Abstract
Background
Preeclampsia affects 3-8% of pregnancies and is a major cause of maternal and perinatal morbidity and mortality worldwide. This complex disorder is characterized by alterations in the immune and vascular systems and involves multiple organs. There is strong evidence for a genetic contribution to preeclampsia. Two different single nucleotide polymorphisms (SNPs) in the endoplasmic reticulum aminopeptidase 2 (ERAP2) gene were recently reported to be associated with increased risk for preeclampsia in two different populations. ERAP2 is expressed in placental tissue and it is involved in immune responses, inflammation, and blood pressure regulation; making it is an attractive preeclampsia candidate gene. Furthermore, ERAP2 expression is altered in first trimester placentas of women destined to develop preeclampsia.
Methods
A case-control design was used to test for associations between two SNPs in ERAP2, rs2549782 and rs17408150, and preeclampsia status in 1103 Chilean maternal-fetal dyads and 1637 unpaired African American samples (836 maternal, 837 fetal).
Results
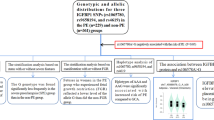
We found that the fetal minor allele (G) of rs2549782 was associated with an increased risk for preeclampsia in the African American population (P = 0.009), but not in the Chilean population. We found no association between rs17408150 and risk for preeclampsia in the Chilean population. Association between rs17408150 and risk for preeclampsia was not tested in the African American population due to the absence of the minor allele in this population.
Conclusions
We report an association between fetal ERAP2 and preeclampsia in an African American population. In conjunction with previous studies, which have found maternal associations with this gene in an Australian/New Zealand population and a Norwegian population, ERAP2 has now been associated with preeclampsia in three populations. This provides strong evidence that ERAP2 plays a role in the development of preeclampsia.
Similar content being viewed by others
Background
Preeclampsia (PE) affects 3-8% of pregnancies worldwide, with rates varying by ethnicity, and leads to potentially devastating complications for both the mother and fetus[1, 2]. Preeclampsia is clinically characterized by high blood pressure and proteinuria, usually occurring after 20 weeks of gestation. Although this serious disorder is common during pregnancy, its etiology remains poorly understood[1]. Preeclampsia is considered a disease of the placenta, with shallow trophoblast invasion[3–5] and poor spiral artery remodeling[6–8] being central features of this disorder. It is postulated that immune, vascular, and inflammatory disturbances participate in the placental dysfunction that ultimately produces the preeclampsia phenotype[9].
A genetic susceptibility to preeclampsia has been established with both maternal and fetal genes contributing to disease[2, 10–17]. Preeclampsia is a multi-factorial trait, with multiple genes, as well as environmental and social factors contributing to disease risk[18–20]. Johnson et al. recently reported that Endoplasmic reticulum aminopepetidase 2 (ERAP2) was associated with preeclampsia in an Australian/New Zealand family-based study and a Norwegian case-control study of maternal samples[21]. Although ERAP2 was associated with risk for preeclampsia in both populations, different polymorphisms of the gene were identified in each group. ERAP2 is expressed in the syncytiotrophoblast and it is a member of the oxytocinase subfamily of M1 aminopeptidases, which are known to play a critical role in the maintenance of normal pregnancy[22–24]. Additionally, ERAP2 is involved in the regulation of blood pressure, immune responses, and pro-inflammatory cytokine production[22, 25–28]. It was recently shown that ERAP2 expression was altered in first trimester placentas of pregnancies destined to develop preeclampsia[29]. The involvement of ERAP2 in multiple pathways known to influence the risk for preeclampsia, its expression in placental tissue, and the previously described altered expression of ERAP2 in placentas before maternal symptoms developed[29]; suggest that the fetal ERAP2 gene contributes to the development of preeclampsia.
In the present study, we investigated whether the previously described associations between ERAP2 and risk for preeclampsia [21] replicated in other ethnic groups and extended our study design past maternal only samples to also include fetal samples. We examined the association between ERAP2 and risk for preeclampsia in two distinct case-control cohorts: Chilean (1103 maternal-fetal dyads) and African American (836 maternal and 837 fetal samples). We genotyped the two SNPs in ERAP2, rs17408150 and rs2549782, that were previously identified as being associated with preeclampsia. Our results demonstrate that the rs2549782 SNP of the fetal ERAP2 gene is significantly associated with risk for preeclampsia in the African American population; further suggesting that this gene plays a key role in the development of disease and may provide insight into the disparity between preeclampsia rates between ethnic groups.
Methods
Chilean study design and population
A case-control study was initiated by searching the clinical database and bank of biological samples of the Perinatology Research Branch (Eunice Kennedy Shriver National Institute of Child Health and Human Development, NIH, DHHS) and included Hispanic women and their neonates in the following groups: 1) Cases - women with preeclampsia and their neonates (n = 528 dyads); and 2) Controls - women who delivered at term with a normal pregnancy outcome and their neonates (n = 575 dyads). Participants received obstetrical care at the Sótero del Río Hospital in Santiago, Chile (an affiliate of the Pontificia Católica de Chile in Santiago, Chile). Exclusion criteria included: (1) known major fetal anomaly or demise; (2) multi-fetal pregnancy; (3) serious maternal medical illness (renal insufficiency, congestive heart disease, etc.); (4) refusal to provide written informed consent; and (5) a clinical emergency, which prevented counseling of the patient about participating in the study, such as fetal distress or maternal hemorrhage. All women provided written informed consent before collection of the samples. The use of clinical data and collection and utilization of maternal and neonatal blood for research purposes was approved by the Institutional Review Boards of the Sótero del Río Hospital, the Eunice Kennedy Shriver National Institute of Child Health and Human Development, NIH, DHHS and Virginia Commonwealth University. Ethnically, the Chilean population is estimated at nearly 95% white and mestizo (mixed white and Amerindian); 3% Amerindian; and 2% other. Mixtures between the conquering Spaniards, largely Andalusians and Basques, and the Mapuches (Araucanians) produced the principle Chilean racial type (2002 census).
