Abstract
Background
Adjuvant chemotherapy for stage III colon cancer is internationally accepted as standard treatment with established efficacy. Several oral fluorouracil (5-FU) derivatives with different properties are available in Japan, but which drug is the most appropriate for each patient has not been established. Although efficacy prediction of 5-FU derivatives using expression of 5-FU activation/metabolism enzymes in tumors has been studied, it has not been clinically applied.
Methods/design
The B-CAST study is a multicenter, prospective cohort study aimed to identify the patients who benefit from adjuvant chemotherapy with each 5-FU regimen, through evaluating the relationship between tumor biomarker expression and treatment outcome. The frozen tumor specimens of patients with stage III colon cancer who receives postoperative adjuvant chemotherapy are examined. Protein expression of thymidine phosphorylase (TP), dihydropyrimidine dehydrogenase (DPD), epidermal growth factor receptor (EGFR), and vascular endothelial growth factor (VEGF) are evaluated using enzyme-linked immunosorbent assay (ELISA). mRNA expression of TP, DPD, thymidylate synthase (TS) and orotate phosphoribosyl transferase (OPRT) are evaluated using reverse transcription polymerase chain reaction (RT-PCR). The patients’ clinical data reviewed are as follow: demographic and pathological characteristics, regimen, drug doses and treatment duration of adjuvant therapy, types and severity of adverse events, disease free survival, relapse free survival and overall survival. Then, relationships among the protein/mRNA expression, clinicopathological characteristics and the treatment outcomes are analyzed for each 5-FU derivative.
Discussion
A total of 2,128 patients from the 217 institutions were enrolled between April 2009 and March 2012. The B-CAST study demonstrated that large-scale, multicenter translational research using frozen samples was feasible when the sample shipment and Web-based data collection were well organized. The results of the study will identify the predictors of benefit from each 5-FU derivative, and will contribute to establish the “personalized therapy” in adjuvant chemotherapy for colon cancer.
Trial registration
ClinicalTrials.gov: NCT00918827, UMIN Clinical Trials Registry (UMIN-CTR) UMIN000002013
Similar content being viewed by others
Background
Colorectal cancer (CRC) is the second most common cancer and the third most fatal cancer in Japan. In particular, colon cancer has been increasing in recent years [1, 2]. Postoperative adjuvant chemotherapy for patients with stage III colon cancer is internationally accepted as a standard care to improve survival, and there are several options as treatment regimens. The Guidelines 2010 for the Treatment of Colorectal Cancer published by the Japanese Society for Cancer of the Colon and Rectum (JSCCR) [3] recommend four regimens as adjuvant therapy for stage III disease: 5-fluorouracil (5-FU)/leucovorin (LV), UFT/LV, capecitabine, 5-FU/LV (or capecitabine) + oxaliplatin. In addition, S-1 [4] or S-1 + oxaliplatin [5] are used on an experimental basis.
In Japan, oral 5-FU derivatives (5-FUs) have been preferred because of their convenience, leading to the development of several oral 5-FUs with different properties. UFT (Taiho Pharmaceutical Co., Ltd., Tokyo, Japan) is a combination drug of tegafur, a prodrug of 5-FU, and uracil, an inhibitor of dihydropyrimidine dehydrogenase (DPD) that is a degradative enzyme for 5-FU, in a molar ratio of 4:1 [6]. Concomitant use of folic acid derivative LV with UFT promotes stabilising the ternary complex and augmenting the inhibition of thymidylate synthase (TS) by 5-FU. Capecitabine (Chugai Pharmaceutical Co., Ltd., Tokyo, Japan) is designed to be specifically transformed from 5’-deoxy-5-fluorouridine (5’-DFUR) to 5-FU by thymidine phosphorylase (TP), which is in higher concentrations in tumor tissues than in normal tissues, with the aim of reducing the gastrointestinal and hematological toxicities of 5-FU [7]. S-1 (Taiho Pharmaceutical Co., Ltd.) combines tegafur, gimeracil and oteracil, in a molar ratio of 1:0.4:1. Gimeracil, a DPD inhibitor, is about 200-fold more potent than uracil. Oteracil inhibits the conversion of 5-FU to active metabolites in the gastrointestinal tract, resulting in reduction of gastrointestinal toxicity of 5-FU [8]. These preparations have different profiles of adverse event (AE). UFT is reported to be often associated with liver dysfunction in Japanese patients [4, 9]. A most common AE of capecitabine is hand-foot syndrome (HFS) [10]. S-1 often causes mild hematological toxicity and fatigue [4].
