Abstract
Background
Carcinosarcoma of the colon is a rare histopathological entity with uncertain histogenesis, that shows both epithelial and mesenchymal malignant differentiation. Carcinosarcoma rarely affects the gastrointestinal tract and only few cases are reported in the colon. Herein we describe a carcinosarcoma of the ascending colon, with morphological, ultrastructural and molecular analysis.
Case presentation
An 81-year-old man was hospitalised for asthenia, weight loss and iron-deficiency anaemia. The patient underwent colonoscopy and adenocarcinoma was diagnosed by endoscopic biopsy. A right hemicolectomy was performed and, during surgical operation, liver metastases were detected. Histological examination of the surgical specimen revealed areas of both carcinomatous and sarcomatous differentiation, completely separated by fibrous septae. The sarcomatous component exhibited areas of smooth muscle and osteoblastic differentiation, with focal osteoid material deposition. Molecular analysis conducted separately on the epithelial and mesenchymal components revealed the same p53 gene mutation (R282W in exon 8) and identical polymorphisms in p53 exon 4, in EGFR exons 20 and 21, and in c-kit exon 17. Microsatellite markers analysis revealed a common loss of heterozygosis on 18q. Overall, the data are consistent with a common origin of the two tumor components. The patient was treated with 8 cycles of oral capecitabine (1250 mg/m2 twice a day for 14 days repeated every 28 days) and two years after surgery is alive with liver metastases.
Conclusion
Carcinosarcoma of the colon is a rare tumour with both epithelial and sarcomatous components. Molecular analysis of the current case suggests the histogenesis from a common cell progenitor.
Similar content being viewed by others
Background
Carcinosarcoma is a rare histopathological entity, exhibiting both epithelial and mesenchymal malignant differentiation, with uncertain histogenesis. Carcinosarcoma has been described in various organs, although head and neck, and female urogenital system are the most frequent sites of occurrence [1]. In the gastrointestinal tract, carcinosarcoma arises predominantly in the oesophagus, in the stomach and in the biliary tract [2], whereas carcinosarcoma of the large intestine has been reported only rarely. This type of tumour generally displays an aggressive behaviour and poor prognosis. Herein we present a case of carcinosarcoma of the ascending colon.
Case presentation
Clinical features
An 81-year-old man with a past medical history of atherosclerotic heart disease, arterial hypertension, mitral insufficiency, bilateral carotid artery disease and early chronic renal failure was hospitalised for asthenia and weight loss. Laboratory investigation revealed iron-deficiency anaemia, with low haemoglobin (Hb) concentration (7.8 g/dl; normal range: 13–17 g/dL), median cellular volume (MCV) level (67.2 fl; normal range: 80–97 fl) and serum ferritin concentration (3.3 ng/mL; normal range: 30–400 ng/dL). Serum levels of carcinoembryonic antigen (CEA), carbohydrate antigen (CA) 19-9 and alphafoetoprotein (AFP) were within normal limits. Stool guaiac was positive for occult blood. Colonoscopy demonstrated an exophytic mass in the ascending colon and multiple diverticula in the entire colon, especially in the sigmoid region. Endoscopic biopsies were performed and at histological examination, adenocarcinoma was diagnosed. Chest x-ray was negative for metastatic disease. A week later a right hemicolectomy and regional lymph node dissection were performed. During surgery, liver metastases were detected. Computer tomography (CT) scan carried out after surgery identified 3 liver nodules in segment 4, in segment 8 and in segment 5, measuring 15 cm, 10 cm and 10 cm in their greatest dimension, respectively. The patient was subsequently treated with capecitabine at 1250 mg/m2 orally twice a day for 14 days repeated every 28 days for 8 cycles. Capecitabine was chosen for adjuvant therapy in this case since it has been reported to be as effective as 5-fluorouracil but with milder side effects in stage III colon cancer [3]. No specific chemotherapeutic agents have been shown to be effective in carcinosarcoma [4]. Two years after surgical treatment, the patient is alive with liver metastases.