African American study design and population
A case-control study was initiated by searching clinical databases and bank of biological samples at the University of Pennsylvania and the Perinatology Research Branch (Eunice Kennedy Shriver National Institute of Child Health and Human Development, NIH, DHHS), at Wayne State University. Study subjects included African American women and neonates in the following groups: 1) Cases - women with preeclampsia (n = 424) and neonates born to women with preeclampsia (n = 375); and 2) Controls - women who delivered at term with a normal pregnancy outcome (n = 412) and neonates delivered at term to women with a normal pregnancy outcome (n = 462). Participants in this study received obstetrical care at the University of Pennsylvania Medical Center, Philadelphia, PA or the Hutzel Women's Hospital, Detroit, MI. The criteria for cases, controls, and exclusion of subjects in the African American study were the same as described for the Chilean study. Of the maternal and neonatal subjects identified, 78% of samples were identified as maternal-neonatal dyads. To obtain adequate sample sizes for this study, therefore, maternal and neonatal samples were tested independently and un-paired samples were included in each group. The use of clinical data and collection and utilization of maternal blood, cord blood, and neonatal cheek swabs for research purposes was approved by the Institutional Review Boards of the University of Pennsylvania, Wayne State University, the Eunice Kennedy Shriver National Institute of Child Health and Human Development, NIH, DHHS, and Virginia Commonwealth University. African American ethnicity was self-reported for all samples.
Clinical definitions
Preeclampsia was defined based on the presence of gestational hypertension (systolic blood pressure ≥140 mmHg and/or diastolic blood pressure ≥90 mmHg) and proteinuria (≥300 mg in a 24-hour urine collection, two or more dipstick measurement of 1+, or one or more dipstick measurement ≥2+) according to ACOG[1] and the National High Blood Pressure Education Program[30]. Patients were considered to have a normal pregnancy outcome if they did not have any medical, obstetrical, or surgical complication, and delivered a term neonate (≥37 weeks) of appropriate birth weight for gestational age[31, 32] without complications.
Sample collection
Maternal blood samples were obtained from the mother at the time of enrollment in the protocol. Umbilical cord blood samples or neonate cheek swabs were obtained immediately after delivery. Blood samples were collected with a vacutainer into tubes containing EDTA. The plasma tubes were balanced and centrifuged at 1300g for 10 minutes at 4°C to separate cellular components from clear plasma, and the samples were stored at -70°C until assay.
DNA extraction
DNA was extracted from maternal and cord blood with a Qiagen Autopure system using standard procedures (Qiagen). DNA was extracted from neonate check swabs using traditional methods as previously described[33].
Genotyping
Single-nucleotide polymorphism analysis was performed using real-time allelic discrimination TaqMan assays (Applied Biosystems) with modifications. All PCR reactions contained 25-75 ng of DNA, 6.25 ul TaqMan Universal Master Mix (Applied Biosystems) (2×), 0.3 ul TaqMan Genotyping Assay (Applied Biosystems) (20×), and water for a final volume of 12.5 ul. Real-time PCR was performed on an ABI 7500 Fast Real-Time PCR Machine (Applied Biosystems) under the following conditions: 50°C for 2 min, 95°C for 10 min, and 40 cycles of amplification (92°C for 15 sec and 60°C for 1 min). For each cycle, the software determined the fluorescent signal from the VIC- or FAM- labeled probe (Applied Biosystems). Allelic discrimination for ERAP2 was performed using TaqMan Genotyping assays C___3282749_20 for SNP rs2549782 and C___25649505_10 for SNP rs17408150 (Applied Biosystems).
Statistical Analysis
Logistic regression in R was used to test for differences in clinical characteristics between disease classes for non-genetic variables. Fisher's exact tests implemented in the PLINK software[34] were used to test individual SNPs for genetic associations with case-control status and to confirm Hardy-Weinberg equilibrium. SNPs with an independent effect were further investigated by multiple logistic regression in R to condition by covariates found to be significantly different between cases and controls in the clinical characteristics analysis. An additive term for the significant SNP(s) was coded as 0, 1, or 2, based on copy number of the minor allele. Allele frequencies from the control groups were used to determine the odds ratios at which our study design had 80% power at an alpha of 0.05. Power calculations were made using the Genetic Power Calculator[35], assuming a 5% disease prevalence.
