Abstract
Background
Provision of effective care to all women and newborns during the perinatal period is a viable strategy for achieving the Sustainable Development Goal 3 targets on reducing maternal and neonatal mortality. This study examined perinatal care (antenatal, intrapartum, postpartum) and its association with perinatal deaths at three district hospitals in Bunyoro region, Uganda.
Methods
A cross-sectional study was conducted in which a questionnaire was administered consecutively to 872 postpartum women before discharge who had attended antenatal care and given birth in the study hospitals. Data on care received during antenatal, labour, delivery, and postpartum period, and perinatal outcome were extracted from medical records of the enrolled postnatal women using a pre-tested structured tool. The care received from antenatal to 24 h postpartum period was assessed against the standard protocol of care established by World Health Organization (WHO). Poisson regression was used to assess the association between care received and perinatal death.
Results
The mean age of the women was 25 years (standard deviation [SD] 5.95). Few women had their blood tested for hemoglobin levels, HIV, and Syphilis (n = 53, 6.1%); had their urine tested for glucose and proteins (n = 27, 3.1%); undertook an ultrasound scan (n = 262, 30%); and had their maternal status assessed (n = 122, 14%) during antenatal care as well as had their uterus assessed for contraction and bleeding during postpartum care (n = 63, 7.2%). There were 19 perinatal deaths, giving a perinatal mortality rate of 22/1,000 births (95% Confidence interval [CI] 8.1–35.5). Of these 9 (47.4%) were stillbirths while the remaining 10 (52.6%) were early neonatal deaths. In the antenatal phase, only fetal examination was significantly associated with perinatal death (adjusted prevalence ratio [aPR] = 0.22, 95% CI 0.1–0.6). No significant association was found between perinatal deaths and care during labour, delivery, and the early postpartum period.
Conclusion
Women did not receive all the required perinatal care during the perinatal period. Perinatal mortality rate in Bunyoro region remains high, although it’s lower than the national average. The study shows a reduction in the proportion of perinatal deaths for pregnancies where the mother received fetal monitoring. Strategies focused on strengthened fetal status monitoring such as fetal movement counting methods and fetal heart rate monitoring devices during pregnancy need to be devised to reduce the incidence of perinatal deaths. Findings from the study provide valuable information that would support the strengthening of perinatal care services for improved perinatal outcomes.
Similar content being viewed by others
Introduction
For countries to meet the national Sustainable Development Goal 3 targets to: (1) reduce the maternal mortality ratio to 70 deaths/100,000 live births by 2030 [1]; (2) reduce neonatal mortality rate to 12/1000 live births by 2030; and (3) reduce still births to 10 or less stillbirths/1000 total births as indicated in the WHO Every Newborn Action plan [2], there is need to improve the quality of perinatal care [3]. Indeed, provision of effective care to all women and newborns during delivery in health facilities has been estimated to prevent approximately 113,000 maternal deaths, 531,000 still births, and 1.325 million neonatal deaths annually [4].
Quality of care is defined by World Health Organization (WHO) as the extent to which health services given to individuals improve their desired health outcomes. For this to happen, the healthcare needs to be safe, effective, timely, efficient, equitable and people-centred [5]. To improve the quality of care during the perinatal period, WHO proposes a number of health care recommendations, including their time, frequency and method of provision to be given to the women during the antenatal, labour and delivery, and postnatal periods [6,7,8]. The WHO recommendations were designed to diagnose, prevent, and treat causes of maternal and neonatal deaths, and stillbirths [5]. As part of these recommendations, mothers are encouraged to have at least four antenatal care visits, have their labour monitored using a partograph, and receive postnatal care for the first 24 h. However, even when the number of women receiving this care tends to be generally satisfactory [9,10,11,12], neonatal mortality and stillbirth rates have remained high in Sub-Saharan Africa [13, 14].
Studies conducted to assess the associations between improved perinatal care and birth outcomes have had positive conclusions. A study that assessed the impact of implementing the 2016 WHO recommendations on antenatal care in South Africa revealed a 5.8% absolute decrease in stillbirths with the implementation of the recommendations [15]. A study conducted in Ethiopia showed that complete providers’ adherence to the recommendations during antenatal care was significantly associated with a decrease in neonatal complications [16]. Finally, a study in Uganda showed that having four or more antenatal visits reduced the odds of stillbirth, early neonatal death, low birth weight, and a 5-minute Apgar score of less than seven [17]. For the intrapartum period, studies have shown that the use of a partograph to monitor the indicated parameters during labour reduces birth asphyxia, a cause of perinatal deaths [18].
Although the studies above have shown a positive impact of adopting the WHO recommendations on birth outcomes, they have been limited to independent phases of care and not the full spectrum of care including the antenatal, intrapartum and postnatal care. In this study we document the association between perinatal care received during the antenatal, intrapartum, and postnatal periods, and perinatal deaths.