Pathological features
Methods
Representative sections of the tumour and all lymph nodes isolated from the surrounding adipose tissue were fixed in 10% buffered neutral formalin, embedded in paraffin and routinely processed. From each block, 5 μm-thick sections were cut and stained with haematoxylin and eosin (H&E).
For immunohistochemical studies, the avidin-biotin peroxidase complex method was used with the following antibodies: cytokeratin 20 (CK20), desmin, vimentin, S-100, c-kit, CD34, sarcomeric actin, smooth muscle actin, osteonectin. The antibodies used are detailed in Table 1.
For ultrastructural examination, small samples were retrieved from paraffin-embedded material, deparaffinised in xylene, rehydrated in ethanol, post-fixed in osmium tetroxyde (OsO4), dehydrated and embedded in epoxy resin. Ultrathin sections were counterstained in uranile acetate and lead citrate and observed in a Jeol JEM 1010 (Tokyo, Japan) electron microscope operating at 80 kV.
For the molecular detection of somatic genetic alterations, the p53 gene (exons 4 through 9), the c-kit gene (exons 9, 11, 13 and 17) and the EGFR gene (kinase domain, exons 18 through 21) were evaluated by denaturing high-performance liquid chromatography (DHPLC) technique (The WAVE™ Nucleic Acid Fragment Analysis System, Transgenomic Inc., Nebraska, USA), followed by direct sequencing when required. K-Ras gene mutation status was assessed by direct sequencing. Distinct formalin-fixed paraffin-embedded material from both carcinomatous and sarcomatous components of the tumour was isolated by macrodissection. Genomic DNA was extracted by the phenol-chloroform method. Fifty ng of DNA were used for the specific amplification of all the exons listed above, as previously described [5–7]. After the polymerization reaction, all PCR (Polymerase Chain Reaction) products were visualised on a 2% agarose gel; 10 μl of the PCR product were denatured at 95°C and slowly cooled to room temperature to ensure equimolar homo- and heteroduplexes formation prior being loaded for DHPLC analysis. The running methods used are listed in Table 2. All samples that showed an elution profile different from a wild type control underwent direct sequencing by BigDye® Terminator v1.1 Cycle Sequencing Kit chemistry, purified by DyeEx 2.0 Spin kit (Qiagen, Hilden, Germany) and analysed by capillary electrophoresis on Abi Prism 310 (Applied Biosystem, Foster City, California, USA). Sequences obtained were aligned with normal sequences and examined for detection of mutations. For allelic status testing, 10 microsatellite markers on chromosomal arms 9p, 11p, 13q, 17q and 18q were investigated (Rb, D9S171, D11S1336, D13S258, D13S317, D13S631, D17S855, D18S35, D18S51 and D18S585). Specific PCRs with fluorescent primers were conducted followed by loss of heterozygosis (LOH) analysis with GeneScan software (Applied Biosystem, Foster City, California, USA).
Results
The surgical specimen included a 4 cm long ileal segment, a 13.5 cm long colonic segment, and the caecal appendix. At the ileocaecal valve, on the colonic side, an exophytic, centrally ulcerated mass, measuring 7 cm in its greatest dimension, was documented. Twenty-two lymph nodes were isolated from the adipose tissue surrounding the bowel wall.