Results
Clinical Characteristics of the Study Populations
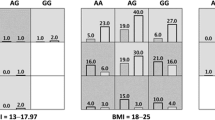
Table 1 displays the demographic and clinical characteristics of mothers and neonates from pregnancies with preeclampsia as well as controls. For Chilean subjects, no significant differences were observed in maternal age or fetal sex between groups. Consistent with previous epidemiologic studies, Chilean patients with preeclampsia showed a significantly higher body mass index (BMI) (P <0.001) and fewer previous live births (P = 0.007). In accordance with preeclampsia resulting in intrauterine growth restriction and indicated preterm birth, offspring born to Chilean women with preeclampsia showed a significantly lower gestational age at delivery and birth weight (P < 0.001). Similar results were observed in African American subjects. Maternal age was not significantly different between cases and controls for either the maternal or the fetal study groups, whereas, gestational age at delivery and birth weight were significantly different between cases and controls for both groups (P < 0.001). Additionally, in the fetal group, mothers with preeclampsia showed a significantly higher BMI (P = 0.049) and fewer previous live births (P = 0.040). Although these measures were not significant in the maternal study group, they were trending in the same direction. In the fetal group, there were significantly more female neonates than male (P = 0.024). Significant differences in fetal sex have been reported in the literature, but results vary with some studies reporting a bias towards male fetuses, some reporting a bias towards female fetuses, and still others reporting no differences in fetal sex in association with preeclampsia[36–44]. No significant difference in fetal sex was observed between cases and controls in the maternal study group.
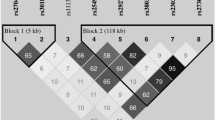
Chilean Population
The minor allele (G) frequencies for rs2549782 in maternal and fetal samples were 0.3386 and 0.3292, respectively. The minor "A" allele frequencies for rs17408150 in maternal and fetal samples were 0.0422 and 0.0395 respectively. The minor allele frequencies are consistent with published data and the Johnson et al. study[21, 45]. Single SNP analysis revealed no associations between ERAP2 polymorphisms rs2549782 and rs17408150 and preeclampsia in either maternal or fetal samples (Table 2). All SNPs were found to be in Hardy-Weinberg equilibrium in the maternal and fetal control samples and no substantial linkage disequilibrium was observed (R2 = 0.087 and 0.072, respectively).
African American Population
The minor allele (G) frequencies for rs2549782 in maternal and fetal samples were 0.4103 and 0.3990 respectively. The minor allele frequencies are consistent with published data and the Johnson et al. study[21, 45]. We did not genotype rs17408150 in this population because the minor "A" allele is reported to be < 1.0% in individuals of African descent[45].
To establish the genetic similarity between the University of Pennsylvania Medical Center and Hutzel Women's Hospital African American samples, and determine if these groups were appropriately combined into a single study population, we compared allele frequencies for three genes: ERAP2, MTHFR, and COMT. Allele frequencies of both COMT and MTHFR are not only known to differ among major ethnic categories, but substantial variation has also been demonstrated in subpopulations of each, including African American[45–51]. Genotypes for MTHFR and COMT were readily available for our samples and based on their aforementioned ethnic variation, they represented ideal genes for the genetic comparison of the two African American sample collection locations. Minor allele frequencies for ERAP2, MTHFR, and COMT were comparable between both African American study sites (Table 3). Additionally, the same COMT haplotype structure was identified in each group and the haplotype frequencies were comparable. The genetic similarity of the two groups across six variable SNPs and COMT haplotype structure and frequency, supported combing the groups into a single African American study population.
Single SNP analysis yielded a significant association between the fetal rs2549782 and preeclampsia in the African American population (P = 0.009), while no association was observed in the maternal SNP (Table 2). Additional multiple logistic regression analysis was performed on the fetal group to adjust for risk factors of preeclampsia (BMI, previous live births, and gravidity) that were found to be significant in the clinical measures analysis (Table 4). rs2549782 remained significant (P = 0.012) and was associated with an increased risk for preeclampsia (OR = 1.529; CI: 1.099, 2.128). Of the previously identified clinical measures tested, only the number of previous live births remained significant, with a larger number of previous live births decreasing the risk for preeclampsia (OR = 0.845; CI: 0.744, 0.960). All SNPs were found to be in Hardy-Weinberg equilibrium in the maternal and fetal groups. Finally, we used two methods to confirm that the positive association we observed was not attributed to population stratification based on the different African American sample collection locations. First, multiple logistic regression analysis was performed in R to test whether there was an interaction between the fetal genotype and the sample collection location. No significant association was observed between a location × fetal rs2549782 interaction and the risk for preeclampsia (P = 0.098). Second, we performed a cluster analysis in PLINK using a Cochran-Mantel-Haenszel model that tested for overall disease/gene association, while controlling for clusters. After controlling for the sample collection location, the fetal rs2549782 was still significantly associated with an increased risk for preeclampsia (P = 0.027; OR = 1.302; CI: 1.029, 1.648). These results, in addition to the absence of evidence for differences in the rates of preeclampsia between African American groups in the United States, justifies combining these samples in this study.
Discussion
Preeclampsia is one of the leading causes of maternal and perinatal morbidity and mortality worldwide; yet its etiology is poorly understood[1]. It is thought that poor placentation and inadequate maternal blood supply lead to placental hypoxia and the placental release of factors that contribute to intravascular inflammation[52–54], generalized endothelial dysfunction[55–59] and the maternal symptoms. A genetic susceptibility to preeclampsia is well established and genes involved with the immune system, inflammation, hemodynamics, endothelial dysfunction, oxidative stress, and angiogenesis have been associated with preeclampsia[10, 15–17]. The identification of genes involved in a variety of physiologic processes reflects the complex nature of this disorder.
