Abstract
Background
The mannose 6-phosphate/insulin-like growth factor 2 receptor (M6P/IGF2R) encodes for a multifunctional receptor involved in lysosomal enzyme trafficking, fetal organogenesis, cytotoxic T cell-induced apoptosis and tumor suppression. The purpose of this investigation was to determine if the M6P/IGF2R tumor suppressor gene is mutated in human head and neck cancer, and if allelic loss is associated with poor patient prognosis.
Methods
M6P/IGF2R loss of heterozygosity in locally advanced squamous cell carcinoma of the head and neck was assessed with six different gene-specific nucleotide polymorphisms. The patients studied were enrolled in a phase 3 trial of twice daily radiotherapy with or without concurrent chemotherapy; median follow-up for surviving patients is 76 months.
Results
M6P/IGF2R was polymorphic in 64% (56/87) of patients, and 54% (30/56) of the tumors in these informative patients had loss of heterozygosity. M6P/IGF2R loss of heterozygosity was associated with a significantly reduced 5 year relapse-free survival (23% vs. 69%, p = 0.02), locoregional control (34% vs. 75%, p = 0.03) and cause specific survival (29% vs. 75%, p = 0.02) in the patients treated with radiotherapy alone. Concomitant chemotherapy resulted in a better outcome when compared to radiotherapy alone only in those patients whose tumors had M6P/IGF2R loss of heterozygosity.
Conclusions
This study provides the first evidence that M6P/IGF2R loss of heterozygosity predicts for poor therapeutic outcome in patients treated with radiotherapy alone. Our findings also indicate that head and neck cancer patients with M6P/IGF2R allelic loss benefit most from concurrent chemotherapy.
Similar content being viewed by others
Background
Squamous cell carcinoma of the head and neck is diagnosed in over 40,000 Americans each year, resulting in over 12,000 annual deaths [1]. Carcinomas of the head and neck are often associated with multiple areas of dysplasia or carcinoma in situ (CIS) in noncontiguous mucosa, as well as with the development of second primary cancers of the aerodigestive tract. The concept of "field cancerization" hypothesizes that regions of the mucosal epithelium, although normal in appearance, are "preconditioned" by chronic exposure to carcinogenic agents, thus priming them for the subsequent development of invasive lesions [2].
The use of modern molecular biological techniques has supported and greatly expanded our understanding of the "cancer field effect". Analysis of X-chromosome inactivation in female patients with multiple head and neck cancers shows that distinct tumors arise from regional clonal growths of phenotypically normal, mutated preneoplastic cells [3–5], a phenomenon similar to that also observed in liver cancer patients with cirrhosis [6]. Long-term smoking and alcohol abuse are strongly associated with these clonal growths in the upper aerodigestive tract (reviewed in [7]).
Frequent allelic loss at chromosomal locations 2q, 3p, 4q, 6p, 6q, 8p, 8q, 9p, 11q, 13q, 14q and 17q is observed in head and neck cancer [4, 8–11]. Molecular studies of hyperplastic, dysplastic, CIS, and invasive head and neck lesions indicate that loss of heterozygosity at chromosomal locations 3p, 9p and 17p are early events in head and neck carcinogenesis [4, 12]. Specific tumor suppressor genes, such as FHIT (3p14.2) p16 (9p21), p53 (17p13.1) and RB1 (13q14.2) have also been shown to be mutated in head and neck cancer [4, 13]. Nevertheless, the large number of additional chromosomal regions with high frequencies of allelic loss in head and neck cancer strongly suggests that many suppressor genes still remain to be identified.
The mannose 6-phosphate/insulin-like growth factor 2 receptor (M6P/IGF2R) maps to chromosome location 6q25-27 [14]; a chromosomal region predicted to contain a head and neck tumor suppressor gene [10, 11]. It encodes for a receptor that functions in intracellular lysosomal enzyme trafficking, transforming growth factor beta activation, and IGF2 degradation (reviewed in [15, 16]). Granzyme B internalization by the M6P/IGF2R is also required for cytotoxic T cells to induce apoptosis in cells targeted for death, resulting in this receptor being referred to as a "death receptor" [17]. Elevated IGF2 levels during murine development arising from M6P/IGF2R deficiency result in cardiac abnormalities, cleft palate, fetal overgrowth and perinatal lethality [15, 18]. Furthermore, large offspring syndrome frequently observed in cloned animals is associated with epigenetic changes in gene regulation and decreased M6P/IGF2R expression [19]. Thus, the M6P/IGF2R plays a crucial role in regulating mammalian fetal growth and development.