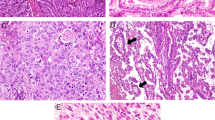
Microscopically, about 70% of the tumour displayed features of moderately differentiated adenocarcinoma, invading the subserosa (pT3). The carcinoma was composed of neoplastic epithelial cells, arranged in nests forming glandular structures with areas of central necrosis. Neoplastic epithelial cells exhibited rare mitotic figures, an increased nuclear/cytoplasmic ratio and prominent nucleoli. Approximately 30% of the tumour presented mesenchymal features. The sarcomatous component was completely separated from its carcinomatous counterpart by fibrous septae (Fig. 1). In the sarcomatous component, fascicular spindle cells admixed with bizarre large cells and focal osteoid-like matrix deposition were found. Fascicular spindle cells showed a moderately eosinophilic cytoplasm, with slightly enlarged nuclei. Large cells were markedly pleomorphic and exhibited enormously swollen nuclei with irregularly dispersed chromatin, focally surrounding areas of osteoid material deposition in the extracellular matrix. Metastasis of adenocarcinoma (N1) was found in 1 out of 22 lymph nodes detected. According to the TNM classification [8], the pathological stage was pT3N1.
The epithelial component was immunoreactive for CK20 in approximately 30% of neoplastic cells, whereas it was negative for vimentin and osteonectin. In the mesenchymal component, spindle cells were diffusely immunoreactive for smooth muscle actin (Fig. 2) and partially positive for vimentin, while large cells were focally immunoreactive for osteonectin (Fig. 3). Both the epithelial component and the mesenchymal component were negative for S100, desmin, CD34, c-kit and sarcomeric actin.
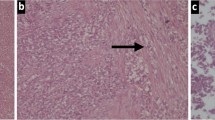
Ultrastructural examination was performed on both epithelial and mesenchymal areas of differentiation. Epithelial cells were organised in glandular structures encircled by basal membrane and showed typical surface microvilla and basal hemidesmosomes (Fig. 4A). Spindle cells exhibited myofibroblastic differentiation with peripheral cytoplasmic thin filaments and interspersed focal densities (Fig. 4B). There was no admixture of the two components.
Ultrastructural examination: (a) Carcinomatous component: glandular epithelial structure with surface microvilla (arrow); in the inset: enlargement of the basement membrane (arrow) and hemidesmosomes (red arrows). (b) Sarcomatous component: spindle cells with actin cytoplasmic thin filaments and focal densities (enlargement in the inset). Scale bar: 2µm.
The molecular screening performed to detect mutations revealed in both tumour components the same mutation R282W in exon 8 of the p53 gene (Figs. 5A, 5B). No mutation was found in the k-ras gene. Although no mutations could be detected, identical polymorphisms were identified in the carcinomatous as well as in the sarcomatous components in p53 exon 4, in EGFR exons 20 and 21, and in c-kit exon 17. The microsatellite analysis evidenced shared allelic retentions and loss among the epithelial and the mesenchymal neoplastic counteparts. Of the 10 STRs (Short Tandem Repeats) investigated, 7 were considered informative and four of them displayed an identical pattern comparing normal and the two tumoral components. An almost complete loss of the second allele was appreciated for D18S585, D18S35 and D18S51 markers (18q21) in both tumor' parts (Fig. 6).
DHPLC diagram and p53 sequencing analysis. (a) DHPLC diagram. The carcinomatous component is represented in black while the sarcomatous component in red and the wild-type control sample in blue. The same genetic alteration in both tumour components is illustrated by the presence of an extra peak in the neoplastic specimens in comparison with the normal control. (b) Sequencing analysis showing p53 exon 8 mutation R282W (arrow).
Discussion
Carcinosarcoma is widely considered a rare, highly aggressive tumour. Carcinosarcoma of the colon was first reported by Weidner et al in 1986 [9] and to the best of our knowledge, cases of colon carcinosarcomas and sarcomatoid carcinomas reported in literature are 17 [4, 9][10–12][13–15][16–18][19–21][22–24], summarised in Table 3. Affected patients show an age between 41 and 84 years, with a median age of 66 years and a slight predilection for women. Lymph nodes and distant sites metastases disclose a predominance of the carcinomatous component. Shah et al reported even an increased epithelial component in the spleen metastasis, comparing with the primary colon site [19]. Only one case with a metastasis from the sarcomatous component was documented [18].
