Abstract
Background
In sub-Saharan Africa, few services specifically address the needs of women in the first year after childbirth. By assessing the health status of women in this period, key interventions to improve maternal health could be identified. There is an underutilised opportunity to include these interventions within the package of services provided for woman-child pairs attending child-health clinics.
Methods
This needs assessment entailed a cross-sectional survey with 500 women attending a child-health clinic at the provincial hospital in Mombasa, Kenya. A structured questionnaire, clinical examination, and collection of blood, urine, cervical swabs and Pap smear were done. Women's health care needs were compared between the early (four weeks to two months after childbirth), middle (two to six months) and late periods (six to twelve months) since childbirth.
Results
More than one third of women had an unmet need for contraception (39%, 187/475). Compared with other time intervals, women in the late period had more general health symptoms such as abdominal pain, fever and depression, but fewer urinary or breast problems. Over 50% of women in each period had anaemia (Hb <11 g/l; 265/489), with even higher levels of anaemia in those who had a caesarean section or had not received iron supplementation during pregnancy. Bacterial vaginosis was present in 32% (141/447) of women, while 1% (5/495) had syphilis, 8% (35/454) Trichomonas vaginalis and 11% (54/496) HIV infection.
Conclusion
Throughout the first year after childbirth, women had high levels of morbidity. Interface with health workers at child health clinics should be used for treatment of anaemia, screening and treatment of reproductive tract infections, and provision of family planning counselling and contraception. Providing these services during visits to child health clinics, which have high coverage both early and late in the year after childbirth, could make an important contribution towards improving women's health.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
In recent years, maternal health services in resource-constrained settings have increasingly focused on the importance of skilled birth attendants and the management of intrapartum complications [1]. Also, much efforts have been made to rationalise the package of services for antenatal care [2, 3]. Antenatal care coverage remains high in most of Africa and the proportion of births which occur within medical services is steadily increasing [4, 5]. By contrast however, few resources are allocated to delivering specific services for women in the year after childbirth. The essential package of postpartum services is poorly defined, and the optimum structure and number of visits for these services remains uncertain [6]. Given weaknesses in the current model for health services for women after childbirth, it is worthwhile to examine alternative configurations of service delivery. Most notably, contact with health services in the year after childbirth presents a vital opportunity to assist women return to full health, and to prevent sexual and reproductive health problems in this period.
The postpartum period, defined by WHO as beginning one hour after delivery of the placenta and continuing until six weeks after childbirth [7], is a period of substantial transition as women move from pregnancy and childbirth back to reproductive potential. Many studies in Africa refer to the postpartum period in more general terms, even including up to two years after childbirth [8–12]. Some definitions of maternal mortality include late maternal deaths (deaths between six weeks and one year after childbirth) [13]. This acknowledges the fact that some physiological effects of pregnancy still occur in this period and that the health of women at this time warrants specific attention [14, 15]. The pre-pregnant state has not yet completely returned within six weeks of childbirth, lactation usually continues throughout the first year, often the menstrual cycle has not yet normalized and sexual activity may not have resumed. Further, with screening, detection and treatment of diseases at several time points in the year after giving birth, the safety of future pregnancies could be improved, as well as offering the inherent benefits of improvements in women's overall health status.
Though in many settings over half of maternal deaths occur after childbirth [16, 17], data on the health of women during this time are sparse. Moreover, reports usually focus on life-treating obstetric complications such as postpartum haemorrhage with a relative neglect of important common morbidities [7, 18–20]. Thus, while several previous studies have highlighted the contribution of the postpartum period to maternal mortality, few have described the burden of more common chronic conditions such as anaemia and depression [21–23]. In addition, most recent studies among postpartum women in Kenya have concentrated on HIV-infected women [8, 10, 11], and additional information is required about the burden of disease in women without HIV infection, who constitute the majority in these settings.
This study describes acute and chronic morbidity in the year after childbirth, which can be considered as either: conditions associated with pregnancy and childbirth; diseases specific to the postpartum period (such as those related to breastfeeding or the return of reproductive potential); or as intercurrent illnesses (such as cervical neoplasia). Further, the study sets out how patterns of sexual behaviour and morbidity vary with the length of time since delivery. Identifying the needs of women in the year after childbirth would inform selection of essential interventions to secure the health of women during this period, tailored to their changing needs over this time course. Provision of these interventions for women bringing their child for health care could achieve high population coverage as child-health services have good uptake in most countries [24].
