (2011). https://doi.org/10.1186/1471-244X-11-94
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-244X-11-94