Multiple options are available for adjuvant therapy with 5-FUs for colon cancer, however, which drug is the most appropriate for each patient has not been established. The efficacy of 5-FUs is reported to be related to the expression of enzymes that correlate to 5-FU activation/metabolism in tumors and/or blood. Ichikawa et al. [11] reported that of 37 patients with metastatic CRC, UFT/LV was useful in those with low tumor mRNA expression of TS, DPD, and orotate phosphoribosyl transferase (OPRT). Nishimura et al. [12] disclosed that from analysis of 88 patients with Dukes B/C CRC who received 5’-DFUR therapy, those with high tumor TP protein expression in enzyme-linked immunosorbent assay (ELISA) showed better prognosis. On the other hand, TP is also known as a platelet-delivered endothelial cell growth factor, and it has been reported that metastatic CRC with high tumor mRNA levels of TP had poor prognosis [13].
Prediction of efficacy in 5-FUs treatment has been studied [14] but has not been clinically applied yet, because of no large prospective studies or because of difficulty in measurement as point of versatility and cost. “Personalized therapy”, which means to select the best option from different treatments based on individual patients’ factors, could improve not only the efficacy but also the safety, patient’s quality of life and cost-effectiveness in adjuvant therapy for colon cancer.
We therefore conducted a prospective cohort study named the B-CAST study (Biomarker-cohort study of adjuvant chemotherapy for stage III colon cancer), to identify the patients who benefit from adjuvant chemotherapy with each 5-FU derivative, through evaluating the relationships between tumor biomarker expression and treatment outcome.
Methods/design
The design of study
This study is a multicenter, prospective cohort study evaluating the relationships between tumor biomarker expression and treatment outcome of adjuvant chemotherapy in patients with stage III colon cancer. In this paper, the disease stage is described by the 7th UICC–TNM classification system.
Six candidate biomarkers are selected for this study: TP, DPD, TS and OPRT as key enzymes correlating to 5-FU activation/metabolism [11–14], and epidermal growth factor receptor (EGFR) and vascular endothelial growth factor (VEGF) as promising markers which are correlated to tumor proliferation and/or metastasis of CRC [15–18] and which are already in clinical use as targets of the molecular-target drug.
The frozen tumor samples from surgical specimen of patients with stage III colon cancer who receives postoperative adjuvant chemotherapy are examined. Protein expression of TP, DPD, EGFR and VEGF are evaluated using ELISA, and mRNA expression of TP, DPD, TS and OPRT are evaluated using reverse transcription polymerase chain reaction (RT-PCR).
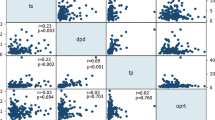
The patients’ clinical data including demographic and pathological characteristics [19], regimens, drug doses and treatment duration of adjuvant chemotherapy, and treatment outcomes including AEs and survivals are collected (Tables 1, 2). Then, relationships among the protein/mRNA expression and the patients’ clinical data are analyzed (Figure 1). The primary endpoint is disease free survival (DFS), and secondary endpoints are relapse free survival (RFS), overall survival (OS), and incidence and severity of AEs.
The registration period is from April 2009 to March 2012, and the follow-up period is 5 years from the enrollment of the last subject.
Selection of candidate patients
Candidate patients are asked to give informed consent prior to surgery (Figure 2). Main inclusion criteria are as follows:
-
1)
Clinical stage II or III colon cancer
-
2)
Pathologically confirmed adenocarcinoma
-
3)
Curatively resectable
-
4)
No prior chemotherapy or radiotherapy for colon cancer
-
5)
Adequate general condition for postoperative adjuvant chemotherapy
-
6)
No other active malignancies (i.e. diagnosed within 5 years)
-
7)
No contraindication to 5-FUs
Patients who have given written informed consent are tentatively enrolled at the Foundation for Biomedical Research and Innovation, Translational Research Informatics Center (FBRI-TRI) using a Web-based enrollment system and a “sample number” is issued. A list of collected information at tentative enrollment is shown in Table 1.