Methods
Study design and setting
A cross-sectional study was conducted between March and June 2020 in the three public district hospitals of Bunyoro region, Uganda. The region is comprised of eight districts that include Kakumiro, Kibaale, Kagadi, Kikuube, Hoima, Masindi, Buliisa, and Kiryandongo [19]. The region’s population was estimated at 2,028,500 million people in the 2014 National Demographic and Population Census [20]. Bunyoro region has one of the highest fertility rates in the country (7.5 births per woman), has a high proportion of teenage pregnancies (10.6%), and a high prevalence of early marriages (19%) [21]. The region has three district hospitals (Kagadi, Kiryandongo and Masindi). A district hospital is the highest-level public health facility in any given district and covers a catchment population of approximately 500,000 people. The district hospitals offer preventive, promotive, and both in and out patient curative services in all areas of child and adult medicine [22]. The hospitals are also responsible for supervising and planning for all the lower-level facilities within the district. An average of 300 births and eight [8] perinatal deaths are registered at each of these hospitals in any given month.
Study population
Women in their early postpartum period receiving care in the three participating district hospitals were screened at discharge for eligibility to join the study. A mother was eligible for inclusion in the study if: (1) she attended antenatal care in the study hospitals; (2) she gave birth in the study hospitals; (3) birth was conducted by a skilled health professional; (4) she provided written informed consent to participate in the study; and (5) she had a health record indicating care received during the antenatal, intrapartum, and postpartum periods.
Sample size and sampling
We hypothesized that occurrence of perinatal death would be different between women receiving the recommended perinatal care and those not receiving the care recommended. Using sample size formula for comparison of two proportions, and estimates of the prevalence of perinatal death among women who received the recommended care to be 2.5% and 5.3% among those who had not received based on a study done in Uganda [17], a sample size of 825 would be sufficient to test the hypothesis; assuming 5% level of significance, 80% power, adjusting for a design effect of 2 to cater for clustering at health facility level, and a non-response of 10%. We determined the number of women to be enrolled from each hospital using probability proportionate to size based on postnatal data from the hospitals. One hundred and ninety (190), 317, and 318 women were to be selected from Kiryandongo, Kagadi, and Masindi hospitals respectively. Consecutive sampling within each of the hospitals was used to select participants for the study.
Data collection
At each hospital, data was collected by qualified midwives fluent in the local language of the area (Runyoro) and not directly involved in the routine patient care at the participating hospitals. Women in their early postpartum period were identified using the ward registers and screened for eligibility to join the study. Following the consent process, a questionnaire was administered to collect socio-demographic data from the participants. Data on care received from start of antenatal care to 24 h postpartum and perinatal outcome was extracted from the participants’ hospital notes using a pre-tested structured data extraction tool designed using the Open Data Kit (ODK) software.
The dependent variable in this study was either a perinatal death or a live baby. Perinatal death referred to a documented still birth (death after 28 weeks of pregnancy before or during birth) or a neonatal death (death in the first 24 h after birth). This data was extracted from the women’s discharge forms or patient files. The independent variables included: antenatal care, intrapartum care, and postpartum care within 24 h after birth.
Antenatal care comprised of: number of antenatal contacts, time of initiation of antenatal care, examinations (fetal status and maternal status) during every contact, urine and blood tests conducted, ultrasound scan, prophylaxis for anaemia and malaria, and immunization against tetanus. This data was extracted from the women’s antenatal cards or mother child health passports. Intrapartum care included: fetal heart rate monitoring (fetal condition), progress of labour monitoring (cervical dilatation, descent of presenting part, and uterine contractions), and maternal condition monitoring (blood pressure and pulse rate measurements). Data on intrapartum care was extracted from the women’s partographs or patient files. Finally, the postpartum care within 24 h after birth considered by the study included: uterine assessments, maternal vital status monitoring, and urine voiding assessment. In particular, uterine assessment involved examination for uterine contraction, vaginal bleeding, and fundal height, while maternal vital status assessment included measuring of the woman’s blood pressure, temperature, and pulse rate. Postpartum care data was extracted from the women’s patient files.
Data management and statistical analysis
Data collected were exported to STATA version 13 for cleaning and analysis. For perinatal death (primary outcome), a score of 1 was assigned if a woman had a perinatal death and a score of 0 if a woman did not have a perinatal death. Each care parameter received by women during the perinatal period was assigned a score of 1 if it was received at least once during the entire period while a score of 0 if it was not received at all during the entire period. Antenatal contacts were categorized into less than four and four or more contacts as used in previous studies of pregnancy outcome to allow generalizability and comparison of results, although the current guidelines recommend eight contacts to be sufficient contact [17, 23, 24].
Continuous variables (age, income and parity) were categorized at analysis and all variables were summarized and presented as proportions stratified by the perinatal outcome. Perinatal mortality rate, stillbirth rate, and early neonatal death rate were calculated based on the WHO definition. Perinatal mortality was defined as the number of perinatal deaths per 1000 births; stillbirth rate as the number of stillbirths per 1000 total births; and the early neonatal death rate as the probability that a child born alive died during the first 24 h after birth, expressed per 1000 live births [25]. The mortality rates were then adjusted for clustering.
