Abstract
Background
Quickly and accurately localizing small peripheral pulmonary lesions can avoid prolonged operative time and unplanned open thoracotomy. In this study, we aimed to introduce and evaluate a new technique combining virtual simulation and methylene blue staining for the localization of small peripheral pulmonary lesions.
Methods
Seventy four (74) patients with 80 peripheral pulmonary lesions <20 mm in size on computer tomography (CT) were virtually punctured using a radiotherapy planning simulator on the day before operation. Under general anaesthesia, methylene blue dye was injected to the virtually identified point according to the surface point, angle and depth previously determined by the simulator. The wedge resection of the marked lesion was performed under video-assisted thoracoscopic surgery (VATS) and the specimens were sent for immediate pathologic examination. According to pathology results, appropriate surgical procedures were decided and undertaken.
Results
The average lesion size was 10.4±3.5 mm (range: 4-17 mm) and the average distance to the pleural surface was 9.4±4.9 mm. Our preoperative localization procedure was successful in 75 of 80 (94%) lesions. Histological examination showed 28 benign lesions and 52 lung cancers. The shortest distance between the edges of the stain and lesion was 5.1±3.1 mm. Localization time was 17.4±2.3 min. All patients with malignant lesions subsequently underwent lobectomy and systematic lymph node dissection. No complications were observed in all participants.
Conclusions
The novel technique combining the preoperative virtual simulation and methylene blue staining techniques has a high success rate for localizing small peripheral pulmonary lesions, particularly for those tiny lesions which are difficult to visualise and palpate during VATS.
Similar content being viewed by others
Background
In recent years, the widespread utilization of CT scanning and the increasing awareness of health screening have resulted in identification of a large number of small pulmonary lesions. It has been reported that a large number, about 59% to 73%, of those lesions with a localized area of ground glass opacity nodules are early stage cancers [1] while some lesions are benign. Generally, the wedge resection of the nodule is performed first for pathologic examination, and further treatment planning for small peripheral pulmonary nodules will depend on pathologic findings to prevent unwanted thoracotomy. However, the challenge that we often face during the surgery is to quickly and accurately localize those small nodules, particularly those tiny nodules which are difficult to be quickly palpated. Inadequate nodule localization might lead to a prolonged operative time and even conversion to an unplanned open thoracotomy [2, 3]. Therefore, several preoperative localization techniques have been introduced as a method of improving the success rate of video-assisted thoracoscopic surgery (VATS) [4–9]. Each technique has its strengths and limitations. In this study, we introduce a novel technique which applies the virtual simulation, a technique for radiotherapy planning [10, 11], in combination with methylene blue staining for the localization of small peripheral pulmonary nodules. In this study, we describe this procedure and assess the performance of this technique in 80 small peripheral pulmonary lesions from 74 Chinese patients.
Methods
Participants
From February 2012 to February 2013, 74 participants aged from 29 to 81 years were recruited from Shanghai Chest Hospital for medical check-ups. All participants met the following criteria. First, they underwent chest CT scanning with an identified peripheral pulmonary lesion <20 mm in diameter in the outer third of the lung field. Those lesions were not directly visible on the lung surface. Second, those lesions had not been pathologically examined before this study so that the diagnosis of the lesions was unknown. Third, no other overt abnormalities were detected in blood routine, blood glucose, electrolyte and ECG results. They had normal lung, liver, kidney and blood coagulation functions. Abdominal ultrasound, brain MRI, and whole body bone scan showed no signs of metastases in those patients. Participants with at least one of the following were excluded: 1) lesions >20 mm which could be easily localized, 2) lesions located in the middle and inner two thirds of the lung field where the wedge resection was not feasible, 3) lesions close to the pleural surface with visible pleural retraction, 4) impossible to inject methylene blue dye because the identified lesions were blocked by a large skeletal structure such as scapula according to CT scanning results, and 5) lesions close to heart, large blood vessels, diaphragm and major nerves with a high risk of injuring them. Among 74 participants recruited, 80 lesions were identified. As the probability of finding malignancy among the participants with lesions was high, all eligible participants with lesions went through the proposed localization procedure. This project was approved by the Ethics Review Committee of Shanghai Chest Hospital and informed consent was obtained from all participants, including consent for participation, and consent to publish findings and to use anonymous images in medical publications.