The M6P/IGF2R is also mechanistically involved in the genesis of human cancer [6, 20–24]. M6P/IGF2R loss of heterozygosity coupled with intragenic loss-of-function mutations in the remaining allele is a common event in human cancers [6, 20–22]. Inheritance of a tandem repeat polymorphism in the 3' UTR of M6P/IGF2R furthermore predicts for enhanced susceptibility to oral cancer [25]. Moreover, tumor cell growth is inhibited when M6P/IGF2R expression is restored to normal while it is increased when gene expression is reduced [26–29]. The results of these mutational and functional studies clearly demonstrate that the M6P/IGF2R possesses the characteristics necessary to be classified as a tumor suppressor gene [30].
We tested in this investigation the hypothesis that M6P/IGF2R loss of heterozygosity in locally advanced, non-metastatic squamous cell carcinomas of the head and neck is associated with poorer patient prognosis. The patients used in this study were enrolled in a randomized trial of twice daily radiotherapy with or without concurrent chemotherapy [31]. We report herein that M6P/IGF2R loss of heterozygosity occurs frequently in head and neck cancer, and that it predicts for poor therapeutic outcome.
Methods
Patient Population and Treatment
Patients with locally advanced but non-metastatic squamous carcinoma of the head and neck who participated in or who met eligibility criteria but declined enrollment in a phase 3 trial of hyperfractionated irradiation with or without concurrent chemotherapy constituted the study population. Details of their treatment and outcome have been published previously [31]. Briefly, patients receiving radiation therapy alone were given a continuous course of 125 cGy twice daily to a total dose of 75 Gy. Patients assigned to combined modality treatment received 70 Gy via a split-course of 125 cGy twice daily. They also received two cycles of cisplatin and 5-fluorouracil during the first and sixth weeks of irradiation. All protocols were approved by the Duke University Medical Center Institutional Review Board.
Tissue Microdissection and M6P/IGF2RLoss of Heterozygosity Analysis
Microdissection of malignant and surrounding normal non-mucosal tissue was performed as previously described [6, 20, 21]; tumor histology was confirmed by a pathologist (R.T. Volmer). Paraffin-embedded sections (10 μm in thickness) were microdissected following deparaffinization, and the tissue was then digested by proteinase K in tris-EDTA buffer at 55°C for 4 hr. Six different gene-specific polymorphisms were used to assess head and neck tumors for M6P/IGF2R loss of heterozygosity [32, 33].
A tetranucleotide (ACAA) insertion/deletion polymorphism in the 3'-UTR of the M6P/IGF2R [34] was detected with 2 rounds of nested polymerase chain reaction (PCR). The forward and reverse first round PCR primers were KK*ACAA*F1: 5'-GGAGAGTTTGCCTGTTCTATGCC-3' and KK*ACAA*R: 5'-CAAATCAATCTTTGGGC AGG-3', respectively. The forward and reverse second round PCR primers were KK*ACAA*F2: 5'-AGTCAGGAATGGCTGCACC-3'and KK*ACAA*R: 5'-CAAATCAATC TTTGGGCAGG-3', respectively; the KK*ACAA*F2 primer was end-radiolabeled with 33P-dATP prior to PCR. Each round of PCR consisted of 31 cycles at 94°C for 20 seconds, 55°C for 40 seconds, and 72°C for 45 seconds; Platinum® Taq DNA polymerase (GibcoBRL, Baltimore, MD) was used for DNA amplification. The PCR product (5 μl) containing the 3'-UTR (ACAA) insertion/deletion polymorphism was mixed with 5 μl of formamide-based stop buffer, heated to 95°C for 10 min, placed on ice, electrophoresed on a 6% acrylamide gel, and then exposed to film.
Five identified single nucleotide polymorphisms, c. 901C>G (exon 6), c. 1197A>G (exon 9), c. 1737A>G (exon 12), c. 2286A>G (exon 16), and c. 5002A>G (exon 34), were also analyzed following 2 rounds of nested PCR; the exon specific forward and reverse primers have been previously described [32, 33]. The exons containing these polymorphisms were PCR amplified from genomic DNA using PCR conditions identical to those described above. The single nucleotide polymorphisms used to determine M6P/IGF2R loss of heterozygosity were assessed by direct sequencing of PCR products according to the manufacturer's protocol (Thermo Sequenase, USB Corporation, Cleveland, OH) (Figure 1). M6P/IGF2R loss of heterozygosity frequency is independent of the polymorphism used for its estimation (p = 0.3).
M6P/IGF2R loss of heterozygosity in human head and neck cancer. A single nucleotide polymorphism (c. 1197A>G transition) in exon 9 of the M6P/IGF2R was used to determine loss of heterozygosity in these representative samples [32, 33]. (A) Informative head and neck cancer without M6P/IGF2R loss of heterozygosity (i.e. both A and G polymorphisms expressed in tumor). (B) Informative head and neck cancer with M6P/IGF2R loss of heterozygosity (i.e. only G polymorphism expressed in tumor). (C) Non-informative head and neck cancer. Arrow, location of A>G polymorphism; arrowhead, A allele absent.
