Abstract
Background
Intraoperative detection of 18F-FDG-avid tissue sites during 18F-FDG-directed surgery can be very challenging when utilizing gamma detection probes that rely on a fixed target-to-background (T/B) ratio (ratiometric threshold) for determination of probe positivity. The purpose of our study was to evaluate the counting efficiency and the success rate of in situ intraoperative detection of 18F-FDG-avid tissue sites (using the three-sigma statistical threshold criteria method and the ratiometric threshold criteria method) for three different gamma detection probe systems.
Methods
Of 58 patients undergoing 18F-FDG-directed surgery for known or suspected malignancy using gamma detection probes, we identified nine 18F-FDG-avid tissue sites (from amongst seven patients) that were seen on same-day preoperative diagnostic PET/CT imaging, and for which each 18F-FDG-avid tissue site underwent attempted in situ intraoperative detection concurrently using three gamma detection probe systems (K-alpha probe, and two commercially-available PET-probe systems), and then were subsequently surgical excised.
Results
The mean relative probe counting efficiency ratio was 6.9 (± 4.4, range 2.2–15.4) for the K-alpha probe, as compared to 1.5 (± 0.3, range 1.0–2.1) and 1.0 (± 0, range 1.0–1.0), respectively, for two commercially-available PET-probe systems (P < 0.001). Successful in situ intraoperative detection of 18F-FDG-avid tissue sites was more frequently accomplished with each of the three gamma detection probes tested by using the three-sigma statistical threshold criteria method than by using the ratiometric threshold criteria method, specifically with the three-sigma statistical threshold criteria method being significantly better than the ratiometric threshold criteria method for determining probe positivity for the K-alpha probe (P = 0.05).
Conclusions
Our results suggest that the improved probe counting efficiency of the K-alpha probe design used in conjunction with the three-sigma statistical threshold criteria method can allow for improved detection of 18F-FDG-avid tissue sites when a low in situ T/B ratio is encountered.
Similar content being viewed by others
Background
Intraoperative gamma probe detection of various radioisotopes during radioguided surgery has become commonplace and is an established discipline within the practice of surgery [1]. Along these lines, 18F-fluorodeoxyglucose (18F-FDG), which is widely used for diagnostic positron emission tomography (PET) imaging for a variety of solid malignancies, has recently become the object of increased investigations into its utility for the identification of 18F-FDG-avid tissue sites during radioguided surgery [2–12]. In this specific regard, it has become increasingly advantageous to specifically design intraoperative radiation detection probes to directly or indirectly detect the resultant 511 KeV gamma emissions following positron annihilation emanating from 18F-FDG-avid tissues. Nevertheless, most gamma detection probes that are currently commercially available have been designed for detecting radioisotopes of gamma-ray energies much lower than 511 KeV. Such radioisotopes include: (1) 99mTc (140 and 142 KeV) that has most commonly been used for sentinel lymph node biopsy procedures and parathyroid surgery; (2) 111In (171 and 247 KeV) that has been used with octreotide to detect neuroendocrine tumors; (3) 123I (159 KeV) that has been used with metaiodobenzylguanidine to detect neuroblastomas and pheochromocytomas; and (4) 125I (35 KeV) that has been used with anti-TAG-72 monoclonal antibodies and anti-CEA monoclonal antibodies during radioimmunoguided surgery [1].
The success of detecting and localizing 18F-FDG-avid tissue sites during 18F-FDG-directed surgery is affected by several factors, including: (1) the counting efficiency of the detection probe used; and (2) the target-to-background (T/B) ratio of the radioactive emissions of 18F-FDG. Various authors have examined the role played by the T/B ratio for correctly identifying 18F-FDG-avid tissue sites for PET imaging [13] and during 18F-FDG-directed surgery [14–20]. The finding of a low T/B ratio of 18F-FDG is multifactorial, and can be influenced by factors such as the paucity of tumor vascularization, the co-existence of large areas of tumor necrosis, the existence of an intrinsic low metabolic rate for some tumors, and the close proximity of tumor to areas of elevated physiologic 18F-FDG uptake or accumulation [1, 16–20]. Gulec et al. [16–18] has suggested that a minimum in situ T/B ratio of 1.5-to-1.0 for 18F-FDG is necessary, in order “for the operating surgeon to be comfortable that the difference between tumor and normal tissue are significant” during 18F-FDG-directed surgery. However, it has been our own experience that the observed in situ T/B ratio seen during 18F-FDG-directed surgery is commonly less than 1.5-to-1.0, and is highly dependent upon the specific detection probe used. Therefore, the in situ intraoperative detection and localization of 18F-FDG-avid tissue sites during 18F-FDG-directed surgery can be very challenging when utilizing standard gamma detection probes and PET probes that rely solely on a fixed T/B ratio (i.e., ratiometric threshold) as the threshold for probe positivity for the identification of 18F-FDG-avid tissue sites.