Methods
At Coast Provincial General Hospital in Mombasa, Kenya, 500 women attending an immunization and acute care paediatric clinic participated in a cross-sectional survey to describe the levels of maternal morbidity in the year after childbirth. The survey, held in 2006, also investigated the feasibility of providing HIV testing and counselling, and the levels of HIV-related disease in this population [25, 26]. Study activities formed part of a project to improve maternal health services in Coast Province Kenya. From 2002 to 2005 this project focused on strengthening antenatal and intrapartum services; however as it appeared that few women attended postpartum services and their needs were ill defined, this survey was planned to assess women's needs after childbirth and to define a service package that could be provided for women bringing their child for health care. The study was approved by the Kenyatta National Hospital Ethics and Research Committee.
The study population consisted of consecutive women who were older than 16 years, biological mothers of the child, and between four weeks and one year after childbirth.
After completion of the child-health visit, women were approached and invited to participate in the study. Those willing to participate gave written informed consent and were interviewed using a pre-tested structured questionnaire administered in Swahili, the local language.
Besides information on demographic characteristics, data were collected on access to sexual and reproductive health services; family planning needs and sexual health status. Women were screened for mild and major depression (using ICD-10 definitions [27]) and for harmful alcohol use with the AUDIT tool [28]. Thereafter study nurses did a clinical examination and collected blood, urine, a cervical swab and a Pap smear. Full details of test procedures and the sample size calculation are provided elsewhere [26]. Urine dipstick detected nitrites and leucocytes. Blood samples were used for malaria microscopy, RPR test for syphilis and serial rapid HIV testing. Trichomonas vaginalis and candida were detected in a wet mount, and Nugent's criteria used for diagnosing bacterial vaginosis. Participants were advised to return for test results and, if required, received treatment according to local guidelines. For conditions such as syphilis, malaria and severe anaemia, women with positive results were contacted and asked to return to the clinic immediately. All participants were offered HIV counselling and same-day testing; those testing positive were enrolled in an HIV care and treatment clinic at the study site.
Study measures and data analysis
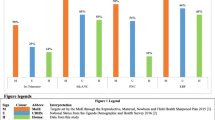
Data collected during interviews and laboratory investigations were double entered using Statistical Package for Social Science, version 11.5 (Chicago, USA). For analysis, women were divided into three groups according to the time period since childbirth: early (four weeks to two months), middle (two to six months) and late periods(six to twelve months). These categories were selected to be broadly consistent with the local child immunization schedule and the anticipated patterns of illness in women. Sexually-active women not using contraceptive methods were defined as having an unmet need for contraception. Lactational amenorrhea (exclusive breastfeeding and amenorrhea) was classified as a contraceptive method. Haemoglobin levels below 11 g/l were considered anaemia and a mean corpuscular volume below 81fl microcytic [29].
Intercooled Stata 8.0 (Stata Corporation, College Station, Texas, USA) was used to assess the distribution of sexual behaviour, contraceptive need, morbidity and other variables among women presenting in the early, middle and late periods. Also, the demographic and reproductive health characteristics of these three groups were compared to assess whether systematic differences exist which might be explained by differential health-seeking patterns. For example, we assessed whether poorer or multiparous women were less likely to attend visits in the late period. A chi-square test was used for analysis of binary variables and Mantel-Haenszel odds ratios were calculated. For continuous variables, a Student's t test and Wilcoxon's rank-sum test were used for comparing variables with a normal or non-normal distribution respectively. One way analysis of variance was used to compare means of continuous variables in each of the time periods.
Results
Characteristics of study population
Of 776 eligible women, 500 (64%) agreed to participate. Reasons given for declining participation included: lack of time (120), need for partner approval before participation (54), and having a child requiring urgent additional care [48]. Most study participants (82%, 395/484) had attended services for well children, such as immunization.
The majority of women were married 431/500 (86%), though only half had entered secondary or tertiary education (Table 1). On average, women were 25.5 years old (standard deviation [sd] = 4.5 years) and 40% were primiparous (195/490). Almost all had attended antenatal care at least once (480/500; 98%), though only 58% of these women had came for four or more antenatal visits (278/480), as recommended by WHO [30]. Four fifths of women (78%; 389/500) had delivered at a health facility. The caesarean section rate was 12% (60/493).