Modified Poisson with robust standard errors was used to assess for the association between perinatal deaths and perinatal care. Separate models were built for each level of care including the antenatal, intrapartum and postpartum care. All variables that had p-value of less than or equal to 0.20 at bivariate analysis were considered for multivariate analysis and logical model building was used to generate the final models. In the antepartum model, education level and ANC prophylaxis were found as confounders while maternal status monitoring, ultrasound scan, health facility attended, blood tests, ANC start trimester, and ANC contacts were considered as known confounders. All eight were included in the final model even when not statistically significant. For the intrapartum model, education level was a confounder while fetal condition assessment and labour progress assessment are known confounders, so all were included in the final model. Finally postpartum model was confounded by the education level and health facility attended while uterine assessment was considered a known confounder and all three were included in the final model. For all models, the measures of associations are presented as prevalence ratio (PR) with their 95% confidence intervals and p-values. A p-value of < 0.05 is considered significant.
Ethical considerations
Ethical approval to conduct the study was obtained from the Makerere University School of Medicine Research and Ethics Committee (REC REF# 2019 − 137) and the Uganda National Council for Science and Technology (HS483ES). Written informed consent to participate in the study was obtained from all participants prior to enrolment in the study, and unique identifiers and not personal names were used for participant identification.
Results
Description of the study population
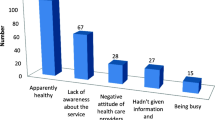
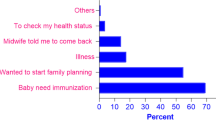
A total of 3,320 women were screened for eligibility to join the study, and 872 (26.3%) were enrolled. The commonest reason for exclusion was having not attended antenatal care at the study hospitals where they gave birth from (2,371, 96.9%). Other reasons for exclusion included patients being referred to study hospitals from lower facilities due to intrapartum complications, mothers arriving at the facility after birth (birth before arrival (BBA)) and refusing to provide informed consent to participate in the study. Figure 1 provides details of the participants flow stratified by health facility.
The mean age (standard deviation, SD) of the 872 enrolled participants was 25 (5.95) years. Majority of the participants were married or in a stable relationship (n = 782, 89.7%), and more than half (n = 453, 52%) had never received any formal education. Although many of the participants had two or more children (n = 615, 70.5%), almost all (n = 846, 97%) earned less than 500,000 Uganda Shillings ($140) per month. Table 1 provides details of the characteristics of the study participants.
Perinatal deaths among the study participants
Of the 872 women enrolled in the study, 9 (1%) had still birth giving a stillbirth rate of 10 deaths per 1000 total births (95% CI -1.9–22.5). In addition, 10 (1.2%) women lost their babies within the first 24 h of their birth giving the early neonatal death rate of 12 deaths per 1000 live births (95% CI -5.5–28.4). Overall, 19 women lost their babies in the perinatal period resulting in a perinatal mortality rate of 22 deaths per 1000 births (95% CI 8.1–35.5). Among the women who had perinatal death, 10 (52.6%) had delivered by spontaneous vaginal delivery and 9 (47.4%) were delivered by a C-section. No perinatal death was observed among women with assisted vaginal delivery. Most of the deaths were among women who earned less than UGX 100,000 ($28.6) per month compared to those who earned a higher salary (15, 79.0% versus 4, 21.0% respectively, p < 0.001). Similarly, most of the perinatal death were observed in women with no/only primary education, aged 20 to 35 years of age, married, and with no employment (Table 1). Perinatal deaths were mainly caused by childbirth related complications (15/19, 78.9%) specifically birth asphyxia [14] and fetal head retention [1]. The other causes of death were prolonged pregnancy [1], birth defects [1], suffocation [1], and unknown cause [1]. Birth asphyxia resulted from prolonged, obstructed labour, and prolapsed cord.
Antenatal care components associated with perinatal death
In the antenatal period, most women received prophylaxis for anaemia, malaria, and tetanus, and had their fetal status monitored at least once during the entire period (n = 741, 85% and n = 852, 97.7% respectively). However, a few women had their hemoglobin levels estimated nor their blood tested for HIV and syphilis (n = 53, 6.1%); had their urine tested for glucose and proteins (n = 27, 3.1%); took an ultrasound scan (n = 262, 30%); and had their BP, weight, and pallor (maternal status) assessed (n = 122, 14%). No perinatal death was observed among women who had eight or more contacts and had their urine tested for glucose and proteins. Details of the antenatal care received by women are provided in Supplement Table 1.
The prevalence of perinatal death was significantly lower among women whose fetal status examination (Fetal Heart Rate (FHR), Lie, Position, Fundal Height (FH)) was conducted during antenatal contacts compared to those who did not have it done (aPR = 0.22, 95% CI 0.1–0.6). The prevalence of perinatal death was also lower among women who attended antenatal care four or more times (aPR = 0.87, 95% Cl 0.3–2.3), and those who had their blood tested for hemoglobin level, HIV and syphilis (aPR = 0.88, 95% CI 0.1–6.8), although these associations were not statistically significant. However, the reverse was noted among women who undertook an ultrasound scan (aPR = 1.72, 95% Cl 0.6–4.8); had their blood pressure, weight and pallor assessed (aPR = 1.72, 95% Cl 0.6–4.6); and received iron/folic acid, fansidar, and tetanus toxoid during pregnancy (aPR = 1.96, 95% Cl 0.5–8.3). These women experienced a higher prevalence of perinatal death despite the associations not being statistically significant compared to those who did not undertake these interventions. Details of the associations between antenatal care received and perinatal death are provided in Table 2.