In this regard, it is our contention that improved in situ intraoperative detection of 18F-FDG-avid tissue sites with a gamma detection probe system can be attained by taking advantage of the increased probe counting efficiency offered by the K-alpha probe design [21] and by utilizing a variance-based statistical analysis schema [22] with the three-sigma criteria [23, 24].
A variance-based statistical analysis schema was previously described by Currie for qualitative detection and quantitative determination in radiochemistry [22]. By applying hypothesis testing, Currie reduced the threshold for a significant difference between background radiation and target radiation to a variance-based statistical model. Such hypothesis testing and statistical modeling has become commonplace in the analysis of medical data, including medical imaging [25, 26]. The application of variance-based modeling to the determination of the threshold for gamma detection probe positivity, in the form of the three-sigma criteria for gamma detection probe positivity, was popularized by Thurston [23, 24] and has since then been well validated in radioimmunoguided surgery involving 125I- labeled anti-TAG-72 monoclonal antibodies [24, 27–31]. The three-sigma criteria defines a tissue as being probe positive when the count rate in that tissue exceeds three standard deviations above the count rate detected with normal adjacent background tissue [23, 24, 27–31].
An example of a gamma detection probe that can greatly benefit from the three-sigma statistical threshold criteria is the K-alpha probe [21]. The K-alpha probe design, which was also elucidated by Thurston in 2007, utilizes the concept of detecting secondary, lower energy gamma emissions (K-alpha x-ray fluorescence) that result when a thin metal foil plate (typically lead) is placed between a cadmium-zinc-telluride crystal and a source of gamma emissions, such as 18F-FDG [21]. It is our contention that when concurrently utilized, the K-alpha probe design and the three-sigma criteria can improve the intraoperative detection of 18F-FDG-avid tissue sites, even at very low T/B ratios for 18F-FDG, and would represent a methodology that is superior to a fixed T/B ratio (i.e., ratiometric threshold) methodology used by other gamma detection probe systems for detection of 18F-FDG-avid tissue sites.
In the current report, we evaluated the probe counting efficiency and the success rate of in situ intraoperative detection of 18F-FDG-avid tissue sites (using the three-sigma statistical threshold criteria method and the ratiometric threshold criteria method) that were assessed concurrently with three gamma detection probe systems (consisting of the K-alpha probe system and two commercially-available PET-probe systems) during 18F-FDG-directed surgery.
Methods
All data analyzed in this manuscript were obtained from the master database of an institutional review board (IRB)-approved, prospective, pilot study protocol for multimodal imaging and detection performed during 18F-FDG-directed surgery for known or suspected malignancy at the Arthur G. James Cancer Hospital and Richard J. Solove Research Institute of The Ohio State University Wexner Medical Center that was previously approved by the Cancer IRB of the Office of Responsible Research Practices of The Ohio State University.
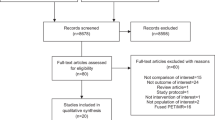
From a total of 65 patients who gave informed consent to participate in the IRB-approved, prospective, pilot study protocol, a total of 60 patients were taken to the operating room, and of which 58 patients underwent 18F-FDG-directed surgery for known or suspected malignancy using gamma detection probes. Of those 58 patients undergoing 18F-FDG-directed surgery for known or suspected malignancy using gamma detection probes, we identified all cases in which 18F-FDG-avid tissue sites were identified on same-day preoperative diagnostic PET/CT imaging, and for which each of these 18F-FDG-avid tissue sites underwent attempted in situ intraoperative detection (based upon determination of the in situ counts per second measurements recorded during 18F-FDG-directed surgery) concurrently using three separate gamma detection probe systems, and then were subsequently surgical excised. The first system was the K-alpha probe system [21]. The two other systems represented commercially-available PET-probe systems that were designed specifically to directly or indirectly detect resultant 511 KeV gamma emissions following positron annihilation emanating from 18F-FDG-avid tissue sites. These two commercially-available PET-probe systems were the RMD Navigator™ Gamma-PET™ probe system (RMD PET probe; Dynasil Corporation, Watertown, MA) and the Neoprobe® neo2000® GDS PET probe system (Neoprobe PET probe; Devicor Medical Products, Incorporated, Cincinnati, OH). All three gamma detection probe systems had to be used concurrently in each case for attempted in situ intraoperative detection in order for any particular case to qualify for inclusion in the current analyses.