Participants had given birth a median 3.3 months (IQR = 1.9-6.1) ago. Mixed feeding of infants predominated in each time interval (92%; 454/494) and 96% (124/129) of women were still breastfeeding in the late period. Overall, the demographic characteristics of women in each study period were similar, with the exception of educational status, where women with lower educational levels appeared more likely to attend child-health clinics in the late period.
Psychosocial vulnerability
Household income was low, with 62% of women below 135$/month (310/500) and 14% less than 41$/month (69/500). Levels of physical and sexual violence are high in this population: more than a third had been coerced into sex (196/497), nearly 10% had been physically forced to have sex (40/491) and 19% had been pushed or hit by an intimate partner (95/499; Table 2). Since childbirth, 8% of women (38/499) had experienced sexual and/or physical violence (4 women reported both forms of violence).
Using ICD-10 definitions, 4% of women (18/500) had depression, with 2% of women currently having a major depressive episode (8/499; Table 3). The prevalence of depression diagnosed with DSM-IV criteria was slightly higher (5%; 24/499). Depression increased over the early, middle and late periods with both depression measures (OR = 2.0 per increase in time period, 95%CI = 1.0-3.7; P = 0.04 with ICD-10 and OR = 2.1, 95%CI = 1.2-3.8; P = 0.008 with DSM-IV). Less than 10% of women in each group reported having drunk alcohol during pregnancy or breastfeeding (38/477), 7 of whom reported having 5 or more drinks on 1 occasion in this time. A relatively small proportion of women used alcohol in a hazardous or harmful manner in the year preceding pregnancy (2%; 11/477).
Sexual behaviour and contraceptive use
Sexual activity increased with duration of time since childbirth, from 54% of women in the early period (71/131) to 80% (193/240) in the middle and 90% (116/129) in the last interval (P < 0.001). The large majority (86%, 296/344) of sexually-active women had not used condoms since childbirth (Table 2).
Though less than half said their most recent pregnancy was planned (46%; 231/500), in all study periods around a third of women had an unmet need for contraception (38% overall; 187/497). Of women using contraception, injectable methods were most commonly used (114 women), followed by oral contraception [19] and only three women were using an intra-uterine device.
Levels of contraception were incongruous with women's stated fertility intentions - only 3% of women desired more children within two years (13/499). Half in the early period expressed a desire for more children (50%; 65/130), while two thirds of women in the last group mentioned this (64%, 83/129; P = 0.02).
Self-reported health problems and health seeking behaviour
Only 13% of participants who had delivered in a health facility said they received information about warning signs of postpartum complications (48/376), and 23% were told to return for a postpartum check-up (87/381). About 10% of women had attended the check-up visit (58/500). More than a third had experienced health problems since childbirth (178/302; 37%), of whom 43% sought health care (71/164). At time of interview, 53% of women (257/483) said they felt unwell. The most frequent symptoms were abdominal pain, fever and foul-smelling vaginal discharge, all of which increased with duration of time since childbirth. Abdominal pain and vaginal discharge were strongly associated: women with pain were 4.3 times more likely to report vaginal discharge than other women (95%CI = 2.4-7.7; P < 0.001).
The vast majority believed they would benefit from a health worker visit to their home in the postpartum period (462/492; 94%). As an indicator of level of access to sexual and reproductive health services in the area, only 6% had previously been screened for cervical cancer (27/485).
Clinical morbidity
About one in twenty women was underweight (6%; 28/487), similar to the proportion obese (8%; 38/487). The mean haemoglobin was 10.5 g/l (sd = 1.8 g/l), with more than half the population anaemic (54%; 265/489) and 5% having severe anaemia (hb < 7 g/L; 26/489). Anaemia was less common in women who reported taking iron supplementation as prescribed during pregnancy (50%; 128/254) than women who took some iron (56%; 81/144), or did not take any supplementation (62%; 56/91; P = 0.05, chi-square test for trend). Higher levels of anaemia were also seen in underweight women (76%; 19/25), women who had a caesarean section (75%; 44/59) and those with an income below 41$/month (59%; 40/68). Few women had malaria parasitaemia, consistent with reported levels of bed net use - about two thirds reported they slept under a net the previous night (68%; 339/497).
