Abstract
Background
Purpose of the study was to investigate alterations in midbrain serotonin transporter (SERT) binding in patients with epilepsy and symptoms of depression compared to patients with epilepsy with no symptoms of depression.
Methods
We studied 12 patients with epilepsy (7 patients had focal and 5 had generalized epilepsy syndromes). The presence of self-reported symptoms of depression was assessed using Beck Depression Inventory (BDI) and the Emotional State Questionnaire (EST-Q). The binding potential of the SERT was assessed by performing brain single photon emission tomography (SPET) using the SERT radioligand 2-((2-((dimethylamino)methyl)phenyl)thio)-5-(123)iodophenylamine (123I-ADAM).
Results
Seven patients had BDI and EST-Q subscale scores greater than 11 points, which was interpreted as the presence of symptoms of depression. We found that 123I-ADAM binding was not significantly different between patients with epilepsy with and without symptoms of depression. In addition, 123I-ADAM binding did not show a significant correlation to either BDI or EST-Q depression subscale scores and did not differ between patients with focal vs. generalized epilepsy.
Conclusion
The results of our study failed to demonstrate alterations of SERT binding properties in patients with epilepsy with or without symptoms of depression.
Similar content being viewed by others
Background
The frequent coexistence of epilepsy and depression has encouraged researchers to explore potential shared mechanisms underlying these disorders. Depression occurs far more frequently in patients with epilepsy than in the general population, affecting approximately 30% of this patient population [1, 2]. At the same time, the presence of a psychiatric disorder, such as depression, has been shown to reduce seizure threshold, and depression and attempted suicide themselves are risk factors for epilepsy [3–5]. These findings have led to the concept of a bidirectional relation between epilepsy and depression [6]. This issue is important, as the presence of depression is likely to be the most important factor influencing quality of life in patients with epilepsy [7, 8], and can negatively impact both medical and surgical treatment outcomes [9–11].
The dysfunction of the brain serotonin (5-hydroxytryptamine or 5-HT) system has been suspected to be the common denominator for the shared pathogenic mechanisms of epilepsy and depression. Alterations in serotonergic signaling are associated with the pathogenesis of depression in patients with major depressive disorder - findings that are clinically supported by the effect of selective serotonin reuptake inhibitors (SSRIs) in the treatment of depression. Several neuroimaging studies using different positron emission tomography (PET) or single photon emission tomography (SPET) tracers for various components of serotonergic system in the brain have supported the involvement of 5-HT in major depressive disorder. These alterations include increased serotonin transporter (SERT) binding in the thalamus and limbic regions [12], or decreased brainstem and midbrain SERT binding [13–15], as well as reduced 5-HT1A receptor binding potential in various limbic and neocortical regions and the raphe nuclei [16].
A growing body of evidence implicates the role of serotonin system in epilepsy. This includes studies in which the anticonvulsant effects of SSRIs have been confirmed, such as Favale et al. [17]. In this study, citalopram was administered to non-depressed patients with poorly controlled epilepsy who then experienced a marked drop in seizure frequency [17]. Previous neuroimaging works have used PET tracers for 5-HT1A receptors to investigate the role of the serotonergic system in epilepsy and depression. These studies have concentrated on patients with both temporal lobe epilepsy (TLE) and depression and have shown reduced 5-HT1A receptor binding potential in the ipsilateral temporal lobe as well as in thalamic regions, hippocampus, anterior insula, anterior cingulate, and the raphe nuclei in the depressed patients [18–20]. Thus, in TLE patients with depression, there appear to be alterations in the serotonergic system not only in the brain regions affected by epilepsy, but also more generally in ipsilateral and contralateral areas associated with regulation of emotion, these are changes that are similar to those described in patients with major depressive disorder alone.