In each instance, a count rate (i.e., counts per second) was taken from an area selected for the measurement of background tissue count rate and from the area of presumed 18F-FDG-avid tissue selected for the measurement of target tissue count rate. An area of presumed normal tissue within a region adjacent to the area of the target tissue was selected for the measurement of background tissue count rate. Three separate recorded values were used to generate each averaged target tissue count rate measurement determined for each area of presumed 18F-FDG-avid tissue. All values used for the averaged count rate measurements were reported as averaged counts per second. All of the averaged target tissue count rate measurements that are reported in this paper represent measurements taken on an area of presumed 18F-FDG-avid tissue before it was surgically excised (i.e., in situ measurements). None of the averaged target tissue count rate measurements that are reported in this paper represent measurements taken on an area of presumed 18F-FDG-avid tissue after it was surgically excised (i.e., ex situ measurements).
The counting efficiency [32] of each of the three gamma detection probe systems was calculated for each 18F-FDG-avid tissue site identified during in situ intraoperative detection. The probe counting efficiency was defined as a relative probe counting efficiency ratio for each of the individual three gamma detection probe systems, consisting of the ratio of the averaged target tissue count rate for each 18F-FDG-avid tissue site using each of the individual three gamma detection probe systems as compared to the averaged target tissue count rate of the gamma detection probe system with the lowest averaged target tissue count rate for each 18F-FDG-avid tissue site. Thus, the relative probe counting efficiency ratio for the gamma detection probe system with the lowest averaged target tissue count rate will resultantly be reported as 1.0.
A calculated fixed T/B ratio was calculated for each target tissue as the ratio of the averaged target tissue count rate to the background tissue count rate. A calculated three-sigma criteria count rate was calculated for each target tissue by the methodology popularized of Thurston [23, 24], based upon taking the standard deviation derived from the normal background tissue count rate and multiplying that standard deviation by a factor of three and then adding that number to the normal background tissue count rate. For the calculated fixed T/B ratio method (i.e., ratiometric threshold criteria method), a ratiometric threshold of 1.5-to-1.0 or greater was set as the ratiometric threshold criteria of probe positivity. For the calculated three-sigma criteria count rate method, three-sigma statistical threshold of probe positivity was met when the calculated three-sigma criteria count rate for the target tissue was exceeded by the actual target tissue count rate. The determination of probe positivity for successful in situ intraoperative detection of 18F-FDG-avid tissue sites by each of the three gamma detection probe systems was then compared both by the ratiometric threshold criteria method and by the three-sigma statistical threshold criteria method.
All results were expressed as mean (± SD, range). The software program IBM SPSS® 19 for Windows® (SPSS, Inc., Chicago, Illinois) was used for the data analysis. All mean value comparisons were made by one-way analysis of variance (ANOVA). All categorical variable comparisons were made using 2 × 2 or 2 × 3 contingency tables that were analyzed by either the Pearson chi-square test or the Fisher exact test, when appropriate. Categorical variable comparisons were made for probe type as a function of threshold criteria and for threshold criteria as a function of probe type. P-values determined to be 0.05 or less were considered to be statistically significant. All reported categorical variable comparisons P-values were two-sided.
Results
Of those 58 patients undergoing 18F-FDG-directed surgery for known or suspected malignancy using gamma detection probes, we identified seven patients (four Caucasian males, two Caucasian females, and one African-American female) who underwent same-day preoperative diagnostic PET/CT imaging and in whom all three previously described gamma detection probe systems were then concurrently utilized for attempted in situ intraoperative identification of 18F-FDG-avid tissue sites between the dates of March 3, 2009 and March 19, 2009. These seven patients had a mean age of 57 (± 12, range 41–80) years, a mean body weight of 79.8 (± 16.8, range 59.9–102.1) kilograms or 176 (± 37, range 132–225) pounds, and a mean same-day pre-scanning blood sugar of 99 (± 21, range 78–137) milligrams per deciliter. The mean 18F-FDG injection dose was 540 (± 51, range 433–587) MBq or 14.6 (± 1.4, range 11.7–15.9) millicuries.
Within this group of seven patients, a total of nine separate 18F-FDG-avid tissue sites, which were identified on same-day preoperative diagnostic PET/CT imaging, were intraoperatively assessed in situ with all three gamma detection probe systems, and were subsequently surgical excised. Additionally, in one of the seven patients, there were four intraoperative clinically suspicious sites (i.e., intraoperative clinically palpable sites) within the surgical field that were not 18F-FDG-avid on preoperative same-day diagnostic PET/CT imaging, but were intraoperatively assessed in situ with all three gamma detection probe systems and were subsequently surgical excised.
The nine separate 18F-FDG-avid tissue sites had a mean SUVmax of 8.6 (± 3.8, range 1.9–13.4) on same-day preoperative diagnostic PET/CT imaging. The mean time from 18F-FDG injection to same-day preoperative diagnostic PET/CT imaging in the seven patients evaluated was 94 (± 38, range 66–179) minutes, with only one patient exceeding mean time of 94 minutes from 18F-FDG injection to same-day preoperative diagnostic PET/CT imaging. The mean time from 18F-FDG injection to the time of the start of surgery in the seven patients evaluated was 219 (± 61, range 168–305) minutes. The mean time from 18F-FDG injection to the time of attempted in situ intraoperative gamma probe detection in the seven patients evaluated was 295 (± 87, range 187–409) minutes.