It was recently reported by Johnson et al. that the ERAP2 gene was associated with preeclampsia[21]. They found an association with the rs2549782 SNP in an Australian/New Zealand maternal cohort and the rs17408150 SNP in a Norwegian maternal cohort. In the present study, we sought to test whether there were associations between the two previously identified SNPs in ERAP2 and risk for preeclampsia in two distinct ethnic sample sets, Chilean and African American. In contrast to the previous study, we also included fetal samples to determine if the fetal ERAP2 gene was associated with risk for preeclampsia. We were motivated to use this design by the fact that placental tissue is of fetal origin and by interest in determining if any genetic association might be attributed to the sharing of alleles between mother and fetus of one-half, in accordance with Mendelian segregation patterns. We found that, in African Americans, the presence of the minor allele (G) of the rs2549782 SNP in the fetal ERAP2 gene increased the risk for preeclampsia. We found no associations between the two SNPs in the Chilean population, or the rs2549782 SNP of the maternal ERAP2 gene in the African American population.
Preeclampsia is usually diagnosed after 20 weeks of gestation, but it is thought that problems arising early in pregnancy, especially during placentation, are the origin of this disorder. ERAP2 is expressed in the syncytiotrophoblast and it has been reported that expression of this gene was down-regulated in first trimester placentas of women who subsequently developed preeclampsia[23, 29]. The identification of aberrant gene expression, before maternal symptoms develop, suggests a role for ERAP2 early in the disease course.
ERAP2 has the potential to contribute to the development of preeclampsia in multiple ways due to its involvement in the regulation of immune responses, pro-inflammatory cytokine production, and blood pressure[22, 25–28]. Preeclampsia is associated with a predominant T Helper Cell Type 1 (Th1) immune response, which correlates to poor placentation, inflammation, and endothelial dysfunction[60]. One of the primary roles of ERAP2 is Human Leukocyte Antigen (HLA) trimming of class 1-binding peptides. Decreased levels of HLA-G have been reported in the circulation of women with preeclampsia and reduced cell-surface expression has been reported in trophoblasts[22, 27, 61, 62]. Interferon-gamma (IFN γ) regulates both ERAP2 and ERAP1 genes and they have been implicated in immune activation and inflammation[28]. ERAP1, which is closely related to and forms complexes with ERAP2[61], also cleaves the cell surface receptors for pro-inflammatory cytokines.
Pregnancy is a pro-inflammatory state, and inflammation is a key regulator of placentation[52, 54, 63, 64]. Although normal pregnancy is pro-inflammatory, preeclampsia is associated with an exaggerated state of systemic inflammation, and aberrant production of placental cytokines has been widely reported [65]. The placental release of pro-inflammatory cytokines, or the pre-existence of increased inflammation in the maternal vasculature, could both contribute to the development of preeclampsia. In addition to being pro-inflammatory, many cytokines also regulate other processes that are important to the establishment and maintenance of pregnancy. Placentation is tightly regulated by the oxygen balance to ensure adequate remodeling of the maternal spiral arteries and sufficient perfusion of the placenta[66]. Hypoxia Inducible Factor 1α (HIF-1α) is a transcription factor that mediates cellular responses to hypoxia and its expression is altered in preeclampsia[67–69]. HIF-1α is regulated through oxygen dependent and independent mechanisms, and several of the cytokines that are modulated by ERAP2 have been shown to participate in the oxygen independent regulation mechanisms[70].
Finally, ERAP2 regulates blood pressure through the renin-angiotensin (RAS) pathway. Specifically, ERAP2 cleaves Angiotensin III and kallidin, both of which are involved in regulating the dilation and constriction of blood vessels[27]. Abnormalities in the processing of these vasoactive substances could be a cause of maternal high blood pressure, but they also might participate in placental hypoxia, which is a key feature of preeclampsia. Defects in the RAS system have been demonstrated both in the maternal system and fetal tissue[71, 72], further emphasizing the potential for ERAP2 to be involved in the pathophysiology of preeclampsia.
Compared to white women (defined as not African American, Asian, Hispanic, or Native American), Caughey et al. found higher rates of preeclampsia among African American women and lower rates among Hispanic women [2]. Additionally, maternal-paternal ethnic discordance was reported to be associated with an increased incidence[2]. This supports the hypothesis that the genetic basis for preeclampsia is heterogeneic. Our results, in conjunction with the findings of Johnson et al., provide a potential explanation for the observed differences between ethnic groups[21]. Four ethnic populations were examined between the two studies. Allelic variation between European groups, especially Mediterranean, central Europe, and Scandinavia are well characterized and support that they are distinct populations[45–51]. The Chilean population is representative of a Mediterranean ethnic background, specifically from Spanish decent. ERAP2 appears to contribute to the risk for preeclampsia in three of the ethnic groups, with two different allelic variants being associated with risk. Maternal variants increase the risk for preeclampsia in an Australian/New Zealand cohort and a Norwegian cohort[21]. Although preeclampsia is thought to be a placental disorder, the maternal phenotype and, in particular, the susceptibility of the maternal system to disease plays an important role in this disorder[18]. Chronic hypertension, obesity, diabetes, and renal disease, all put a woman at increased risk of developing this disorder. A fetal variant increases the risk for preeclampsia in the African American cohort. Importantly, the placenta is fetal tissue and our results strengthen the argument that primary defects in the placenta play a central role in the development of preeclampsia. Moreover, this finding is consistent with the observation of altered ERAP2 expression in placentas from women who developed preeclampsia.