Collection/storage/submission of tumor samples
Two 5 mm-cubed tissue blocks are taken from the land wall of the primary tumor immediately after surgery, and separately put in 2 predefined tubes. One for protein analysis is put in the blank tube and placed in a freezer. The other for mRNA analysis is immersed in RNAlater® (Life Technologies Japan Ltd., Tokyo, Japan) in the tube. After rapped with a small air-cushion bag, the tube is placed in a freezer such that the tissue block is gradually moistened with RNAlater® before freezing.
In a preliminary experiment using xenografts, there was no difference in the sample stabilities between the samples stored in a deep freezer (−80°C) and those stored in a freezer for general use (usually at −20°C) for up to 8 weeks (data not shown). From these observations, samples are allowed to be stored frozen in a freezer for general use for up to 8 weeks.
Each tube is labeled with the “sample number” issued at the tentative enrollment. The samples are collected by SRL Medisearch Co., Ltd. (SRLM) (Tokyo, Japan), a commercial laboratory company with a nationwide network. The collected samples are temporarily stored in a −80°C depository at SRLM, and then sent to the measurement facility (Kamakura Research Laboratories, Chugai Pharmaceutical Co., Ltd., Kanagawa, Japan).
Final enrollment
After a pathological examination is completed, patients who meet all of the following criteria are finally enrolled in the study (Figure 2):
-
1)
Pathologically confirmed stage III colon cancer
-
2)
Judged to be curatively resected (R0 resection)
-
3)
Agreed to receive postoperative adjuvant chemotherapy containing 5-FUs
A list of collected information at final enrollment is shown in Table 1. A “final registration number” is issued for each patient after confirming eligibility at FBRI-TRI.
Measurement of biomarkers
The samples from patients who are eligible for “final enrollment” are examined in the measurement facility in accordance with the Standard Operating Procedures. The samples from ineligible patients (i.e. pathological stage II) are discarded without being examined.
Measurement of protein expression
The tumor block is wholly homogenized using an analysis buffer and then centrifuged. Using the resulting supernatant, the protein expressions of TP, DPD, EGFR, and VEGF are evaluated by ELISA. For TP and DPD, the methods established by Chugai Pharmaceutical Co., Ltd. are used [20, 21]. For EGFR and VEGF, Human EGFR Duo Set ELISA kit and Human VEGF Quantikine ELISA Kit (R&D Systems Inc., Minneapolis, MN, USA) are used, respectively. All measurements are performed in duplicate, and the mean is used for analyses.
Measurement of mRNA expression
The tumor block is wholly homogenized using an analysis buffer. The total RNA is extracted from the homogenate using Sepasol®-RNA I Super G (Nacalai Tesque Inc., Kyoto, Japan) and precipitated with ethanol. The RNA quality is determined using Experion™ Automated Electrophoresis Station (Bio-Rad Laboratories, Inc., Hercules, CA, USA) and assessed based on the RNA Quality Indicator which is calculated from the observed and reference values at 18S and 28S peaks using Experion software (Bio-Rad Laboratories, Inc.). If the RNA quality is adequate, cDNA is synthesized using 5 μg of total RNA.
The mRNA expressions of TP, DPD, TS, and OPRT are evaluated by real-time PCR (LightCycler®480 Real-Time PCR System, Roche Diagnostics, Mannheim, Germany) with commercially available primer/probe sets (Nihon Gene Research Laboratories Inc., Sendai, Japan). Using glyceraldehyde-3-phosphate dehydrogenase (GAPDH) as the internal standard, the mRNA expression of the target gene is quantified. All measurements are performed in duplicate, and the mean will be used for analyses.