Leukocyturia and positive nitrite status were most frequent in the early and middle periods. Reproductive tract infections were common, with an overall prevalence of bacterial vaginosis of 32% (141/447) and candida infection of 8% (36/454). Unlike these latter conditions, Trichomonas vaginalis was associated with genital symptoms. Of women reporting vaginal discharge symptoms, 14% had trichomoniasis (8/57), while 7% of women without discharge symptoms had trichomoniasis (27/393; P = 0.059). Compared with women in the early and mid period, a higher proportion in the late group had genital ulcers (4%; 4/109) or warts (3%, 3/109) and syphilis (2%, 2/128). Three quarters of participants reported having accessed HIV testing during pregnancy or childbirth (372/496) and 54/496 (11%) were HIV infected. Abnormal Pap smears, more common in the period closest to childbirth, identified a total of 4% (15/395) low-grade squamous intraepithelial lesions and 2% (8/395) high-grade squamous intraepithelial lesions.
Discussion
The study describes the burden and patterns of morbidity in the year after childbirth. Conditions associated with pregnancy, childbirth or breastfeeding predominate in the early and middle periods, while illnesses stemming from a return of sexual function and a transition to reproductive potential were commoner in the latter period. Broadly speaking, therefore, in the initial period after childbirth, interventions targeting breast health, the urinary tract and anaemia are most pertinent, while promotion of sexual health and prevention of unintended pregnancy have more importance in subsequent periods. It is, however, difficult to make a definitive distinction between needs of women in each time period and whether morbidities in these periods are related to pregnancy, return of reproductive potential or intercurrent illness. For example, throughout the first year, high levels of fever, abdominal pain and abnormal vaginal discharge make vigilance for sepsis important, a major cause of maternal mortality in Africa [16].
Over one third reported health problems and overall perceived health status was low. Among women in the early postpartum in Zambia, 84% reported at least one health problem [31]. A large study in India found 23% had health problems in the early postpartum [32] with even higher levels reported in Sri Lanka [33]. Taken together, it is thus clear that health problems are common among women after childbirth, but health care services are not commiserate with these levels of ill health.
Prevalence of treatable reproductive tract infections was high, similar to previous findings in Kenya [34]. The association between bacterial vaginosis and postpartum endometritis is potentially important in this population, but also its links with complications in a future pregnancy such as preterm delivery and preterm rupture of membranes [35–39]. STIs generally increased with each period since childbirth, concurring with the reported increase in sexual activity over time and the low condom use throughout. Low condom use, comparable to levels in a similar population in Zimbabwe [9], may be due to women perceiving themselves at low risk for pregnancy in the postpartum [40]. Absence of syphilis infection within two months of childbirth likely reflects the high coverage of antenatal care and quality of these services. As reported previously [25], acceptability of HIV testing was high among study participants and around four fifths received their results. Women with HIV infection have high morbidity and mortality in the year after childbirth [11] - for example, in our population, two thirds had anaemia and 20% reported current febrile symptoms [26]. These women require specific HIV care and treatment in addition to the needs of women described in this paper. Among the whole study population, levels of violence were remarkably high, though comparable with previous prevalence estimates in the general population in eastern Africa [41].
More than half of recent pregnancies were unplanned, and despite a desire to postpone pregnancy, more than a third of women had unmet need for contraception. Adequate birth spacing confers many benefits for women and their children and WHO recommends at least two to three years between pregnancies [42]. Women attending child health clinics need to be made aware of the benefits of adequate birth spacing, supported in their fertility choices, and to be offered contraception and dual protection. With adequate family planning services, uptake of hormonal contraception is high among postpartum women in Kenya [10], as much as 72% in a study [8].
Over half the women, and three quarters of some high-risk groups (such as those who had a caesarean section), had anaemia. Anaemia may be exacerbated by pregnancy and childbirth, and current WHO recommendations for populations with a severe prevalence of anaemia (>40%, as in this population) are that preventative and therapeutic iron supplementation should be given to all women of childbearing age and routinely in the postpartum [43]. Giving women attending child health clinics haematinic supplements, which are highly effective in reducing anaemia [44], may prevent anaemia in subsequent pregnancies.
That demographic characteristics of women in each of the three time periods were similar, suggests that health-seeking patterns were not strongly influenced by socio-demographic characteristics. These characteristics were, however, important in a study in rural Zambia [45]. In our population, differences between the study groups in experiences of sexual violence and depression indicates that psychosocial experiences may affect the timing and number of visits to child health centres.