2-((2-((dimethylamino)methyl)phenyl)thio)-5-(123)iodophenylamine (123I-ADAM) is a novel SPET tracer that has shown a high binding affinity for SERT as well as high selectivity for 5-HT transporter over those for norepinephrine and dopamine, and which has been proven to have excellent brain uptake in rats [21]. Subsequently, other studies demonstrated the feasibility of its use in human subjects [22–25]. Newberg et al. [26] used SPET to demonstrate alterations in SERT binding in patients with major depression; in this study, SERT binding was decreased in the midbrain region of patients with major depressive disorder and the degree of decrease correlated significantly with the severity of depressive symptoms [26]. These findings were generally corroborated by a later study by the same group using a larger sample size [27]. However, to our knowledge, no studies of SERT binding have been conducted in patients with epilepsy.
The aim of the current study was to investigate SERT binding in the midbrain of patients with epilepsy with symptoms of depression, and to determine differences in SERT binding compared to patients with epilepsy without symptoms of depression.
Methods
Subjects
This study was approved by the Research Ethics Committee of the University of Tartu. We studied 12 patients (7 men and 5 women; ages ranging from 21 to 55 years; mean age 36.3 ± 8.9 years) with epilepsy who were recruited from the outpatient clinic at the Department of Neurology and Neurosurgery in University of Tartu and West-Tallinn Central Hospital in Tallinn, Estonia. Patients were otherwise healthy, with no history of other neurological disorders except epilepsy, and did not use antidepressant medications prior to this study. All patients gave informed consent to participate in the study.
In the current study, all patients with symptoms of depression were consulted regarding their affective disorder, and treatment with antidepressant medications was offered following the 123I-ADAM SPET study.
Assessment of symptoms of depression
Patients were screened for self-reported symptoms of depression using the Beck Depression Inventory (BDI) [28] and the Emotional State Questionnaire (EST-Q) [29]. Questionnaires were administered directly before the start of the 123I-ADAM SPET imaging session. A cut-off score of > 11 points was used to define the presence of symptoms of depression on the BDI. EST-Q is a self-report questionnaire for depression and anxiety that uses the rating of 33 items on a five-point frequency scale. This questionnaire has five subscales: depression, anxiety, agoraphobia–panic, fatigue, and insomnia. In the current study, a cut-off score of > 11 points was used to define the presence of symptoms of depression on the EST-Q depression subscale.
Methods
We examined serotonin transporter (SERT) binding potential by performing brain SPET study with 2-((2-((dimethylamino)methyl)phenyl)thio)-5-(123)iodophenylamine (123I-ADAM). The subjects received a dose of 185 MBq 123I-ADAM (MAP Medical Finland) intravenously. To block the thyroid gland, potassium perchlorate (KClO4; 800 mg) was given orally at least 20 min prior to the injection of 123I-ADAM. Brain SPET studies were acquired 4 hours after the injection of 123I-ADAM.
SPET studies were performed using a SPET/CT INFINIA Hawkeye 4 (GE Healthcare) dual head gamma camera with low energy high-resolution collimators (Lehr collimators). The energy window was centered on 159 keV (+/-10%). SPET scans were acquired in a step and shoot mode with total angular range of 360 degrees thereby arc per detector being 180 degrees. View angle 3 degrees, 120 views, 30 sec per projection. Acquisition time was 30 min. Matrix size was 128 × 128, with a zoom of 1.0.
Data were reconstructed using the Xeleris Functional Imaging Workstation software (GE Healthcare). Transverse slices were reconstructed parallel to the canthomental plane. SPET data were reconstructed using a Butterworth filter (critical frequency 0.4, power 6), followed by the Chang attenuation correction (threshold 5, coefficient 0.11). SPET and MRI data were automatically coregistered using MPI Tool software (ATV Inc., Kerpen, Germany). To measure the individual SERT occupancy, irregular regions of interest (ROIs) were manually drawn over the midbrain and over the cerebellum as the reference area. The 123I-ADAM binding was assessed using MRI-guided ROIs in the midbrain and cerebellum. ROIs were placed on transaxial MRI slices over the midbrain and cerebellum and then transferred onto corresponding SPET slices. In addition, radio-uptake and the specific uptake ratios (SURs) of midbrain were assessed. As a measure of brain SERT availability, the ratio of specific-to-nonspecific 123I-ADAM binding for the midbrain compared to the cerebellum were calculated in mean counts/pixel using the following equation: SUR = specific binding/nonspecific binding = target- cerebellum/cerebellum.