After all eligible samples are examined, the measurement results are submitted to FBRI-TRI data center. They are not reported to the attending physician, so that the subsequent treatment is not affected by the measurement results.
Treatment
Adjuvant chemotherapy
The study protocol does not define treatment regimens and schedule of hospital visits during chemotherapy. When the chemotherapy is finished, the following information regarding adjuvant chemotherapy is reported using a Web-based case report system: treatment regimen, dose of each drug, duration of treatment, relative dose intensity, and AEs. Details of collected information are shown in Table 2.
Surveillance for relapse
Surveillance for relapse in accordance with a schedule described in the JSCCR Guidelines is recommended [3] (Figure 3). Web-based outcome reporting is conducted 3 times, at 1, 3, and 5 years from the last registration (Figure 2). Cases of relapse and/or other malignancy are required to be reported with the date of confirmation and the site. Cases of death are required to be reported with the date and cause of death. For surviving patients, the date of the last confirmation of survival is required to be reported.
Treatment outcomes
Efficacy
DFS (primary endpoint) is defined as the time to relapse, other malignancies or death, whichever comes first. Patients alive and free of relapse or other malignancies are censored at time of the last follow-up. RFS is defined as the time to relapse or death. Patients alive and free of relapse are censored at time of last follow-up. OS is defined as the time to death. The intervals are calculated from the date of surgery.
Safety
The types and severities of AEs are evaluated according to the National Cancer Institute Common Terminology Criteria for Adverse Events version 3.0 (National Cancer Institute, Bethesda, MD, USA). HFS is assessed in accordance with the assessment criteria for HFS [22]. The most severe grade of each AE during whole treatment period is reported. The following AEs are required to be reported as “priority survey items”: leukocytopenia, neutropenia, HFS, diarrhea, vomiting, anorexia/nausea, increased aspartate aminotransferase (AST), increased alanine aminotransferase (ALT), and hyperbilirubinemia. Other AEs should be reported when the severity is grade 3 or higher.
Statistical matters
Target sample size calculation
As no studies evaluating the relationship between tumor expression of 5-FU activation/metabolism enzymes and prognosis numerically through the hazard ratio (HR), the necessary sample size was calculated through simulation using previous data on tumor TP.
In 6,731 Japanese colon cancer patients, mean logarithmic tumor TP (log TP) determined by ELISA was 4.31 with a standard deviation (SD) of 0.61, with a normal distribution (unpublished data). We thus assumed that log TP in the present study population follows a normal distribution with a similar mean and SD. The protocol preparation committee concluded that capecitabine, the efficacy of which may be affected by tumor TP [12], is recommended to be chosen when increased tumor TP produces a 7% increase in 5-year DFS rate. In the present study, therefore, the HR of 1-unit decrease in log TP for DFS was estimated to be 1.3 (equivalent to a 7% decrease in 5-year DFS rate).
On the assumption that DFS would follow an exponential distribution with a 5-year DFS rate of 70% [3, 23, 24] in this study with a registration period of 2 years*, a follow-up period of 5 years, and patient enrollment following a uniform distribution over 2 years* from the start of the study, a proportional hazard model with log TP as the covariate and log HR as the true regression coefficient was applied to produce simulated data with 1,000 iterations for each given HR and sample size. The proportional hazard model was fitted to these simulated data to test the significance of the regression coefficient at a two-sided significance level of α=0.05 based on the null hypothesis that “tumor TP is not correlated with DFS.” Statistical Analysis System version 9.1 (SAS institute Inc., Cary, NC, USA) was used for simulation.
The simulation results showed that a sample size of 950 with a HR of 1.3 would provide a power of 80% or more. With an estimated dropout rate of approximately 5%, the target sample size of 1,000 was estimated to evaluate the relationship between tumor TP and DFS in patients treated with capecitabine. Since three regimens (capecitabine, UFT/LV, and intravenous 5-FU/LV, respectively) were used, the total target sample size of 3,000 was needed to ensure that similar analyses would be performed for each of the three regimens.
*: Because of the delayed cumulative pace of patient enrollment, the registration period was extended in February 2011, from 2 years to 3 years.