Taq DNA polymerase can introduce sequence errors during PCR amplification, and unequal amplification of the two alleles can result in false positive detection of loss of heterozygosity. Thus, both the normal and tumor DNA templates were amplified in three independent PCR reactions, and assessed for tumor M6P/IGF2R loss of heterozygosity. Due to the potential of contaminating the tumor tissue sample with normal stroma, allele loss in informative patients was defined as a >50% decrease in the ratio of the polymorphic band intensities in the tumor tissue versus that in the surrounding normal stromal tissue; this was quantified using a densitometer.
Statistical Analysis
Relapse-free survival represented the primary clinical endpoint. Locoregional control was evaluated as a secondary endpoint since the vast majority of head and neck cancers recur either locally at the primary site or regionally in the neck; cause specific survival was also assessed. All curves were computed using the Kaplan-Meier method starting from the time of study entry. Curves for different subgroups were compared by the Cox-Mantel test. A chi-squared test was used to compare the clinical characteristics between M6P/IGF2R informative and excluded patients and informative patients with and without M6P/IGF2R loss of heterozygosity. A p-value < 0.05 was considered to be statistically significant.
Results
M6P/IGF2RLoss of Heterozygosity Analysis
The study population consisted of 116 patients enrolled in a phase III randomized clinical trial comparing radiation alone versus radiation plus concurrent chemotherapy for advanced head and neck cancer [31] plus an additional 23 patients who met all the entrance criteria but declined enrollment. A total of 52 tumors could not used in this investigation because either the tissue slides were unavailable or the DNA could not be PCR amplified. Of the remaining 87 patients, 56 (64%) were informative (i.e. polymorphic), and the tumors in 54% (30/56) of these patients had M6P/IGF2R loss of heterozygosity (Figure 1). The M6P/IGF2R informative patients and those not used in this study were insignificantly different from each other for the clinical characteristics of gender, age, race, smoking history, baseline hemoglobin, Karnofsky performance status, tumor resectability, treatment, tumor stage, nodal stage, overall staging and site of primary tumor (Table 1).
Clinical Outcome
The median follow-up for surviving patients enrolled on this trial [31] is now 76 months (range: 2 to 128 months). M6P/IGF2R loss of heterozygosity was associated with significant reductions in 5 year relapse-free survival {37% (95% CI: 20% to 54%) vs. 65% (95% CI: 46% to 84%); p = 0.05}, locoregional control {46% (95% CI: 28% to 64%) vs. 76% (95% CI: 58% to 94%); p = 0.03} and a non-significant reduction in cause-specific survival {43% (95% CI: 25% to 61%) vs. 69% (95% CI: 49% to 89%); p = 0.1}.
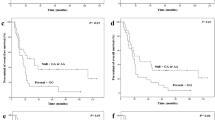
Since the clinical trial demonstrated a significant benefit for patients receiving radiotherapy and concurrent chemotherapy [31], outcome was also analyzed according to whether or not patients received chemotherapy (Figures 2,3,4). Patients in the radiotherapy (RT), loss of heterozygosity (LOH) group had significantly lower 5 year relapse-free survival {23% (95% CI: 2% to 44%) vs. 69% (95% CI: 46% to 92%); p = 0.02} (Figure 2), locoregional control {34% (95% CI: 11% to 57%) vs. 75% (95% CI: 54% to 98%); p = 0.03} (Figure 3) and cause specific survival {29% (95% CI: 5% to 53%) vs. 75% (95% CI: 54% to 96%); p = 0.02} (Figure 4) than those in the RT, non LOH group. These results indicate that M6P/IGF2R allelic loss results in poor patient outcome when RT alone is employed since all other measured clinical characteristics of the head and neck cancer patients were comparable to those in patients with a non-mutated M6P/IGF2R tumor suppressor gene (Table 1).
Kaplan-Meier estimates of relapse-free survival in patients with head and neck cancer. Tumors treated with radiotherapy alone (solid lines) were either mutated (RT, LOH) or unmutated (RT, non LOH) at the M6P/IGF2R locus. Tumors treated with combined modality therapy (dashed lines) were also either mutated (CM, LOH) or unmutated (CM, non LOH) at the M6P/IGF2R locus. Patient number (n), patients that failed (parentheses), censored patients (angled bars), and median follow-up times are provided for each patient group. RT, radiotherapy; CM, combined modality therapy; LOH, loss of heterozygosity.
Kaplan-Meier estimates of locoregional control in patients with head and neck cancer. Tumors treated with radiotherapy alone (solid lines) were either mutated (RT, LOH) or unmutated (RT, non LOH) at the M6P/IGF2R locus. Tumors treated with combined modality therapy (dashed lines) were also either mutated (CM, LOH) or unmutated (CM, non LOH) at the M6P/IGF2R locus. Patient number (n), patients that failed (parentheses), censored patients (angled bars), and median follow-up times are provided for each patient group. RT, radiotherapy; CM, combined modality therapy; LOH, loss of heterozygosity.