In Table 1, the mean value of various count rate variables, relative probe counting efficiency ratio, and T/B ratio for the nine 18F-FDG-avid tissue sites tested by the three different gamma detection probe systems are shown.
The mean of the averaged target tissue count rate for the nine 18F-FDG-avid tissue sites was 960 (± 907, range 80–2509) counts per second using the K-alpha probe system, 203 (± 153, range 45–446) counts per second using the RMD PET probe system, and 150 (± 121, range 32–322) counts per second using the Neoprobe PET probe system (P = 0.006).
The mean of the background tissue count rate in an area of presumed normal tissue within a region adjacent to the nine 18F-FDG-avid tissue sites was 755 (± 858, range 32–2257) counts per second using the K-alpha probe system, 133 (± 104, range 37–344) counts per second using the RMD PET probe system, and 71 (± 65, range 18–197) counts per second using the Neoprobe PET probe system (P = 0.014).
The probe counting efficiency was assessed for all three gamma detection probe systems. The mean relative probe counting efficiency ratio was 6.9 (± 4.4, range 2.2–15.4) for the K-alpha probe system, was 1.5 (± 0.3, range 1.0–2.1) for the RMD PET probe system, and was 1.0 (± 0, range 1.0–1.0) for the Neoprobe PET probe system (P < 0.001).
The mean of the calculated fixed T/B ratio for the nine 18F-FDG-avid tissue sites was 1.6 (± 0.6, range 1.1–2.5) for the K-alpha probe system, 1.6 (± 0.5, range 1.2–2.4) for the RMD PET probe system, and 2.3 (± 1.0, range 1.4–4.2) for the Neoprobe PET probe system (P = 0.073).
The mean of the calculated three-sigma criteria count rate for the nine 18F-FDG-avid tissue sites was 827 (± 901, range 49–2400) counts per second for the K-alpha probe system, 165 (± 117, range 55–400) counts per second for the RMD PET probe system, and 94 (± 76, range 31–239) counts per second for the Neoprobe PET probe system (P = 0.012).
The detection success rate for probe positivity for the nine separate 18F-FDG-avid tissue sites by the ratiometric threshold criteria method and by the three-sigma statistical threshold criteria method at the time of attempted in situ intraoperative detection was assessed for all three gamma detection probe systems. The K-alpha probe system detection success rate for probe positivity was in 3/9 cases (33%) by the ratiometric threshold criteria method and in 8/9 cases (89%) by the three-sigma statistical threshold criteria method. The RMD PET probe system detection success rate for probe positivity was in 3/9 cases (33%) by the ratiometric threshold criteria method and in 4/9 cases (44%) by the three-sigma statistical threshold criteria method. The Neoprobe PET probe system detection success rate for probe positivity was in 7/9 cases (78%) by the ratiometric threshold criteria method and in 8/9 cases (89%) by the three-sigma statistical threshold criteria method. Therefore, with each of the three gamma detection probe systems tested, successful in situ intraoperative detection of 18FDG-avid tissue sites was more frequently accomplished by using the three-sigma statistical threshold criteria method than by using the ratiometric threshold criteria method. While the overall categorical variable comparison of the three gamma detection probe systems utilized as a function of the specific threshold criteria used was not found to be statistically significant (P = 0.094), the individual categorical variable comparison of the K-alpha probe as a function of the specific threshold criteria used demonstrated that the three-sigma statistical threshold criteria method was significantly better than the ratiometric threshold criteria method for determining probe positivity for the K-alpha probe (P = 0.050). All other categorical variable comparisons for probe type as a function of threshold criteria and for threshold criteria as a function of probe type were found not to be statistically significant, with the lack of significant differences in these categorical variable comparisons most realistically attributable to the small number of cases available for each of these resultant 2 × 2 and 2 × 3 contingency table analyses.
The previously mentioned four intraoperative clinically suspicious sites that were identified in one of the seven patients (that were not 18F-FDG-avid on preoperative same-day diagnostic PET/CT imaging, but were intraoperatively assessed in situ with all three gamma detection probe systems and were subsequently surgical excised) were not determined to be probe positive by the ratiometric threshold criteria method or by the three-sigma statistical threshold criteria method at the time of attempted in situ intraoperative detection by any of the three gamma detection probe systems.