Labour, delivery, and first 24 h maternal postpartum care components associated with perinatal death
During labour and delivery, most women had their labour monitored at least once for fetal condition (fetal heart rate) (n = 660, 75.7%), maternal condition (blood pressure and pulse rate) (n = 505, 57.9%), and labour progress (cervical dilatation, descent of presenting part, and uterine contraction) (n = 611, 70.1%). Details of the care received by women are provided in Supplement Table 1. The prevalence of perinatal death was lower among women whose fetal condition was assessed during labor (aPR = 0.88, 95% Cl 0.0-21.2), maternal condition was measured including blood pressure and pulse rate (aPR = 0.29, 95% CI 0.1–1.1), and whose progress of labour was monitored including cervical dilatation, descent of presenting part, uterine contraction (aPR = 0.94, 95% CI 0.1–19.5), although these associations were not statistically significant (Table 3).
Lastly, in the first 24 h of the postpartum period, most women had their BP, pulse rate and temperature (maternal status) taken at least once (n = 533, 61.1%). However, only 7.2% (n = 63) of the women had their uterus assessed for contraction and bleeding (uterine assessment) (Supplement Table 1). The prevalence of perinatal death was higher among women whose uterus (uterine contraction, vaginal bleeding, FH) and maternal status (BP, PR, temperature) were assessed 24 h after birth compared to those who were not assessed although the associations were not statistically significant (aPR = 2.40, 95% Cl 0.8–6.9 for women whose uterine assessment was done and aPR = 1.41, 95% CI 0.3–6.7 for women whose maternal status was assessed) (Table 3).
Discussion
This study found a perinatal mortality rate of 22 per 1,000 births, comprised by a stillbirth rate of 10 per 1,000 total births and early neonatal mortality rate of 12 per 1,000 live births. Most perinatal deaths occurred among women who delivered spontaneously per vagina; had no/or only primary education; earned less than 100,000UGX ($28.6) per month; and were married. Prevalence of perinatal death was lower among women whose fetus was monitored during antenatal; who attended antenatal care four or more times; had their blood tested for HIV, syphilis, and hemoglobin level; and had their labour and delivery monitored for the fetal state, maternal state, and labour progress.
The estimated perinatal mortality in this setting is quite high with at least 2 in every 100 women having a perinatal death. This high number of perinatal deaths indicates that quality of care received during the perinatal period may have a direct impact on perinatal outcomes. However, although the perinatal mortality is high, it is still lower than the rates observed in earlier studies in Uganda that is 58(3%) stillbirths and 198 (11%) poor birth outcome in Western Uganda, 1432 (4.2%) late stillbirths and 495 (1.8%) early neonatal death in Eastern Uganda, and perinatal mortality of 43/1000 births in Northern Uganda [17, 26, 27] and also lower than the estimated perinatal mortality rates for the same region (institutional perinatal mortality of 26.1/1000 births) [28]. This difference in estimated mortality could be attributed to the stringent inclusion criterion used for women to join this study. In order to reduce on the missing data from the records, we excluded women who were emergency referrals, and those who did not attend antenatal care or delivered outside the study hospitals. Unfortunately, risk of perinatal mortality tends to be higher in women who are referred and those that do not attend antenatal care [29, 30], meaning that the actual mortality rates may be higher than those estimated by the study.
Perinatal mortality was common among women who had spontaneous vaginal deliveries compared to other forms of deliveries. Even with the supervision of a trained health worker, vaginal deliveries may have higher risks of perinatal deaths than operative deliveries. This could be because of malpresentations that may not be easily corrected due to limited time for manipulation, emergency deliveries when there are pregnancy complications like pre-eclampsia and eclampsia, multiple gestation, and preterm deliveries resulting in adverse outcomes [31, 32]. This observation is similar to findings from other studies including a study conducted in Ghana which showed a 5.9% prevalence of stillbirths among women who had delivered vaginally [31].
The higher prevalence of perinatal deaths observed among married women than the single women may be a unique finding to this study. Previous studies have shown that single/separated/divorced women are likely to have higher risk of perinatal death than married women due to the social, mental and monitory support they receive from their spouses [33, 34]. The difference observed in this study could be a result of the wealth status of the women in this particular region despite being married. Women in Bunyoro may not be fully empowered and supported by their spouses to seek services during pregnancy and childbirth, and thus the benefits of being married may not be appreciated in this setting [35].
Women earning less than UGX 100,000 ($28.6) per month were also observed to have more perinatal deaths than those earning more. This finding confirms results from earlier studies that have shown a higher risk of perinatal death among poor women in developing countries [34, 36, 37]. This could explain the occurrence of perinatal death among women who had less than eight contacts and had not undertaken an ultrasound scan in this study. Women who earn less are less likely to effectively use maternal health services like antenatal care which are known to reduce the risk of perinatal death even when they are free of charge due to their inability to meet the indirect costs like transport and personal needs [38]. Strategies aiming at economic empowerment of women could improve their access to maternal health services.