Kaplan-Meier estimates of cause specific survival in patients with head and neck cancer. Tumors treated with radiotherapy alone (solid lines) were either mutated (RT, LOH) or unmutated (RT, non LOH) at the M6P/IGF2R locus. Tumors treated with combined modality therapy (dashed lines) were also either mutated (CM, LOH) or unmutated (CM, non LOH) at the M6P/IGF2R locus. Patient number (n), patients that failed (parentheses), censored patients (angled bars), and median follow-up times are provided for each patient group. RT, radiotherapy; CM, combined modality therapy; LOH, loss of heterozygosity.
Patients in the RT, LOH group also fared worse than those in the combined modality (CM), LOH group, although the differences were not statistically significant in these smaller subgroups: 5 year relapse-free survival {23% (95% CI: 2% to 44%) vs. 54% (95% CI: 26% to 82%); p = 0.18}, locoregional control {34% (95% CI: 11% to 57%) vs. 61% (95% CI: 34% to 88%); p = 0.25} and cause specific survival {29% (95% CI: 5% to 53%) vs. 59% (95% CI: 30% to 88%); p = 0.12}. Patients in the CM, LOH group had 5 year relapse-free survival, locoregional control and cause specific survival that were statistically indistinguishable from those in the CM, non LOH group (p > 0.2). Combined modality therapy also did not provide any significant benefit over radiation alone for patients with a non-mutated tumor M6P/IGF2R (p > 0.2). Thus, patients with a non-mutated M6P/IGF2R who received RT alone had the same long-term outcome as the overall population of patients who received RT and concurrent chemotherapy [31]. This implies that M6P/IGF2R allelic loss may help to identify a group of head and neck cancer patients who can be adequately treated with RT alone without exposure to the added morbidity of combined modality therapy.
The development of second primaries was independent of the M6P/IGF2R mutation status in the primary tumor (p = 0.8). Three of the 30 (10%) patients with M6P/IGF2R loss of heterozygosity and two of the 26 (8%) patients without loss of heterozygosity at this locus developed second primaries.
Discussion
M6P/IGF2R loss of heterozygosity occurs frequently in human breast, liver and lung cancer [6, 20–22], and the remaining allele of 30 to 50% of these tumors contains an intragenic loss-of-function point mutation in the ligand binding domains [35]. The M6P/IGF2R is also commonly mutated in gastrointestinal and endometrial malignancies because its coding sequence contains a poly-G region that is a mutational target in tumors with mismatch repair deficiencies and microsatellite instability [23, 24]. Functional studies show that the introduction of an exogenous wild-type M6P/IGF2R into human colorectal cancer cells with a single inactivated allele significantly decreases growth rate and enhances apoptosis [26]. Conversely, loss of M6P/IGF2R expression promotes cancer cell growth by increasing intracellular signaling from both the insulin-like growth factor I receptor and the insulin receptors [36].
We demonstrate herein that loss of heterozygosity at the M6P/IGF2R locus in head and neck cancer is also associated with poor patient prognosis. Loss of heterozygosity in cancer can occur either because of chromosomal deletion or somatic recombination resulting in uniparental disomy [37]. Comparative genomic hybridization studies in head and neck cancer [10, 38] demonstrate that 6q deletion frequency (> 50%) is similar to that which we observed at the M6P/IGF2R locus. This provides evidence that M6P/IGF2R loss of heterozygosity in head and neck cancer is due primarily to either gene deletion or chromosomal loss rather than somatic recombination.
Since chromosomal deletion can affect more than one gene, M6P/IGF2R loss of heterozygosity alone does not rule out the possibility that other adjacent genes also have a tumor suppressor function in head and neck cancer. However, our previous finding, that both alleles of the M6P/IGF2R are mutated in greater than 50% of squamous cell carcinomas of the lung [22], supports our postulate that the M6P/IGF2R is a key head and neck cancer tumor suppressor gene at chromosome location 6q.
The clinical trial from which the tumor specimens used in this study were derived showed improvements in relapse-free survival, locoregional control, and overall survival for those patients randomized to combined modality therapy [31]. This investigation established that patients whose tumors had M6P/IGF2R loss of heterozygosity and were treated with radiotherapy alone had a significantly worse prognosis than their counterparts with a non-mutated allele. Conversely, patients with an intact M6P/IGF2R had a similar prognosis whether they received radiotherapy alone or combined modality treatment. Thus, our findings suggest that head and neck cancer patients with tumor M6P/IGF2R loss of heterozygosity would benefit most from combined modality treatment.