However, perhaps women with severe postpartum depression in early period were less likely to bring their child for immunizations, spuriously lowering depression in this group. There is a biological explanation for higher rates of abnormal Pap smears shortly after childbirth. False positive smears can be caused by cervical inflammation related to the birth process, which regresses gradually over time [46, 47]. Overall, coverage of cervical cancer screening in Kenya remains notably low and this cancer the most common malignancy among women in the country [48].
This study has several limitations. While factors such as sexual activity, rate of caesarean section and prevalence of HIV are broadly comparable to those in urban areas of Kenya [49, 50], it is difficult to generalise the findings to rural areas, or to lower-level health facilities. In addition, women who do not attend child-health clinics, women whose child has died, or the substantial proportion who declined study participation may differ in important ways from the study population. Rates of morbidity are also likely to vary markedly between populations, in for example postpartum clinics and child-health clinics, or between community and hospital-based samples. Moreover, self-reported symptoms and behaviour incur recall and social desirability bias, though can be useful indicators of perceived health status.
Evaluation of morbidity in the whole year since childbirth makes it difficult to compare our findings with studies that included only women in the conventional six-week postpartum. However, including a longer period is a strength of this study, as it acknowledges the high risk women have for mortality between six weeks and a year after childbirth [14, 15]; is cognisant of the need for a continuum of care throughout this time; and presents evidence of the potential benefits of optimising the interface between women and health workers during child health visits to address the substantial burden of disease women have throughout this period.
Conclusion
Although most of the common problems women experienced were not life-threatening, they likely have marked influence on their wellbeing and health status in the long run. Most conditions could be addressed through provision of health promotion and preventive interventions, which is highly complementary to the intrapartum focus on acute severe problems.
The year after childbirth, an important part of women's lifecycle, is a neglected component of the continuum of care and support for women. Women in this period require interventions such as prevention and treatment of anaemia and reproductive tract infections, but also provision of family planning counselling and services, mental health services and distribution of condoms. Though many indicated they might benefit from home visits, this intervention requires additional study [51, 52]. Interface with women at child-health clinics, however, offers an opportunity to provide or facilitate entry to sexual and reproductive health services, and to encourage their long-term use.
The potential benefits of extending postpartum services beyond the conventional six-week period after childbirth may necessitate revision of the classic approach to postpartum care. The findings of this study indicate that consideration is warranted of recommending an early visit around four to six weeks postpartum and later visits at three, and six to nine months after childbirth, which concurs with the immunization schedule in many countries. Adequate care for women in the year after childbirth, possibly provided in child-health centres, could make an important contribution to international commitments to improve maternal health [53].
References
Making pregnancy safer: the critical role of the skilled attendant: a joint statement by WHO, ICM and FIGO. [http://www.who.int/reproductive-health/publications/2004/skilled_attendant.pdf]
What is the effectiveness of antenatal care? (Supplement) Copenhagen, WHO Regional Office for Europe (Health Evidence Network report). [http://www.euro.who.int/Document/E87997.pdf]
WHO Antenatal Care Randomized Trial: Manual for the Implementation of the New Model. [http://www.who.int/reproductive-health/publications/RHR_01_30/index.html]
Health service coverage (includes Antenatal Care Coverage by country for years 1990-1999 and 2000-2006). [http://www.who.int/whosis/whostat/EN_WHS08_Table2_HSC.pdf]
Skilled attendant at birth - 2008 updates. [http://www.who.int/reproductive-health/global_monitoring/skilled_attendant_at_birth2008.pdf]
Levitt C, Shaw E, Wong S, Kaczorowski J, Springate R, Sellors J, Enkin M: Systematic review of the literature on postpartum care: methodology and literature search results. Birth. 2004, 31 (3): 196-202. 10.1111/j.0730-7659.2004.00305.x.
Pregnancy, childbirth, postpartum and newborn care: a guide for essential practice. [http://www.who.int/making_pregnancy_safer/documents/924159084x/en/index.html]
Balkus J, Bosire R, John-Stewart G, Mbori-Ngacha D, Schiff MA, Wamalwa D, Gichuhi C, Obimbo E, Wariua G, Farquhar C: High uptake of postpartum hormonal contraception among HIV-1-seropositive women in Kenya. Sex Transm Dis. 2007, 34 (1): 25-29. 10.1097/01.olq.0000218880.88179.36.