Statistical analysis
Statistical analysis was performed with STATISTICA 8.0. Student’s t-tests were used to compare variables between the two groups of patients (with symptoms of depression vs. without symptoms of depression). A correlation analysis was used to assess the relationship between depression scale scores, demographic, and clinical characteristics, and SERT binding potential.
Results
A summary of patient characteristics, including their demographic and clinical characteristics is included in Table 1. Seven patients had focal epilepsy; six of these had had long-term EEG monitoring performed in order to define focus localization. Of these seven patients, six patients had TLE (two with right sided and four with left sided TLE) and one patient had probable frontal lobe epilepsy (FLE; lateralization to the right side). Five patients had generalized epilepsy syndrome. MRI scans for the generalized epilepsy patients were all normal. On the MRI, three patients with focal epilepsy presented with mesial temporal sclerosis, one with hippocampal atrophy, and one with cysts in temporomesial structures. Epilepsy could be considered treatment resistant in the majority of the patients, eight of whom were on polytherapy with antiepileptic drugs (AEDs). The patients with focal epilepsy, as a group, were comparable to the patients with generalized epilepsy regarding age, age at epilepsy onset, epilepsy duration, use of AEDs, as well as their mean BDI and EST-Q questionnaire scores.
Seven patients had BDI and EST-Q depression subscale scores greater than 11 points, which was interpreted as the presence of symptoms of depression. The mean BDI and EST-Q depression subscale scores for the whole patient group were 11.5 ± 6 and 14 ± 4.3, respectively. The maximal BDI score was 20; in all patients with symptoms of depression, the BDI score was in the range of mild to moderate severity.
In the current study, patients with symptoms of depression, as a group, did not significantly differ from patients without symptoms of depression in either demographic or clinical variables (Table 2). A comparison of these patient groups indicated that patients with symptoms of depression showed a trend towards a longer duration of epilepsy, which did not reach statistical significance.
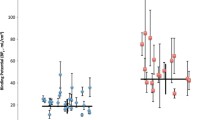
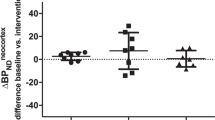
Using SPET, we observed that 123I-ADAM binding to SERT did not differ significantly between the patients with epilepsy who had symptoms of depression vs. those without. In addition, SERT binding potential of 123I-ADAM did not show any statistically significant correlation with either the BDI or the EST-Q depression subscale scores. SERT binding potential was also not correlated with any demographic or clinical characteristics, including age, duration of epilepsy, or age at disease onset. We also observed that the SERT binding potential did not differ between patients with focal vs. generalized epilepsy.
One patient with moderate symptoms of depression on BDI committed suicide shortly following the 123I-ADAM imaging study.
Discussion
In the current study, we sought to study SERT binding properties in the midbrain region in patients with epilepsy, and to determine whether SERT binding differed between depressed vs. non-depressed patients with epilepsy. Our results did not indicate any difference in SERT binding potential between these patient groups.
There could be several reasons for these negative results. Previous work with PET and SPET tracers for SERT in depressed patients has shown some conflicting results. The majority of reports show increased SERT binding in the thalamus and limbic regions of depressed patients compared to controls [30], but others have shown decreased SERT binding potential in the amygdala and midbrain of depressed patients [13–15]. Studies using 123I-ADAM SPET to measure SERT binding in major depressive disorder have also indicated decreased SERT binding in the midbrain, medial temporal lobe, and basal ganglia of depressed patients compared to controls [26, 27]. At the same time, however, reports showing no differences in midbrain SERT availability for 123I-ADAM in patients with depression compared to healthy controls have also been published [31, 32]. It has been hypothesized that, in case of major depressive disorder, the SERT binding potential is elevated, but that in major depressive disorder with comorbid psychiatric illnesses, regional SERT binding could be decreased [12]. Taking this into account, and considering the fact that there are no SERT binding studies done in patients with epilepsy, it could be difficult to predict the directionality of alterations in SERT binding in patients with epilepsy and comorbid depression. Addressing this hypothesis more fully would likely require a study with a larger sample size.