Similarly, women whose pregnancies were assessed at least once for fetal heart rate, fetal lie, and position, and fundal height during the antenatal period were observed to significantly have a lower prevalence of perinatal death. This confirms the protective nature of the fetal status monitoring intervention which identifies perinatal death risk factors like fetal distress for better management [39]. A lower prevalence was also seen among women whose blood was tested for HIV, syphilis and hemoglobin; attended antenatal four or more times; and started antenatal care late though the relationship was not significant. This emphasizes the importance of maternal screening in identification and management of perinatal death risk factors [39,40,41]. Therefore, availability of equipment, diagnostic tests, and adequate numbers of skilled health care providers could increase on the frequency and number of women assessed coupled with proper management of the identified risks. Lack of these characterizes resource constrained settings like Uganda [42,43,44].
Our findings however differ from previous studies in regard to antenatal contacts and time of start for antenatal care. Previous studies found increased antenatal contacts and early starting of antenatal care to significantly reduce the occurrence of perinatal death [17, 45, 46]. The difference in findings observed in this study could be a result of the low proportions of early initiation of ANC, ANC attendance of 4 and above, and stillbirth, and exclusion of referrals in this study; indulgence in self-care among experienced women [47]; and the fact that health care providers perceive women who start ANC late to be at risk and thus maximize care to them.
Despite the relationship not being statistically significant, generally women whose labour was monitored to assess fetal heart rate (fetal condition), maternal blood pressure and pulse rate (maternal condition), and cervical dilatation, descent of presenting part, and uterine contraction (labour progress) were seen to have fewer perinatal deaths. These intrapartum interventions when used are known to save life [39, 48]. These findings are in agreement with findings of a study conducted in Ethiopia, Zanzibar and Nepal respectively where women whose fetal heart rate, cervical dilatation, uterine contractions, and blood pressure were not monitored as recommended had higher odds of experiencing stillbirths [48,49,50]. This further calls for well-trained health care providers, sufficient infrastructure, and availability of necessary equipment.
Women assessed for uterine and maternal status immediately after birth experienced more perinatal deaths compared to those who were not. The assessment of these women by health care providers during the postnatal period could have been influenced by their health state during antenatal or labour and delivery. Women often experience pregnancy related complications or undergo operative delivery that could be associated with perinatal death [51, 52]. This calls for closer monitoring and observation by the health care providers during the postnatal period. Women who have experienced complications or undergone operative delivery are at risk of experiencing perinatal deaths due to an already compromised state of the baby [18] and compromised breastfeeding resulting from mother’s poor health state [53]. However, this finding contrast an earlier study conducted in five countries of Bangladesh, Ethiopia, Ghana, Guinea-Bissau and Uganda which revealed that women with stillbirth were less likely to report having received a postnatal check [54]. The difference in these findings, if true, may indicate a disparity in the perception of postpartum care received by women by both health care providers and the women themselves.
However, even when all these health care recommendations are taken to be protective by World Health Organization in its guidelines [6,7,8], some of these have not been statistically significant in this study. Taking an ultrasound scan; having blood pressure, weight and pallor assessment; and receiving iron/folic acid, fansidar, and tetanus toxoid during pregnancy have not been observed to be statistically associated with adverse outcomes in this study. Therefore, this study may not be powered enough to explain their influence on perinatal death.
Furthermore, the study has not observed an association between perinatal death and perinatal care except for fetal status monitoring during pregnancy. This may have resulted from the low occurrence of perinatal deaths shown in this paper. This study may also not be powered enough to explain perinatal care influence on perinatal death. Further studies with higher statistical power could re-assess the association between perinatal care and perinatal death.
This study had some limitations. First, this study extracted the data on care from patient records and was not corroborated by patient or provider interviews. It is possible that information recorded did not exactly reflect the care provided to mothers during these periods of care. In addition, there is no data on direct observation of the care processes which would have explained or validated the data extracted from the patient records. This could have affected the assessment of the relationships between care processes and birth outcomes. Secondly, the source of data also makes it hard to appreciate the in-depth factors that could influence occurrence of perinatal deaths including personal factors like beliefs, values, experiences, and ability to access services. Thirdly, the study did not include women who were referred for childbirth from other facilities and did not attend antenatal care in the study hospitals yet perinatal deaths are common among these women [29, 30]. Follow up on baby status after birth was also for 24 h only instead of 7 days. Therefore, the estimated perinatal death rates may be lower than the actual values in this setting. The study did not capture information on type of pregnancy, existing co-morbidities, gestation age at birth, care given to the newborn, and the effect of postnatal care to the mother on the newborn which could have influenced the occurrence of perinatal deaths among mothers. Lastly, it was a cross sectional study that merely provided a snapshot of the care processes and their associated birth outcomes in these facilities. To mitigate the limitations, interviews were held with women and health care providers to validate the care provided and observations of care provided during the process of data extraction was done to give insight on the context in which care was provided, although this was limited and not documented and thus not included in the study findings. Despite the limitations, results from the study are still valid as they highlight the gaps in care, the linkage between care provided and outcome, and make suggestions for strengthening perinatal care, which provides a basis for further studies. To our knowledge, this could be the first study to document association between perinatal care recommendations and perinatal death in a resource limited setting.