The mechanism by which M6P/IGF2R allelic loss in head and neck tumors increases the effectiveness of adjuvant chemotherapy is presently unknown, but it is clearly of clinical importance. A primary function of this receptor in placental mammals involves the degradation of extracellular IGF2. M6P/IGF2R allelic loss would therefore result in enhanced cellular bioavailability of this potent growth factor, thereby potentially increasing both cell proliferation and resistance to apoptosis [29]. The M6P/IGF2R also facilitates the activation of TGFβ, a potent cell growth inhibitor that is secreted in an inactive form (reviewed in [15, 16]). M6P/IGF2R mutation is therefore one mechanism by which cancer cells can become refractory to TGFβ's mitoinhibitory effect.
We have previously shown that M6P/IGF2R mutation in squamous cell carcinoma of the lung is highly correlated with increased TGFβ concentrations in both the tumor and patient plasma [39]. Elevated TGFβ in the latter stages of tumor progression directly contributes to enhanced tumor angiogenesis, metastasis formation and a decreased host immune response (reviewed in [40]). Together these findings predict that tumors with a mutated M6P/IGF2R would be more resistant to therapy than those with an intact receptor. Moreover, if some chemotherapeutic agents are not only directly cytotoxic to cancer cells, but also reduce tumor production of growth factors, such as IGF2 and TGFβ, adjuvant chemotherapy would be more useful in treating tumors with a mutated M6P/IGF2R, as observed in this study.
M6P/IGF2R is normally imprinted in mice with only the maternal copy of the gene being expressed [41]. In contrast, both copies of the M6P/IGF2R are expressed in humans because genomic imprinting at this locus was lost in the primate lineage approximately 75 million years ago [42]. Importantly, restoration of biallelic M6P/IGF2R expression in mice results in a marked reduction in offspring weight late in embryonic development that persists into adulthood [43]. This demonstrates that M6P/IGF2R allelic loss or haploid insufficiency markedly enhances cell proliferation and/or survival during fetal development. Therefore, mutation of even a single allele of the M6P/IGF2R in human somatic cells is predicted to also promote cell growth.
Haploid insufficiency for tumor suppressor genes, such as Nf2, p27 Kip1, p53, Ptch, Pten and TGFβ, is known to promote tumor formation (reviewed in [44, 45]). Yamada et al. [6] demonstrated that in patients chronically infected with hepatitis B and/or hepatitis C viruses, the M6P/IGF2R is mutated not only in hepatocellular carcinomas (HCCs), but also in the phenotypically normal hepatocytes adjacent to these tumors. Interestingly, only one M6P/IGF2R allele is inactivated in the adjacent cirrhotic tissue even when both alleles are mutated in the HCC. These findings are consistent with normal appearing, preneoplastic hepatocytes forming clonal masses in the liver because M6P/IGF2R haploid insufficiency affords them with a selective growth and/or survival advantage relative to normal hepatocytes [46].
The liver is not the only organ in which regions of normal appearing tissue have a clonal origin. Entire lobules and large ducts of normal breast tissue can be derived from a single progenitor cell [47], and LOH at various chromosomal locations is frequently detectable in morphologically normal lobules adjacent to breast tumors [48]. Lung tumors and head and neck tumors that develop in a localized region also often have a common clonal origin [3, 4, 49]. The high frequency of M6P/IGF2R loss of heterozygosity observed in the head and neck tumors in this study suggests that the phenomenon of "field cancerization", first described by Slaughter and his colleagues [2] in 1953, may in part result from the clonal proliferation of mucosal epithelial cells with M6P/IGF2R allelic loss.
Conclusions
The observations in this study raise the intriguing possibility that selection of head and neck cancer patients for concurrent chemotherapy can be based upon the intratumoral mutational status of M6P/IGF2R. Furthermore, since M6P/IGF2R loss of heterozygosity in squamous cell carcinomas is highly correlated with an elevated plasma TGFβ level [39], patient prognosis may potentially be assessed by a simple blood test. This would be desirable since the morbidity of combined modality therapy is greater than that of radiotherapy alone [50, 51].
Abbreviations
- CIS:
-
carcinoma in situ
- HCC:
-
hepatocellular carcinoma
- IGF2:
-
insulin-like growth factor 2
- LOH:
-
loss of heterozygosity
- M6P/IGF2R:
-
mannose 6-phosphate/insulin-like growth factor 2 receptor
- PCR:
-
polymerase chain reaction
- SNP:
-
single nucleotide polymorphism
- TGFβ:
-
transforming growth factor beta
- UTR:
-
untranslated region.
References
Parker SL, Tong T, Bolden S, Wingo PA: Cancer statistics, 1996. CA Cancer J Clin. 1996, 46: 5-27.
Slaughter DP, Southwick HW, Smejkal W: "Field cancerization" in oral stratified squamous epithelium. Cancer. 1953, 6: 963-968.