A strength of our study is the inclusion of both maternal and fetal genes, which gives us the ability to discriminate between maternal and fetal genetic effects. The mother and fetus share fifty percent genetic identity so failure to include both maternal and fetal genes in a study creates the potential for a true association with the unmeasured gene to manifest as an observed association with the measured gene based on the correlation between maternal and fetal genotypes. There is also the potential for both the maternal and fetal ERAP2 genes to contribute to the risk for preeclampsia in a single ethnic population. By measuring only the maternal genes, an additional fetal association could be missed. Thus, the question still remains whether both maternal and fetal ERAP2 contribute to preeclampsia in different ethnic populations where only maternal genes were tested.
A second potential source of variation between ethnicities is the finding that two different SNPs in the ERAP2 gene are associated with risk for preeclampsia. Both of these SNPs are missense mutations that are predicted to alter the three-dimensional structure of the protein and damage function. Additionally, rs2549782 resides within the highly conserved zinc-binding domain. While both SNPs are expected reduce enzyme function, they likely alter function to different degrees and are not equivalent mutations. Moreover, the SNPs reside in different domains of the protein and since ERAP2 has multiple functions, the mutations could have significantly different physiologic consequences.
Alternatively, the observed variation could be explained by differences in linkage disequilibrium (LD) structure between populations or failure to account for larger haplotype structure. Although, the SNPs tested in these studies are predicted to alter enzyme function, they might not represent the causal variant in preeclampsia. These populations might share the same causal variant, but that variant could be in LD with different SNPs in each population. Finally, two haplotypes of ERAP2 have recently been described that lead to changes in mRNA decay and ultimately Major Histocompatibility Complex (MHC) class I presentation on cell surfaces[73]. The haplotypes are composed of numerous SNPs, with rs2549782 representing one of the four coding SNPs that are considered diagnostic[73]. The frequency of each haplotype was estimated to be 0.5 across multiple ethnic groups and similar patterns of long-range LD were also observed; indicating a single ancestral division of functional significance[73]. Neither our study, nor Johnson et al. included the depth of sequencing necessary to characterize the reported haplotypes.
Our findings did not support a genetic association between ERAP2 and the risk for preeclampsia in either the Chilean population or the maternal African American population. However, it should be noted that the present study had limited statistical power to detect very small effects. In the Chilean population, our study was adequately powered to detect Odds Ratios of at least 2.3 for rs17408150 and 1.5-1.7 for rs2549782. In the African American population, our study was adequately powered to detect Odds Ratios of 1.6 - 1.9 for rs2549782. The effect sizes for a single risk factor in a complex disorder are expected to be relatively modest. Furthermore, we only tested for associations between two SNPs in the ERAP2 gene so we are unable to rule out the possibility that different variants of this gene are associated with risk for preeclampsia in these populations. Future studies, increasing the number of markers to saturate the maternal and fetal ERAP2 genes, are needed to characterize the haplotype structures of each group in order to distinguish between maternal and fetal effects of this gene.
Conclusions
Our results show that fetal carriage of the minor allele (G) of rs2549782 in the ERAP2 gene increases the risk for preeclampsia in African Americans. We found no associations between the maternal rs2549782 SNP of the ERAP2 gene and risk for preeclampsia in either the African American or Chilean populations or the rs17408150 SNP of the ERAP2 gene and risk for preeclampsia in the Chilean population. The association of rs2549782 with risk for preeclampsia is consistent with findings of a previous study that found an association of maternal ERAP2 alleles in an Australian/New Zealand population[21]. The results of our study, in combination with those of Johnson et al.[21], describe replicated associations between ERAP2 and preeclampsia in three distinct populations. These observations represent an important step in understanding the pathophysiology of preeclampsia and how genetic variation might play a significant role in ethnic differences.
References
ACOG practice bulletin. Diagnosis and management of preeclampsia and eclampsia. Number 33, January 2002. American College of Obstetricians and Gynecologists. Int J Gynaecol Obstet. 2002, 77 (1): 67-75.
Caughey AB, Stotland NE, Washington AE, Escobar GJ: Maternal ethnicity, paternal ethnicity, and parental ethnic discordance: predictors of preeclampsia. Obstet Gynecol. 2005, 106 (1): 156-161.
Zhou Y, Damsky CH, Chiu K, Roberts JM, Fisher SJ: Preeclampsia is associated with abnormal expression of adhesion molecules by invasive cytotrophoblasts. J Clin Invest. 1993, 91 (3): 950-960.
Kadyrov M, Schmitz C, Black S, Kaufmann P, Huppertz B: Pre-eclampsia and maternal anaemia display reduced apoptosis and opposite invasive phenotypes of extravillous trophoblast. Placenta. 2003, 24 (5): 540-548.
Kadyrov M, Kingdom JC, Huppertz B: Divergent trophoblast invasion and apoptosis in placental bed spiral arteries from pregnancies complicated by maternal anemia and early-onset preeclampsia/intrauterine growth restriction. Am J Obstet Gynecol. 2006, 194 (2): 557-563.
Brosens I: A Study of the Spiral Arteries of the Decidua Basalis in Normotensive and Hypertensive Pregnancies. J Obstet Gynaecol Br Commonw. 1964, 71: 222-230.
Brosens I, Robertson WB, Dixon HG: The physiological response of the vessels of the placental bed to normal pregnancy. J Pathol Bacteriol. 1967, 93 (2): 569-579.
Brosens I: The uteroplacental vessels at term: the distribution and extent of physiological changes. Trophoblast Res. 1988, 3: 61-68.