All nine separate 18F-FDG-avid tissue sites (which were identified on same-day preoperative diagnostic PET/CT imaging, and which were intraoperatively assessed in situ with all three gamma detection probe systems and subsequently surgical excised), were visualized as 18F-FDG-avid tissue sites on same-day perioperative ex situ specimen PET/CT imaging. The mean time from 18F-FDG injection to same-day perioperative specimen PET/CT imaging for the nine separate 18F-FDG-avid tissue specimens evaluated was 488 (± 130, range 340–661) minutes. None of the four intraoperative clinically suspicious sites that were identified in one of the seven patients (that were not 18F-FDG-avid on preoperative same-day diagnostic PET/CT imaging, but were intraoperatively assessed in situ with all three gamma detection probe systems and were subsequently surgical excised) were visualized as potential 18F-FDG-avid tissue sites on same-day perioperative ex situ specimen PET/CT imaging.
Final histopathologic evaluation of the nine separate 18F-FDG-avid tissue sites revealed squamous cell carcinoma of the head and neck region in five 18F-FDG-avid tissue sites, as well one site containing invasive ductal carcinoma of the breast, one site containing non-small cell carcinoma of the lung, one site containing malignant melanoma, and one site containing eccrine porocarcinoma. Final histopathologic evaluation of the four intraoperative clinically suspicious sites identified in one of the seven patients (that were not 18F-FDG-avid on preoperative same-day diagnostic PET/CT imaging and were not intraoperatively detected in situ with any of the three gamma detection probe systems and were subsequently surgical excised and were not visualized as potential 18F-FDG-avid tissue sites on same-day perioperative ex situ specimen PET/CT imaging) showed benign lymphoid tissue only.
Discussion
It is our observation that in situ T/B ratios for 18F-FDG-avid tissue sites detected intraoperatively are often less than 1.5-to-1.0, making localization of such 18F-FDG-avid tissue sites very challenging when utilizing standard gamma detection probes and PET probes that rely solely on a fixed T/B ratio (ratiometric threshold criteria method) as the threshold for probe positivity. Therefore, an optimized gamma detection probe design that allows for the in situ intraoperative detection and localization of 18F-FDG-avid tissue sites having an in situ T/B ratio of less than 1.5-to-1.0 is essential to performing successful 18F-FDG-directed surgery.
In the current report, we evaluated the probe counting efficiency and the success rate of in situ intraoperative detection of 18F-FDG-avid tissue sites (using the three-sigma statistical threshold criteria method and the ratiometric threshold criteria method) for three gamma detection probe systems tested during 18F-FDG-directed surgery. We found that the mean relative probe counting efficiency was significantly better (P < 0.001) for the K-alpha probe system than for the two commercially-available PET-probe systems. Likewise, we found that successful in situ intraoperative detection of 18F-FDG-avid tissue sites was more frequently accomplished by using the three-sigma statistical threshold criteria method than by using the ratiometric threshold criteria method with each of the three gamma detection probe systems tested. In that regard, as based upon categorical variable comparison of the K-alpha probe as a function of the specific threshold criteria used, we specifically found that the three-sigma statistical threshold criteria method was significantly better than the ratiometric threshold criteria method for determining probe positivity for the K-alpha probe (P = 0.050). Yet, there was a general lack of significant differences in our analyses of all other individual categorical variable comparisons between probe type as a function of threshold criteria and between threshold criteria as a function of probe type. It is our contention this finding is most realistically attributable the small sample size (n = 9) that was available for the 2 × 2 and 2 × 3 contingency table analyses.
When applying commercially-available PET probe systems for the detection of 18F-FDG-avid tissue sites, the probe counting efficiency falls off rapidly with increasing gamma energy levels [19, 20]. The intrinsic counting efficiency (i.e. the efficiency taking collimation and probe housing into account) of such commercially-available PET probe systems is less than 2% at a gamma energy level of 511 KeV [19, 20]. The physical size and weight of a typical PET probe is primarily a function of the side shielding that is required to block background radiation, to limit the field of view, and to collimate the head of the probe, with the intention to limit the area of the tissue contributing to the probe count rate and to provide better spatial resolution between tissues of differing radioactivity levels [1]. Attempts at improving PET probe design by further increasing collimation and by creating crystal geometry of sufficient diameter and thickness to capture a higher percentage of 511 KeV gamma emissions would result in a PET probe construct that would be prohibitively large in physical size, heavy in weight, and expensive [1, 21]. These factors represent significant barriers to the clinical application of currently commercially-available PET probe systems for the detection of 18F-FDG-avid tissue sites.