Herein we report a carcinosarcoma with distinct epithelial and mesenchymal components, at the morphological, immunohistochemical and ultrastructural levels. Moreover, the sarcomatous component was composed of cells reminiscent of smooth muscle differentiation and cells with osteoblastic appearance. Some authors classified as large bowel carcinosarcomas epithelial tumours with areas of sarcomatoid differentiation, weakly immunoreactive for cytokeratins and with no evidence of osteosarcomatous nor chondrosarcomatous differentation [12, 13, 20, 21]. According to Aramendi et al., these cases are not properly carcinosarcomas, but should be considered sarcomatoid poorly differentiated carcinomas [23]. In the present case, the sarcomatous component completely lacked any epithelial signs of differentiation; furthermore, we noted areas of osteosarcomatous differentiation and osteoid material deposition. The topographic distribution was remarkable for the complete separation of the two components. Ultrastructural examination confirmed such distinct separation. Bertram et al. instead reported intermixed epithelial and mesenchymal components [14]. Other authors have classified as carcinosarcomas or sarcomatoid carcinomas tumours with sarcomatous features immunoreactive for cytokeratin and epithelial membrane antigen (EMA), but lacking carcinomatous component [4, 15, 16]. Shoji highlights the difficulty in making the correct diagnosis, since sarcomatous component closely resembles sarcoma, except for cytokeratin-immunoreactivity [16].
Treatment, as underlined by Bertram et al., should follow guidelines for common colon adenocarcinomas [14] and the poor prognosis associated with this tumour should require a strict follow-up. Remarkably, the patient reported here is still alive, two years after surgical resection of the primary tumour, despite the presence of liver metastases. Therefore we believe that aggressive therapy may be indicated in these tumours.
The histogenesis of carcinosarcoma is still controversial. Morphologically, the presence of distinct carcinomatous and sarcomatous components suggests a different origin (multiclonal hypothesis). The molecular analysis performed in the current case supports the hypothesis of a common cell precursor (monoclonal hypothesis), since the same mutation R282W in exon 8 of the p53 gene as well as the same allelic status, with the loss of 18q21, were identified in both carcinomatous and sarcomatous components.
Studies conducted on carcinosarcomas of nasopharynx [25], uterus [26, 27] and breast [28], documented a large overlap of cytogenetic and molecular alterations in the two tumour components. Furthermore, Van Rees et al. [29] described an uncommon case of adenosquamous carcinoma raised in a Barrett esophagus where the two malignant components showed loss of the same allele at all informative chromosomal markers tested as well as the same missense mutation in the p53 tumor-suppressor gene. All these findings are consistent with our results suggesting the hypothesis of a common progenitor of both epithelial and mesenchymal components. Therefore morphological divergence, even at the extreme levels displayed by carcinosarcomas, necessarily appears late in tumor progression, well after the initial hits that cause cancer.
Conclusion
Herein we describe a case of carcinosarcoma of the colon, with epithelial and mesenchymal components, completely different and separate at the morphological, immunohistochemical and ultrastructural levels. Molecular analysis revealed the same mutation R282W in exon 8 of the p53 gene and identical LOH for D18S585, D18S35 and D18S51 in both carcinomatous and sarcomatous components, supporting the hypothesis of a common cell progenitor.
References
Wick MR, Swanson PE: Carcinosarcomas: current perspectives and an histological review of nosological concepts. Semin Diagn Pathol. 1993, 10: 118-127.
Iezzoni JC, Mills SE: Sarcomatoid carcinomas (carcinosarcomas) of the gastrointestinal tract: a review. Semin Diagn Pathol. 1993, 10: 176-187.
Twelves C, Wong A, Nowacki MP, Abt M, Burris H, Carrato A, Cassidy J, Cervantes A, Fagerberg J, Georgoulias V, Husseini F, Jodrell D, Koralewski P, Kroning H, Maroun J, Marschner N, McKendrick J, Pawlicki M, Rosso R, Schuller J, Seitz JF, Stabuc B, Tujakowski J, Van Hazel G, Zaluski J, Scheithauer W: Capecitabine as adjuvant treatment for stage III colon cancer. N Engl J Med. 2005, 352: 2696-704. 10.1056/NEJMoa043116.