Tavengwa NV, Piwoz EG, Iliff PJ, Moulton LH, Zunguza CD, Nathoo KJ, Hargrove JW, Humphrey JH: Adoption of safer infant feeding and postpartum sexual practices and their relationship to maternal HIV status and risk of acquiring HIV in Zimbabwe. Trop Med Int Health. 2007, 12 (1): 97-106.
Richardson BA, Otieno PA, Mbori-Ngacha D, Overbaugh J, Farquhar C, John-Stewart GC: Hormonal contraception and HIV-1 disease progression among postpartum Kenyan women. AIDS. 2007, 21 (6): 749-753. 10.1097/QAD.0b013e328032790f.
Walson JL, Brown ER, Otieno PA, Mbori-Ngacha DA, Wariua G, Obimbo EM, Bosire RK, Farquhar C, Wamalwa D, John-Stewart GC: Morbidity among HIV-1-infected mothers in Kenya: prevalence and correlates of illness during 2-year postpartum follow-up. J Acquir Immune Defic Syndr. 2007, 46 (2): 208-215. 10.1097/QAI.0b013e318141fcc0.
Collin SM, Chisenga MM, Kasonka L, Haworth A, Young C, Filteau S, Murray SF: Factors associated with postpartum physical and mental morbidity among women with known HIV status in Lusaka, Zambia. AIDS Care. 2006, 18 (7): 812-820. 10.1080/09540120500465061.
Beyond the numbers: Reviewing maternal deaths and complications to make pregnancy safer. [http://www.who.int/reproductive-health/publications/btn/text.pdf]
Hoj L, da Silva D, Hedegaard K, Sandstrom A, Aaby P: Maternal mortality: only 42 days?. BJOG. 2003, 110 (11): 995-1000.
Ronsmans C, Graham WJ: Maternal mortality: who, when, where, and why. Lancet. 2006, 368 (9542): 1189-1200. 10.1016/S0140-6736(06)69380-X.
Sebitloane HM, Mhlanga RE: Changing patterns of maternal mortality (HIV/AIDS related) in poor countries. Best Pract Res Clin Obstet Gynaecol. 2008, 22 (3): 489-499. 10.1016/j.bpobgyn.2007.11.003.
Li XF, Fortney JA, Kotelchuck M, Glover LH: The postpartum period: the key to maternal mortality. Int J Gynaecol Obstet. 1996, 54 (1): 1-10. 10.1016/0020-7292(96)02667-7.
Waterstone M, Wolfe C, Hooper R, Bewley S: Postnatal morbidity after childbirth and severe obstetric morbidity. BJOG. 2003, 110 (2): 128-133. 10.1046/j.1471-0528.2003.02151.x.
Prual A, Huguet D, Garbin O, Rabe G: Severe obstetric morbidity of the third trimester, delivery and early puerperium in Niamey (Niger). Afr J Reprod Health. 1998, 2 (1): 10-19.
Vallely L, Ahmed Y, Murray SF: Postpartum maternal morbidity requiring hospital admission in Lusaka, Zambia - a descriptive study. BMC Pregnancy Childbirth. 2005, 5 (1): 1-10.1186/1471-2393-5-1.
Glazener CM, Abdalla M, Stroud P, Naji S, Templeton A, Russell IT: Postnatal maternal morbidity: extent, causes, prevention and treatment. Br J Obstet Gynaecol. 1995, 102 (4): 282-287.
Fikree FF, Ali T, Durocher JM, Rahbar MH: Health service utilization for perceived postpartum morbidity among poor women living in Karachi. Soc Sci Med. 2004, 59 (4): 681-694. 10.1016/j.socscimed.2003.11.034.
Mbizvo MT, Mmiro FA, Kasule J, Bagenda D, Mahomed K, Nathoo K, Mirembe F, Choto R, Nakabiito C, Ndugwa CM, et al: Morbidity and mortality patterns in HIV-1 seropositive/seronegative women in Kampala and Harare during pregnancy and in the subsequent two years. Cent Afr J Med. 2005, 51 (9-10): 91-97.