Bedi GC, Westra WH, Gabrielson E, Koch W, Sidransky D: Multiple head and neck tumors: evidence for a common clonal origin. Cancer Res. 1996, 56: 2484-2487.
Califano J, van der Riet P, Westra W, Nawroz H, Clayman G, Piantadosi S, Corio R, Lee D, Greenberg B, Koch W, et al: Genetic progression model for head and neck cancer: implications for field cancerization. Cancer Res. 1996, 56: 2488-2492.
Tabor MP, Brakenhoff RH, van Houten VM, Kummer JA, Snel MH, Snijders PJ, Snow GB, Leemans CR, Braakhuis BJ: Persistence of genetically altered fields in head and neck cancer patients: biological and clinical implications. Clin Cancer Res. 2001, 7: 1523-1532.
Yamada T, De Souza AT, Finkelstein S, Jirtle RL: Loss of the gene encoding mannose 6-phosphate/insulin-like growth factor II receptor is an early event in liver carcinogenesis. Proc Natl Acad Sci USA. 1997, 94: 10351-10355. 10.1073/pnas.94.19.10351.
van Oijen MG, Slootweg PJ: Oral field cancerization: carcinogen-induced independent events or micrometastatic deposits?. Cancer Epidemiol Biomarkers Prev. 2000, 9: 249-256.
Nawroz H, van der Riet P, Hruban RH, Koch W, Ruppert JM, Sidransky D: Allelotype of head and neck squamous cell carcinoma. Cancer Res. 1994, 54: 1152-1155.
Field JK: Genomic instability in squamous cell carcinoma of the head and neck. Anticancer Res. 1996, 16: 2421-2431.
Bockmuhl U, Wolf G, Schmidt S, Schwendel A, Jahnke V, Dietel M, Petersen I: Genomic alterations associated with malignancy in head and neck cancer. Head Neck. 1998, 20: 145-151. 10.1002/(SICI)1097-0347(199803)20:2<145::AID-HED8>3.0.CO;2-2.
Pack SD, Karkera JD, Zhuang Z, Pak ED, Balan KV, Hwu P, Park WS, Pham T, Ault DO, Glaser M, et al: Molecular cytogenetic fingerprinting of esophageal squamous cell carcinoma by comparative genomic hybridization reveals a consistent pattern of chromosomal alterations. Genes Chromosomes Cancer. 1999, 25: 160-168. 10.1002/(SICI)1098-2264(199906)25:2<160::AID-GCC12>3.0.CO;2-U.
Waber P, Dlugosz S, Cheng QC, Truelson J, Nisen PD: Genetic alterations of chromosome band 9p21-22 in head and neck cancer are not restricted to p16INK4a. Oncogene. 1997, 15: 1699-1704. 10.1038/sj.onc.1201336.
Virgilio L, Shuster M, Gollin SM, Veronese ML, Ohta M, Huebner K, Croce CM: FHIT gene alterations in head and neck squamous cell carcinomas. Proc Natl Acad Sci U S A. 1996, 93: 9770-9775. 10.1073/pnas.93.18.9770.
Laureys G, Barton DE, Ullrich A, Francke U: Chromosomal mapping of the gene for the type II insulin-like growth factor receptor/cation-independent mannose 6-phosphate receptor in man and mouse. Genomics. 1988, 3: 224-229.
Jirtle RL: Mannose 6-phosphate receptors. In: Encyclopedia of Molecular Biology. Edited by: Creidton TE. 1999, New York: Wiley-Liss, Inc, 1441-1447.
Dahms NM, Hancock MK: P-type lectins. Biochim Biophys Acta. 2002, 1572: 317-340. 10.1016/S0304-4165(02)00317-3.
Motyka B, Korbutt G, Pinkoski MJ, Heibein JA, Caputo A, Hobman M, Barry M, Shostak I, Sawchuk T, Holmes CF, et al: Mannose 6-phosphate/insulin-like growth factor II receptor is a death receptor for granzyme B during cytotoxic T cell-induced apoptosis. Cell. 2000, 103: 491-500.
Filson AJ, Louvi A, Efstratiadis A, Robertson EJ: Rescue of the T-associated maternal effect in mice carrying null mutations in Igf-2 and Igf2r, two reciprocally imprinted genes. Development. 1993, 118: 731-736.
Young LE, Fernandes K, McEvoy TG, Butterwith SC, Gutierrez CG, Carolan C, Broadbent PJ, Robinson JJ, Wilmut I, Sinclair KD: Epigenetic change in IGF2R is associated with fetal overgrowth after sheep embryo culture. Nat Genet. 2001, 27: 153-154. 10.1038/84769.
De Souza AT, Hankins GR, Washington MK, Orton TC, Jirtle RL: M6P/IGF2R gene is mutated in human hepatocellular carcinomas with loss of heterozygosity. Nat Genet. 1995, 11: 447-449.