Analysis plan
In each treatment group, the Cox proportional hazard model with covariate as tumor TP is primarily performed to evaluate significant relationship with DFS. Patients receiving oxaliplatin containing regimens will be evaluated separately from those with 5-FU derivatives alone. At 3 years and 5 years after the enrollment of the last subject, an interim and final analysis is conducted using the Cox proportional hazard model as mentioned above, respectively. The abovementioned analyses for tumor TP, the primary variables, are also performed for other measured biomarkers. Since this is an observational study (not an experimental study), no adjustment for multiplicity is applied.
Secondarily, RFS and OS are also studied in the same manner as DFS. The relationships between expression of biomarkers and AEs in each treatment group are also evaluated by applying a logistic regression model.
And as exprolatory analyses, univariate and multivariate relationships among survivals of each treatment group, expression of biomarkers and patient characteristics will be evaluated using the Cox proportional hazard model.
Ethical matters
This study is conducted in accordance with the “Declaration of Helsinki” and “Ethical Guidelines for Clinical Research”, and has been approved by the Institutional Review Boards of each participating institute. Written informed consent is obtained from all patients before enrollment.
Discussion
The B-CAST study is conducted to prospectively evaluate the relationships between tumor biomarker expression and treatment outcome in large sample size of stage III colon cancer patients who received adjuvant chemotherapy, in order to identify the patients who benefit from each 5-FU derivative. A total of 2,128 patients from the 217 institutions were finally enrolled between April 2009 and March 2012. Follow-up will be completed in March 2017.
In this study, frozen tumor samples are used to measure the biomarkers for better quality and quantity of protein/mRNA than those of paraffin-embedded specimens. And in considering of the practical versatility, homogenates of whole specimens of tumor mass, not micro-dissected cancer tissues, are used. The most translational research has conventionally been conducted as mono-institutional research because of difficulty in sample shipment and storage, especially when using frozen samples, resulting in underpowered studies with a small sample size. The B-CAST study demonstrated that large-scale, multicenter translational research using frozen samples was feasible when the sample shipment and Web-based data collection were well organized.
The results of the study will provide the large database of tumor biomarker expression of colon cancer, and will identify the predictors of benefit from each 5-FU derivative. These observations will contribute to establish the “personalized therapy” in adjuvant chemotherapy for colon cancer.
Abbreviations
- CRC:
-
Colorectal Cancer
- JSCCR:
-
Japanese Society for Cancer of the Colon and Rectum
- 5-FU:
-
5-fluorouracil
- LV:
-
Leucovorin
- 5-FUs:
-
5-FU derivatives
- DPD:
-
Dihydropyrimidine Dehydrogenase
- TS:
-
Thymidylate Synthase
- 5’-DFUR:
-
5’-Deoxy-5-Fluorouridine
- TP:
-
Thymidine Phosphorylase
- AE:
-
Adverse Event
- HFS:
-
Hand-Foot Syndrome
- OPRT:
-
Orotate Phosphoribosyl Transferase
- ELISA:
-
Enzyme-Linked Immunosorbent Assay
- EGFR:
-
Epidermal Growth Factor Receptor
- VEGF:
-
Vascular Endothelial Growth Factor
- RT-PCR:
-
Reverse Transcription Polymerase Chain Reaction
- DFS:
-
Disease Free Survival
- RFS:
-
Relapse Free Survival
- OS:
-
Overall Survival
- FBRI-TRI:
-
Foundation for Biomedical Research and Innovation, Translational Research Informatics Center
- SRLM:
-
SRL Medisearch Co., Ltd.
- GAPDH:
-
Glyceraldehyde-3-Phosphate Dehydrogenase
- AST:
-
Aspartate Aminotransferase
- ALT:
-
Alanine Aminotransferase
- HR:
-
Hazard Ratio
- Log TP:
-
Logarithmic tumor TP
- SD:
-
Standard Deviation
References
Cancer statistics in Japan. 2010, http://www.fpcr.or.jp/publication/statistics.html,
Kotake K, Honjo S, Sugihara K, Kato T, Kodaira S, Takahashi T, Yasutomi M, Muto T, Koyama Y: Changes in colorectal cancer during a 20-year period: an extended report from the multi-institutional registry of large bowel cancer, Japan. Dis Colon Rectum. 2003, 46: 32-43.