Virtual simulation ─ methylene blue staining technique
The virtual simulation ─ methylene blue staining technique contains preoperative and intraoperative localization procedures.
Preoperative localization
-
1)
CT scanning: On the day before the operation, a CT scan was performed in the Department of Radiology at the Shanghai Chest Hospital using Siemens SOMATOM Sensation 16 (Siemens AG, Medical Solutions, Germany). Accompanied by one researcher (LZ), patients were placed on the CT table in either a spine or prone position which allowed the shortest access to the targeted lesion. The spine position (Figure 1a) was suitable for injecting methylene blue dye from the front or axilla area while the prone position (Figure 1b) was for injecting from the back. The targeted lesion was located with several scans of contiguous 2 mm section thickness in full inspiration. The researcher marked the alignment lines of the CT gantry with a “+” sign, placing a metallic mark.
-
2)
Image transferring and simulation data for virtual puncturing: The CT images generated in the Department of Radiology were transferred to the Department of Radiotherapy in our hospital, in which an injection plan was developed using the radiation therapy planning system, Phillips-Pinncle 3 (Philips Healthcare). This system was originally designed for developing radiation therapy and we used the various parameters generated from this system for a different purpose: localizing lesions. According to the CT images, the system software calculated the direction and depth of the radiation beam to the lesion. It also calculated the distance between skin surface to the lesion and the distance from the edge of the lesion to the pleural surface. For our purpose, we envisaged that the injection needle could act as a beam and follow the direction of the beam to reach the targeted lesion according to the distance from skin surface to the lesion calculated by the system. For each lesion, the system provided various entry points and angles. We chose the point with either vertical or horizontal angle to minimize operational difficulties and errors (Figure 2). The simulated virtual data for puncturing were recorded for the next step.
-
3)
Puncture point marking: After obtaining the above data, we placed the patient on a simulator (Ximatron series) for radiotherapy planning in the same position as that for the original CT scan to perform a full 3 D simulation. To ensure the same position as that when the data were collected previously, the alignment lines of the CT gantry aimed at those three “+” signs. Guided by those simulation data, through the computer controlled machine and bed movements, the puncture point was identified and marked as “*” (Figure 3 and Figure 4).
-
4)
Injecting methylene blue in the operation room: Under general anaesthesia, the patient was placed in the same position as that for preoperative CT image collection, and 0.3 ml methylene blue was injected at the marked point according to the angle and depth data and again another 0.2 ml at 10 mm from pleural during needle removal to stain the needle pathway (Figure 5).
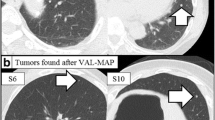
Intraoperative localization procedures
Immediately after injecting methylene blue, the skin was disinfected and thoracoscopy was performed to locate the stain. The surrounding surface was palpated using the index finger for the lesion. The wedge resection of the identified lesion was performed using VATS along with a 3 cm margin of normal lung tissue, including the stained area, and the specimen was placed next to a 5 ml syringe which was taken as a reference length scale to measure the distance between the edge of the lesion and the edge of the stain (Figure 6). The specimen was sent for immediate pathologic examination. All patients with malignant lesions subsequently underwent lobectomy and systematic lymph node dissection. For those with benign lesions, the surgery was completed.
Measurements and data analysis
The preoperative localization time was defined as the period from the time start of CT scanning to the time of marking skin puncture point. Intra-operative localization time was from the injection of methylene blue to the time that the stain was located with the thoracoscope. The success of the localization was determined according to the distance between the edge of the stain and that of the lesion (<20 mm). The success proportions and 95% confidence interval were calculated. Linear regression models were used to assess if age, gender, and the location, distance from pleural surface and size of lesions were associated with the accuracy of this technique. All analyses were performed with Stata SE 12 [12].