Ilekis JV, Reddy UM, Roberts JM: Preeclampsia--a pressing problem: an executive summary of a National Institute of Child Health and Human Development workshop. Reprod Sci. 2007, 14 (6): 508-523.
Chesley LC, Annitto JE, Cosgrove RA: The familial factor in toxemia of pregnancy. Obstet Gynecol. 1968, 32 (3): 303-311.
Lie RT, Rasmussen S, Brunborg H, Gjessing HK, Lie-Nielsen E, Irgens LM: Fetal and maternal contributions to risk of pre-eclampsia: population based study. Bmj. 1998, 316 (7141): 1343-1347.
Esplin MS, Fausett MB, Fraser A, Kerber R, Mineau G, Carrillo J, Varner MW: Paternal and maternal components of the predisposition to preeclampsia. N Engl J Med. 2001, 344 (12): 867-872.
Cnattingius S, Reilly M, Pawitan Y, Lichtenstein P: Maternal and fetal genetic factors account for most of familial aggregation of preeclampsia: a population-based Swedish cohort study. Am J Med Genet A. 2004, 130A (4): 365-371.
Skjaerven R, Vatten LJ, Wilcox AJ, Ronning T, Irgens LM, Lie RT: Recurrence of pre-eclampsia across generations: exploring fetal and maternal genetic components in a population based cohort. Bmj. 2005, 331 (7521): 877-
Chappell S, Morgan L: Searching for genetic clues to the causes of pre-eclampsia. Clin Sci (Lond). 2006, 110 (4): 443-458.
Goddard KA, Tromp G, Romero R, Olson JM, Lu Q, Xu Z, Parimi N, Nien JK, Gomez R, Behnke E, et al: Candidate-gene association study of mothers with pre-eclampsia, and their infants, analyzing 775 SNPs in 190 genes. Hum Hered. 2007, 63 (1): 1-16.
Parimi N, Tromp G, Kuivaniemi H, Nien JK, Gomez R, Romero R, Goddard KA: Analytical approaches to detect maternal/fetal genotype incompatibilities that increase risk of pre-eclampsia. BMC Med Genet. 2008, 9: 60-
Ness RB, Roberts JM: Heterogeneous causes constituting the single syndrome of preeclampsia: a hypothesis and its implications. Am J Obstet Gynecol. 1996, 175 (5): 1365-1370.
Di Renzo GC: The great obstetrical syndromes. J Matern Fetal Neonatal Med. 2009, 22 (8): 633-635.
Romero R: Prenatal medicine: the child is the father of the man. 1996. J Matern Fetal Neonatal Med. 2009, 22 (8): 636-639.
Johnson MP, Roten LT, Dyer TD, East CE, Forsmo S, Blangero J, Brennecke SP, Austgulen R, Moses EK: The ERAP2 gene is associated with preeclampsia in Australian and Norwegian populations. Hum Genet. 2009, 126 (5): 655-666.
Tsujimoto M, Hattori A: The oxytocinase subfamily of M1 aminopeptidases. Biochim Biophys Acta. 2005, 1751 (1): 9-18.
Fruci D, Giacomini P, Nicotra MR, Forloni M, Fraioli R, Saveanu L, van Endert P, Natali PG: Altered expression of endoplasmic reticulum aminopeptidases ERAP1 and ERAP2 in transformed non-lymphoid human tissues. J Cell Physiol. 2008, 216 (3): 742-749.
Zhang Y, Cui Y, Zhou Z, Sha J, Li Y, Liu J: Altered global gene expressions of human placentae subjected to assisted reproductive technology treatments. Placenta. 31 (4): 251-258.
Taylor A: Aminopeptidases: structure and function. Faseb J. 1993, 7 (2): 290-298.
Hattori A, Matsumoto H, Mizutani S, Tsujimoto M: Molecular cloning of adipocyte-derived leucine aminopeptidase highly related to placental leucine aminopeptidase/oxytocinase. J Biochem. 1999, 125 (5): 931-938.
Tanioka T, Hattori A, Masuda S, Nomura Y, Nakayama H, Mizutani S, Tsujimoto M: Human leukocyte-derived arginine aminopeptidase. The third member of the oxytocinase subfamily of aminopeptidases. J Biol Chem. 2003, 278 (34): 32275-32283.
Tanioka T, Hattori A, Mizutani S, Tsujimoto M: Regulation of the human leukocyte-derived arginine aminopeptidase/endoplasmic reticulum-aminopeptidase 2 gene by interferon-gamma. Febs J. 2005, 272 (4): 916-928.
Founds SA, Conley YP, Lyons-Weiler JF, Jeyabalan A, Hogge WA, Conrad KP: Altered global gene expression in first trimester placentas of women destined to develop preeclampsia. Placenta. 2009, 30 (1): 15-24.
Report of the National High Blood Pressure Education Program Working Group on High Blood Pressure in Pregnancy. Am J Obstet Gynecol. 2000, 183 (1): S1-S22.
Alexander GR, Kogan M, Martin J, Papiernik E: What are the fetal growth patterns of singletons, twins, and triplets in the United States?. Clin Obstet Gynecol. 1998, 41 (1): 114-125.
Gonzalez RP, Gomez RM, Castro RS, Nien JK, Merino PO, Etchegaray AB, Carstens MR, Medina LH, Viviani PG, Rojas IT: [A national birth weight distribution curve according to gestational age in Chile from 1993 to 2000]. Rev Med Chil. 2004, 132 (10): 1155-1165.