Kim N, Luchs JS, Halpern D, Davis E, Donovan V, Weston SR, Katz DS: Radiology-pathology conference: carcinosarcoma of the colon. J Clin Imag. 2005, 29: 259-262. 10.1016/j.clinimag.2004.09.002.
Lynch TJ, Bell DW, Sordella R, Gurubhagavatula S, Okimoto RA, Brannigan BW, Harris PL, Haserlat SM, Supko JG, Haluska FG, Louis DN, Christiani DC, Settleman J, Haber DA: Activating Mutations in the Epidermal Growth Factor Receptor Underlying Responsiveness of Non-Small-Cell Lung Cancer to Gefitinib. N Engl J Med. 2004, 350: 2129-2139. 10.1056/NEJMoa040938.
Romagnoli S, Graziani D, Bramerio M, Gambacorta M, Colombo P, Roncalli M, Coggi G, Bosari S: Immunohistochemical profile and c-kit mutations in gastrointestinal stromal tumors. Pathol Res Pract. 2005, 201: 71-81. 10.1016/j.prp.2005.01.005.
Marchetti A, Buttitta F, Merlo G, Diella F, Pellegrini S, Pepe S, Macchiarini P, Chella A, Angeletti CA, Callahan R: p53 alterations in non-small cell lung cancers correlate with metastatic involvement of hilar and mediastinal lymph nodes. Cancer Res. 1993, 53: 2846-2851.
Sobin LH, Wittekind Ch, Eds: TNM classification of malignant tumours. 2002, New York: John Wiley & Sons
Weidner N, Zekan P: Carcinosarcoma of the colon – Report of a unique case with light and immuoistochemical studies. Cancer. 1986, 58: 1126-1130. 10.1002/1097-0142(19860901)58:5<1126::AID-CNCR2820580525>3.0.CO;2-Q.
Staroz F, Botton A, Potet F: Tumeurs malignes du colon a double composante (carcinosarcomes). A propos d'un cas. Ann Pathol. 1995, 15: 457-458.
Roncaroli F, Montironi R, Feliciotti F, Losi L, Eusebi V: Sarcomatoid carcinoma of the anorectal junction with neuroendocrine and rhabdomyoblastic features. Am J Surg Pathol. 1995, 19: 217-223.
Isimbaldi G, Sironi M, Assi A: Sarcomatoid carcinoma of the colon: report of the second case with immuonohistochemical study. Pathol Res Pract. 1996, 192: 483-487.
Gentile R, Castellaneta A: Carcinosarcoma of the colon, one or two tumors?. Pathologica. 1997, 89: 62-68.
Bertram P, Treutner KH, Lietze L, Schumpelick V: True carcinosarcoma of the colon. Langenbecks Arch Chir. 1997, 382: 173-174.
Serio G, Aguzzi A: Spindle and giant cell carcinoma of the colon. Histopathology. 1997, 30: 383-358. 10.1046/j.1365-2559.1997.d01-610.x.
Shoji M, Dobashi Y, Iwabuchi K, Kuwao S, Mikami T, Kameya T: Sarcomatoid carcinoma of the descending colon – A histological, immunoistochemical and ultrastructural analysis. Acta Oncol. 1998, 37: 765-768. 10.1080/028418698430179.
Nakao A, Sakagami K, Uda M, Mitsuoka S, Ito H: Carcinosarcoma of the colon: report of a case and review of the literature. J Gastroenterol. 1998, 33: 276-279. 10.1007/s005350050083.
Takeyoshi I, Yoshida M, Ohwada S, Yamada T, Yanagisawa A, Morishita Y: Skin metastasis from the spindle cell component in rectal carcinosarcoma. Hepatogastroenetrology. 2000, 47: 1611-1614.