Immunization summary: the 2007 edition A statistical reference containing data through 2005. [http://www.unicef.org/publications/files/Immunization_Summary_2007.pdf]
Chersich MF, Luchters SM, Othigo MJ, Yard E, Mandaliya K, Temmerman M: HIV testing and counselling for women attending child health clinics: an opportunity for entry to prevent mother-to-child transmission and HIV treatment. Int J STD AIDS. 2008, 19 (1): 42-46. 10.1258/ijsa.2007.007117.
Chersich MF, Luchters SM, Yard E, Othigo JM, Kley N, Temmerman M: Morbidity in the first year postpartum among HIV-infected women in Kenya. Int J Gynaecol Obstet. 2008, 100 (1): 45-51. 10.1016/j.ijgo.2007.06.053.
The ICD-10 Classification of Mental and Behavioural Disorders. Diagnostic criteria for research. [http://www.who.int/classifications/icd/en/GRNBOOK.pdf]
AUDIT. The Alcohol Use Disorders Identification Test Guidelines for Use in Primary Care. [http://whqlibdoc.who.int/hq/2001/WHO_MSD_MSB_01.6a.pdf]
WHO: Iron Deficiency Anaemia: Assessment, Prevention and Control. A guide for programme managers. 2001, [http://www.who.int/nutrition/publications/en/ida_assessment_prevention_control.pdf]
WHO Antenatal Care Randomized Trial: Manual for the Implementation of the New Model. [http://www.who.int/reproductive-health/publications/RHR_01_30/index.html]
Lagro M, Liche A, Mumba T, Ntebeka R, van Roosmalen J: Postpartum health among rural Zambian women. Afr J Reprod Health. 2003, 7 (3): 41-48. 10.2307/3583287.
Bhatia JC, Cleland J: Obstetric morbidity in south India: results from a community survey. Soc Sci Med. 1996, 43 (10): 1507-1516. 10.1016/0277-9536(96)00105-0.
De Silva WI: Puerperal morbidity: a neglected area of maternal health in Sri Lanka. Soc Biol. 1998, 45 (3-4): 223-245.
Plummer FA, Laga M, Brunham RC, Piot P, Ronald AR, Bhullar V, Mati JY, Ndinya-Achola JO, Cheang M, Nsanze H: Postpartum upper genital tract infections in Nairobi, Kenya: epidemiology, etiology, and risk factors. J Infect Dis. 1987, 156 (1): 92-98.
Nygren P, Fu R, Freeman M, Bougatsos C, Klebanoff M, Guise JM: Evidence on the benefits and harms of screening and treating pregnant women who are asymptomatic for bacterial vaginosis: an update review for the U.S. Preventive Services Task Force. Ann Intern Med. 2008, 148 (3): 220-233.
Swadpanich U, Lumbiganon P, Prasertcharoensook W, Laopaiboon M: Antenatal lower genital tract infection screening and treatment programs for preventing preterm delivery. Cochrane Database Syst Rev. 2008, CD006178-2
Hillier SL, Kiviat NB, Hawes SE, Hasselquist MB, Hanssen PW, Eschenbach DA, Holmes KK: Role of bacterial vaginosis-associated microorganisms in endometritis. Am J Obstet Gynecol. 1996, 175 (2): 435-441. 10.1016/S0002-9378(96)70158-8.
Hillier SL, Martius J, Krohn M, Kiviat N, Holmes KK, Eschenbach DA: A case-control study of chorioamnionic infection and histologic chorioamnionitis in prematurity. N Engl J Med. 1988, 319 (15): 972-978.
Kurki T, Sivonen A, Renkonen OV, Savia E, Ylikorkala O: Bacterial vaginosis in early pregnancy and pregnancy outcome. Obstet Gynecol. 1992, 80 (2): 173-177.
Sexual and reproductive health of women living with HIV/AIDS: Guidelines on care, treatment and support for women living with HIV/AIDS and their children in resource-constrained settings. [http://www.who.int/reproductive-health/docs/srhwomen_hivaids/index.html]
Garcia-Moreno C, Jansen HA, Ellsberg M, Heise L, Watts CH: Prevalence of intimate partner violence: findings from the WHO multi-country study on women's health and domestic violence. Lancet. 2006, 368 (9543): 1260-1269. 10.1016/S0140-6736(06)69523-8.