Watanabe T, Itabashi M, Shimada Y, Tanaka S, Ito Y, Ajioka Y, Hamaguchi T, Hyodo I, Igarashi M, Ishida H, Ishiguro M, Kanemitsu Y, Kokudo N, Muro K, Ochiai A, Oguchi M, Ohkura Y, Saito Y, Sakai Y, Ueno H, Yoshino T, Fujimori T, Koinuma N, Morita T, Nishimura G, Sakata Y, Takahashi K, Takiuchi H, Tsuruta O, Yamaguchi T, Yoshida M, Yamaguchi N, Kotake K, Sugihara K, Japanese Society for Cancer of the Colon and Rectum: Japanese society for cancer of the colon and rectum (JSCCR) guidelines 2010 for the treatment of colorectal cancer. Int J Clin Oncol. 2012, 17: 1-29.
Mochizuki I, Takiuchi H, Ikejiri K, Nakamoto Y, Kinugasa Y, Takagane A, Endo T, Shinozaki H, Takii Y, Takahashi Y, Mochizuki H, Kotake K, Kameoka S, Takahashi K, Watanabe T, Watanabe M, Boku N, Tomita N, Matsubara Y, Sugihara K: Safety of UFT/LV and S-1 as adjuvant therapy for stage III colon cancer in phase III trial: ACTS-CC trial. Brit J Cancer. 2012, 106: 1268-1273.
Takiuchi H, Tomita N, Boku N, Watanabe T, Kotake K, Itabashi M, Takahashi K, Baba H, Morita S, Sugihara K: Preplanned initial safety analysis of ACTS-CC 02 trial: a large randomized phase III trial of SOX versus UFT/LV as adjuvant chemotherapy for high-risk stage III colon cancer [abstract]. J Clin Oncol. 2012, 30 (suppl-Feb 1): 572-
Fujii S, Kitano S, Ikenaka K, Shirasaka T: Effect of coadministration of uracil or cytosine on the anti-tumor activity of clinical doses of 1-(2-tetrahydrofuryl)-5-fluorouracil and level of 5-fluorouracil in rodents. Gann. 1979, 70: 209-214.
Miwa M, Ura M, Nishida M, Sawada N, Ishikawa T, Mori K, Shimma N, Umeda I, Ishitsuka H: Design of a novel oral fluoropyrimidine carbamate, capecitabine, which generates 5-fluorouracil selectively in tumours by enzymes concentrated in human liver and cancer tissue. Eur J Cancer. 1998, 34: 1274-1281.
Shirasaka T, Shimamato Y, Ohshimo H, Yamaguchi M, Kato T, Yonekura K, Fukushima M: Development of a novel form of an oral 5-fluorouracil derivative (S-1) directed to the Potentiation of the tumor selective cytotoxicity of 5-fluorouracil by two biochemical modulators. Anticancer Drugs. 1996, 7: 548-557.
Shimada Y, Hamaguchi T, Moriya Y, Saito N, Kanemitsu Y, Takiguchi N, Ohue M, Kato T, Takii Y, Sato T, Tomita N, Yamaguchi S, Akaike M, Mishima H, Kubo Y, Mizusawa J, Nakamura K, Fukuda H: Randomized phase III study of adjuvant chemotherapy with oral uracil and tegafur plus leucovorin versus intravenous fluorouracil and levofolinate in patients with stage III colon cancer: final results of Japan clinical oncology group study (JCOG0205) [abstract]. J Clin Oncol. 2012, 30 (suppl-May 20): 352-
Twelves C, Wong A, Nowacki MP, Abt M, Burris H, Carrato A, Cassidy J, Cervantes A, Fagerberg J, Georgoulias V, Husseini F, Jodrell D, Koralewski P, Kröning H, Maroun J, Marschner N, McKendrick J, Pawlicki M, Rosso R, Schüller J, Seitz JF, Stabuc B, Tujakowski J, Van Hazel G, Zaluski J, Scheithauer W: Capecitabine as adjuvant treatment for stage III colon cancer. N Eng J Med. 2005, 352: 2696-2704.