Wang H, Parry S, Macones G, Sammel MD, Ferrand PE, Kuivaniemi H, Tromp G, Halder I, Shriver MD, Romero R, et al: Functionally significant SNP MMP8 promoter haplotypes and preterm premature rupture of membranes (PPROM). Hum Mol Genet. 2004, 13 (21): 2659-2669.
Purcell S, Neale B, Todd-Brown K, Thomas L, Ferreira MA, Bender D, Maller J, Sklar P, de Bakker PI, Daly MJ, et al: PLINK: a tool set for whole-genome association and population-based linkage analyses. Am J Hum Genet. 2007, 81 (3): 559-575.
Purcell S, Cherny SS, Sham PC: Genetic Power Calculator: design of linkage and association genetic mapping studies of complex traits. Bioinformatics. 2003, 19 (1): 149-150.
Toivanen P, Hirvonen T: Sex ratio of newborns: preponderance of males in toxemia of pregnancy. Science. 1970, 170 (954): 187-188.
Juberg RC, Gaar DG, Humphries JR, Cenac PL, Zambie MF: Sex ratio in the progeny of mothers with toxemia of pregnancy. J Reprod Med. 1976, 16 (6): 299-302.
Campbell DM, MacGillivray I, Carr-Hill R, Samphier M: Fetal sex and pre-eclampsia in primigravidae. Br J Obstet Gynaecol. 1983, 90 (1): 26-27.
Arngrimsson R, Walker JJ, Geirsson RT, Bjornsson S: A low male/female sex ratio in offspring of women with a family history of pre-eclampsia and eclampsia. Br J Obstet Gynaecol. 1993, 100 (5): 496-497.
Sanchez AR, Macho JE, Estrada HV, Gonzalez AL: [Does the gender of the fetus determine the severity of preeclampsia-eclampsia?]. Ginecol Obstet Mex. 1996, 64: 18-20.
Khong TY, Staples A, Chan AS, Keane RJ, Wilkinson CS: Pregnancies complicated by retained placenta: sex ratio and relation to pre-eclampsia. Placenta. 1998, 19 (8): 577-580.
Makhseed M, Musini VM, Ahmed MA: Association of fetal gender with pregnancy-induced hypertension and pre-eclampsia. Int J Gynaecol Obstet. 1998, 63 (1): 55-56.
Basso O, Olsen J: Sex ratio and twinning in women with hyperemesis or pre-eclampsia. Epidemiology. 2001, 12 (6): 747-749.
Jongbloet PH: Offspring sex ratio at population level versus early and late onset preeclampsia. Early Hum Dev. 2004, 79 (2): 159-163.
Sherry ST, Ward MH, Kholodov M, Baker J, Phan L, Smigielski EM, Sirotkin K: dbSNP: the NCBI database of genetic variation. Nucleic Acids Res. 2001, 29 (1): 308-311.
Stevenson RE, Schwartz CE, Du YZ, Adams MJ: Differences in methylenetetrahydrofolate reductase genotype frequencies, between Whites and Blacks. Am J Hum Genet. 1997, 60 (1): 229-230.
van der Put NM, Eskes TK, Blom HJ: Is the common 677C-->T mutation in the methylenetetrahydrofolate reductase gene a risk factor for neural tube defects? A meta-analysis. Qjm. 1997, 90 (2): 111-115.
Schneider JA, Rees DC, Liu YT, Clegg JB: Worldwide distribution of a common methylenetetrahydrofolate reductase mutation. Am J Hum Genet. 1998, 62 (5): 1258-1260.
Palmatier MA, Kang AM, Kidd KK: Global variation in the frequencies of functionally different catechol-O-methyltransferase alleles. Biol Psychiatry. 1999, 46 (4): 557-567.
Schwahn B, Rozen R: Polymorphisms in the methylenetetrahydrofolate reductase gene: clinical consequences. Am J Pharmacogenomics. 2001, 1 (3): 189-201.
Domschke K, Deckert J, O'Donovan M C, Glatt SJ: Meta-analysis of COMT val158met in panic disorder: ethnic heterogeneity and gender specificity. Am J Med Genet B Neuropsychiatr Genet. 2007, 144B (5): 667-673.
Redman CW, Sargent IL: Pre-eclampsia, the placenta and the maternal systemic inflammatory response--a review. Placenta. 2003, 24 (Suppl A): S21-27.
Gervasi MT, Chaiworapongsa T, Pacora P, Naccasha N, Yoon BH, Maymon E, Romero R: Phenotypic and metabolic characteristics of monocytes and granulocytes in preeclampsia. Am J Obstet Gynecol. 2001, 185 (4): 792-797.
Redman CW, Sargent IL: Placental stress and pre-eclampsia: a revised view. Placenta. 2009, 30 (Suppl A): S38-42.
Roberts JM, Taylor RN, Musci TJ, Rodgers GM, Hubel CA, McLaughlin MK: Preeclampsia: an endothelial cell disorder. Am J Obstet Gynecol. 1989, 161 (5): 1200-1204.
Roberts JM, Taylor RN, Goldfien A: Clinical and biochemical evidence of endothelial cell dysfunction in the pregnancy syndrome preeclampsia. Am J Hypertens. 1991, 4 (8): 700-708.
Maynard SE, Min JY, Merchan J, Lim KH, Li J, Mondal S, Libermann TA, Morgan JP, Sellke FW, Stillman IE, et al: Excess placental soluble fms-like tyrosine kinase 1 (sFlt1) may contribute to endothelial dysfunction, hypertension, and proteinuria in preeclampsia. J Clin Invest. 2003, 111 (5): 649-658.