The use of collimation in PET probe design has very divergent effects on the probe counting efficiency versus the resultant T/B ratio observed, with collimation reducing probe counting efficiency at 18F-FDG-avid tissue sites and increasing the T/B ratio observed at 18F-FDG-avid tissue sites [1, 19, 20]. The effects of collimation are evident in both the determination of the probe counting efficiency and in the T/B ratio observed for the three gamma detection probe systems we examined, with the K-alpha probe having significantly better mean relative probe counting efficiency ratio as compared to the RMD PET probe system or the Neoprobe PET probe (6.9 for the K-alpha probe versus 1.5 for the RMD PET probe and 1.0 for the Neoprobe PET probe; P < 0.001) and with the Neoprobe PET probe having nearly-significantly improvement in the mean T/B ratio observed as compared to the K-alpha probe or the RMD PET probe (2.3 for the Neoprobe PET probe versus 1.6 for the K-alpha probe and 1.6 for the RMD PET probe system; P = 0.073). Therefore, the Neoprobe PET probe performed the best with the ratiometric threshold criteria method because it was specifically designed to maximize the T/B ratio through the use of increased collimation for attempting to directly count the 511 KeV gamma photon emissions. Yet, commercially-available PET probe systems, like the Neoprobe PET probe, which utilize increased collimation and have a resultantly low probe counting efficiency cannot fully take advantage of the three-sigma statistical threshold criteria method.
However, the K-alpha probe design [21], which lacks collimation, has a significantly higher probe counting efficiency, and has a decrease in the T/B ratio, can specifically benefit from the use of the three-sigma statistical threshold criteria method. It is our contention that the higher probe counting efficiency of the K-alpha probe design allowed for successful in situ intraoperative detection of 18F-FDG-avid tissue sites with lower T/B ratios, even down to a T/B ratio as low as 1.1-to-1.0. This is the end result of the fact that the K-alpha probe [21] does not directly count the 511 KeV gamma photon emissions, and instead counts the secondary, lower energy gamma emissions (K-alpha x-ray fluorescence) from a thin lead plate placed between the detection crystal and the source of gamma emissions, producing a much higher probe counting efficiency. Thus, its higher probe counting efficiency and the direct counting of secondary, lower energy gamma emissions by the K-alpha probe lends well to maximizing the benefits from use of the three-sigma statistical threshold criteria method. Furthermore, the K-alpha probe can be designed to be significantly smaller and lighter in weight than any commercially-available PET probe system, since the detection crystal can be made relatively thin and can be housed within a detection probe head with little or no needed collimation [21]. This resultant K-alpha design opens up the possibilities for the production of a commercially-available PET probe system that can be easily adapted for use in laparoscopic and robotic surgeries.
Conclusions
Probe counting efficiency was significantly better for the K-alpha probe system than for the two commercially-available PET-probe systems. Successful in situ intraoperative detection of 18F-FDG-avid tissue sites was more frequently accomplished with each of the three gamma detection probe systems tested by using the three-sigma statistical threshold criteria method than by using the ratiometric threshold criteria method, specifically with the three-sigma statistical threshold criteria method being significantly better than the ratiometric threshold criteria method for determining probe positivity for the K-alpha probe. Our results suggest that the improved probe counting efficiency of the K-alpha probe design used in conjunction with the three-sigma statistical threshold criteria method can allow for improved detection of 18F-FDG-avid tissue sites when a low in situ T/B ratio is encountered. Further research and development are needed to more clearly understand these findings and to optimize gamma detection probe design for the intraoperative detection of 18F-FDG-avid tissue sites during 18F-FDG-directed surgery.
References
Povoski SP, Neff RL, Mojzisik CM, O'Malley DM, Hinkle GH, Hall NC, Murrey DA, Knopp MV, Martin EW: A comprehensive overview of radioguided surgery using gamma detection probe technology. World J Surg Oncol. 2009, 7: 11-10.1186/1477-7819-7-11.
Povoski SP, Hall NC, Murrey DA, Chow AZ, Gaglani JR, Bahnson EE, Mojzisik CM, Kuhrt MP, Hitchcock CL, Knopp MV, Martin EW: Multimodal imaging and detection approach to 18F-FDG-directed surgery for patients with known or suspected malignancies: a comprehensive description of the specific methodology utilized in a single-institution cumulative retrospective experience. World J Surg Oncol. 2011, 9: 152-10.1186/1477-7819-9-152.
Desai DC, Arnold M, Saha S, Hinkle G, Soble D, Fry J, DePalatis LR, Mantil J, Satter M, Martin EW: Correlative whole-body FDG-PET and intraoperative gamma detection of FDG distribution in colorectal cancer. Clin Positron Imaging. 2000, 3: 189-196. 10.1016/S1095-0397(00)00052-2.
Zervos EE, Desai DC, DePalatis LR, Soble D, Martin EW: 18F-labeled fluorodeoxyglucose positron emission tomography-guided surgery for recurrent colorectal cancer: a feasibility study. J Surg Res. 2001, 97: 9-13. 10.1006/jsre.2001.6092.
Sarikaya I, Povoski SP, Al-Saif OH, Kocak E, Bloomston M, Marsh S, Cao Z, Murrey DA, Zhang J, Hall NC, Knopp MV, Martin EW: Combined use of preoperative 18F FDG-PET imaging and intraoperative gamma probe detection for accurate assessment of tumor recurrence in patients with colorectal cancer. World J Surg Oncol. 2007, 5: 80-10.1186/1477-7819-5-80.