Ichikawa W, Uetake H, Shirota Y, Yamada H, Takahashi T, Nihei Z, Sugihara K, Sasaki Y, Hirayama R: Both gene expression for orotate phosphoribosyltransferase and its ratio to dihydropyrimidine dehydrogenase influence outcome following fluoropyrimidine-based chemotherapy for metastatic colorectal cancer. Br J Cancer. 2003, 89: 1486-1492.
Nishimura G, Terada I, Kobayashi T, Ninomiya I, Kitagawa H, Fushida S, Fujimura T, Kayahara M, Shimizu K, Ohta T, Miwa K: Thymidine phosphorylase and dihydropyrimidine dehydrogenase levels in primary colorectal cancer show a relationship to clinical effects of 5'-deoxy-5-fluorouridine as adjuvant chemotherapy. Oncol Rep. 2002, 9: 479-482.
Metzger R, Danenberg K, Leichman CG, Salonga D, Schwartz EL, Wadler S, Lenz HJ, Groshen S, Leichman L, Danenberg PV: High basal level gene expression of thymidine phosphorylase (platelet-derived endothelial cell growth factor) in colorectal tumors is associated with nonresponse to 5-fluorouracil. Clin Cancer Res. 1998, 4: 2371-2376.
Koopman M, Venderbosch S, Nagtegaal ID, van Krieken JH, Punt CJ: A review on the use of molecular markers of cytotoxic therapy for colorectal cancer, what have we learned?. Eur J Cancer. 2009, 45: 1935-1949.
Lockhart AC, Berlin JD: The epidermal growth factor receptor as a target for colorectal cancer therapy. Semin Oncol. 2005, 32: 52-60.
Mayer A, Takimoto M, Fritz E, Schellander G, Kofler K, Ludwig H: The prognostic significance of proliferating cell nuclear antigen, epidermal growth factor receptor, and mdr gene expression in colorectal cancer. Cancer. 1993, 71: 2454-2460.
Lee JC, Chow NH, Wang ST, Huangd SM: Prognostic value of vascular endothelial growth factor expression in colorectal cancer patients. Eur J Cancer. 2000, 36: 748-753.
Takahashi Y, Kitadai Y, Bucana CD, Cleary KR, Ellis LM: Expression of vascular endothelial growth factor and its receptor, KDR, correlates with vascularity, metastasis, and proliferation of human colon cancer. Cancer Res. 1995, 55: 3964-3968.
The Japanese Society for Cancer of the Colon and Rectum: Japanese classification of colorectal carcinoma –second English edition-. 2009, Tokyo: Kanehara & Co., Ltd
Nishida M, Hino A, Mori K, Matsumoto T, Yoshikubo T, Ishitsuka H: Preparation of anti-human thymidine phosphorylase monoclonal antibodies useful for detecting the enzyme levels in tumor tissues. Biol Pharm Bul. 1996, 19: 1407-1411.
Mori K, Hasegawa M, Nishida M, Toma H, Fukuda M, Kubota T, Nagasue N, Yamana H, Hirakawa-YS Chung K, Ikeda T, Takasaki K, Oka M, Kameyama M, Toi M, Fujii H, Kitamura M, Murai M, Sasaki H, Ozono S, Makuuchi H, Shimada Y, Onishi Y, Aoyagi S, Mizutani K, Ogawa M, Nakao A, Kinoshita H, Tono T, Imamoto H, Nakashima Y, Manabe T: Expression levels of thymidine phosphorylase and dihydropyrimidine dehydrogenase in various human tumor tissues. Int J Oncol. 2000, 17: 33-38.
Blum JL, Jones SE, Buzdar AU, LoRusso PM, Kuter I, Vogel C, Osterwalder B, Burger HU, Brown CS, Griffin T: Multicenter phase II study of capecitabine in paclitaxel-refractory metastatic breast cancer. J Clin Oncol. 1999, 17: 485-493.