Another contributing factor to these negative results may be the genetic variability that has been shown for SERT expression in the human brain. For example, individuals with polymorphisms in the promoter (5-HTTLPR) of the SLC6A4 gene, which encodes the SERT protein, exhibit differences in SERT binding properties in neuroimaging studies [33–35]. Genetic studies have shown that there may even be an association between the presence of the combined 5-HTTLPR and 5-HTTVNTR genotype, which results in less efficient transcription of SERT, and the presence of TLE [36]. Genetic variability of SERT expression may influence the development of affective disorders, it would likely affect SERT imaging studies, and could even be related to epileptogenesis. Unfortunately, in the current study, we did not genotype our patients for polymorphisms in SLC6A4.
There are several limitations to the current study. Perhaps the most important, and the one likely to be largely responsible for our negative results, is the relatively small study sample size. The statistical power of the comparison of SERT binding in groups of patients with and without depression was 0.755. We calculated that increasing the power to 0.8 under the same conditions would need 40 subjects, which considering the nature and cost of SPET imaging, would be unachievable.
Since in all patients with symptoms of depression, the BDI score was in the range of mild to moderate severity, it could also be considered as a weakness contributing to the negative results of our study.
The heterogeneity of our study group, regarding the clinical characteristics of epilepsy, could also have led to the observed lack of differences in SERT binding properties. The characteristics of depression, depression-related treatment outcomes, and serotonergic system involvement, based on 5-HT1A receptor imaging studies, are all well-documented in cases of TLE. Little is known about the same aspects in case of focal extra-temporal epilepsies, and even less about generalized epilepsy syndromes. Although some findings have indicated that depression could be specifically related to TLE and mesial temporal sclerosis [37], this has not been confirmed by other reports [38]. It has been shown that the prevalence of depression is similar between patients with TLE and FLE. There are no reports of focal vs. generalized epilepsy in terms of the prevalence of depression. One work did assess symptoms of anxiety, and found that patients with FLE have much higher anxiety scores than patients with generalized epilepsy [39]. In our study, groups of patients with focal vs. generalized epilepsy were comparable in terms of presence of depressive symptoms.
These previous findings seem to indicate that the bidirectional relationship between epilepsy and depression is not specific to TLE. It has been shown that preoperative depressive symptoms predict postoperative seizure outcome in both TLE and FLE [11]. Therefore, common pathogenic mechanisms may be involved in the etiology of depression comorbid with different epilepsy syndromes, and we would expect that this should be demonstrable in patients having different clinical characteristics of epilepsy, such as those included in the current study. Our findings support the notion that depression and the involvement of the serotonergic system in various epilepsy syndromes requires a deeper exploration with further studies.
Conclusions
The results of our study failed to demonstrate alterations of SERT binding potential in patients with epilepsy with symptoms of depression compared to patients with epilepsy without symptoms of depression. Further studies are needed to clarify the role of SERT and, more generally, the serotonergic system in the common pathogenesis of epilepsy and depression.
Abbreviations
- 123I-ADAM:
-
2-((2-((dimethylamino)methyl)phenyl)thio)-5-(123)iodophenylamine
- SPET:
-
Single photon emission tomography
- SERT:
-
Serotonin transporter
- BDI:
-
Beck depression inventory
- EST-Q:
-
Emotional state questionnaire
- 5-HT:
-
Serotonin
- SSRIs:
-
Selective serotonin reuptake inhibitors
- PET:
-
Positron emission tomography
- TLE:
-
Temporal lobe epilepsy
- ROIs:
-
Regions of interest
- MRI:
-
Magnetic resonance imaging
- FLE:
-
Frontal lobe epilepsy
- AEDs:
-
Antiepileptic drugs
References
Tellez-Zenteno JF, Patten SB, Jetté N, Williams J, Wiebe S: Psychiatric comorbidity in epilepsy: a population-based analysis. Epilepsia. 2007, 48: 2336-2344.
Kanner AM, Schachter SC, Barry JJ, Hersdorffer DC, Mula M, Trimble M, Hermann B, Ettinger AE, Dunn D, Caplan R, Ryvlin P, Gilliam F: Depression and epilepsy: Epidemiologic and neurobiologic perspectives that may explain their high comorbid occurrence. Epilepsy Behav. 2012, 24: 156-168. 10.1016/j.yebeh.2012.01.007.