Shah S, Kim DH, Harster G, Hossain A: Carcinosarcoma of the colon and spleen – A fleshy purple mass on colonoscopy. Dig Dis Sci. 2001, 46: 106-108. 10.1023/A:1005682413793.
Kim JH, Moon WS, Kang MJ, Park MJ, Lee DG: Sarcomatoid carcinoma of the colon: a case report. J Korean Med Sci. 2001, 16: 657-660.
Di Vizio D, Insabato L, Zafonte BT, Ferrara G, Pettinato G: Sarcomatoid carcinoma of the colon: a case reoport with literature review. Tumori. 2001, 87: 431-435.
Ishida H, Ohsawa T, Nakada H, Hashimoto D, Ohkubo T, Adachi A, Itoyama S: Carcinosarcoma of the rectosigmoid colon: report of a case. Surg Today. 2003, 33: 545-549.
Aramendi T, Fernández-Aceñero MJ, Villanueva MC: Carcinosarcoma of the colon: report of a rare tumor. Pathol Res Pract. 2003, 199: 345-348. 10.1078/0344-0338-0428.
Macaigne G, Aouad K, Boivin JF, Bellaïche A, Auriault ML, Picard D, Deplus R: Carcinome sarcomatoïde du colon: presentation d'un cas et revue de la littérature. Gastroenterol Clin Biol. 2004, 28: 600-604.
Torenbeek R, Hermsen MAJA, Meijer GA, Baak JPA, Meijer CJLM: Analysis by comparative genomic hybridization of epithelial and spindle cell components in sarcomatoid carcinoma and carcinosarcomas: histogenetic aspects. J Pathol. 1999, 189: 338-343. 10.1002/(SICI)1096-9896(199911)189:3<338::AID-PATH429>3.0.CO;2-Q.
Thompson L, Chang B, Barsky SH: Monoclonal origins of malignant mixed tumors (carcinosarcomas): evidence for a divergent histogenesis. Am J Surg Pathol. 1996, 20: 277-185. 10.1097/00000478-199603000-00003.
Gorai I, Yanagibashi T, Taki A, Udagawa K, Miyagi E, Nakazawa T, Hirahara F, Nagashima Y, Minaguchi : Uterine carcinosarcoma is derived from a single stem cells: an in vitro study. Int J Cancer. 1997, 72: 821-827. 10.1002/(SICI)1097-0215(19970904)72:5<821::AID-IJC19>3.0.CO;2-B.
Wada H, Enomoto T, Tsujimoto M, Nomura T, Murata Y, Shroyer KR: Carcinosarcoma of the breast: molecular-biological study for analysis of histogenesis. Hum Pathol. 1998, 29: 1324-1328. 10.1016/S0046-8177(98)90266-0.
Van Rees B, Rouse R, De Wit M, Van Noesel C, Tytgat G, Lanschot J, Offerhaus G: Molecular evidence for the same clonal origin of both components of an adenosquamous barrett carcinoma. Gastroenterology. 2002, 122: 784-788. 10.1053/gast.2002.31903.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2407/6/185/prepub
Acknowledgements
We thank Patrizia Doi for immunohistochemical studies and Maria Saponaro for molecular studies. Written consent was obtained from the patient for publication of study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
AAS revised the literature and drafted the manuscript. VV conducted the molecular analysis and participated in writing the manuscript. PB carried out the ultrastructural examination. MR performed the surgical operation and clinical follow-up. SF and SB devised the study and revised the manuscript. All the authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Ambrosini-Spaltro, A., Vaira, V., Braidotti, P. et al. Carcinosarcoma of the colon: report of a case with morphological, ultrastructural and molecular analysis. BMC Cancer 6, 185 (2006). https://doi.org/10.1186/1471-2407-6-185
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2407-6-185