Hamaguchi T, Shirao K, Moriya Y, Yoshida S, Kodaira S, Ohashi Y: Final results of randomized trials by the national surgical adjuvant study of colorectal cancer (NSAS-CC). Cancer Chemother Pharmacol. 2011, 67: 587-596.
Kato T, Ohashi Y, Nakazato H, Koike A, Saji S, Suzuki H, Takagi H, Nimura Y, Hasumi A, Baba S, Manabe T, Maruta M, Miura K, Yamaguchi A: Efficacy of oral UFT as adjuvant chemotherapy to curative resection of colorectal cancer: multicenter prospective randomized trial. Langenbecks Arch Surg. 2002, 386: 575-581.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2407/13/149/prepub
Acknowledgement
We are grateful to all of the patients and the co-investigators for their cooperation in B-CAST study. The authors also thank the following additional investigators for their contributions to this study: Koichi Yamashiro, Kenichi Kono and Chikako Harada in data management; Hideo Nishimura in sample anonymization; Hiroyuki Ueshima and Ayano Hosoda as the project office staff; Yoshiharu Sugawara as the coordinator of SRL Medisearch Co., Ltd.; all laboratory staff participated in sample measurement; and Masanori Fukushima, M.D., Ph.D., as a director of FBRI-TRI.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interest
B-CAST study [TRICC0807] is conducted as a part of joint research of Tokyo Medical and Dental University and the Foundation for Biomedical Research and Innovation (FBRI) on construction of foundation for large-scale translational research, with funding from FBRI. FRBI is financed by manufacturers and distributors of the drugs, but there are no competing interest between these companies and the investigators that require disclosure in connection with the study.
MI has received consulting fees from Taiho Pharmaceutical Co. Ltd., Bristol-Myers Squibb and Merck Serono Co. Ltd; honoraria from Taiho, Chugai Pharmaceutical Co. Ltd., and Yakult Honsha Co. Ltd.
K.Kotake has received consulting fees from Taiho and Chugai; honoraria from Taiho, Chugai, Bristol-Myers, Merck Serono, Yakult Honsha, Otsuka, Daiichi Sankyo Co. Ltd., and MSD K. K.
GN has received honoraria from Chugai.
NT and WI have received honoraria from Taiho and Chugai.
KT has received honoraria from Takeda Pharmaceutical Co. Ltd.
TW has received honoraria and research funding from Taiho, Chugai, Daiichi Sankyo, Yakult Honsha, Bristol-Myers, Merck Serono, and Takeda.
MM has received honoraria from Taiho.
YK has received honoraria from Chugai and Sanofi-Aventis K.K.; research funding from Chugai.
IH has received honoraria and research funding from Taiho, Chugai, and Daiichi Sankyo.
TF, and K. Kondo, AK, MK, MO, and KM have no competing interest.
KS has received consultant fees, research funding and honoraria from Taiho, Chugai, Takeda, Yakult Honsha, Daiichi Sankyo, Bristol-Myers, Merck Serono, and Pfizer Co. Ltd.
Authors’ contributions
MI, as a task manager, participated in entire coordinating of the study, design and writing of the protocol, data collection, data analysis, data interpretation, and writing of the manuscript. K. Kotake, GN, NT, WI and KS, as protocol preparation committee, participated in all phases of this study, including design and writing of the protocol, data collection, data analysis, data interpretation, and preparation of the manuscript. KT, TW, TF, K. Kondo, MM, YK, AK, MK, MO, and IH, as steering committee, participated in all phases of this study, including evaluation of the protocol, data collection, data analysis, data interpretation, and preparation of the manuscript. KM, as a chief of statistical analysis, participated in statistical setting of study design and data analysis. All authors reviewed and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Ishiguro, M., Kotake, K., Nishimura, G. et al. Study protocol of the B-CAST study: a multicenter, prospective cohort study investigating the tumor biomarkers in adjuvant chemotherapy for stage III colon cancer. BMC Cancer 13, 149 (2013). https://doi.org/10.1186/1471-2407-13-149
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2407-13-149