Levine RJ, Maynard SE, Qian C, Lim KH, England LJ, Yu KF, Schisterman EF, Thadhani R, Sachs BP, Epstein FH, et al: Circulating angiogenic factors and the risk of preeclampsia. N Engl J Med. 2004, 350 (7): 672-683.
Powers RW, Catov JM, Bodnar LM, Gallaher MJ, Lain KY, Roberts JM: Evidence of endothelial dysfunction in preeclampsia and risk of adverse pregnancy outcome. Reprod Sci. 2008, 15 (4): 374-381.
Saito S, Sakai M: Th1/Th2 balance in preeclampsia. J Reprod Immunol. 2003, 59 (2): 161-173.
Saveanu L, Carroll O, Lindo V, Del Val M, Lopez D, Lepelletier Y, Greer F, Schomburg L, Fruci D, Niedermann G, et al: Concerted peptide trimming by human ERAP1 and ERAP2 aminopeptidase complexes in the endoplasmic reticulum. Nat Immunol. 2005, 6 (7): 689-697.
Sargent IL, Borzychowski AM, Redman CW: Immunoregulation in normal pregnancy and pre-eclampsia: an overview. Reprod Biomed Online. 2006, 13 (5): 680-686.
Borzychowski AM, Sargent IL, Redman CW: Inflammation and pre-eclampsia. Semin Fetal Neonatal Med. 2006, 11 (5): 309-316.
Moffett A, Hiby SE: How Does the maternal immune system contribute to the development of pre-eclampsia?. Placenta. 2007, 28 (Suppl A): S51-56.
Rusterholz C, Hahn S, Holzgreve W: Role of placentally produced inflammatory and regulatory cytokines in pregnancy and the etiology of preeclampsia. Semin Immunopathol. 2007, 29 (2): 151-162.
Caniggia I, Winter JL: Adriana and Luisa Castellucci Award lecture 2001. Hypoxia inducible factor-1: oxygen regulation of trophoblast differentiation in normal and pre-eclamptic pregnancies--a review. Placenta. 2002, 23 (Suppl A): S47-57.
Semenza GL: Hypoxia-inducible factor 1: master regulator of O2 homeostasis. Curr Opin Genet Dev. 1998, 8 (5): 588-594.
Becker CM, Rohwer N, Funakoshi T, Cramer T, Bernhardt W, Birsner A, Folkman J, D'Amato RJ: 2-methoxyestradiol inhibits hypoxia-inducible factor-1{alpha} and suppresses growth of lesions in a mouse model of endometriosis. Am J Pathol. 2008, 172 (2): 534-544.
Kanasaki K, Kalluri R: The biology of preeclampsia. Kidney Int. 2009, 76 (8): 831-837.
Patel J, Landers K, Mortimer RH, Richard K: Regulation of Hypoxia Inducible Factors (HIF) in Hypoxia and Normoxia During Placental Development. Placenta. 31 (11): 951-957.
Irani RA, Xia Y: The functional role of the renin-angiotensin system in pregnancy and preeclampsia. Placenta. 2008, 29 (9): 763-771.
Vefring HK, Wee L, Jugessur A, Gjessing HK, Nilsen ST, Lie RT: Maternal angiotensinogen (AGT) haplotypes, fetal renin (REN) haplotypes and risk of preeclampsia; estimation of gene-gene interaction from family-triad data. BMC Med Genet. 11: 90-
Andres AM, Dennis MY, Kretzschmar WW, Cannons JL, Lee-Lin SQ, Hurle B, Schwartzberg PL, Williamson SH, Bustamante CD, Nielsen R, et al: Balancing selection maintains a form of ERAP2 that undergoes nonsense-mediated decay and affects antigen presentation. PLoS Genet. 6 (10): e1001157-
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2350/12/64/prepub
Acknowledgements and funding
This study was supported, in part, by P60MD002256 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, NIH, DHHS; R01HD034612 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, NIH, DHHS; UL1RR031990 from the National Center for Research Resources and the NIH Roadmap for Medical Research, NIH; University of Pennsylvania Research foundation grant, K12HD001265 (PI Driscoll; Scholar Srinivas) from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, NIH, DHHS; the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development, NIH, DHHS; and 1T32HLO94290-01A1 from the National Heart, Lung, and Blood Institute, NIH, DHHS.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
LDH participated in the design of the study, performed experiments, performed the statistical analysis, and drafted the manuscript. DDH performed experiments. TPY participated in the design of the study, participated in the statistical analysis, and helped to draft the manuscript. JPK provided Chilean and African American purified DNA for use in this study and helped to draft the manuscript. RG coordinated sample collection of Chilean subjects with JPK and RR and helped to draft the manuscript. MAE provided African American DNA for use in this study and helped to draft the manuscript. RR provided Chilean and African American DNA for use in this study and helped to draft the manuscript. JFS conceived of the study, participated in its design and coordinated and helped to draft the manuscript. SS provided African American purified DNA for use in this study and helped to draft the manuscript. All authors have read and approved the final manuscript.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Hill, L.D., Hilliard, D.D., York, T.P. et al. Fetal ERAP2 variation is associated with preeclampsia in African Americans in a case-control study. BMC Med Genet 12, 64 (2011). https://doi.org/10.1186/1471-2350-12-64
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2350-12-64