Results
Characteristics of participants and lesions
Table 1 shows the characteristics of 74 study participants (27 men and 47 women) and 80 lesions. About 31% study participants were smokers. Two cases had previously been diagnosed with a malignant tumor: one underwent surgery for rectal cancer two years after the identification of the current lesion and the other had been received surgery for thyroid cancer three years before. The mean lesion size was 10.4 mm (SD: 3.5), ranging from 4 mm to 17 mm. The mean intra-operative localization time was 17.4 (SD: 2.3) minutes, ranging from 12 to 23 minutes.
Performance of virtual simulation ─ methylene blue staining technique
Seventy five of 80 lesions were successfully localized and the successful localization rate was 94% (95% CI: 86, 98). The stain-lesion distance for those successfully localized lesions was 5.3 (SD: 3.1), ranging from 0 to 12 mm. Histological examination showed 28 benign lesions and 52 lung cancers.
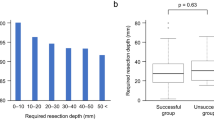
Table 2 shows the stain-lesion distances and successful localization rates by location and pathological diagnosis. There was no significant difference in stain-lesion distance between left and right lungs. The stain-lesion distances were not dependent on the type of histological diagnosis, lesion sizes, age and sex. The lower lobes had a significantly longer stain-lesion distance than upper and middle lobes with a crude average of 3.0 (95% CI: 1.6, 4.3) mm (p<0.001). Further controlling for age, sex, lesion size and pathological diagnosis using the multiple linear regression method, the adjusted difference between lower and upper/middle lobes in stain-lesion distance remained statistically significant with a mean of 3.0 (95% CI: 1.7, 4.4), p<0.001. However, about 80% stain-lesion distances were<5 mm for lesions on middle/upper lobes while 80% stain-lesion distances were <10 mm for lesions on the lower lobes (Figure 7). The successful localization rate was 98% (95% CI: 90, 100) for lesions in upper or middle lobes, which was significantly higher than that for lesions in lower lobes (86%), p=0.036. There were no significant differences in the successful localization rate or stain-lesion difference between left and right lungs and between benign and malignant lesions.
All patients with successfully localized malignant lesions subsequently underwent lobectomy via VATS and systematic lymph node dissection. The postoperative pathology examination revealed all cancer cases as stage T1aN0M0. Wedge resection was performed to remove benign lesions. There were no complications observed in any of the patients as a result of the localization. Among five unsuccessful localized lesions, four were later localized through thorough index palpation around 20-23 mm from the stain. Only one lesion was not localized and the patient underwent thoracotomy. Since the pathologic examination confirmed as a lung cancer case, this patient underwent lobectomy by thoracotomy.
Discussion
In this study, we demonstrated that a new technique could be used to successfully localize small peripheral pulmonary lesions. We found this technique performed well regardless of the pathological diagnosis, lesion size, and distance from lesion to the pleural surface, and patient’s age and gender. This technique performed significantly better for the lesions in upper lobes than in lower lobes. This technique combines the existing virtual simulation technique for planning radiotherapy and methylene blue staining.
With the increasing application of CT to lung cancer screening, small lesions are frequently detected [13, 14]. However, for small lesions, localizing them visually or by palpation during VATS can be difficult [5, 6]. To shorten the time for nodule localization and to prevent unplanned open thoracotomy, several preoperative localization techniques have been introduced as a method of improving the success rate of VATS. Punkett et al. developed a technique of hookwire localization with CT guidance [15–17]. This approach has a high successful localization rate, but increases the risk of some complications including pneumothorax, pleuritic pain, and haemorrhage [18]. It is also associated with a relatively high level of radiation for both patients and doctors. The VATS should be performed immediately after the hookwire placement, which may cause operational difficulties in a busy hospital like ours. Lenglinger et al. developed the percutaneous staining with methylene blue method [8]. Guided by CT, methylene blue dye is injected into the nodule. This method also has a high successful localization rate and no complications associated with the previously mentioned hookwire placement [8, 19, 20]. However, the operation should be performed immediately after the injection before the dye is diffused. To overcome this problem, Nomori and Horio developed a long-lasting point marker termed “colored collagen” which combining atelocollagen, methylene blue and contrast medium [21]. The colored collagen stayed visible at the injected site for several days without toxicity. Another marking technique called “agar marking” was developed by Tsuchida et al. [22]. Powdered agar dissolved in distilled water and kept at >50 degree Celsius to maintain its liquid form which is injected to the target lesion guided by CT. Then, agar can be detected as a hard nodule by palpation, but this approach is difficult to implement. Shennib et al. reported the use of intraoperative intrathoracic ultrasonography for localization of small lesions during VATS [23], which has been assessed by others as a non-invasive and easy to operate technique [24, 25]. However, this technique does not perform well for small lesions <10 mm, particularly for ground glass pulmonary nodules. It also does not perform well for patients with asthma or chronic obstructive pulmonary disease because of the influence of air in the lung tissue. Recently, Chen et al. reported an image-guided navigation system for localization of small pulmonary nodules before thoracoscopic surgery [26]. Although this technique can successfully localize the nodules without some shortcomings of other techniques, the system is costly and complex to operate and has not been commonly used in the current clinical settings.