Conclusion
The study shows a high perinatal mortality rate in Bunyoro although lower than the national average. Fetal status monitoring during the antenatal period significantly reduces occurrence of perinatal deaths. Having many antenatal contacts and blood tested for HIV, hemoglobin, and syphilis during antenatal also reduces the likelihood of having perinatal deaths even when not statistically significant. Generally, monitoring women during labour and childbirth for fetal condition, maternal condition, and labour progress reduces their chance of experiencing perinatal death despite not being statistically significant. Therefore, to address perinatal mortality in this region of Uganda, strategies should focus on the quality of care provided to women by health care providers, particularly care that shows the status of the fetus and the woman during pregnancy and childbirth. Efforts should also be made to empower women so as to enhance their ability to seek for perinatal services.
Data availability
The datasets generated or analyzed during this study are included in this published article (and its supplementary information files).
Abbreviations
- ANC:
-
Antenatal care
- BBA:
-
Birth before arrival
- BP:
-
Blood Pressure
- FHR:
-
Fetal Heart Rate
- FH:
-
Fundal Height
- Fe/Fo:
-
Iron/Folic acid
- PR:
-
Pulse Rate
- SP:
-
Sulphadoxine Pyrimethamine (Fansidar)
- Wt:
-
Weight
- UGX:
-
Uganda Shillings
References
Jolivet RR, Moran A, O’Connor M, Chou D, Bhardwaj N, Newby H, Requejo J, Schaaf M, Say L, Langer A. Ending preventable maternal mortality: phase II of a multi-step process to develop a monitoring framework, 2016–2030. BMC Pregnancy and Childbirth 2018;18.
WHO. Every newborn: an action plan to end preventable death. South Africa; 2014.
Sharma G, Mathai M, Dickson KE, Weeks A, Hofmeyr GJ, Lavender T et al. Quality care during labour and birth: a multicountry analysis of health system bottlenecks and potential solutions. BMC Pregnancy Childbirth 2015;15 (Suppl 2).
Bhutta ZA, Das JK, Bahl R, Lawn JE, Salam RA, Paul VK, Sankar MJ, Blencowe H, Rizvi A, Chou VB. Can available interventions end preventable deaths in mothers, newborn babies, and stillbirths, and at what cost? The Lancet. 2014;384:347–70.
Tuncalp O, Were W, MacLennan C, Oladapo OT, Gulmezoglu AM, Bahl R, Daelmans B, Mathai M, Say L, Kristensen F, Temmerman M, Bustreo F. Quality of care for pregnant women and newborns- the WHO vision. BJOG. 2015;122:1045–9.
WHO. WHO recommendations on antenatal care for a positive pregnancy experience. Geneva: WHO; 2016.
WHO. WHO recommendations Intrapartum care for a positive childbirth experience. Geneva: WHO; 2018.
WHO. WHO recommendations on maternal and newborn care for a positive postnatal experience. Geneva: WHO; 2022.
Adedoun TS, Yaya S. Correlates of antenatal care utilization among women of reproductive age in sub-saharan Africa: evidence from multinomial analysis of demographic and health surveys (2010–2018) from 31 countries. Archives of Public Health. 2020;78.
Andegiorgish KA, Elhoumed M, Qi Q, Zhu Z, Zeng L. Determinants of antenatal care use in nine sub-suharan African countries: a statistical analysis of cross-sectional data from demographic and health surveys. BMJ Open. 2022;12.
Hagos AA, Eshetu C, Degu G. Utilization of partograph and its associated factors among midwives working in public health institutions, Addis Ababa City Administration, Ethiopia, 2017. BMC Pregnancy and Childbirth. 2020;2020.
Dey T, Ononge S, Weeks A, Benova L. Immediate postnatal care following childbirth in Ugandan health facilities: an analysis of demographic and health surveys between 2001 and 2016. BMJ Global Health. 2021;6.
Masaba BB, Mmusi-Pheoe M. Neonatal survival in Sub-suhara: a review of Kenya and South Africa. J Multidisciplinary Health care. 2022;13:709–16.
UNICEF. A neglected tragedy: the global burden of stillbirths. New York; 2020.
Lavin T, Pattinson C, Kelty E, Pillay Y, Preen BD. The impact of implementing the 2016 WHO recommendations on antenatal care for a positive pregnancy experience on perinatal deaths: an interrupted time-series analysis in Mpumalanga Province, South Africa. BMJ Global Health. 2020;5:e002965.
Seyoum T, Alemayehu M, Christensson K, Lindgren H. Effect of complete adherence to antenatal care guideline during first visit on maternal and neonatal complications during the intrapartum and postpartum periods: a prospective cohort study in Northwest Ethiopia. BMJ Open. 2021;11.
McDiehl PR, Boatin A, Mugyenyi RG, Siedner JM, Riley EL, Ngonzi J. Bebell. Antenatal care visit attendance frequency and birth outcomes in rural Uganda: a prospective cohort study. Matern Child Health J. 2021;25(2):311–20.