Alper K, Schwartz KA, Kolts RL, Khan A: Seizure incidence in psychopharmacological clinical trials: an analysis of Food and Drug Administration (FDA) summary basis of approval reports. Biol Psychiatry. 2007, 62: 345-354. 10.1016/j.biopsych.2006.09.023.
Forsgren L, Nyström L: An incident case-referent study of epileptic seizures in adults. Epilepsy Res. 1990, 6: 66-81. 10.1016/0920-1211(90)90010-S.
Hesdorffer DC, Hauser WA, Olafsson E, Ludvigsson P, Kjartansson O: Depression and suicide attempt as risk factors for incident unprovoked seizures. Ann Neurol. 2006, 59: 35-41. 10.1002/ana.20685.
Kanner AM: Depression in epilepsy: a neurobiologic perspective. Epilepsy Curr. 2005, 5: 21-27. 10.1111/j.1535-7597.2005.05106.x.
Cramer JA, Blum D, Reed M, Fanning K, Epilepsy Impact Project Group: The influence of comorbid depression on quality of life for people with epilepsy. Epilepsy Behav. 2003, 4: 515-521. 10.1016/j.yebeh.2003.07.009.
Boylan LS, Flint LA, Labovitz DL, Jackson SC, Starner K, Devinsky O: Depression but not seizure frequency predicts quality of life in treatment-resistant epilepsy. Neurology. 2004, 62: 258-261. 10.1212/01.WNL.0000103282.62353.85.
Hitiris N, Mohanraj R, Norrie J, Sills GJ, Brodie MJ: Predictors of pharmacoresistant epilepsy. Epilepsy Res. 2007, 75: 192-196. 10.1016/j.eplepsyres.2007.06.003.
Kanner AM, Byrne R, Chicharro A, Wuu J, Frey M: A lifetime psychiatric history predicts a worse seizure outcome following temporal lobectomy. Neurology. 2009, 72: 793-799. 10.1212/01.wnl.0000343850.85763.9c.
Metternich B, Wagner K, Brandt A, Kraemer R, Buschmann F, Zentner J, Schulze-Bonhage A: Preoperative depressive symptoms predict postoperative seizure outcome in temporal and frontal lobe epilepsy. Epilepsy Behav. 2009, 16: 622-628. 10.1016/j.yebeh.2009.09.017.
Meyer JH: Imaging the serotonin transporter during major depressive disorder and antidepressant treatment. J Psychiatry Neurosci. 2007, 32: 86-102.
Malison RT, Price LH, Berman R, van Dyck CH, Pelton GH, Carpenter L, Sanacora G, Owens MJ, Nemeroff CB, Rajeevan N, Baldwin RM, Seibyl JP, Innis RB, Charney DS: Reduced brain serotonin transporter availability in major depression as measured by [123I]-2 beta-carbomethoxy-3 beta-(4-iodophenyl)tropane and single photon emission computed tomography. Biol Psychiatry. 1998, 44: 1090-1098. 10.1016/S0006-3223(98)00272-8.
Lehto S, Tolmunen T, Joensuu M, Saarinen PI, Vanninen R, Ahola P, Tiihonen J, Kuikka J, Lehtonen J: Midbrain binding of [123I]nor-beta-CIT in atypical depression. Prog Neuropsychopharmacol Biol Psychiatry. 2006, 30: 1251-1255. 10.1016/j.pnpbp.2006.03.019.
Parsey RV, Hastings RS, Oquendo MA, Huang YY, Simpson N, Arcement J, Huang Y, Ogden RT, Van Heertum RL, Arango V, Mann JJ: Lower serotonin transporter binding potential in the human brain during major depressive episodes. Am J Psychiatry. 2006, 163: 52-58. 10.1176/appi.ajp.163.1.52.
Drevets WC, Frank E, Price JC, Kupfer DJ, Holt D, Greer PJ, Huang Y, Gautier C, Mathis C: PET imaging of serotonin 1A receptor binding in depression. Biol Psychiatry. 1999, 46: 1375-1387. 10.1016/S0006-3223(99)00189-4.