Hall NC, Povoski SP, Murrey DA, Knopp MV, Martin EW: Combined approach of perioperative 18F-FDG PET/CT imaging and intraoperative 18F-FDG handheld gamma probe detection for tumor localization and verification of complete tumor resection in breast cancer. World J Surg Oncol. 2007, 5: 143-10.1186/1477-7819-5-143.
Sun D, Bloomston M, Hinkle G, Al-Saif OH, Hall NC, Povoski SP, Arnold MW, Martin EW: Radioimmunoguided surgery (RIGS), PET/CT image-guided surgery, and fluorescence image-guided surgery: past, present, and future. J Surg Oncol. 2007, 96: 297-308. 10.1002/jso.20869.
Povoski SP, Hall NC, Martin EW, Walker MJ: Multimodality approach of perioperative 18F-FDG PET/CT imaging, intraoperative 18F-FDG handheld gamma probe detection, and intraoperative ultrasound for tumor localization and verification of resection of all sites of hypermetabolic activity in a case of occult recurrent metastatic melanoma. World J Surg Oncol. 2008, 6: 1-10.1186/1477-7819-6-1.
Cohn DE, Hall NC, Povoski SP, Seamon LG, Farrar WB, Martin EW: Novel perioperative imaging with 18F-FDG PET/CT and intraoperative 18F-FDG detection using a handheld gamma probe in recurrent ovarian cancer. Gynecol Oncol. 2008, 110: 152-157. 10.1016/j.ygyno.2008.04.026.
Moffatt-Bruce SD, Povoski SP, Sharif S, Hall NC, Ross P, Johnson MA, Martin EW: A novel approach to positron emission tomography in lung cancer. Ann Thorac Surg. 2008, 86: 1355-1357. 10.1016/j.athoracsur.2008.03.072.
Agrawal A, Hall NC, Ringel MD, Povoski SP, Martin EW: Combined use of perioperative TSH-stimulated 18F-FDG PET/CT imaging and gamma probe radioguided surgery to localize and verify resection of iodine scan-negative recurrent thyroid carcinoma. Laryngoscope. 2008, 118: 2190-2194. 10.1097/MLG.0b013e3181845738.
Hall NC, Povoski SP, Murrey DA, Knopp MV, Martin EW: Bringing advanced medical imaging into the operative arena could revolutionize the surgical care of cancer patients. Expert Rev Med Devices. 2008, 5: 663-667. 10.1586/17434440.5.6.663.
Frangioni JV: The problem is background, not signal. Mol Imaging. 2009, 8: 303-304.
Yasuda S, Makuuchi H, Fujii H, Nakasaki H, Mukai M, Sadahiro S, Tajima T, Ide M, Shohtsu A, Suzuki Y: Evaluation of a surgical gamma probe for detection of 18F-FDG. Tokai J Exp Clin Med. 2000, 25: 93-99.
Yamamoto S, Higashi T, Matsumoto K, Senda M: Development of a positron-imaging detector with background rejection capability. Ann Nucl Med. 2006, 20: 655-662. 10.1007/BF02984676.
Gulec SA, Daghighian F, Essner R: PET-Probe: Evaluation of Technical Performance and Clinical Utility of a Handheld High-Energy Gamma Probe in Oncologic Surgery. Ann Surg Oncol. 2006, Jul 24; [Epub ahead of print]
Gulec SA, Hoenie E, Hostetter R, Schwartzentruber D: PET probe-guided surgery: applications and clinical protocol. World J Surg Oncol. 2007, 5: 65-10.1186/1477-7819-5-65.
Gulec SA: PET probe-guided surgery. J Surg Oncol. 2007, 96: 353-357. 10.1002/jso.20862.
Piert M, Burian M, Meisetschläger G, Stein HJ, Ziegler S, Nährig J, Picchio M, Buck A, Siewert JR, Schwaiger M: Positron detection for the intraoperative localisation of cancer deposits. Eur J Nucl Med Mol Imaging. 2007, 34: 1534-1544. 10.1007/s00259-007-0430-5.
Piert M, Carey J, Clinthorne N: Probe-guided localization of cancer deposits using [18F]fluorodeoxyglucose. Q J Nucl Med Mol Imaging. 2008, 52: 37-49.
Martin EW, Chapman GJ, Subramaniam VV, Povoski SP: Intraoperative detection of gamma emissions using K-alpha X-ray fluorescence. Expert Rev Med Devices. 2010, 7: 431-434. 10.1586/erd.10.33.
Currie LA: Limits for qualitative detection and quantitative determination. Application to radiochemistry. Anal Chem. 1968, 40: 586-593. 10.1021/ac60259a007.