Anokye R, Achaempong E, Anokye J, Budu-Ainooson A, Amekudzie E, Owusu I, Gyamfi N, Akwasi GA, Mprah KW. Use and completion of partograph during labour is associated with a reduced incidence of birth asphyxia: a retrospective study at a peri-urban setting in Ghana. J Health Popul Nutr. 2019;38.
Uganda Bureau of Statistics (UBOS). 2020 Statistical Abstract 2020 [Available from: https://www.ubos.org/wp-content/uploads/publications/11_2020STATISTICAL__ABSTRACT_2020.pdf.
Uganda Bureau of Statistics (UBOS). The National Population and Housing Census 2014 - National Analytical Report Kampala: UBOS. ; 2017 [Available from: https://www.ubos.org/wp-content/uploads/publications/03_20182014_National_Census_Main_Report.pdf.
Uganda Bureau of Statistics (UBOS). The National Population and Housing Census 2014 – Health status and associated factors. Thematic Report Series [Report]. Kampala: UBOS; 2017 [updated November 2017. Available from: https://uganda.unfpa.org/sites/default/files/pub-pdf/Health%20Monograph%2010-01-2018%20With%20Covers.pdf.
Ministry of Health. Guidelines for designation, establishment, and upgrading of health units. Criteria for designation of Levels of Services Delivery of Health Units. Kampala: MoH; 2011.
Asundep NN, Jolly PE, Carson A, Turpin CA, Zhang K, Tameru B. Antenatal care attendance, a surrogate for pregnancy outcome? The case of Kumasi, Ghana. Matern Child Health J. 2014;18(5):1085–94.
Dey SK, Afroze S, Islam T, Jahan I, Hassan Shabuj KM, Suraiya B, Chisti JM, Mannan AM, Shahidullah M. Death audit in the neonatal ICU of a tertiary care hospital in Bangladesh: a retrospective chart review. J Maternal-Fetal Neonatal Med. 2019;32(5).
WHO. Global reference list of 100 core health indicators. Geneva, Switzerland: WHO; 2015.
Waiswa P, Higgins VB, Mubiri P, Kirumbi L, Butrick E, Merai R, Sloan LN, Walker D. Pregnancy outcomes in facility deliveries in Kenya and Uganda: a large cross-sectional analysis of maternity registers illuminating opportunities for mortality prevention. PLoS ONE. 2020;15(6).
Arach OAA, Tumwine K, Nakasujja N, Ndeezi G, Kiguli J, Mukunya D et al. Perinatal death in Northern Uganda: incidence and risk factors in a community-based prospective cohort study. Global Health Action. 2021;14.
Ministry of Health. Annual health sector performance report 2020/21. Kampala; 2021.
Mdoe P, Katengu S, Gugga G, Daudi V, Kiligo IE, Gidabayda J et al. Perinatal mortality audit in a rural referral hospital in Tanzania to inform future interventions: a descriptive study. PLoS ONE. 2022;17(3).
Musaba WM, Ndeezi G, Barageine KJ, Weeks DA, Wandabwa NJ, Mukunya D, Waako P et al. Incidence and determinants of perinatal mortality among women with obstructed labour in eastern Uganda: a prospective cohort study. Maternal Health, Neonatology, and Perinatology. 2021;7.
Dassah TE, Odoi TA, Opoku KB. Stillbirths and very low apgar scores among vaginal births in a tertiary hospital in Ghana: a retrospective cross-sectional analysis. BMC Pregnancy Childbirth. 2014;14(289).
Tesfalul AM, Natureeba P, Day N, Thomas O, Gaw LS. Identifying risk factors for perinatal death at Tororo District Hospital, Uganda: a case-control study. BMC Pregnancy Childbirth. 2020;20(45).
Balayla J, Azoualay L, Abenhaim AH. Maternal marital status and the risk of stillirth and infant death: a population-based cohort study on 40 million births in the United States. Women’s Health Issues: Official Publication of the Jacobs Institute of Women’s Health. 2011;21(5):361–5.
Tesema AG, Tessema TZ, Tamirat SK, Teshale BA. Prevalence of stillbirth and its associated factors in East Africa: generalized linear mixed modeling. BMC Pregnancy Childbirth. 2021;21.
Babughirana G, Gerald S, Mokori A, Nangosha E, Kremers, Glubbels J. Maternal and newborn healthcare practices: assessment of the uptake of lifesaving services in Hoima District, Uganda. BMC Pregnancy Childbirth. 2020;20.
Ashish KC, Wrammer J, Ewald U, Clark RB, Gautam J, Baral G, Baral PK, Malqvist M. Incidence of intrapartum stillbirth and associated risk factors in tertiary care setting of Nepal: a case-control study. Reproductive Health. 2016;13.
Aminu M, Unkels R, Mdegela M, Utz B, Adaji S, Broek DVN. Causes of and factors associated with stillbirth in low and middle income countries: a systematic literature review. BJOG 121(Suppl 4):141–53.
Arthur E. Wealth and antenatal care use: implications for maternal health care utilisation in Ghana. Health Econ Rev. 2012;2.
Goldenberg RL, Griffin J, Kamath-Rayne BD, Harrison M, Rouse DJ, Moran K, Helper B, Jobe AH, McClure EM. Clinical interventions to reduce stillbirths in sub-saharan Africa: a mathematical model to estimate the potential reduction of stillbirths associated with specific obstetric conditions. BJOG. 2016;125:119–29.