Favale E, Audenino D, Cocito L, Albano C: The anticonvulsant effect of citalopram as an indirect evidence of serotonergic impairment in human epileptogenesis. Seizure. 2003, 12: 316-318. 10.1016/S1059-1311(02)00315-1.
Toczek MT, Carson RE, Lang L, Ma Y, Spanaki MV, Der MG, Fazilat S, Kopylev L, Herscovitch P, Eckelman WC, Theodore WH: PET imaging of 5-HT1A receptor binding in patients with temporal lobe epilepsy. Neurology. 2003, 60: 749-756. 10.1212/01.WNL.0000049930.93113.20.
Lothe A, Didelot A, Hammers A, Costes N, Saoud M, Gilliam F, Ryvlin P: Comorbidity between temporal lobe epilepsy and depression: a [18 F]MPPF PET study. Brain. 2008, 131: 2765-2782. 10.1093/brain/awn194.
Hasler G, Bonwetsch R, Giovacchini G, Toczek MT, Bagic A, Luckenbaugh DA, Drevets WC, Theodore WH: 5-HT1A receptor binding in temporal lobe epilepsy patients with and without major depression. Biol Psychiatry. 2007, 62: 1258-1264. 10.1016/j.biopsych.2007.02.015.
Oya S, Choi SR, Hou C, Mu M, Kung MP, Acton PD, Siciliano M, Kung HF: 2-((2-((dimethylamino)methyl)phenyl)thio)-5-iodophenylamine (ADAM): an improved serotonin transporter ligand. Nucl Med Biol. 2000, 27: 249-254. 10.1016/S0969-8051(00)00084-6.
Chou YH, Yang BH, Chung MY, Chen SP, Su TP, Chen CC, Wang SJ: Imaging the serotonin transporter using (123)I-ADAM in the human brain. Psychiatry Res. 2009, 172: 38-43. 10.1016/j.pscychresns.2008.12.006.
Lin KJ, Liu CY, Wey SP, Hsiao IT, Wu J, Fu YK, Yen TC: Brain SPECT imaging and whole-body biodistribution with [(123)I]ADAM - a serotonin transporter radiotracer in healthy human subjects. Nucl Med Biol. 2006, 33: 193-202. 10.1016/j.nucmedbio.2005.10.006.
Frokjaer VG, Pinborg LH, Madsen J, de Nijs R, Svarer C, Wagner A, Knudsen GM: Evaluation of the Serotonin Transporter Ligand 123I-ADAM for SPECT Studies on Humans. J Nucl Med. 2008, 49: 247-254. 10.2967/jnumed.107.046102.
van de Giessen E, Booij J: The SPECT tracer [123I]ADAM binds selectively to serotonin transporters: a double-blind, placebo-controlled study in healthy young men. Eur J Nucl Med Mol Imaging. 2010, 37: 1507-1511. 10.1007/s00259-010-1424-2.
Newberg AB, Amsterdam JD, Wintering N, Ploessl K, Swanson RL, Shults J, Alavi A: 123I-ADAM binding to serotonin transporters in patients with major depression and healthy controls: a preliminary study. J Nucl Med. 2005, 46: 973-977.
Newberg AB, Amsterdam JD, Wintering N, Shults J: Low brain serotonin transporter binding in major depressive disorder. Psychiatry Res. 2012, 202: 161-167. 10.1016/j.pscychresns.2011.12.015.
Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J: An inventory for measuring depression. Arch Gen Psychiatry. 1961, 4: 561-571. 10.1001/archpsyc.1961.01710120031004.
Aluoja A, Shlik J, Vasar V, Luuk K, Leinsalu M: Development and psychometric properties of the Emotional State Questionnaire, a self-report questionnaire for depression and anxiety. Nord J Psychiatry. 1999, 53: 443-449. 10.1080/080394899427692.
Cannon DM, Ichise M, Rollis D, Klaver JM, Gandhi SK, Charney DS, Manji HK, Drevets WC: Elevated serotonin transporter binding in major depressive disorder assessed using positron emission tomography and [11C]DASB; comparison with bipolar disorder. Biol Psychiatry. 2007, 62: 870-877. 10.1016/j.biopsych.2007.03.016.