Hankins GR, De Souza AT, Bentley RC, Patel MR, Marks JR, Iglehart JD, Jirtle RL: M6P/IGF2 receptor: a candidate breast tumor suppressor gene. Oncogene. 1996, 12: 2003-2009.
Kong FM, Anscher MS, Washington MK, Killian JK, Jirtle RL: M6P/IGF2R is mutated in squamous cell carcinoma of the lung. Oncogene. 2000, 19: 1572-1578. 10.1038/sj.onc.1203437.
Ouyang H, Shiwaku HO, Hagiwara H, Miura K, Abe T, Kato Y, Ohtani H, Shiiba K, Souza RF, Meltzer SJ, et al: The insulin-like growth factor II receptor gene is mutated in genetically unstable cancers of the endometrium, stomach, and colorectum. Cancer Res. 1997, 57: 1851-1854.
Souza RF, Appel R, Yin J, Wang S, Smolinski KN, Abraham JM, Zou T-T, Shi Y-Q, Lei J, Cottrell J, et al: The insulin-like growth factor II receptor gene is a target of microsatellite instability in human gastrointestinal tumours. Nat Genet. 1996, 14: 255-257.
Zavras AI, Pitiphat W, Wu T, Cartsos V, Lam A, Douglass CW, Diehl SR: Insulin-like growth factor II receptor gene-167 genotype increases the risk of oral squamous cell carcinoma in humans. Cancer Res. 2003, 63: 296-297.
Souza RF, Wang S, Thakar M, Smolinski KN, Yin J, Zou TT, Kong D, Abraham JM, Toretsky JA, Meltzer SJ: Expression of the wild-type insulin-like growth factor II receptor gene suppresses growth and causes death in colorectal carcinoma cells. Oncogene. 1999, 18: 4063-4068. 10.1038/sj.onc.1202768.
Kang JX, Bell J, Beard RL, Chandraratna RA: Mannose 6-phosphate/insulin-like growth factor II receptor mediates the growth-inhibitory effects of retinoids. Cell Growth Differ. 1999, 10: 591-600.
O'Gorman DB, Costello M, Weiss J, Firth SM, Scott CD: Decreased insulin-like growth factor-II/mannose 6-phosphate receptor expression enhances tumorigenicity in JEG-3 cells. Cancer Res. 1999, 59: 5692-5694.
Chen Z, Ge Y, Landman N, Kang JX: Decreased expression of the mannose 6-phosphate/insulin-like growth factor-II receptor promotes growth of human breast cancer cells. BMC Cancer. 2002, 2: 18-10.1186/1471-2407-2-18.
Clurman B, Groudine M: Tumour-suppressor genes. Killer in search of a motive?. Nature. 1997, 389: 122-123. 10.1038/38116.
Brizel DM, Albers ME, Fisher SR, Scher RL, Richtsmeier WJ, Hars V, George SL, Huang AT, Prosnitz LR: Hyperfractionated irradiation with or without concurrent chemotherapy for locally advanced head and neck cancer. N Engl J Med. 1998, 338: 1798-1804. 10.1056/NEJM199806183382503.
Killian JK, Oka Y, Jang H-S, Fu X, Sohda T, Sakaguchi S, Jirtle RL: Mannose 6-phosphate/insulin-like growth factor 2 receptor (M6P/IGF2R) variants in American and Japanese populations. Hum Mutat. 2001, 18: 25-31. 10.1002/humu.1146.
Oka Y, Waterland RA, Killian JK, Nolan CM, Jang HS, Tohara K, Sakaguchi S, Yao T, Iwashita A, Yata Y, et al: M6P/IGF2R tumor suppressor gene mutated in hepatocellular carcinomas in Japan. Hepatology. 2002, 35: 1153-1163. 10.1053/jhep.2002.32669.
Hol FA, Geurds MP, Hamel BC, Mariman EC: Improving the polymorphism content of the 3' UTR of the human IGF2R gene. Hum Mol Genet. 1992, 1: 347-
Byrd JC, Devi GR, de Souza AT, Jirtle RL, MacDonald RG: Disruption of ligand binding to the insulin-like growth factor II/mannose 6-phosphate receptor by cancer-associated missense mutations. J Biol Chem. 1999, 274: 24408-24416. 10.1074/jbc.274.34.24408.
Osipo C, Dorman S, Frankfater A: Loss of insulin-like growth factor II receptor expression promotes growth in cancer by increasing intracellular signaling from both IGF-I and insulin receptors. Exp Cell Res. 2001, 264: 388-396. 10.1006/excr.2000.5121.
Robinson WP: Mechanisms leading to uniparental disomy and their clinical consequences. Bioessays. 2000, 22: 452-459. 10.1002/(SICI)1521-1878(200005)22:5<452::AID-BIES7>3.0.CO;2-K.