Debella A, Eyeberu A, Getachew T, Atnafe G, Geda B, Dheresa M. Perinatal outcomes in anemic pregnant women in public hospitals of eastern Ethiopia. Int Health. 2023;15(3):274–80.
Wedi COO, Kirtley S, Hopewell S, Corrigan R, Kennedy HS, Hemelaar J. Perinatal outcomes associated with maternal HIV infection: a systematic review and meta-analysis. Lancet HIV. 2016;3(1):e33–e48.
Kananura MR, Kiwanuka N, Ekirapa-Kiracho E, Waiswa P. Persisting demand and supply gap for maternal and newborn care in eastern Uganda: a mixed-method cross-sectional study. Reproductive Health. 2017;14.
Munabi-Babigumira S, Glenton C, Willcox M, Nabudere H. Ugandan health workers’ and mothers’ views and experiences of the quality of maternity care and the use of informal solutions: a qualitative study. PLoS ONE. 2019;14(3).
Kanyesigye H, Ngonzi J, Mulogo E, Fajardo Y, Kabakyenga J. Health care workers’ experiences, challenges of obstetric referral processes and self-reported solutions in South Western Uganda: mixed methods study. Risk Manage Healthc Policy. 2022;15:1869–86.
Shiferaw K, Mengiste B, Gobena T, Dheresa M. The effect of antenatal care on perinatal outcomes in Ethiopia: a systematic review and meta-analysis. PLoS ONE. 2021;16(1).
Afulani AP. Determinants of stillbirths in Ghana: does quality of antenatal care matter? BMC Pregnancy Childbirth. 2016;16.
Jinga N, Mongweyana C, Moolla A, Malete G, Onoya D. Reasons for late presentation for antenatal care, healthcare providers’ perspective. BMC Health Serv Res. 2019;19.
Ekblom A, Malqvist M, Gurung R, Rossley A, Basnet O, Bhattarai P, Ashish KC. Factors associated with poor adherence to intrapartum fetal heart monitoring in relationship to intrapartum related death: a prospective cohort study. PLOS Global Public Health. 2022;2(5).
Agena GA, Modiba ML. Consistency and timeliness of intrapartum care interventions as predictors of intrapartum stillbirth in public health facilities of Addis Ababa, Ethiopia: a case-control study. Pan Afr Med J. 2021;40(36).
Maaløe N, Housseine N, Bygbjerg CI, Meguid T, Khamis SR, Mohamed GA, Nielsen BB, Roosmalen VJ. Stillbirths and quality of care during labour at the low resource referral hospital of Zanzibar: a case-control study. BMC Pregnancy Childbirth. 2016;16.
Khanam R, Saifuddin A, Creanga A, Begum N, Koffi KA, Mahmud A et al. Antepartum complications and perinatal mortality in rural Bangladesh. BMC Pregnancy Childbirth. 2017;17.
Sobhy S, Arroyo-Manzano D, Murugesu N, Karthikeyan G, Kumar V, Kaur I, et al. Maternal and perinatal mortality and complications associated with caesarean section in low-income and middle-income countries: a systematic review and meta-analysis. Lancet. 2019;393(10184):1973–82.
Smith RE, Hurt L, Chowdhury R, Bireshwar S, Wafaie F, Edmond MK et al. Delayed breastfeeding initiation and infant survival: a systematic review and meta-analysis. PLoS ONE. 2017;12(7).
Stefano DL, Bottecchia M, Yargawa J, Akuze J, Haider MM, Galiwango E, Dzabeng F, Fisker BA et al. Stillbirth maternity care measurement and associated factors in population-based surveys: EN-INDEPTH study. Population Health Metrics. 2021;19(Suppl 1).
Acknowledgements
We are thankful to all women who agreed to participate in the study, the health facility and perinatal unit leadership that made access to women and their records possible, and the research assistants who ensured that quality data is obtained. Special appreciation is given to the study site supervisors who ensured that data is timely accessed and collected. Lastly, we appreciate the district health officers for allowing this study to be conducted in their districts.
Funding
This study was self-funded by the principal investigator.
Author information
Authors and Affiliations
Contributions
MM, DKK, JIN, and GE designed the study and wrote the study protocol. MM, JIN, JO and WM conducted the analysis and interpretation of the data. MM and WM prepared the first drafts of the manuscript. All authors participated in revising the manuscript, and approved the final draft.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
Ethical approval to conduct the study was obtained from the Makerere University School of Medicine Research and Ethics Committee (REC REF# 2019 − 137) and the Uganda National Council for Science and Technology (HS483ES). Written informed consent to participate in the study was obtained from all participants prior to enrolment in the study, and unique identifiers and not personal names were used for participant identification. For participants below 18 years and those with no education, informed consent was sought from their parents/guardians. All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Muwema, M., Nankabirwa, J.I., Edwards, G. et al. Perinatal care and its association with perinatal death among women attending care in three district hospitals of western Uganda. BMC Pregnancy Childbirth 24, 113 (2024). https://doi.org/10.1186/s12884-024-06305-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-024-06305-5