Herold N, Uebelhack K, Franke L, Amthauer H, Luedemann L, Bruhn H, Felix R, Uebelhack R, Plotkin M: Imaging of serotonin transporters and its blockade by citalopram in patients with major depression using a novel SPECT ligand [123I]-ADAM. J Neural Transm. 2006, 113: 659-670. 10.1007/s00702-005-0429-7.
Catafau AM, Perez V, Plaza P, Pascual JC, Bullich S, Suarez M, Penengo MM, Corripio I, Puigdemont D, Danus M, Perich J, Alvarez E: Serotonin transporter occupancy induced by paroxetine in patients with major depression disorder: a 123I-ADAM SPECT study. Psychopharmacology (Berl). 2006, 189: 145-153. 10.1007/s00213-006-0540-y.
Ruhé HG, Ooteman W, Booij J, Michel MC, Moeton M, Baas F, Schene AH: Serotonin transporter gene promoter polymorphisms modify the association between paroxetine serotonin transporter occupancy and clinical response in major depressive disorder. Pharmacogenet Genomics. 2009, 19: 67-76. 10.1097/FPC.0b013e32831a6a3a.
van Dyck CH, Malison RT, Staley JK, Jacobsen LK, Seibyl JP, Laruelle M, Baldwin RM, Innis RB, Gelernter J: Central serotonin transporter availability measured with [123I]beta-CIT SPECT in relation to serotonin transporter genotype. Am J Psychiatry. 2004, 161: 525-531. 10.1176/appi.ajp.161.3.525.
Joensuu M, Lehto SM, Tolmunen T, Saarinen PI, Valkonen-Korhonen M, Vanninen R, Ahola P, Tiihonen J, Kuikka J, Pesonen U, Lehtonen J: Serotonin-transporter-linked promoter region polymorphism and serotonin transporter binding in drug-naïve patients with major depression. Psychiatry Clin Neurosci. 2010, 64: 387-393. 10.1111/j.1440-1819.2010.02111.x.
Schenkel LC, Bragatti JA, Torres CM, Martin KC, Gus-Manfro G, Leistner-Segal S, Bianchin MM: Serotonin transporter gene (5HTT) polymorphisms and temporal lobe epilepsy. Epilepsy Res. 2011, 95: 152-157. 10.1016/j.eplepsyres.2011.03.013.
Quiske A, Helmstaedter C, Lux S, Elger CE: Depression in patients with temporal lobe epilepsy is related to mesial temporal sclerosis. Epilepsy Res. 2000, 39: 121-125. 10.1016/S0920-1211(99)00117-5.
Swinkels WA, van Emde BW, Kuyk J, van Dyck R, Spinhoven P: Interictal depression, anxiety, personality traits, and psychological dissociation in patients with temporal lobe epilepsy (TLE) and extra-TLE. Epilepsia. 2006, 47: 2092-2103. 10.1111/j.1528-1167.2006.00808.x.
Tang WK, Lu J, Ungvari GS, Wong KS, Kwan P: Anxiety symptoms in patients with frontal lobe epilepsy versus generalized epilepsy. Seizure. 2012, 21: 457-460. 10.1016/j.seizure.2012.04.012.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2377/13/204/prepub
Acknowledgements
This study was supported by Estonian Science Foundation grant ETF6786.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
ML participated in the conception and design of the study, acquisition and analysis of data, and drafted the manuscript; MP participated in the design of the study, acquisition of SPET data, and revised the manuscript critically; LV participated in the conception of the study, acquisition of data, and revised the manuscript critically; KGP participated in the conception of the study, acquisition of data, and revised the manuscript critically; SH participated in the conception and design of the study, coordinated the study, and revised the manuscript critically. All listed authors have read the manuscript and have given their final approval of the version to be published.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Liik, M., Paris, M., Vahter, L. et al. 123I-ADAM SPET imaging of serotonin transporter in patients with epilepsy and comorbid depression. BMC Neurol 13, 204 (2013). https://doi.org/10.1186/1471-2377-13-204
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2377-13-204