Report of a WHO Technical Consultation on Birth Spacing. Geneva, Switzerland, 13-15 June 2005. [http://www.who.int/making_pregnancy_safer/publications/birth_spacing/en/]
Iron Deficiency Anaemia: Assessment, Prevention and Control. A guide for programme managers. [http://www.who.int/nutrition/publications/micronutrients/anaemia_iron_deficiency/WHO_NHD_01.3/en/index.html]
van Eijk AM, Ayisi JG, Slutsker L, Ter Kuile FO, Rosen DH, Otieno JA, Shi YP, Kager PA, Steketee RW, Nahlen BL: Effect of haematinic supplementation and malaria prevention on maternal anaemia and malaria in western Kenya. Trop Med Int Health. 2007, 12 (3): 342-352.
Lagro M, Liche A, Mumba T, Ntebeka R, van Roosmalen J: Postpartum care attendance at a rural district hospital in Zambia. Trop Doct. 2006, 36 (4): 205-208. 10.1258/004947506778604742.
Levitt C, Shaw E, Wong S, Kaczorowski J, Springate R, Sellors J, Enkin M: Systematic review of the literature on postpartum care: selected contraception methods, postpartum Papanicolaou test, and rubella immunization. Birth. 2004, 31 (3): 203-212. 10.1111/j.0730-7659.2004.00306.x.
Rarick TL, Tchabo JG: Timing of the postpartum Papanicolaou smear. Obstet Gynecol. 1994, 83 (5 Pt 1): 761-765.
Summary report on HPV and cervical cancer statistics in Kenya. [http://www.who.int/hpvcentre]
AIDS Epidemic Update: December 2007. [http://www.unaids.org/en/KnowledgeCentre/HIVData/EpiUpdate/EpiUpdArchive/20%2007/default.asp]
Central Bureau of Statistics (CBS) [Kenya], Ministry of Health (MOH) [Kenya], and ORC Macro. 2004. Kenya Demographic and Health Survey Calverton, Maryland: CBS, MOH, and ORC Macro.
Ransjo-Arvidson AB, Chintu K, Ng'andu N, Eriksson B, Susu B, Christensson K, Diwan VK: Maternal and infant health problems after normal childbirth: a randomised controlled study in Zambia. J Epidemiol Community Health. 1998, 52 (6): 385-391. 10.1136/jech.52.6.385.
Shaw E, Levitt C, Wong S, Kaczorowski J: Systematic review of the literature on postpartum care: effectiveness of postpartum support to improve maternal parenting, mental health, quality of life, and physical health. Birth. 2006, 33 (3): 210-220. 10.1111/j.1523-536X.2006.00106.x.
Lagro MGP, Stekelenburg J: [The Millennium project of the United Nations, focusing on adequate postpartum care to reduce maternal and neonatal mortality world-wide]. Ned Tijdschr Geneeskd. 2006, 150 (20): 1143-1147.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2393/9/51/prepub
Acknowledgements
We gratefully acknowledge the contribution of the postpartum study team: Jacinta Mutegi, Mary Kiambi, Moka Kilonza, and the study nurses, as well as women who participated in the study. The staff of Coast Provincial General Hospital, especially Dr K Shikely, Matron V Kapune and Dr G Ogweno added tremendous value to this study. Also, we acknowledge the input of the reviewers which improved the manuscript considerably. The work was carried out at the International Centre for Reproductive Health, Mombasa, Kenya.
Sources of funding
This study was finded by the European Union grant KE/AIDCO/2001/460 as part of the Uzazi Bora project. Matthew Chersich's contribution to the design and conduct of the study was supported by a PhD fellowship from the University of Gent. Nicole Kley's work on this study was made possible through the Postgraduate Program of International Affairs awarded by the Robert-Bosch-Foundation in cooperation with the German National Academic Foundation.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
MFC participated in the design of the study and drafted the manuscript. SL and NK participated in the design of the study and development of the initial draft. EY, CN and MO participated in the study coordination, collection of data and helped to draft the manuscript. MT made a substantial contribution to the study design, analysis and interpretation of findings. All authors read and approved the final manuscript.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Chersich, M.F., Kley, N., Luchters, S.M. et al. Maternal morbidity in the first year after childbirth in Mombasa Kenya; a needs assessment. BMC Pregnancy Childbirth 9, 51 (2009). https://doi.org/10.1186/1471-2393-9-51
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2393-9-51