Bockmuhl U, Schwendel A, Dietel M, Petersen I: Distinct patterns of chromosomal alterations in high- and low-grade head and neck squamous cell carcinomas. Cancer Res. 1996, 56: 5325-5329.
Kong FM, Anscher MS, Sporn TA, Washington MK, Clough R, Barcellos-Hoff MH, Jirtle RL: Loss of heterozygosity at the mannose 6-phosphate insulin-like growth factor 2 receptor (M6P/IGF2R) locus predisposes patients to radiation-induced lung injury. Int J Radiat Oncol Biol Phys. 2001, 49: 35-41. 10.1016/S0360-3016(00)01377-8.
Pasche B: Role of transforming growth factor beta in cancer. J Cell Physiol. 2001, 186: 153-168. 10.1002/1097-4652(200002)186:2<153::AID-JCP1016>3.0.CO;2-J.
Barlow DP, Stöger R, Herrmann BG, Saito K, Schweifer N: The mouse insulin-like growth factor type-2 receptor is imprinted and closely linked to the Tme locus. Nature. 1991, 349: 84-87. 10.1038/349084a0.
Killian JK, Tao Li T, Nolan CM, Thanh Vu TH, Hoffman AR, Jirtle RL: Divergent evolution in M6P/IGF2R imprinting from the Jurasic to the Quaternary. Hum Mol Genet. 2001, 10: 1721-1728. 10.1093/hmg/10.17.1721.
Wutz A, Theussl HC, Dausman J, Jaenisch R, Barlow DP, Wagner EF: Non-imprinted Igf2r expression decreases growth and rescues the Tme mutation in mice. Development. 2001, 128: 1881-1887.
Islam MQ, Islam K: A new functional classification of tumor-suppressing genes and its therapeutic implications. Bioessays. 2000, 22: 274-285. 10.1002/(SICI)1521-1878(200003)22:3<274::AID-BIES9>3.0.CO;2-G.
Quon KC, Berns A: Haplo-insufficiency? Let me count the ways. Genes Dev. 2001, 15: 2917-2921. 10.1101/gad.949001.
Jirtle RL: Genomic imprinting and cancer. Exp Cell Res. 1999, 248: 18-24. 10.1006/excr.1999.4453.
Tsai YC, Lu Y, Nichols PW, Zlotnikov G, Jones PA, Smith HS: Contiguous patches of normal human mammary epithelium derived from a single stem cell: implications for breast cancer. Cancer Res. 1996, 56: 402-404.
Deng G, Lu Y, Zlotnikov G, Thor AD, Smith HS: Loss of heterozygosity in normal tissue adjacent to breast carcinomas. Science. 1996, 274: 2057-2059. 10.1126/science.274.5295.2057.
Wistuba II, Lam S, Behrens C, Virmani AK, Fong KM, LeRiche J, Samet JM, Srivastava S, Minna JD, Gazdar AF: Molecular damage in the bronchial epithelium of current and former smokers. J Natl Cancer Inst. 1997, 89: 1366-1373. 10.1093/jnci/89.18.1366.
Wendt TG, Grabenbauer GG, Rodel CM, Thiel HJ, Aydin H, Rohloff R, Wustrow TP, Iro H, Popella C, Schalhorn A: Simultaneous radiochemotherapy versus radiotherapy alone in advanced head and neck cancer: a randomized multicenter study. J Clin Oncol. 1998, 16: 1318-1324.
Calais G, Alfonsi M, Bardet E, Sire C, Germain T, Bergerot P, Rhein B, Tortochaux J, Oudinot P, Bertrand P: Randomized trial of radiation therapy versus concomitant chemotherapy and radiation therapy for advanced-stage oropharynx carcinoma. J Natl Cancer Inst. 1999, 91: 2081-2086. 10.1093/jnci/91.24.2081.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2407/3/4/prepub
Acknowledgements
This study was supported in part by NIH grants CA25951 and ES08823. For additional information on the M6P/IGF2R or genomic imprinting, visit the following website: http://www.geneimprint.com.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
None declared.
Authors' Contributions
TAJ conceived of the study, performed LOH determinations and drafted the manuscript. DMB provided patient samples and assisted in editing of manuscript. JKK, YO, H-SJ and XF identified M6P/IGF2R SNPs and performed LOH determinations. RTV confirmed tumor histology while RWC performed statistical analysis of the data. MSA assisted in experimental design and editing of manuscript. RLJ conceived of the study, participated in its design and coordination, and assisted in editing of manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Jamieson, T.A., Brizel, D.M., Killian, J.K. et al. M6P/IGF2Rloss of heterozygosity in head and neck cancer associated with poor patient prognosis. BMC Cancer 3, 4 (2003). https://doi.org/10.1186/1471-2407-3-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2407-3-4