Thurston MO: Development of the gamma-detecting probe for radioimmunoguided surgery. Radioimmunoguided Surgery (RIGS) in the Detection and Treatment of Colorectal Cancer. Edited by: Martin EW. 1994, Austin: R.G. Landes Company, 41-65. 1
Martin EW, Thurston MO: The use of monoclonal antibodies (MAbs) and the development of an intraoperative hand-held probe for cancer detection. Cancer Invest. 1996, 14: 560-571. 10.3109/07357909609076901.
Vardi Y, Shepp LA, Kaufman L: A statistical model for positron emission tomography. J Am Statist Assoc. 1985, 80: 8-20. 10.1080/01621459.1985.10477119.
Turkheimer FE, Aston JA, Cunningham VJ: On the logic of hypothesis testing in functional imaging. Eur J Nucl Med Mol Imaging. 2004, 31: 725-732. 10.1007/s00259-003-1387-7.
Arnold MW, Young DC, Hitchcock CL, Schneebaum S, Martin EW: Radioimmunoguided surgery in primary colorectal carcinoma: an intraoperative prognostic tool and adjuvant to traditional staging. Am J Surg. 1995, 170: 315-318. 10.1016/S0002-9610(99)80295-5.
Bertsch DJ, Burak WE, Young DC, Arnold MW, Martin EW: Radioimmunoguided Surgery system improves survival for patients with recurrent colorectal cancer. Surgery. 1995, 118: 634-638. 10.1016/S0039-6060(05)80029-7. discussion 638–639
Bertsch DJ, Burak WE, Young DC, Arnold MW, Martin EW: Radioimmunoguided surgery for colorectal cancer. Ann Surg Oncol. 1996, 3: 310-316. 10.1007/BF02306288.
Arnold MW, Hitchcock CL, Young DC, Burak WE, Bertsch DJ, Martin EW: Intra-abdominal patterns of disease dissemination in colorectal cancer identified using radioimmunoguided surgery. Dis Colon Rectum. 1996, 39: 509-513. 10.1007/BF02058702.
Barbera-Guillem E, Arnold MW, Nelson MB, Martin EW: First results for resetting the antitumor immune response by immune corrective surgery in colon cancer. Am J Surg. 1998, 176: 339-343. 10.1016/S0002-9610(98)00192-5.
Knoll GF: Radiation Detection and Measurement. 2010, New York: John Wiley & Sons, 4
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2407/13/98/prepub
Acknowledgements
The authors would like to thank the following surgeons at OSUMC for the inclusion of data from their 18F-FDG-directed surgery patients in this paper: Drs. David Cohn, Amit Agrawal, Enver Ozer, Carl Schmidt, and Susan Moffatt-Bruce.
The authors would like to thank Dr. Donn Young from the Center for Biostatistics of the Comprehensive Cancer Center at OSUMC for his input into the statistical analyses used in this paper.
The authors would like to thank Dr. Charles Hitchcock from the Department of Pathology at OSUMC, Deborah Hurley, Marlene Wagonrod, and the entire staff of the Division of Nuclear Medicine from the Department of Radiology at OSUMC, Nichole Storey from the Department of Radiology at OSUMC, and the operating room staff from the Arthur G. James Cancer Hospital and Richard J. Solove Research Institute at OSUMC for their ongoing assistance with the 18F-FDG-directed surgery program.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
Gregg J. Chapman has equity in Navidea Biopharmaceuticals and is a paid consultant for Dynasil Corporation; however, he reports no conflicts of interest with regards to the conduct of this study.
Edward W. Martin, Jr. has equity in Actis, Ltd and Navidea Biopharmaceuticals; however, he reports no conflicts of interest with regards to the conduct of this study.
All the other authors declare that they have no competing interests to report.
Authors’ contributions
SPP was responsible for the overall study design, data collection, data analysis and interpretation, writing of all drafts of the manuscript, and has approved the final version of the submitted manuscript. GJC was involved in study design, data interpretation, writing portions of the manuscript, and has approved the final version of the submitted manuscript. DAM was involved in study design, data collection, data analysis and interpretation, writing portions of the manuscript, and has approved the final version of the submitted manuscript. RL was involved in study design, data interpretation, writing portions of the manuscript, and has approved the final version of the submitted manuscript. EWM was involved in study design, critiquing drafts of the manuscript, and has approved the final version of the submitted manuscript. NCH was involved in study design, data interpretation, writing portions of the manuscript, and has approved the final version of the submitted manuscript.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Povoski, S.P., Chapman, G.J., Murrey, D.A. et al. Intraoperative detection of 18F-FDG-avid tissue sites using the increased probe counting efficiency of the K-alpha probe design and variance-based statistical analysis with the three-sigma criteria. BMC Cancer 13, 98 (2013). https://doi.org/10.1186/1471-2407-13-98
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2407-13-98