In our study, we introduced a new technique combining the existing virtual simulation for radiotherapy planning technique and methylene blue staining for the localization of small peripheral pulmonary lesions. With a successful localization rate of 94%, this technique has the following advantages. First, the doctors are not exposed to radiation during the preoperative localization period, and the patients are only exposed to radiation during the initial CT image collection. Second, the patients do not need to be sent to the operating room immediately after virtual puncture, which allows sufficient time for preoperative preparation. Third, patients are less stressed when methylene blue dye was injected under general anaesthesia. Forth, since the injection is performed under general anaesthesia, complications such as pneumothorax and haemorrhage are rare and can be relatively easily handled. Fifth, the operation is performed immediately after the methylene blue injection with little time for the dye to diffuse around the tissue. Finally, since the virtual puncture can be performed using equipment commonly available, it can be easily adopted by most hospitals without extra cost for new equipment. The special equipment required for this technique is a CT simulator (radiation therapy planning system), which is generally available in most hospitals with facilities for radiation therapy. The cost of methylene blue dye is minimal and the total cost of the whole procedure is equivalent to that of a chest CT scan.
However, there are some limitations. First, unlike the real-time CT guided localization methods, the accuracy of our technique depends on the similarity between the body position for virtual puncture and that for injecting the dye. Any inconsistency may cause deviation from the targeted lesion, particularly for the cases in which injection needs to be performed from the back. At the early stage of the study, we instructed patients to cross their hands on the back of the head in a prone position during virtual puncture. Such a position is difficult to repeat during the injection when patients are under general anaesthesia. To minimize such deviation, during the simulation puncture, we instructed patients to naturally rest their hands to their thighs to imitate a position as the one when they were under general anaesthesia for the dye injection. Second, if the injection path is blocked by a costa, the needle entry point should be moved upward or downward and the needle angle will also be changed. This may also cause an inaccurate staining point. Our data showed that the technique performed much better for lesions in the upper and middle lobes than those in the lower lobes. The poor performance for localizing lesions in the lower lobe could be partly explained by those limitations. Our technique failed to localize five of the 80 lesions, three of them were due to inconsistent body positions between simulation and actual injection as previously described, one was due to the lesion being close to the pleural surface and one due to too much dye being injected causing wide diffusion around the tissue. Further investigation is needed to improve the performance of this technique for localizing small peripheral lesions, particularly those in the lower lobes.
From our clinical experience of successful localization, it is important to keep the same body position for the dye injection as that during the simulation. If possible, a horizontal or vertical injection angle should be adopted to inject approximately 0.3 ml of methylene blue dye into the target lesion site and again about 0.2 ml into about 10 mm from the pleural surface during the removal of the needle. Too much dye should be avoided to prevent a large stained area.
Conclusions
Applying CT simulation technique to virtually localize small peripheral lesions and injecting methylene blue dye to the target point according to the simulated data can lead to a high successful localization rate. This technique does not require new equipment and the patients have lower exposure to radiation compared to using a real-time CT guided approach. Injection of the methylene blue dye under general anaesthesia minimises patients stress and associated complications. This technique is safe, effective and readily acceptable with an overall successful localization rate of 94%, even higher for those lesions in middle and upper lobes (98%). Further efforts are needed to improve the successful localization rate and minimize errors.
Abbreviations
- CT:
-
Computer tomography
- VATS:
-
Video-assisted thoracoscopic surgery.
References
Wahidi MM, Govert JA, Goudar RK, Gould MK, McCrory DC: Evidence for the treatment of patients with pulmonary nodules: when is it lung cancer?: ACCP evidence-based clinical practice guidelines (2nd edition). Chest. 2007, 132 (3 Suppl): 94S-107S.
Mayo JR, Clifton JC, Powell TI, English JC, Evans KG, Yee J, McWilliams AM, Lam SC, Finley RJ: Lung nodules: CT-guided placement of microcoils to direct video-assisted thoracoscopic surgical resection. Radiology. 2009, 250 (2): 576-585. 10.1148/radiol.2502080442.
Powell TI, Jangra D, Clifton JC, Lara-Guerra H, Church N, English J, Evans K, Yee J, Coxson H, Mayo JR, et al: Peripheral lung nodules: fluoroscopically guided video-assisted thoracoscopic resection after computed tomography-guided localization using platinum microcoils. Ann Surg. 2004, 240 (3): 481-488. 10.1097/01.sla.0000137132.01881.57. discussion 488-489
Kohi MP, Naeger DM, Kukreja J, Fidelman N, Laberge JM, Gordon RL, Kerlan RK: Preoperative CT-guided percutaneous wire localization of ground glass pulmonary nodules with a modified Kopans wire. J Thorac Dis. 2013, 5 (2): E31-34.
Saito H, Minamiya Y, Matsuzaki I, Tozawa K, Taguchi K, Nakagawa T, Hashimoto M, Hirano Y, Ogawa J: Indication for preoperative localization of small peripheral pulmonary nodules in thoracoscopic surgery. J Thorac Cardiovasc Surg. 2002, 124 (6): 1198-1202. 10.1067/mtc.2002.127331.
Suzuki K, Nagai K, Yoshida J, Ohmatsu H, Takahashi K, Nishimura M, Nishiwaki Y: Video-assisted thoracoscopic surgery for small indeterminate pulmonary nodules: indications for preoperative marking. Chest. 1999, 115 (2): 563-568. 10.1378/chest.115.2.563.
Endo M, Kotani Y, Satouchi M, Takada Y, Sakamoto T, Tsubota N, Furukawa H: CT fluoroscopy-guided bronchoscopic dye marking for resection of small peripheral pulmonary nodules. Chest. 2004, 125 (5): 1747-1752. 10.1378/chest.125.5.1747.
Lenglinger FX, Schwarz CD, Artmann W: Localization of pulmonary nodules before thoracoscopic surgery: value of percutaneous staining with methylene blue. AJR Am J Roentgenol. 1994, 163 (2): 297-300.
Zhang L, Shen-Tu Y: The advance and new methods explore of pulmonary tiny lesions preoperative localization. Zhongguo Fei Ai Za Zhi. 2012, 15 (6): 381-385.
Aird EG, Conway J: CT simulation for radiotherapy treatment planning. Br J Radiol. 2002, 75 (900): 937-949.
Hanna GG, Van SDKJR, Carson KJ, O’Sullivan JM, Hounsell AR, Senan S: Conventional 3D staging PET/CT in CT simulation for lung cancer: impact of rigid and deformable target volume alignments for radiotherapy treatment planning. Br J Radiol. 2011, 84 (1006): 919-929. 10.1259/bjr/29163167.
StataCorp: Stata Statistical Software: Release 12. 2011, College Station, Texas: StataCorp LP
Diederich S: Lung cancer screening: rationale and background. Cancer Imaging. 2011, 11 Spec No A: S75-78.
Diederich S, Thomas M, Semik M, Lenzen H, Roos N, Weber A, Heindel W, Wormanns D: Screening for early lung cancer with low-dose spiral computed tomography: results of annual follow-up examinations in asymptomatic smokers. Eur Radiol. 2004, 14 (4): 691-702. 10.1007/s00330-003-2200-5.
Plunkett MB, Peterson MS, Landreneau RJ, Ferson PF, Posner MC: Peripheral pulmonary nodules: preoperative percutaneous needle localization with CT guidance. Radiology. 1992, 185 (1): 274-276.
Sawhney R, McCowin MJ, Wall SD, Block MI: Fluoroscopically guided placement of the Kopans hookwire for lung nodule localization prior to thoracoscopic wedge resection. J Vasc Interv Radiol. 1999, 10 (8): 1133-1134. 10.1016/S1051-0443(99)70207-1.
Soleto MJ, Olivera MJ, Pun YW, Moreno R, Nieto S, Caballero P: Hookwire localization of pulmonary nodules for video-thorascopic surgical resection. Arch Bronconeumol. 2002, 38 (9): 406-409. 10.1016/S0300-2896(02)75252-6.
Zhou JH, Li WT, Chen HQ, Peng WJ, Xiang JQ, Zhang YW, Wang SP, Yang F, Zhou X, Luo XY: CT-guided hookwire localization of small solitary pulmonary nodules in video-assisted thoracoscopic surgery. Zhonghua Zhong Liu Za Zhi. 2009, 31 (7): 546-549.
Wang YZ, Boudreaux JP, Dowling A, Woltering EA: Percutaneous localisation of pulmonary nodules prior to video-assisted thoracoscopic surgery using methylene blue and TC-99. Eur J Cardiothorac Surg. 2010, 37 (1): 237-238. 10.1016/j.ejcts.2009.07.022.
Wicky S, Mayor B, Schnyder P: Methylene blue localizations of pulmonary nodules under CT-guidance: a new procedure used before thoracoscopic resections. Int Surg. 1997, 82 (1): 15-17.
Nomori H, Horio H: Colored collagen is a long-lasting point marker for small pulmonary nodules in thoracoscopic operations. Ann Thorac Surg. 1996, 61 (4): 1070-1073. 10.1016/0003-4975(96)00024-0.
Tsuchida M, Yamato Y, Aoki T, Watanabe T, Koizumi N, Emura I, Hayashi J: CT-guided agar marking for localization of nonpalpable peripheral pulmonary lesions. Chest. 1999, 116 (1): 139-143. 10.1378/chest.116.1.139.
Shennib H, Bret P: Intraoperative transthoracic ultrasonographic localization of occult lung lesions. Ann Thorac Surg. 1993, 55 (3): 767-769. 10.1016/0003-4975(93)90293-Q.
Piolanti M, Coppola F, Papa S, Pilotti V, Mattioli S, Gavelli G: Ultrasonographic localization of occult pulmonary nodules during video-assisted thoracic surgery. Eur Radiol. 2003, 13 (10): 2358-2364. 10.1007/s00330-003-1916-6.
Mattioli S, D’Ovidio F, Daddi N, Ferruzzi L, Pilotti V, Ruffato A, Bolzani R, Gavelli G: Transthoracic endosonography for the intraoperative localization of lung nodules. Ann Thorac Surg. 2005, 79 (2): 443-449. 10.1016/j.athoracsur.2004.07.087. discussion 443-449
Chen W, Chen L, Qiang G, Chen Z, Jing J, Xiong S: Using an image-guided navigation system for localization of small pulmonary nodules before thoracoscopic surgery: a feasibility study. Surg Endosc. 2007, 21 (10): 1883-1886. 10.1007/s00464-007-9198-8.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2407/14/79/prepub
Acknowledgements
We thank all patients for their participation, staff members in the Department of Anaesthesia, Department of Radiology, and Department of Radiotherapy, the Shanghai Chest Hospital for their cooperation and assistance in data collection. ZW was supported by the Senior Research Fellowship of National Health & Medical Research Council (NHMRC) of Australia (APP1042343).
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
This study was conceived and designed by YS and LZ. YS, LZ, HG, FM, MC and ZD participated in the acquisition of data. YS, LZ and ZW participated in the statistical analysis, drafting and critical revision of the manuscript. All authors read and approved the final manuscript.
Yang Shentu, Liang Zhang contributed equally to this work.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Shentu, Y., Zhang, L., Gu, H. et al. A new technique combining virtual simulation and methylene blue staining for the localization of small peripheral pulmonary lesions. BMC Cancer 14, 79 (2014). https://doi.org/10.1186/1471-2407-14-79
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2407-14-79